How to use this guide
This guide helps integrated care boards (ICBs) to assess the effectiveness of the information they collect and use. Using information insightfully – supported by robust corporate governance arrangements – enables the ICB board to:
- be assured the organisation is meeting its statutory duties
- spot early warning signs of quality, performance or financial issues across the system
- ensure that care provided across the system is continuously improving and services meet the population’s current and future needs
- stand back and consider whether the ICB’s leadership, culture, systems and processes are getting the right results
This guide is built around the 6 functional areas which underpin how ICBs deliver their purpose. It suggests, within each functional area, a range of indicators, information and lines of enquiry to help ICBs – it does not mean that ICBs need to structure their board reporting in this way. It is not a checklist of data and behaviours; it is a starting point that ICB boards can adapt and develop in line with their needs, reflecting the scale and complexity of their systems. This similar guidance is for boards of NHS providers.
This guide is structured as follows:
- chapter 1: expectations of ICB boards, and ICBs’ core purpose and functions
- chapter 2: high level principles which underpin the effective use of information
- chapter 3: suggested information sets to support the delivery of each function
- chapter 4: considerations for processes and practices
NHS England’s oversight and assessment of ICBs
The ICB board and NHS England have a common interest in assessing the performance of the ICB and enabling its success. It is the ICB board’s responsibility to ensure the organisation is meeting its duties, and NHS England has the statutory power to intervene if it is failing or is at risk of failure.
The board needs to understand current performance of both the ICB and partner organisations against local and national metrics and the causes of any underperformance. However, these metrics do not represent the full range of information that ICBs should look at, which is why this guide goes further and sets out other types of information for systems to consider to meet their overall objectives. ICB boards should frequently consider each domain as they manage services, reduce health inequalities and plan.
Read this framework which sets out how NHS England gains assurance from ICBs that they are exercising their delegated primary care functions safely, effectively and in line with legal requirements. ICBs need to assure themselves they are complying with these obligations.
1. The ICB board’s role
Core purpose of integrated care systems
As the NHS leader in the integrated care system, ICBs need to demonstrate strong system leadership and foster a culture of collaboration and co-operation to deliver ICS’s 4 core purposes. These are to:
- improve population health and healthcare
- tackle inequalities in outcomes, experience and access
- enhance productivity and value for money
- help the NHS support broader social and economic development
6 core functions underpin delivery of these:
- strategy and planning
- leadership of the NHS
- arranging for the provision of healthcare services (strategic commissioning)
- assuring performance, quality and delivery
- securing transformation and learning
- governance and people
ICBs have responsibilities to:
- their community, for the quality and safety of services provided, through a range of mechanisms, from citizens’ juries and panels to local oversight and scrutiny committees
- the public, for the responsible use of taxpayers’ funds
- providers, for their professional conduct as commissioners of care
- the Integrated Care Partnership (ICP) and its partner members, using the integrated care strategy to inform system strategy
- NHS England (including any functions delegated to it by NHS England)
What this means for the ICB board
ICB boards are responsible for co-ordinating and supporting the provision of high-quality healthcare to their communities, encompassing primary and secondary care services. It is their responsibility to ensure the organisation is successfully discharging its duties today and will continue to do so in the future.
It does this principally in meetings of the board, including board development sessions and board committees, to secure assurance that effective executive accountability and delivery arrangements are in place, target performance is being achieved, and delivery plans are well founded and progress against them is being made. It is principally the responsibility of the chair to ensure the board and its committees are constituted and supported by appropriate governance arrangements to undertake this task effectively.
The questions ICB boards need to ask themselves continuously are:
- are we meeting our statutory duties and regulatory requirements?
- are we having a positive impact on the communities we serve?
- are the ways of working, systems and processes effective to deliver the ICP strategy?
To be effective, ICB boards need to use information to:
- plan effectively: look at what is driving changes in demand, identify services which can help tackle immediate and long-term conditions, reduce avoidable ill-health and eliminate inequalities – and in parallel ensure workforce and capital plans reflect these areas
- manage resources: based on what the organisation knows about care needs across the system’s communities and strategic priorities, establish a focused set of delivery and outcome expectations to make the most effective use of budgets and resources
- ensure high-quality care is being provided: understand the provider landscape across different services, the collaborative(s), place(s) and other dynamics between organisations and procure cost-effective services to improve outcomes and wider population health
- have assurance about care being delivered: use timely, accurate information on the quality and efficiency of care provided to gain assurance on the services being commissioned, pre-empt any issues and identify areas of improvement
- consider risks and mitigations: identify, evaluate and manage risks to the ICB’s strategic and operational objectives. Information should support boards to determine the level and type of risks acceptable to the organisation, and what is deemed appropriate for assurance and ensuring effective controls have been implemented. ICB boards must ensure their own organisation is well-run and operates effectively, setting the tone and culture of their organisation and their system. They must be assured their organisation delivers its statutory responsibilities and correctly discharges the functions NHS England has delegated to it. Boards also have a responsibility to ensure there is a system-wide focus on improvement, learning and innovation
Effective governance arrangements
Effective governance is essential for the quality and timely flow of information to and from the board. This is critical for the board to make the right decisions to improve services and build trust among its system partners, patients and communities.
‘Active’ governance means issues are considered by the most appropriate people, relevant information is reviewed in the most useful format at the right time, and the level of scrutiny produces rigorous challenge and an effective response.
Reporting structures must be complemented by clear and effective policies and procedures which are well understood in the organisation and kept under regular review. These policies should clearly set out:
- standing orders for how the ICB carries out its business
- nominated/designated individuals where appropriate
- financial instructions which detail the financial thresholds and limits that apply to the organisation and its budget holders
- schemes of reservation and delegation which set out where responsibility and accountabilities lie and where they have been delegated to committees, executives or other forums. ICBs must ensure these schemes address the functions that are formally delegated to them by NHS England (for example, primary care commissioning)
- clear mechanisms for escalation to the board – from within the organisation as well as system partners – and for the cascading of decisions throughout the organisation and to the wider system
Schemes of delegation are especially important when organisations consider new models of collaboration, including across systems, to deliver care differently. Boards must be clear where decision-making and accountability sits when making any changes to the organisation’s delegated functions.
An organisation’s governance is constantly evolving. As the drivers and conditions for effective governance change, for example, leadership changes or the organisation refocuses or restructures, regular reviews ensure governance remains fit for purpose.
Board committees
ICB boards should make best use of board committees, delegating functions and responsibilities that are best considered in these forums to allow more dedicated time for detailed review. These can be standing committees (for example, Audit, Finance, Quality) or time-limited, for example, if a board has requested a focus on a particular topic (such as population health) or programme that requires more detailed oversight and scrutiny, such as a major transformation or investment programme. Read the guidance on ICB constitutions and governance on NHS England’s website.
Boards should review committees’ effectiveness as well as structure regularly (at least annually) to ensure they are fit for purpose and support board governance and organisational oversight.
Committees should report regularly to the board, and in a balanced and insightful way which does not simply repeat the information and discussion that has taken place at the committee.
Confidence in information presented – assurance or reassurance?
When receiving reports, the board and its committees should ensure there is a balance of assurance and reassurance in the information it receives. Boards need to have confidence that the information is a true reflection of performance and improvement and there are no other issues or considerations arising that warrant further review. The diagram below outlines the questions and lines of enquiry board members should be pursuing.
One of the benefits non-executive board members (NEMs) bring to board and committee performance is by providing independent perspectives on how the data and other information are scrutinised. To foster a diverse experience base, each NEM can sit on multiple committees, for example, quality and finance, so they can gain different perspectives.
Figure 1: lines of enquiry board members should be pursuing
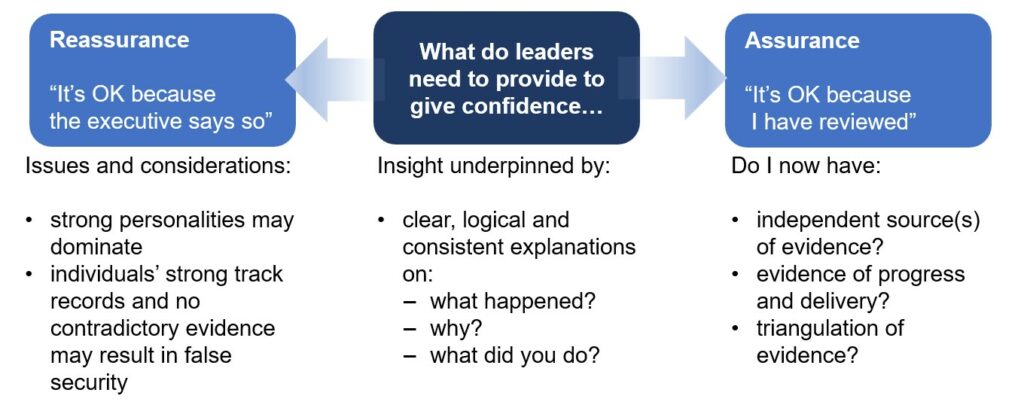
Issues and considerations:
strong personalities may dominate
individuals’ strong track records and no contradictory evidence may result in false security
What do leaders need to provide to give confidence…
Insight underpinned by:
clear, logical and consistent explanations on:
what happened?
why?
what did you do?
Assurance – “It’s OK because I have reviewed”
Do I now have:
independent source(s) of evidence?
evidence of progress and delivery?
triangulation of evidence?
Well-led, successful boards should be scrutinising the information and data presented to them. Crucial to this is having an open and curious mindset, with board members actively seeking to uncover issues and find solutions. To this end, boards should be promoting a transparent reporting culture throughout their organisation and the wider system, so that information or data perceived as negative are not suppressed or made to appear less negative.
2. Meaningful information
The information ICB boards rely on to carry out their role will be qualitative, quantitative and sometimes open to interpretation or judgement. This information helps the ICB board to:
- understand their population’s health needs and identify any inequalities to assess current and unmet needs or gaps in care provision
- set strategic plans and identify the short, medium and long-term KPIs and milestones to assess delivery
- identify providers and partners able to deliver care at the requisite level of quality, access and efficiency
- gain assurance on the short-term delivery of services and the longer-term population health improvements and post-care outcomes
- have the confidence to ask uncomfortable questions regarding variations in quality and parity of care across the ICB and take steps to address them
- oversee planning and delivery of strategic improvement and transformation across the system
- obtain the appropriate granularity and transparency of performance information by place or locality – recognising that some ICBs will have a greater number of these than others
- baseline and benchmark performance across the ICB and compare it to ‘statistical neighbours’ – other ICBs or places with similar characteristics – peer groups and national trends
In some cases, boards will need to use different types of information to ‘triangulate’ a particular topic or issue, for example, using qualitative intelligence to support or challenge information from quantitative sources and vice versa (see below).
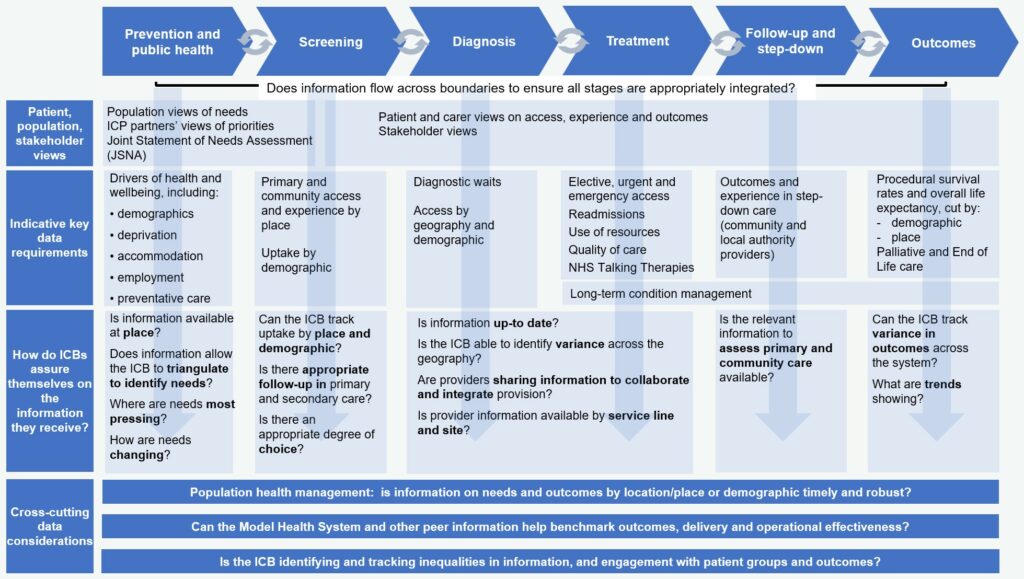
Boards should make a clear distinction between strategic and operational matters, focusing their attention on a limited number of priority areas for each. Strong working relationships with business intelligence and analytical teams across the system is integral to ensuring information available to the board and ICB is high quality and timely. Figure 2 sets out some of the main data considerations for boards.
Figure 2. Suggested information considerations for ICB boards
Information and corporate governance – processes and structures
An effective and high-performing board needs to be supported by a robust corporate governance structure that enables the seamless flow of information and decision-making up and down the organisation. This structure needs to be complemented with policies on risk, escalation and delegation for the board to operate effectively.
Board-level information
Boards should not review too many metrics or other sources of intelligence at any one time as this results in information overload. To avoid this, adopt a consistent approach for reporting and apply it across the organisation, with appropriate data being viewed in the most suitable forums and robust escalation processes being implemented alongside. Boards should consider the appropriate frequency at which certain metrics are brought to their attention.
Findings with a material importance for the organisation should be identified and reported promptly through the board and analysed through a thematic lens.
When reviewing information, the board should be cognisant of the culture and behaviours across the organisation and how they may impact on what it receives. The board should also ensure the information reflects the views of stakeholders and patient, carer and public voices. Boards need to consider how this information is collected and communicated, whether specific resources are allocated to support information gathering and generation of intelligence, and what the threshold is for direct reporting to the board. They also need to consider what information should be used to hold themselves and their chief executive to account.
Using information
The NHS generates a lot of data. Boards do not need to see every metric every month, otherwise they would be overwhelmed. Information needs to be scrutinised at the right level in the organisation and reviewed or escalated accordingly. Information presented must:
- be timely, reflecting the most recent data available
- cover both improvement – using statistical methods to track trends over time, looking at variation and not just comparing against targets at a point in time – and assurance – looking at whether standards are being met and comparing performance against relevant historical data or external benchmarks
- be valid and subject to review – are the measures fit for purpose? How much weight can be placed on the data?
- allow for deep dives to understand care quality and performance within a directorate, department, team, service and at the point of care
Presenting information to ICB boards
Information presented to the board will mostly focus on delivery of the ICB’s 6 core functions. The frequency and reporting of metrics depends on requirements, data availability, how quickly the data may change and the board reporting cycle. Boards need to agree the frequency at which indicators are reported (which may include bespoke local priority areas). Boards also need to consider the areas of data which require development, for example due to incompleteness, such as primary and community services. Information for boards should adhere to these principles:
- be clearly and simply presented
- highlight variation in performance, activity and outcomes using Statistical Process Control (SPC) charts
- combine clear and accessible graphic overviews and statistical summaries alongside brief commentary, with detailed statistics and data reporting provided by exception
- incorporate trends, forecasts and benchmarks
- balance retrospective and prospective information
- use the same data sources, where possible, as other organisations, providers and commissioners within the system
Information presented to the board should direct their attention to significant risks, issues and exceptions – particularly deteriorating or worsening trends – although there is value in avoiding a negativity bias. Successes, good performance and examples of successful innovation, intervention and improvement should be highlighted.
The test of whether the information provided to the board has had an impact is the extent to which it is readily interpretable and provides assurance, stimulates debate, leads to insight and informs decision making. Effective use of information provides early warning of potential quality, performance, financial or other problems, and should develop all board members’ understanding of the organisation, the local health economy and its performance. This information needs to be complemented by qualitative information, which can provide alternative perspectives including staff and patient voices.
Some metrics may lend themselves to dashboard style reporting, while others may generate more insight if they are presented as thematic reports to inform in-depth discussions of specific areas at board meetings.
Papers should always be provided with adequate time for members to review and scrutinise the information in advance. Board members should have access to information online and in between meetings. Reporting and the assurance of performance and issues provided within it may also need to be supplemented with more in-depth discussions of specific areas at board meetings.
Triangulation
Boards will often be presented with a range of information cutting across multiple areas of activity. Seemingly non-related elements can, when taken together, reflect an underlying issue that otherwise may not have been picked up in time. Other information may highlight unintended consequences of policies or decisions that need drilling down into.
Consequently, boards should always be aware of potential interlinkages, triangulating where necessary to identify and focus in on the root causes of emerging issues. Boards should triangulate data – using information to provide different perspectives on, for example, population health needs, organisational performance and long-term outcomes.
Triangulation in a system context
Triangulation uses multiple indicators and types of information to gain insight into complex areas that cannot necessarily be measured using metrics alone. In healthcare, this can be a powerful tool to identify ‘hard truths’, inform decision-making, and lead to better outcomes in patient safety and experience, performance and clinical quality and workplace culture.
For an ICB, triangulation can be particularly effective to understand how services are being delivered by partners. For example, a combination of poor staff survey results, Freedom to Speak Up (FTSU) reports and high staff sickness absence could indicate a workplace culture problem, and a combination of patient complaints, poor Friends and Family Test feedback, and performance waiting times exceeding local and national trends could identify a ‘red flag’ in service delivery.
Using national and local data
While most data considered by boards is drawn from local systems, boards must also consider national data and reviews. National dashboards and data sources such as the Model Health System can provide opportunities for benchmarking and review of progress against national targets and comparable peer ICBs and may draw out themes such as health inequalities which may be less evident from local data alone. Board members can use these alongside the information presented in board packs to ensure they are forming a broad understanding and triangulating the information they receive. Improvement tools such as NHS IMPACT and national and local clinical audits can also support ICBs to understand their data and focus their improvement resource to improve population outcomes.
Availability of data and analytical tools
Data literacy and understanding the nuances of statistics and data reporting will vary across a board. ICB boards should consider training and support requirements, for example NHS England’s Making Data Count team provides board development sessions with a focus on using SPC (rather than traditional reporting styles such as RAG reporting) to aid them in understanding how data can be best visualised to guide effective discussion and decision-making.
SPC is one of the most effective analytical approaches to guide decision-making, looking at data over time using a control chart to reveal the type of variation in a process. There is a strong evidence base which demonstrates the benefits to decision makers of this easily understood and statistically robust approach. Effective approaches to understanding variation between systems include the use of funnel plots and distribution charts. Using appropriate ‘statistical neighbours’ can lead to greater insight and learning on more effective approaches and best practice.
Many boards now use SPC as the primary method of analysis to understand quality, performance, workforce and finance data. Boards have reported several benefits* including:
- a strengthened ability to challenge
- reduced time being distracted by insignificant changes in data
- better governance processes
- greater clarity on where the board should focus its attention
*BMJ leader paper describes the impact of Making Data Count board training: National Health Service trust boards adopt statistical process control reporting: the impact of the Making Data Count Training Programme
Read the best practice sample format for an integrated performance report (IPR). This uses a range of SPC views to identify variation and focus the board’s attention on priority areas for action.
Analytical capability of systems and the availability of cutting-edge analytics will vary. This may constrain the effective communication of data and statistics to the board. The wider data landscape of the system, such as population health data at place and neighbourhood level and shared care records, are integral to a board’s ability to be well informed and more data-led in its decision-making.
3. ICB functional areas
ICBs differ in terms of their geography, population, demographics and wider determinants of health. However, there are some principles that all boards can apply to how they use information to deliver their objectives.
For each of the 6 functional areas, this guide includes:
- a set of questions boards should ask themselves to be effective
- the information ICBs should consider using to answer these
The framework ICBs choose to use needs to be flexible enough to balance the crucial ingredients of success in financial, operational and quality terms, and cover the perspectives of patients, commissioners, providers and local stakeholders, along with regulatory requirements and the delivery of NHS England delegated functions. Ultimately, it should allow ICBs to select and modify those indicators most relevant to them considering their own strategic priorities.
General principles
When reviewing an indicator, boards should consider:
- the frequency at which the information is available and the underlying rate of change
- triangulation with other indictors and information to gain an insight into a complex area or root causes
- benchmarking against peers and regional and national averages (for example using the Model Health System)
- variation across areas such as population groups, sub-ICB areas and providers
- health inequalities by deprivation and population groups
- using statistical analysis to help interpret if differences or changes over time require further investigation
The information boards need covers all areas of care, including primary, where ICBs have a unique role to ensure the population can access the care they need now and in the future. In some of the suggested areas there are gaps in the information which is routinely available, for example, data is available on almost all hospital activity but generally not for primary and community health and care services where availability and quality vary regionally.
The metrics have been developed with ICBs and will be amended annually based on ICB feedback.
A. Strategy and planning
ICB boards provide strategic oversight of their system, ensuring their partner organisations deliver against their – and the wider system – objectives. ICBs are accountable for the management of care at all levels. The system strategy should optimise the way resources are used and allocated to mitigate clinical and financial risk while improving outcomes, tackling inequalities and contributing to broader social development.
To develop a credible strategy which optimises the way funds and resources are deployed, ICB boards need to receive high quality information to understand the current and future health needs of their populations and the current and future patterns of healthcare delivery and commissioning in their region.
Strategic information should help the board understand trends in health needs, provision and patient satisfaction, and provide forecasts and anticipate future performance issues and changes in population needs. This should include an external focus and understanding of the context for reform and local opinion.
To tackle inequalities the board needs to understand variation across population groups and within systems at provider, place and neighbourhood level and to understand how performance is changing over time.
Boards should ensure there is ongoing evaluation of the impact of strategic improvement and change programmes.
Elements of successful strategy development include understanding the current challenges within the system and expected trends in disease to ensure the strategy can be developed to drive future care models which best meet the population needs within available resources. Boards need to focus on:
- population health and demand forecasting: the information boards receive should enable them to regularly review current and future health needs of the local population using a population health management This will help boards understand changes in needs over time as well as health inequality trends and progress
- current provision and activity planning: boards need to receive information that enables them to understand the challenges and opportunities of service provision, including performance of acute and primary care and information on finance, workforce and digital challenges
- resource planning: boards need to use information to allocate resources, considering capital and workforce, in line with the activity plans
- integrated community based and preventative care: better outcomes are achieved for people with long-term conditions when they are treated earlier and closer to home. Therefore, the board’s strategy should ensure care is provided in an increasingly joined-up and integrated fashion to improve the health and wellbeing of the population by:
- addressing fragmentation through place-based partnerships
- evolving primary care networks towards integrated neighbourhood teams (teams of teams) and provider collaboratives
- using population health management approaches
- collaborating even more closely with ICP partners, local authorities, VCSE organisations and care providers
- local engagement: it is critical that ICBs involve local populations in how they plan and provide health and care services, service reconfigurations and identify healthcare needs. ICB boards should ensure patients and service users are engaged with, and that perspectives from those with lived experience reach the board and are heard regularly
- collaboration: ICBs need to ensure there is effective collaboration across providers, partners and places. ICBs also need effective integrated or joint commissioning arrangements with their local authorities, so that together they take a holistic and comprehensive view of their local population’s needs for both health and social care services out of hospital, and to achieve the goal of integrated services
- information: a consistent approach to information and data management and reporting across system partners, including primary care system partners, with timely updating and flow of information against strategic objectives throughout the system. This could be supported by an intelligence function, a system-wide, multi-disciplinary team of intelligence professionals from across the ICS that co-ordinates a range of analytical skills to support the needs of the system (see Building an ICS Intelligence Function)
Strategy and planning – questions for ICB boards
- What are the current demographics, health needs and outcomes of the population across the ICS geography and how are they likely to evolve over time?
- Is there a good understanding of how inequalities manifest in the system?
- How are services currently configured across the system and how well do they meet population health needs? Are there gaps?
- On a cost-benefit basis, where are the opportunities for improvement likely to lie across the system? Is there evidence to support this and what are the associated challenges and changes necessary to deliver them?
- What are the delivery challenges of and opportunities for providers in the system?
- Does the population have appropriate access to services (including primary care services such as general practice, community pharmacy, dental and optometry)?
- How well are services integrated (including the acute and primary care interface and integration with social care) and how could this be improved?
- Are prevention and screening programmes operating effectively and in line with national targets and ambitions?
- Is there a clear plan for how organisations in the system, for example, provider collaboratives and place-based partnerships, work together to deliver the system strategy?
- Do strategic planning and commissioning decisions need to be taken collaboratively with other ICBs for particular services?
- Is the organisation engaging with the necessary partner organisations and patient and service user groups, and getting the views it needs to consider all its communities’ healthcare needs?
- Does the organisation co-produce strategy and service design with partners?
Population health, health inequalities, prevention
Relevant indicators and measures
- Population profile: Breakdown of population by demography, deprivation and socioeconomic factors (for example, Thriving Places Index information on education and learning, mental and physical health, place and environment, work and local economy); disease frequency and multimorbidity; risk factors (for example hypertension); life expectancy and healthy life expectancy; birth and mortality rates.
- Health inequalities: Aggregation and comparison for specific patient cohorts in areas including cancer (for example diagnosis at stage 1 and 2); cardiovascular disease (for example, stroke rate of nonelective admissions, myocardial infarction); diabetes (referrals, complications, completion of diabetes prevention programme); people with a learning disability and autistic people (annual health checks and physical health checks).
- Screening and diagnostics: Earlier diagnosis and coverage statistics (for example, bowel, breast and cervical cancer; cancers diagnosed at stage 1 and 2); dementia diagnosis rate.
- Vaccination: Progress to increase vaccination uptake for children and young people towards WHO recommended levels; over 65 seasonal flu vaccination rates; children receiving reinforcing dose DTaP/IPV and 2 doses MMR; Human papillomavirus (HPV) vaccine coverage.
Strategic overview
Relevant indicators and measures
- High-level view on services and providers: Spending and service use trends; waiting times and forecasting by type of care, sector, provider (and provider share); potential and emerging continuity of service risks; modelling on potential population changes (for example housing construction) which may impact demand; analysis of new and potential market entrants. Beneficial to compare with national, regional and other ICB trends.
Overview of current providers (acute and primary)
Relevant indicators and measures
- Provider strengths and weaknesses in capability; access and delivery in acute, community, mental health, ambulance and primary care including performance against oversight framework metrics; contract outcomes and in addressing third party concerns.
Delivering national priorities and targets
Relevant indicators and measures
- For example, those set out in planning guidance; oversight framework metrics; greener NHS (see Green Plan Guidance Annex B)
Social value and economic development
Relevant indicators and measures
- Compliance with 10% social value weighting across contracts; gross value added to economy arising from jobs in health and care; gross value added to economy arising from improved health of population.
B. Leadership
ICBs collect and disseminate the information the system and its organisations need to plan and deliver effective services for their population. The ICB has a pivotal role in establishing a coherent clinical strategy for the system, and in ensuring that resources are allocated to reflect the needs of its population.
Unlike the other domains, the information the board needs on leadership is likely to be based on the views of other organisations and their behaviour, for example ensuring there is effective collaboration among its system partners. Good leadership involves several approaches including influencing, building shared accountability, and assessing the capabilities, strengths and development needs of organisations across the system.
In addition, as part of its assurance, ICB boards need to ensure there are clear and explicit governance arrangements and effective decision-making structures between partner organisations for whole-system delivery and performance to deliver the integrated care strategy, the Joint Forward Plan (including ICB commissioning), system financial position and capital plan effectively.
ICB boards need to work effectively with stakeholders and ensure active involvement of all parties across their organisation and the wider ICS, including acute, mental health, community and ambulance trusts, primary care providers (general practice, community pharmacy, optometry and dental), independent and third sector providers of health and social care services and local authorities, and patients and the public. In some circumstances, ICBs may need to come together to make strategic planning and commissioning decisions for services that are delivered over a wider geography than an individual ICB. ICBs need to ensure:
- mutual accountability: the board invites feedback and role models a curious culture to understand where care can be improved, which sets the tone for engaging with partner organisations
- collaboration: the board creates and role models a culture and environment that engenders collaboration and peer support across organisations
- openness and accessibility: ensure board members (executive and non-executive) meet regularly with colleagues across the system, are problem-sensing and feed information and intelligence to and from the board
- transparency: delivery requirements and performance of each party in the ICS must be clear and contracts for services must be awarded against objective criteria (as required by the Provider Selection Regime)
- market management: engaging with providers, understanding their strengths and weaknesses and the collaborative dynamics across the different sectors in the system to ensure effective arrangement of care (see below)
- delivery: of functions NHS England has delegated to them and providing assurance to NHS England regarding their discharge
Leadership – questions for ICB boards
- What do stakeholders think of the ICB’s leadership?
- Is there a system-wide culture of collaboration and transparency?
- Is the ICB tackling challenges with a coherent clinical strategy which allocates resources effectively and according to need?
- Is the ICB collaborating with other ICBs to ensure strategic commissioning decisions are made at the right level and have the necessary resources?
- Is there a healthy culture across the system to enable honest and open dialogue and where colleagues feel able to ask the difficult questions?
- Are plans and common goals agreed?
- Are responsibilities and accountabilities clear within the system?
- Are there effective mechanisms for sharing risk?
- Are clear governance and effective decision-making arrangements in place?
- Are there any disputes between organisations in the system and if so, are these effectively resolved?
- Are future leaders actively developed within the system and is succession planning in place?
Leadership
Relevant indicators and measures
- 360-degree feedback from stakeholders; fit and proper persons test data; third party reviews and audits relating to leadership and culture; talent development and succession planning (effective senior recruitment including roles vacant and filled by target date; interim senior leadership position;, number of ‘hard to fill’ – longer than 6 months – posts); spend on external recruitment agencies for senior roles.
Local integration
Relevant indicators and measures
- Progress made to create integrated neighbourhood teams to support the integration of primary care and community services, and approaches to support proactive care and prevention.
Mutual accountability
Relevant indicators and measures
- Risk: Evidence of effective risk sharing and governance mechanisms within the system.
C. Arranging for the provision of healthcare services (strategic commissioning)
ICBs need to arrange services to reflect local need and commission accordingly, using public and patient input to shape service design. Alongside understanding current population needs, they should also take a longer-term view, looking at what is driving healthcare need and identifying strategies and services which can help to tackle long-term conditions and reduce avoidable ill health. ICBs need to:
- understand population needs, inequalities and views on how services should be provided. This should include considering how needs are likely to evolve over time, how patients want to access services to address them and what this means for the system’s plans
- focus on the strategy’s priorities – on the basis that ICBs can’t do everything. For example, optimising use of resources, focusing on life-expectancy or programmes to minimise severe acuity of demand
- identify services to meet these needs, any gaps (both now and in the future) and strategies to mitigate them within resources available
- select and contract providers for these services, following appropriate processes to procure services and agree and manage contracts
- adapt and be open to adjusting commissioning strategies based on new data, changing needs or emerging challenges. This can also include partnerships and alliances across primary and secondary providers in the system, or co-commissioning with other ICBs at the appropriate scale
In addition, ICBs need to be mindful of patients’ legal right to choice as well as the potential benefits of increasing choice of providers within the system. ICBs need to identify gaps and opportunities for improvement in local service delivery to encourage market entrants or consider the need for service reconfigurations where necessary.
Arranging for the provision of healthcare services (strategic commissioning) – questions for ICB boards
- Does the ICB use trend data on local population health needs and resource allocation tools (for example to identify gaps in services) to plan effectively for the allocation of resources and care improvement?
- What additional information and other resources are available to support care improvements, service transformation and improvements in efficiency?
- Is investment being used to shape the provision of care services, so they meet current and future demand, and are new services required?
- Does the ICB understand the economics of service provision and hold meaningful discussions with providers to get value for money?
- Are commissioned services addressing inequalities of access and outcomes as per the standard contract?
- Are existing services commissioned in line with new or existing national standards and targets? Are they safe? How do they compare to peers?
- Do services meet terms set out in their contracts, in particular for access and quality?
- Has the ICB established effective partnership and delegation arrangements (for example, place-based partnerships, collaboratives) to design and deliver the models of care required to meet the needs of the local population in line with agreed plans?
- Has the ICB considered how organisations collaborate to deliver services or functions where the required scale or capability does not currently exist within the system?
- Are new services required to meet changes in demand? Or should the focus of the model of care shift to ensure the system can deliver high quality healthcare in the future?
- Is choice being offered to patients and service users?
- Is the organisation following appropriate processes and complying with the ICB’s legal duties when changing services (including the Provider Selection Regime)?
- Are contracts designed effectively with transparent terms and conditions to hold providers to account (and if necessary to terminate the contract) and are there plans to ensure longer term continuity of service provision, for example as contracts expire?
- What do patients think about commissioned services? Does the ICB listen to and work with its communities, clinicians and patients to design services and improve access? Do providers seek regular feedback from patients and act on it?
Finance – identifying resources available
Relevant indicators and measures
- Actual year-to-date and forecast year-end performance (for example, overall outturn, cashflow, capital, variance to allocation, forecast variance %); net expenditure by service and major programme area; system capital allocation (capital allocation, variance to allocation, forecast variance %); medium and long-term financial planning and resource allocation based on identified service and population needs.
Capital
Relevant indicators and measures
- A summary of progress against the ICB’s capital programme, including the overall capital budget and sub-allocations; areas of risk that require capital investment; 5 years’ capital requirements and likely gap to allocation.
Demand and capacity modelling
Relevant indicators and measures
- System wide demand and capacity modelling for population based on current service model (for example demand trends into general practice).
Benchmarking
Relevant indicators and measures
- Comparative spend per head by sector (for example, primary, secondary, community care) considering population and comparison with national and regional trends; commissioning costs; drug spend and proportion on generic drugs; day case rates.
Quality, safety and service design
Relevant indicators and measures
- Variation: Identifying and reducing unwarranted variations in quality of care; benchmarking services with peers and statistical neighbours (in addition to what’s set out in section A on strategy and planning).
- Service change and reconfiguration: Outputs from evaluations of service change and reconfiguration; outcomes from public engagement and consultations; Equality and Health Inequalities Impact Assessments for proposals; number and status of challenges to service reconfiguration proposals or decisions.
- Collaborative working: Joint working between health and social care (such as joint appointments); local area agreements. Affordability and care pathway management: A&E attendances per total population benchmarked; reductions in emergency bed days; outpatient to follow-up ratios; referral rates for specialties; agency spending.
- Area specific performance against contract: This covers a wide range of areas for example, diagnostics (such as creation and use of new diagnostic capacity); learning disabilities and autism (such as autism assessment waiting times); mental health (number of adults and older adults completing NHS Talking Therapies, number of inappropriate out of area placements); community services (such as urgent community response services targets on 2 hour referral); maternity, neonatal and women’s health (such as fill rates against funded establishment, preterm births under 37 weeks); abortion services (for example, wait times for surgical and medical procedures); UEC (such as general and acute bed occupancy; mental health A&E waits); Continuing Healthcare (such as incomplete referrals exceeding 28 days).
Patient choice
Relevant indicators and measures
- Data indicating that meaningful choice is being offered at first point of referral and other relevant parts of the pathway; patient experience measures – experience of choice at point of referral.
Procurement
Relevant indicators and measures
- Assurance that appropriate procurement processes are being used which are compliant with the requirements of the Provider Selection Regime.
Audits, independent reviews and CQC
Relevant indicators and measures
- National surveys and inquiries; CQC rating for health providers including general practice; system outliers identified through national clinical audits; Coroner Regulation 28 notices; Parliamentary & Health Service Ombudsman complaints and reports; National Audit for Care at the End of Life.
D. Assuring performance, quality and delivery
ICBs need to ensure that providers of care in the system they are commissioning services from are delivering against their contracted standards, meeting patient needs and are operating within the overall financial envelope for the system.
Understanding performance and patient satisfaction is important to inform future development, commissioning decisions and potential service redesign. ICBs should use performance, quality and delivery information to:
- review the delivery of NHS priorities both short-term (access, targets) and longer-term (survival rates, outcomes)
- benchmark data of organisations within the system and compared to peer ICBs, alongside regional and national trends, taking mitigating actions as necessary
- identify and agree actions where data and intelligence suggest an emerging issue that requires raising with providers and / or NHS England
- identify how to change services, taking account of patient views
- review value for money and best use of resources, looking at both for the whole system and the ICB
- encourage an open culture of reporting, ensuring challenges are openly shared and solved together
Information for monitoring performance and assurance should provide an accurate and balanced picture of current and recent performance, including financial, clinical, regulatory and patient perspectives. This should be appropriately standardised to take account of known factors that affect outcomes, such as the age and deprivation profile of patients, and enable comparisons with the performance of similar organisations and health economies.
GREAY BOX Assuring performance, quality and delivery – questions for ICB boards
- Is data collected comprehensive, relevant and as up to date as possible?
- Are providers meeting national standards and quality and safety expectations? If not, do you know what the factors driving this are?
- How does delivery of services in particular places compare with that at peer places in other systems? If poorer, do you understand why?
- Are you assured providers are meeting local expectations and following best practice?
- Are contracts being used effectively to oversee and secure delivery? Are the activity levels of contracted providers in line with expectations? Is demand following expectations?
- Are services being delivered efficiently and effectively? Is there any continuity of service risks in providers?
- Is the board aware of serious concerns relating to patients or staff that have been raised within the ICB and system partners via complaints, FOI requests and other channels, and are they assured they are being dealt with?
- Is the ICB correctly discharging the functions that NHS England has delegated to them and receiving the appropriate assurance? Does the board reflect regularly on the delivery of its delegated functions, preventing risks and issues from arising and to ensure high quality commissioning?
- Are the services having the overall desired effect such as reducing inequalities, improving public health and moving towards delivering national targets and standards?
- Do providers seek regular feedback from patients and act on it?
- Does the ICB use quality and performance intelligence to enable systemwide improvements, including transforming care pathways and reducing unwarranted variation?
- What is the ICB’s financial position? What is the financial position of the delegated functions?
- How do providers perform against the productivity metrics and their efficiency plans?
- Does the ICB have robust financial controls in place to ensure expenditure will not exceed the running cost allowance?
- Does the system have agreed and effective plans for emergency planning and response?
Performance
Relevant indicators and measures
- Waiting lists: 18-week referral to treatment waiting times and number of patients waiting over 52/65/78/104 weeks by provider and clinical area.
- Attendances: Standardised activity rates for admissions and outpatient; activity vs pre-pandemic levels; virtual outpatient and emergency attendances; day case and theatre utilisations.
- Elective cancellations: Number of last-minute elective operations cancelled for non-clinical reasons; number of patients not treated within 28 days of last minute elective cancellation.
- Primary care: Appointments and activity by area; dentistry (such as dental activity units and children/adults seen in time period); GP (such as GP indicators and total QOF points by practice); community pharmacy (such as number active locally, prescription statistics, Electronic Prescription Service use); General Ophthalmology Services (such as number of tests and devices supplied); optometry; friends and family test information (overlaps with access, quality and safety, patient experience).
- Area specific performance: This will include metrics that are specific to a certain area or pathway for example cancer (28-day Faster Diagnosis Standard, 5 year cancer survival rate; cancer 62 day standard); community care (stranded inpatients with no criteria to reside, continuing healthcare referrals completed within 28 days); diagnostics (patients receiving a diagnostic test within 6 weeks); mental health (NHS Talking Therapies and perinatal access, complex care cases including psychological therapies); UEC (ambulance handover times; 12-hour trolley waits; A&E 4-hour performance).
Quality and safety
Relevant indicators and measures
- Patient safety incident reporting rates and analysis; Patient Reported Outcome Measures (PROMS); Freedom to Speak up (FTSU); Patient Advice and Liaison Service (PALS); complaints data (including numbers, status and themes); admissions caused by medication errors; healthcare associated infections (HCAI); readmission rates; standardised mortality rates; neonatal deaths and stillbirths per 1,000 total live births; hospital admissions due to fracture and violence (including sexual violence); mixed-sex accommodation breaches; breaches of waiting time targets and progress towards 18-week target; litigation and claims; progress against clinical governance plan; NHS staff survey culture sub-score.
- Patient experience: In addition to relevant information on quality and safety, experience and satisfaction measures and surveys; patient and public voices and groups (such as focus groups, citizens’ panels); breakdown of patient feedback by pathway of care, provider or commissioner.
Split out activity and financial statement
Relevant indicators and measures
- Performance against system specific activity targets; actual activity and expenditure and variance from contract for key services and providers; benchmarking for primary care, community care and the voluntary sector.
Access
Relevant indicators and measures
- Number of appointments, UDAs delivered; number of Pharmacy First contacts; total GP hours per patient by practice; patients accessing GP appointments within 2 weeks; percentage of patients with urgent healthcare need assessed same or next day; performance against targets in access, continuity, experience of access and patient activation measures (in ONS survey from autumn 2024); self-referral pathways (progress in expanding self-referral pathways); progress to improve abortion access (wait times, patient travel out of ICB or region and growth in surgical capacity); progress expanding pharmacy oral contraception and blood pressure services.
- For acute, community and mental health providers: total open beds; reduction in outpatient follow-up (OPFU); waiting time breaches; day case rates; DNA rates.
Providers’ targets and standards
Relevant indicators and measures
- Breaches of targets should be highlighted by the provider unit on a quarterly basis; summary of issues raised in local providers’ declaration of compliance with the core standards for better health.NHS111Percentage of in-hours calls to 111; number of call handlers (FTE); availability of urgent mental health support.
Providers’ financial management
Relevant indicators and measures
- Actual year-to-date and forecast outturn income and expenditure performance against profiled plan; actual year-to-date and forecast outturn and performance against profiled planned cash (EFL) target; year-to-date and forecast outturn performance against profiled planned capital resource limit; year-to-date performance against turnaround plan (where applicable); actual year-to-date and forecast outturn against profiled planned balance sheet; summary of data errors flagged by NHS England EFM data team highlighting potential inaccuracies.
Efficiency and productivity
Relevant indicators and measures
- Headline productivity (for example, cost per WAU, implied productivity growth cost weighted activity growth); operational and clinical productivity (for example, average length of stay, bed occupancy classed as clinically ready for discharge); workforce productivity (for example, implied workforce productivity growth, elective admissions per clinical WTE); A&E attendances (Type 1 & 2) per emergency medicine consultant (for example medical staff, consultant and nursing staff cost per WAU); workforce drivers (for example temporary staff spend as a percentage of total spend); non-pay efficiency (for example top 10 medicines – savings delivered).
Providers critical facilities maintenance and failure risk
Relevant indicators and measures
- Estimates of the potential severity and cost of infrastructure failure, and the impact on clinical services, staff morale and productivity; triangulate with quality metrics such as PLACE, premises assurance model and safety culture measures, and track investment.
E. Learning and transformation
This domain considers how ICBs support learning and transformation within systems, primarily by understanding the system workforce, digital and data, infrastructure and learning (encompassing both continuous improvement and research).
ICBs lead and enable system wide transformation, including:
- promoting and co-ordinating development of technology, data and digital at system level and sharing best practice across and collaborating with partner organisations. Data and insights should be accessible and clinicians, patients and stakeholders should be involved in their interpretation, to ensure insights align with practical experience and the needs of the community
- ensuring board visibility of NHS policies and national (and international) good practice and technological innovation that could and should be applied within the system
- supporting a culture of continuous improvement and innovation across the system, promoting evidence-based decision making and ensuring staff have the necessary skills and tools to do this effectively
- understanding the system workforce, considering any gaps (including in VCSE organisations), best practice and future requirements in line with the NHS Long Term Workforce Plan
ICBs should stay abreast of latest developments and priorities emerging from national innovation programmes, such as the Innovation Ecosystem Programme.
Learning and transformation – questions for ICB boards
- Is the system making progress to implement national and local workforce, education and training plans?
- How are partner organisations managing the wider system workforce, and are there any issues which should be solved at system rather than organisational level?
- Does the ICB have a robust data governance framework that defines how data is collected, managed and used? Are regular audits and reviews carried out to ensure that data use is compliant, ethical and aligned with organisational objectives?
- Are risks arising from digital transformation well understood, and are effective mitigation strategies, including those to address digital exclusion, in place?
- Is the system maximising potential benefits of research and innovation including new digital technologies?
- Does the board have a view of the research activity across its settings and specialties and the equity of access to research for its populations?
- Is the board assured their organisation and wider system is maintaining robust cybersecurity monitoring and plans?
- Are data and technology being used to drive continuous improvement and reduce health inequalities?
- Are there mechanisms to gather feedback and refine data collection processes and decision-making frameworks?
- Is the same data consistently shared across the whole system? Are stakeholders involved in its interpretation?
- How is the system (and, if applicable, the ICB) progressing with implementing infrastructure projects (for example new EPR system or major estates upgrade)?
- Is there a common approach to procurement across the ICB and its partner trusts, to maximise value for money and deliver sustainability goals?
- Are there effective mechanisms to support transformation and improvement?
- Has the system put in place plans and processes to strengthen their leadership, management and delivery of high-quality transformation and improvement support to providers?
- Does the ICB have an approach to supporting and enabling continuous improvement across all sectors? Is clinical engagement a part of this?
Workforce (system)
Relevant indicators and measures
- NHS Long Term Workforce Plan and People Promise: Progress made to implement the NHS Long Term Workforce Plan and People Promise retention interventions (and impact on staff retention and attendance); monthly staff workforce breakdown by type (such as professionally qualified clinical staff, Hospital and Community Health Services doctors, nurses and health visitors) and trend analysis; weighted patients and direct patient care staff in GP practices and PCNs.
- Workforce overview: overview of system workforce (for example, total headcount; total WTE and FTE; demographics gross salary bill; bank and agency usage/spend; and turnover vacancy, recruitment, retention, attrition and leaver rates) aggregated at areas available (for example, staff group, ward site, organisation).
- Workforce development: Commissioning education and training and regional and system workforce development; clinical placements and apprenticeship pathways vs NHS Long Term Workforce Plan targets; proportion of apprenticeship levy spent
- Staff health and wellbeing: Sickness and long-term sickness absence; presenteeism factors (for example, staff attending work when unwell); average sick days per FTE; thematic analysis of sickness reason; NHS Staff Survey questions (for example, on manager and organisational support for staff wellbeing).
Digital
Relevant indicators and measures
- Digital maturity score across sectors; progress made to implement a system wide plan and national digital plans (for example integrated EPR); virtual ward capacity and usage; estimated local digital exclusion and mitigations; use of NHS App or comparable digital tools; progress against plans to implement data and digital services in support of integration; digital exclusion mitigations.
Data
Relevant indicators and measures
- Progress to establish shared care records and establish ICB intelligence functions; implementation of Community Faster Data Flows and progress on 2024/25 priorities in community data plan.
Infrastructure
Relevant indicators and measures
- Progress on joint work to maximise value for money and sustainability across estates, procurement, supply chain and commercial; and integrated estates strategy.
Learning
Relevant indicators and measures
- Education and training: short, medium and long term metrics to align with system strategy on duty to promote education and training (for example completion statistics on mandatory and statutory training including Oliver McGowan Mandatory Training on Learning Disability and Autism; numbers trained in the National patient safety syllabus).
- Research: Progress relating to duty to facilitate, promote and use research including an understanding of activity for both commercial and non-commercial research across settings and the NHS Research Secure Data Environment Network; delivery of NIHR portfolio research studies to time and target; partnerships with academia and other research organisations, including NIHR infrastructure, and the ICS Research Engagement Network.
- Innovation: Progress in facilitating the adoption and spread of product and service innovations, including by implementing new care pathways and workforce education. Transition to the Federated Data Platform and using data to innovate care delivery
Sustainability and net zero
Relevant indicators and measures
Progress against system green plan (see Green Plan guidance in Annex B for nationally suggested metrics). Locally tracked metrics could include summary of investment requirements and investments made to achieve net zero; CO2 reduction as % of direct emissions; % of GPs prescribing metered dose inhalers vs total number of inhalers.
Improvement
Relevant indicators and measures
- Evidence of a standardised improvement approach (for example NHS IMPACT), and appropriate metrics and measurement plans for selected improvement areas.
Estates
Relevant indicators and measures
- Summary of the ICB’s mandated Premises Assurance Model Self-Assessment; top estates and facilities compliance risks scored and RAG rated with mitigations by areas of service/estate; summary of clinical service impact caused by addressing non-compliance.
F. Effective governance and people
This domain considers how the ICB governs itself internally, how it supports partners to govern effectively and how it manages and support its people. As well as leading the system, the ICB board needs to manage and oversee an effective, well-led organisation with the internal policies and processes to deliver their functions successfully. Boards should ensure:
- information is triangulated, including qualitative and quantitative data, themes from complaints and FOI requests to highlight issues around patient experience and safety, and make a judgement on whether a provider and ICB are doing everything they should be, and how integrated (or fragmented) the care is
- there are healthy internal cultures and board-level awareness of issues pertaining to staff, with whistleblowing, bullying, grievances, complaints, Freedom to Speak Up (FTSU) and other issues of concern being raised directly with the board when appropriate
- as the system-leader with overall responsibility for the delivery of NHS services, there is adequate system risk management and reporting of significant issues across the ICB including those that could pose potential reputational damage
- board members have clear roles, responsibilities and accountabilities, and there are regular reviews of board performance and capability, and analysis of required skillsets and expertise as the organisation and wider healthcare landscape evolves
- decision-making and internal processes are fit for purpose and transparent, and they proactively address conflicts of interest
Workforce (ICB)
Relevant indicators and measures
- Workforce overview: overview of ICB workforce (for example, total headcount; total WTE and FTE; demographics; gross salary bill; external contractor and supplier usage and spend on staff; and turnover, vacancy, recruitment, retention, attrition and leaver rates).Workforce development: Commissioning of education and training and regional workforce development; clinical placements and apprenticeship pathways vs NHS Long Term Workforce Plan targets.
- Staff health and wellbeing: Sickness and long-term sickness absence; average sick days per FTE; thematic analysis of sickness reason; NHS Staff Survey questions (for example perceptions of manager and organisational support for staff wellbeing).Review and escalation of serious issues: Internal focus on ICB staff experience and culture including numbers and status of complaints, grievances, disciplinaries and employment tribunals; number of Freedom To Speak Up (FTSU) Guardians; FTSU reporting numbers, status, outcomes and themes.
- Staff engagement and experience: NHS Staff Survey results for staff engagement theme and sub-themes of involvement, advocacy and motivation; people promise scores and sub-scores; staff engagement and morale theme and sub-theme scores.
- Equality, diversity and inclusion: NHS Workforce Race Equality Standard (WRES) and NHS Workforce Disability Equality Standard (WDES) data and responses to returns; diversity across bands and in senior leadership team; Gender Pay Gap reporting; NHS Staff Survey results compared across aggregated groups (for example on staff experience of discrimination and perception of the organisation providing equal opportunities).
Delegated functions
Relevant indicators and measures
- Transfer of delegated functions from NHS England: Key statistics, reporting, internal audits and self-certifications where relevant relating to pharmacy, optometry and dentistry (POD), complaints (performance, quality and accessibility of the ICB complaints function), specialised commissioning.
Staff screening
Relevant indicators and measures
- NHS Employment standards: Staff hired need to have the relevant pre-recruitment checks carried out:
- identity
- criminal record
- work health assessment
- professional registration and qualifications
- right to work
- employment history and reference(s)
4. Putting the insightful ICB board into practice
The limited time available means the board must explicitly prioritise which areas it is going to examine. The board should focus its detailed examination on where there is concern about underperformance today or in the future, and on strategic questions with significant implications for the population, services and finances. To release time for this detailed examination, the board must have confidence in the broader executive accountability and delivery arrangements that ensure the ICB is successfully discharging its functions.
Some questions boards should reflect on include:
- does it get the right balance in the time it spends on operational and strategic issues, and between assurance and decision-making?
- is the board size, membership and mix of skills what the board needs or are there gaps? Does the board work well as a team, with clear responsibilities and accountabilities?
- are the board committees and sub-committees covering all the key areas and providing the level of assurance required?
- does the board have the information it needs from across the system, and if not, how does it plan to fill information gaps?
How boards should use their time
Board members have limited time to support the board’s dual role of developing the organisation’s long-term strategy and overseeing its day-to-day operations. Boards should focus on where they can add value, concentrating on the strategic challenges their organisations must address and the most materially impactful operational and governance issues.
As a rule of thumb, boards should split their time between strategic issues and the most important and immediate matters at hand, relying on executive directors and subcommittees to raise topics as necessary. Boards should delegate the dedicated oversight and scrutiny of activities to committees, relying on them to have the appropriate judgement and rigour to be effective gatekeepers of what goes to the board for information or decision.
Board reports are often written without the limited time of the reader front of mind. Also, they can lack the transparency and rigour necessary to get to the heart of the issue, the options for addressing it and any trade-offs.
Part of managing time and resource efficiently and effectively is how board committees are used. ICB boards are expected to have committees for audit, renumeration and quality, and can have additional committees depending on local preference and prioritisation, for example, for performance, finance, primary care, population health, mental health, learning disabilities and autism, and patient experience.
Board meetings
Boards and their committees will need to consider whether and when to hold part of their meetings in private. It is important to establish a set of transparent principles for deciding when to take items in private, and to do so by exception rather than by general rule. Such principles should be in accordance with the ICB’s constitution and, where applicable, the Public Bodies (Admission to Meetings) Act 1960. The main principle will relate to items that are in commercial confidence and may apply to contract issues and disputes or potential service reconfiguration.
As part of being transparent, boards should consider how information is shared with partners and the public, for example, updates from board meetings, availability of performance and quality reports, and public access to reporting dashboards.
A year in the life of the board
ICB boards should consider how they allocate their time over the course of a year, and specifically for each board meeting. Boards should plan and agree agendas which have a clear strategic purpose and ensure there is a fully integrated annual cycle of business. Appendix 1 provides an example ICB board agenda and annual board cycle. Each board will want to adapt the cycle and design its agenda plan to fit its local priorities. As the ICB board, and its partner organisations, must agree a system strategy on which to base the design and delivery of health and care services across the system, this should be regularly covered as part of the focus on strategic issues.
Board development
ICBs may wish to incorporate the consideration of skills, knowledge, experience and ideal board size alongside regular activities they undertake as part of board development and assurance. These could include partnership governance self-assessments to ensure the board is appropriately skilled and represented; reviewing the NHS Leadership Competency Framework; using discussion prompts on the role and functioning of the ICB board and other governance considerations; board development programmes; and NHS Leadership Academy training.
Boards can use 360-degree feedback to ask partners in the system to feed back on the ICB constitution, board and committees and whether the board has the right skills and experience to carry out its functions. The statutory requirement for the ICB board is to keep the skills, knowledge and experience of the unitary board as a collective under review. Individual board members should also have regular appraisals to identify areas of strength and further development. The CQC well-led framework and its reviews of leadership and governance may further inform understanding of board members’ skills, knowledge and experience.
Systems for raising concerns and whistleblowing and listening to a wide range of voices
There must be clear accountability arrangements in place to ensure the ICB discharges its duties with regard to engaging patients, its population, and clinical and care professional leaders, and its Freedom to Speak Up (FTSU) responsibilities. The board is responsible for making sure a system is in place for raising concerns and whistleblowing, and there is a robust approach for reporting and escalating to the board. ICB board members, like all ICB employees, are expected to listen out for voices that may otherwise be missed (whether staff, patient and service user, or members of the public). These sources of information may prove to be the first signs that there are significant unreported issues and identify problems with a provider or system partner that pose a risk to staff, patients and service users. Such problems – in addition to the impact on the individuals concerned – potentially pose a wider system-level risk.
Improving the analysis behind board and sub-committee reports
The NHS, with its partners, is developing analytical capability, improving the quality and timeliness of data (quantitative and qualitative), and strengthening benchmarking tools. ICB boards will be better informed and supported in their decision-making if they have high-quality data and more sophisticated data analysis. NHS England is implementing the Federated Data Platform and promotes adoption of good practice through Making Data Count, Getting It Right First Time, Model Health System, RightCare and the NHS Benchmarking Network.
Locally, systems are encouraged to establish intelligence functions, pooling analytic capability and embedding the use of population health and integrated data, with well-managed data platforms providing high quality data to the board.
Appendix 1: Indicative ICB board agenda and annual board cycles (based on one meeting every other month)
View and download a word version of an indicative ICB board agenda and annual board cycles.
Appendix 2: ICB statutory duties
The source of ICB duties
The duties of ICBs arise from legislation (for example, the NHS Act 2006, as amended by the Health and Care Act 2022), formal agreements and undertakings with other public bodies (for example, delegated commissioning agreements with NHS England) and contractual obligations (for example, as a party to an NHS Standard Contract for the delivery of healthcare services).
The Health and Care Act 2022 transferred all the statutory duties of CCGs (bar those relating to governance) to ICBs. These are numerous and stem not only from health legislation but also, for example, from criminal justice and children’s legislation. Central to the duties transferred to every ICB are those that require it to arrange for the provision of services to meet the healthcare needs of its population, to achieve financial balance, and to ensure the services it commissions are high quality, including addressing inequalities in healthcare outcomes.
In making decisions about how to fulfil its duties and exercise its powers, the ICB must have regard to statutory guidance (such as guidance that is made by a Secretary of State, in particular for health and social care, or by a public body, in particular NHS England, in accordance with the specific powers they are given in legislation to make such guidance).
Likewise in accordance with statute, the Government sets overarching priorities for the NHS, through the Secretary of State issuing the Mandate to NHS England. NHS England’s priorities and operational planning guidance sets out the objectives against which NHS England assesses the performance of the NHS and its expectations of ICBs and trusts to help to achieve those objectives. In exercising its functions in making arrangements to meet the needs of its population, the ICB must act consistently with the Mandate, together with NHS England and the Secretary of State’s concurrent duty to promote a comprehensive health service.
Flexibilities and powers introduced by the Health and Care Act 2022
In addition, the Health and Care Act 2022 introduced new flexibilities – for example, allowing NHS England and ICBs to delegate their functions to one another or certain other statutory bodies, or to enable the joint exercise of those functions – and other powers, including giving ICBs a general power to require information from trusts further underpinning the sharing of information that partnership working requires.
Provider collaboratives and place partnerships are not set out in the Act but may utilise its flexibilities to establish binding governance. Likewise, the requirement of the National Quality Board for every ICS to establish a System Quality Group, chaired by the ICB executive lead for quality, is not a statutory requirement but is enabled by ICS partners’ general requirement to work together collaboratively across health and social care.
The Act introduced the requirement on NHS England to undertake an annual assessment of every ICB and provides for it to issue guidance to ICBs about the exercise of their functions. NHS England also has powers to issue directions to ICBs about their management or use of their financial or other resources. Where NHS England considers an ICB is failing or has failed to discharge its functions (properly or at all), or if there is a significant risk that the ICB will fail to do so, NHS England may direct an ICB on the exercise of its functions. NHS England also has functions connected with monitoring, supporting and directing NHS trusts, and has enforcement powers connected with its administering of the NHS Provider Licence which applies to both NHS trusts and foundation trusts. In this context NHS England oversees ICBs and trusts.
Implications of the Act’s new duties, powers and flexibilities
The commissioning bodies that were forerunners of ICBs were expected to set out their commissioning intentions and then secure delivery through contracting with providers, within the context of national planning guidance directed at both commissioners and trusts.
While the ICB still sets out its commissioning plan (as part of the Joint Forward Plan (JFP)) and contracts with providers in the context of the national planning guidance, the Act supplements this with accountability derived from shared duties to develop – and commitments to deliver – the Integrated Care Strategy, the five-year JFP, joint capital plan and system financial balance and objectives. Therefore, the ICB board and its sub-/committees will want to consider not only the contractual performance of its providers and the organisational and financial health of the ICB itself, but also progress in delivering against these shared commitments.
ICBs and their partners will have established delivery programmes for these plans – including for subsidiary plans, such as the system workforce plan and the digital plan – which will report progress to the Integrated Care Partnership (ICP) and partner organisations as appropriate.
Likewise, the progress of the parties in better organising themselves together for delivery (the “system architecture”) – such as establishing partnerships at place level, provider collaboratives and shared teams (for example analytics) – will also be reported to the ICP.
Key statutory duties
This table sets out key statutory duties, which relate to the establishment and core functions of ICBs. It is not exhaustive and is intended to capture the statutory duties that are most relevant to the functional areas in the insightful ICB board.
View and download a word version of key statutory duties table.

