Cancer experience of care
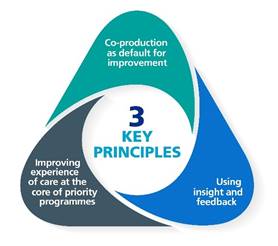 The experience that a person has of their care, treatment and support is one of the three parts of high-quality care, alongside clinical effectiveness and safety. In line with the national Experience of Care team, we follow the three key principles of delivering the best possible experience of care in systems.
The experience that a person has of their care, treatment and support is one of the three parts of high-quality care, alongside clinical effectiveness and safety. In line with the national Experience of Care team, we follow the three key principles of delivering the best possible experience of care in systems.
We work to improve experience of care for all that are affected by cancer, and their family and carers, by using feedback, sharing examples of good practice and working together to support people, networks and communities to make improvements.
We ask health care providers and systems to:
- make sure their plans and work programmes aim to improve experience of cancer care, tackle health inequalities, improve staff experience and support carers
- support and encourage people, from all backgrounds, to provide feedback on their cancer care and treatment
- work with people with relevant lived experience to make improvements together based on what matters most to patients, and their families and carers
The National Cancer Patient Experience Survey
The National Cancer Patient Experience Survey (NCPES) is sent out every year to adults 16 years and above to ask people about their recent experiences of NHS cancer care and treatment. The survey covers all NHS trusts that provide adult cancer services in England, and has been designed to help us understand the experience of cancer care; to assist NHS organisations to make improvements to cancer care; and to provide information to charities and other groups that support cancer patients.
The results from previous surveys are available on the NCPES website. You can find more information about the survey and how to get support completing the survey on the website, along with other ways to provide feedback on cancer care.
The Under 16 Cancer Patient Experience Survey
Improving cancer care for children and young people is a key commitment in the NHS Long Term Plan. The Under 16 Cancer Patient Experience Survey is a national survey that gathers feedback from children and young people and their parents/carers on their experience of cancer care and treatment. This helps us to understand what is good about children and young people’s cancer care and identify how we can make improvements.
The results are published on the Under 16 Cancer Patient Experience Survey website, capturing the experiences of care for children and young people under 16 and their parents/carers from Principal Treatment Centres. You can find more information about the survey and how to get support completing the survey on the website, along with other ways to provide feedback on cancer care.
The Cancer Experience of Care Award
Since 2019, NHS England has worked in collaboration with Macmillan and the Patient Experience Network (PEN) to deliver the National Cancer Patient Experience Survey (CPES) Award. In 2022, the award was renamed to the ‘Cancer Experience of Care Award’, recognising and promoting the use of CPES data while expanding the criteria to include other sources of insight and feedback.
The award is presented at the annual Patient Experience Network National Awards to a team which used insight and feedback to grow improvements in experiences of cancer care. There is an emphasis on patient involvement and coproduction, and the sharing of good practice across the cancer sector.
The Award winner and finalists can be found on the Patient Experience Network website, along with the presentations delivered at the Award ceremony.
The Cancer Experience of Care Improvement Collaboratives
The Cancer Experience of Care Improvement Collaborative brings together groups of cancer healthcare professionals and people with lived experience from different organisations to improve services. The aim of the Improvement Collaborative is for each project team to use insight and feedback (like trust level Cancer Patient Experience Survey results) to improve the experience of care for cancer patients and their friends and family who may provide unpaid care and support. Project teams are able to make improvements based on what matters to people who use cancer services that align with local, regional, and national priorities.
Principles of the collaborative:
· Working in partnership with people with lived experience to co-produce and co-design improvement projects using a structured framework – quality, service improvement and redesign (QSIR) tools
· Using insight and feedback (e.g. surveys, complaints, feedback, compliments) to improve experience
· Sharing and learning together across England
Hear from people with lived experience about how they have been involved in the collaborative and influenced change together:
What people have said about being involved:
“I’ve been a GP for 35 years and I’ve never before seen primary and secondary care coming together in this way…this is meaningful, because it is based on what the patients are telling us they need” – project team member, 2021
“The rewards of being a part of a project team, which is focused around improving patient experience are immense”. – project lived experience partner, 2021
“Great to be part of a supportive and organised collaborative. Learning is encouraged and any progress, however small is recognised and encouraged” - project Team member, 2022
Hear from people who took part in the 2021-22 collaborative about their experiences and learnings:
Improving experience of care along cancer diagnostic pathways
In 2020, staff, patients and carers co-produced a set of 32 quality markers. The quality markers show what a good experience of care looks like along cancer diagnostic pathways based on what matters most to them. Cancer Alliances, with providers and people who use their services, have been asked to assess their own services against the quality markers to improve experience of care.
For more information about the quality markers and wider work in the Faster Diagnosis team please visit our Faster Diagnosis pages.
