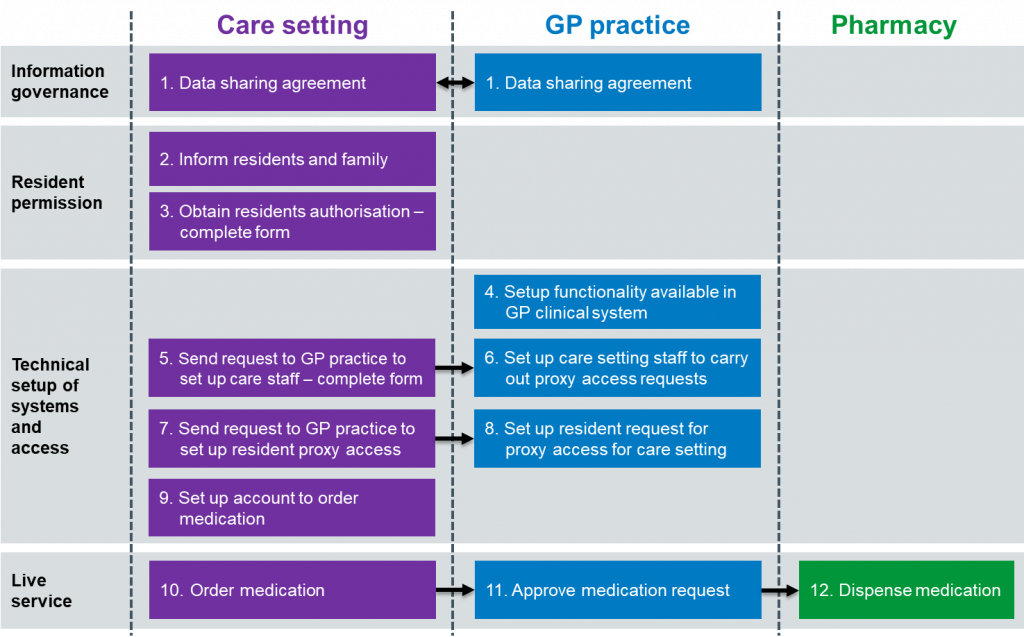
Step by step process
The actions which need to be completed by care homes, GP practices and community pharmacies are described below.
Step 1. GP practice and care home data sharing agreement
The Care home lead and the GP practice lead must create a high-level data sharing agreement that sets out:
- what information is going to be shared between care home, GP practice, and pharmacy where relevant, and why.
- The rules around security, accuracy, use, and deletion of data
The NHS Digital website gives more information, including a short video, about data sharing agreements. This data sharing agreement template for care homes/practice can be downloaded and amended here.
All care home staff will also need to sign an agreement based on these principles (see Step 5 below).
Step 2. Care home tells residents about changes in how repeat medication will be ordered
The Care home lead must tell all residents about the new way of ordering medication and explain that this means care home staff will use proxy access to do this.
A letter must be given to all residents or sent to their representatives, explaining how this will work, and what the benefits and risks are. An information leaflet and an example of a letter to residents are available to download.
All residents should be offered a one-to-one discussion with the care home manager/lead before agreeing to the new way of ordering their medication.
Step 3. Care home gets each resident’s permission
The Care home lead must get signed permission from each resident/patient (or their representative) to show that they understand the new ordering process and are willing to give care home staff proxy access to their GP record. This template consent form can be downloaded and adapted.
Each resident or their representative will need to sign a personalised form and be given a copy of it. A single form listing all residents in a home is not acceptable. This step could take up to 2–3 weeks to complete.
The GP makes the final decision. If they have any concerns, they will not grant proxy access and will discuss this with the resident/patient.
Step 4. GP practice sets up proxy access in their clinical system (if necessary)
Most GP practices already have GP online services set up and people with proxy access using them. Setting up care home staff has one difference.
Step 5. Care home sends request to GP practice to set up staff
Before proxy access can be given, each member of care home staff who will be responsible for ordering medication must be set up on the GP system.
The care home manager/lead and each member of staff must complete to request proxy access rights. An example form can be downloaded here. This form can also be used to remove access from a member of staff.
The Care home lead must send completed forms to the GP practice, keeping a copy for the care home’s records.
Step 6. GP practice sets up access for care home staff
The GP practice lead should:
- create separate folders on a secure shared drive for each care home
- save all forms from the care home (both for requesting, and removing, access)
- set up a proxy access login for each member of care home staff
Step 7. Care home sends residents’ consent forms to the GP practice
The Care home lead sends signed copies of the residents’ authorisation forms to the GP practice lead or their generic inbox as agreed locally.
Step 8. GP practice sets up proxy access for each resident
The GP practice lead should:
- scan/file the authorisation form into the resident’s patient record
- create a proxy access account, for repeat medication ordering only, for approved members of care home staff. Then send them their set up and log-in details to a secure email account.
Step 9. Care home staff verify their own accounts
Once the GP practice has given proxy access, each care home staff member must complete several steps before starting to order medication for a resident.
Each GP system does this slightly differently and so a set of user guides has been produced to help you get started. You can find links to these in the next section, Step 10.
Step 10. Order medication online
As each GP system works in a slightly different way, a set of user guides is available to explain what to do to start ordering.
Step 11. GP practice approves or rejects medication request
When medication is ordered by the care home (the monthly date must be agreed with the practice and the community pharmacy informed under the medication cycle planner already in place) a member of the GP practice team will process these online requests in the same way as all other repeat prescription requests.
Once approved by a GP, the practice will follow the agreed process for dispensing and delivering medication.
TPP and EMIS have produced standard operating procedures (SOP) guides for GP practices:
Step 12. Dispense medication
The authorised prescription will be:
- sent directly, electronically, to the community pharmacy using the electronic prescription system (EPS), or
- collected from the GP practice by the community pharmacy or care home.
Once dispensed the medicine will be ready for collection from the pharmacy or may be delivered to the care home by local agreement.
View the next sections in this guide: