Appendix 1: How we delivered against the government’s mandate to the NHS
The government’s 2023 mandate to NHS England sets out the organisation’s strategic direction and describes the healthcare priorities and the contribution NHS England is expected to make within its allocated budget and helps to ensure that the NHS is accountable to both Parliament and the public.
The government’s 2023 mandate sets out three priorities: cut NHS waiting lists and recover performance; support the workforce through training, retention and modernising the way staff work; and deliver recovery using data and technology. The mandate also sets an additional objective to continue work to deliver the NHS Long Term Plan, to transform services and improve outcomes. This assessment of delivery against the 2023 mandate captures our broad assurance of performance using data between April 2023 to March 2024. This follows assessments by policy teams at NHS England and the DHSC.
Priority 1: Cut NHS waiting lists and recover performance
This objective’s purpose is to ensure that the NHS can recover services for patients. We know that current waiting times are unacceptable, and that performance is not good enough. Our ambition is to go further and pull out all the stops to improve services for our patients.
Despite the challenges, the NHS has made progress to reduce the number of people waiting the longest time for elective care, assisted by NHS activity levels rising to 110.5% of pre-pandemic levels by March 2024. The number of patients waiting more than 52 weeks for treatment reduced to around 310,000 in March 2024, from over 370,000 in April 2023 and the proportion waiting over six weeks for diagnostic tests decreased from 27.6% in April 2023 to 21.8% in March 2024. By the end of March 2024 160 Community Diagnostic Centres were operational and had cumulatively delivered 8m tests since July 2021.
Cancer survival is at an all-time high, with one-year survival rates at 74.6% and five-year survival rates at over 55.7%. The Faster Diagnosis Standard was exceeded by 2.3% in March 2024, and cancer patients rated their overall experience as 8.89 out of 10 in the 2023 Cancer Patient Experience Survey.
There has been high growth in demand for hospital services, including a 6.7% increase in emergency admissions, 11% increase in same day admissions and 4.4% increase for overnight admissions compared to 2022/23. Despite these pressures, 4-hour A&E performance was 74.3% in March 2024. Whilst this did not meet the ambition of 76%, it was an improvement against 71.5% in March 2023. The 2023/24 average ambulance category 2 response time was 36 minutes and 22 seconds. Whilst this did not meet the ambition of an average of 30 minutes, it was over 13 minutes faster than 2022/23. Discharge delays were reduced due to a combination of increased intermediate care capacity, the publication of the intermediate care framework and community rehabilitation and reablement model, as well as improved discharge processes. As a result, an average of 500 fewer patients per day spent the night in hospital. Capacity has increased – the permanent inpatient bed base expanded by over 5,000 by January 2024 and virtual wards were scaled up, with 11,856 beds available by March 2024.
NHS England introduced a range of other initiatives to achieve improvements in elective and non-elective care, including 400,000 long-waiting patients being offered the opportunity to request a change of provider, provision of better information on patient choice and waiting times, and ensuring Crisis Mental Health services are now available via NHS 111. Despite demand increasing, over 50% of GP appointments were seen on the same or next day and over 83.3% of appointments were provided within two weeks of contact. The launch of the Pharmacy First initiative has made it easier for patients to access treatment for common conditions and has expanded access to blood pressure and contraception services.
Priority 2: Support the workforce through training, retention and modernising
Additional funding for the Long Term Workforce Plan begins in 2025/26, but in advance of that, progress can already be seen in an improvement in retention and staff engagement rates through 2023/24.
NHS England has begun work with UCAS to expand clinical training places and has broadened the scope and reach of NHS recruitment campaigns. Work has been targeted at modernising curricula and career pathways and improving learner experience. This has included research to establish which factors contribute to effective practice-based learning, the launch of the Allied Health Profession Preceptorship document and the Safer Learning Environment Charter for maternity services.
Work to expand and reform medical training is under way. The initial years of medical school expansion secured an increase in places for 2023/24 ahead of trajectory, and a pilot medical doctor degree apprenticeship was developed and will start in Autumn 2024. NHS England continues to support the Enhancing Doctors’ Working Lives programme, which was established to enhance flexibility and address concerns raised by doctors in training.
Priority 3: Deliver recovery through the use of data and technology
NHS England has continued to make progress in utilising data and technology to enhance NHS services. The aim of having Electronic Patient Records in 90% of Trusts was met in December 2023, reducing reliance on paper, and significantly improving both clinical safety and performance. The aim of registering 75% of the adult population with the NHS App was met, and the range of features available via the App has continued to grow. As of March 2024, 6 million secondary care appointments, on average, are managed via the App each month. 84% of GP practices now give patients sight of new information added to their GP health record (“prospective record access”) via the App and, since January 2024, patients in England can view their prescription details and order repeat prescriptions via the App.
NHS England has supported the procurement of a Federated Data Platform and Privacy Enhancing Technology, which went live in March 2024. An ICS system-wide dashboard went live in 40 ICSs, which combines data feeds to and from frontline providers to give real-time management of capacity and performance across acute, community, and mental health providers. 56% of NHS trusts in England are piloting at least one or more Artificial Intelligence technology products, impacting over 1 million patients across health and care pathways.
Continue work to deliver the NHS Long Term Plan to transform services and improve outcomes
NHS England has continued to prioritise the transformation of our services and improve outcomes. This includes delivering 9.5 million personalised care interventions – well beyond the target of 5 million. The number of 2-hour referrals to Urgent Community Response teams increased by 36% over 2023/24, with 84% of people on average receiving a response within 2 hours.
During the first year of the three-year delivery plan for maternity and neonatal services (running from 2023-2026), progress has been made with a record number of full-time equivalent midwives in post, at 25,071 in March 2024. Maternal Mental Health Services were established in 39 ICBs, with the rest in development and the Maternity Safety Support Programme review was completed and its recommendations implemented.
Children and Young People’s services are being transformed through initiatives such as launching the pilot of family support workers in urgent care and expanding the pilot for paediatricians working within 111.
A national investment of £121 million in 2023/24 has supported the delivery of services for people with a learning disability and autistic people. By March 2024, 78% of eligible people on a GP learning disability register received an annual health check and 75% had an accompanying health action plan. Keyworker services for autistic children and young people at risk of admission or admitted in a mental health hospital are now operational in all ICBs. NHS England continued to support implementation of the national framework for autism assessment pathways and to understand the impact of demand and capacity pressures across the all-age autism assessment pathway. Despite this, the number of people receiving a first contact appointment within 13 weeks has reduced, in part due to the demand for Autism Assessments growing significantly.
There was an increase in children and young people accessing mental health services – reaching 94% of the target set out in the NHS Long Term Plan, an increase in access to adult community mental health teams – reaching 115% of the NHS Long Term Plan target, and an increase in adults accessing talking therapies – reaching 66% of the NHS Long Term Plan target. Where targets are not being met, NHS England has clear improvement plans in place, including focusing on expanding and retaining the mental health workforce.
Progress was made in secondary prevention. Over 1.6 million referrals were made into the NHS Diabetes Prevention Programme, with those who complete the programme reducing their risk of developing type 2 diabetes by 37%. Over 25,000 referrals were made to the Type 2 Diabetes Path to Remission Programme, with around 50% of participants putting their Type 2 diabetes into remission. On healthcare inequalities, the National Healthcare Inequalities Improvement Programme has continued to develop at pace. Seven Core20PLUS Accelerator sites – one per region – have been launched, deploying improvement methodologies to test innovative approaches that address inequalities locally. Six pilot sickle cell disease A&E bypass wards have also been established in high-prevalence areas.
Appendix 2: Meeting our Public Sector Equality Duty
In May 2023, NHS England’s Board approved and published NHS England’s equality objectives and targets for 2023/24 and for 2024/25. Progress against these equality objectives and targets was reviewed during 2023/24 and in May 2024, NHS England’s Board considered a paper recommending the approval and publication of a review report for 2023/24. The Board also approved updated equality objectives and targets for 2024/25 and 2025/26.
In developing our equality objectives and targets, we are required to focus on the Equality Act 2010’s nine protected characteristics where there is evidence of a need to take strategic action to address discrimination or other matters that are unlawful under the 2010 Act, advance equality of opportunity or there is a need to foster good relations. The 2023/24 review report demonstrates how NHS England continued to meet our statutory requirements under the Equality Act 2010’s Public Sector Equality Duty (PSED) and the associated Specific Equality Duties (SEDs). Central to these statutory requirements is the duty to publish equality information annually. The report demonstrates the breadth and depth of the work undertaken by NHS England in furtherance of the PSED and the SEDs.
The full 2023/24 review report is available on NHS England’s website. It provides a range of key equality information, as of March 2024, as required by the SEDs and informed the revision of our equality objectives and targets for 2024/25 and 2025/26.
Part 1 of this report explains the ongoing changing context within which the new NHS England is now functioning and what reporting, required by the SEDs, is covered by this report.
Part 2 provides a summary assessment of our performance against our eight equality objectives and the associated targets set for 2023/24. It also explains whether or not the targets sets for 2024/25 will be amended and whether they will be rolled over to 2025/26.
Part 3 provides further information on work undertaken by NHS England during 2023/24. It also provides an update on issues identified for future consideration in the future objectives report published in May 2023. This included explaining how during 2023/24 NHS England took positive steps to address issues and questions raised by the Women and Equalities Select Committee and the Equality and Human Rights Committee in relation to Black maternal health, learning disability and autism, mental health, and low paid ethnic minority staff.
Part 4 explains that the Board was asked to approve the equality objectives and proposed targets for 2024/25 and 2025/26.
Appendix A sets out NHS England’s equality objectives and updated targets for 2024/25 and 2025/26. For ease of access, these objectives and targets are also provided here.
Appendix 3: Reducing health inequalities
NHS England has continued to work towards delivering its statutory, governance and operational support responsibilities for health inequalities throughout the period. We have achieved this by setting a clear direction, creating a culture of continuous quality improvement, and developing frameworks for accountability. Work to reduce healthcare inequalities in 2023/24 had particular focus on system efforts to narrow the gap in healthcare access, experience, and outcomes, and to strengthen accountability and capability to act on inequalities.
Our strategic approach to reducing healthcare inequalities
There is an urgent need to prevent and manage ill health, particularly in groups that experience the worst outcomes. In 2023/24, we worked with ICSs to focus on five priority areas for tackling healthcare inequalities:
Priority 1: Restore NHS services inclusively
Following the publication of the Delivery Plan for Recovering UEC Services, we achieved 65% coverage of High Intensity Use services (proportion of A&Es with access to a high intensity use scheme), aiming to improve wait times and patient experience for all. At ICS level, 37 of the 42 ICSs’ have at least partial coverage (some localities within the ICS having access).
We published a framework for NHS action on inclusion health to drive increased focus on securing good access to, and experiences of, healthcare among socially excluded groups experiencing multiple disadvantages. The framework was developed in collaboration with the Office for Health Improvement and Disparities and the UK Health Security Agency. It was also informed by the engagement of people with lived experience and Voluntary Community Faith and Social Enterprise organisations. A plan is in place to support the delivery of actions set in the framework at ICS and place level.
Priority 2: Mitigate against digital exclusion
We published Inclusive Digital Healthcare: a Framework for NHS action on digital inclusion in September 2023, setting out five domains for actions to help ensure that the spread of digital health is inclusive, and complementary to non-digital services and support. We have hosted several webinars in early 2024 to socialise the framework.
Priority 3: Ensure datasets are complete and timely
The Healthcare Inequalities Improvement Dashboard was upgraded to version 2.1 in July 2023. Developments include new hospital activity indicators with breakdowns by inequality variables to inform action on inclusive recovery of services and methodological improvements, including calculation of age standardised rates and display of confidence intervals on charts.
Priority 4: Accelerate preventative programmes that proactively engage those at greatest risk of poor health outcomes
We made significant progress in developing a new Core20PLUS5 Handbook which will brings together best evidence and practice examples to support successful delivery of Core20PLUS5 interventions for underserved groups. Reference was made to NHS England’s handbook development in the Government’s Major Conditions Strategy strategic framework published in May 2023.
We have undertaken a whole system, end-to-end clinical pathway review, to improve the quality of care for people living with Sickle Cell Disorder (SCD). This covered screening, routine management of SCD and management of crises presentation in A&E, resulting in significant new NHS England investment to improve access to urgent care, experience, and outcomes for people with Sickle Cell Disorder (PwSCD). Furthermore, funding was secured for sickle cell blood group genotyping and work to initiate this intervention to reduce adverse reaction to blood transfusions in PwSCD commenced. In addition, funding was agreed to deliver several sickle cell disease hyperacute unit pilots in high prevalence metropolitan areas. The first site in Manchester went live in February 2024.
Priority 5: Strengthen leadership and accountability
NHS England’s Statement on Information on Health Inequalities was published, in support of our duties under section 13SA of the NHS Act 2006 (as amended). The statement sets out a description of the powers available to ICBs, trusts and foundation trusts to collect, analyse and publish information on health inequalities.
We have also developed and deployed a range of interventions including a multiyear strategic partnership with the Royal Society of Medicine for a healthcare inequalities education programme; continued work with the Healthcare Financial Management Association to develop an ICB finance toolkit for health inequalities which includes a series of policy briefings and four e-learning modules; in partnership with NHS Horizons, we developed and delivered a School for Change Agents programme with a focus on tackling healthcare inequalities with 2,261 people signed up to participate; in partnership with the Health Foundation and Q Community we co-designed and delivered an Improving Equitably programme; in response to the Chief Medical Officer’s Coastal Health Report 2021.
More broadly, we continue to provide strategic direction for the system by influencing action on healthcare inequalities and collaborating with partners. For example, we contributed to the development of the DHSC policy paper Major Conditions Strategy: case for change and our strategic framework by providing evidence, through engagement with systems.
Framework for action – Core20PLUS5 approach
Core20PLUS5 remains our approach to supporting reductions in healthcare inequalities at both national and system level. This year we have successfully recruited more than 250 additional Core20PLUS Ambassadors – people working in the NHS, partner organisations and voluntary sector – to promote the reduction of health inequalities for all, particularly groups who are more likely to experience healthcare inequalities, such as communities living in deprived areas. We also recruited 44 Healthcare Financial Management Association (HFMA) health inequalities finance fellows as part of this cohort.
Our collaboration with the Institute for Healthcare Improvement has seen seven Core20PLUSAccelerator sites supported to build quality improvement capability at the same time as advancing action across the priority clinical areas and population groups represented within the Core20PLUS5 approach.
Our Core20PLUS Connectors programme has 30 Connector sites across the seven NHS regions, 543 connectors have been recruited to the end of March 2024, working with 70 delivery partner organisations from local voluntary, community, faith, and social enterprise organisations, and local Healthwatch partners to influence and engage local people on how to overcome barriers to accessing services.
Through the programme’s collaboration with partners and national clinical programme teams we have agreed a set of metrics and indicators within a health inequalities monitoring framework. In addition, a sub-set of these health inequalities indicators has been proposed for inclusion in the NHS Oversight Framework. The new indicators provide a measurement framework to monitor progress and impact of health inequalities improvement activities across the NHS.
Appendix 4: Working in partnership with people and communities
In 2023/24, we focused on reviewing how the new NHS England involves people and communities in our work.
The Board asked the People and Communities division to develop a new Participation Policy, based on learning from different approaches taken by the three legacy organisations. A review found that each organisation’s approach had its strengths:
- Health Education England’s People’s Advisory Forum fostered meaningful dialogue within its governance structure, ensuring community voices guided decision-making
- NHS England’s robust support package for Patient and Public Voice (PPV) Partners promoted inclusivity through training, support sessions, and coaching
- NHS Digital’s user-centred approach ensured that engagement is integrated into project management practices.
The revised policy will support our legal duty to involve the public (section 13Q of the NHS Act 2006 (as amended)).
In order to discharge its legal duty to involve the public, NHS England has an assurance process in place for its commissioning decisions that affect the recipients of NHS services, including their carers and representatives. National and regional reporting on public involvement provides assurance that NHS England has met its legal duty during the reporting period.
We worked with ICBs to build a network of engagement professionals which supported them to embed the 2022 statutory guidance and share effective practice. Network sessions included sharing insight across systems, evaluating impact, and using AI in engagement and insight.
Maximising the impact of NHS volunteers and the VCSE sector
In July 2023, the NHS Volunteering taskforce published its report highlighting untapped volunteering potential and a desire to increase activity. The report had recommendations for NHS England that focused on developing volunteering infrastructure, improving data capture, and reducing barriers. To meet the recommendations, we:
- Invested in the development of a recruitment portal for volunteering opportunities
- Invested £10 million in a national grant programme, in partnership with NHS Charities Together and CW+, to develop system level volunteering infrastructure
- Continued delivery of the Volunteer to Career programme, in partnership with Helpforce, supporting routes into careers, particularly clinical workforce pathways
- Moved the NHS Volunteer Responders Programme from a COVID-19 response to a flexible model, with its 42,000 volunteers available to the NHS at times of need.
- Maintained support for ambulance trusts through an extension to the National Ambulance Auxiliary service with 57,000 hours of additional capacity provided.
Chaplaincy and spiritual support
Following engagement, NHS England published new Chaplaincy Guidelines in August 2023, providing a best practice guide for those managing healthcare chaplaincy services in NHS providers, to support chaplaincy services to meet equality obligations.
Supporting Primary Care Networks to work with people and communities
We built on the previous years’ work to trial various engagement approaches through our test and learn sites. We shared learning from those sites to build capacity and confidence around using community-centred approaches, understanding health creation at a place-based level and the training needs of new community teams.
Work with young people
NHS Cadets, in partnership with St John Ambulance, recruits young people from deprived communities and under-represented groups. The Cadets develop their first aid, mental health, leadership, and communication skills with the view to considering a career in health and care. To date more than 5,000 14- to 18-year-olds have enrolled as NHS Cadets, including 1730 in 2023/24 when 80% were from deprived or under-represented groups.
The Young People’s Health Challenge is designed to inspire 7- to 14-year-olds from deprived communities and underrepresented groups to find out more about the NHS, raise health literacy, and create aspirations to work or volunteer in the NHS. It also provides opportunities for NHS organisations to include youth voices. We developed three toolkits aimed at different levels of ability offering over 60 challenges. The toolkit is now offered across the systems for use by NHS organisations and their partners.
Working in partnership with carers
Work has continued over the past year on our Commitment to Carers, including formalising and improving carer data collection and coding, which is essential to understand of the needs of carers and provide greater levels of support. The biannual System Maturity Matrix assessment continued to provide insight; and showed a positive development journey and opportunities to share learning. This gave a clear view of progress on the Commitment to Carers commitments made in the NHS Long Term Plan.
New duties provided in the Health and Care Act 2022 include involving carers. The VCSE Health and Wellbeing Alliance supported the involvement of carers in the development of ICS strategies, work on carers and virtual wards, and contingency planning for carers. The Health and Wellbeing Alliance Carers partnership is pulling together a directory of materials, case studies and best practice examples to provide “off the shelf” knowledge and learning for systems at different stages on their development journey with addressing the recognition and support needs of unpaid carers.
Our Mind the Gap projects have improved carers from deprived communities and under-represented groups access services. We funded the Junction Foundation & Carers Together Foundation and NHS North Tyneside ICB to produce a Transitions Passport to help young adult carers to access services, in recognition that 87% of young carers are not properly supported into adulthood (Carers’ Society, 2021).
Listening to what matters most to unpaid carers is strengthened by an annual conference that is hosted by different regions to highlight best practice and share learning. The conference this year was held in Bristol in our South-west region and the next conference will be in the North West.
NHS England is developing the best ways to use the NHS App to give unpaid carers proxy access (with consent) to medical records, test results and online prescriptions and helping unpaid carers manage their own mental and physical health through digital therapeutics.
The Unpaid Carers Ministerial Roundtable held in 2023 was a useful opportunity to identify areas of common interest and establish new links across government examples being; links to the new digital resource developed by the Department for Work and Pensions; aligning our regional leadership with the Department for Education pilot programmes which include young carers and the Outcomes, Care Leavers and Capital team delivering the Schools Census.
Networks and forums
Across the organisation, we run a wide range of forums, advisory groups and sounding boards, involving people from different communities and health interests. These include the NHS Youth Forum, the Older People’s Sounding Board, the LGB Sounding Board and the Adult Mental Health Advisory Network.
A key forum is the NHS Citizen Advisory Group, which brings together patient and PPV Partners from across various NHS England forums. It champions appropriate, effective, and meaningful engagement, including identifying good practice and opportunities for improvement. This year it worked with NHS England on its equality duties, the NHS Long Term Plan, the revised Participation Policy; and engagement within mental health programmes.
Learning Disability and Autism Advisory Group and Forum
The Learning Disability and Autism Advisory Group advises on changes which affect autistic people and people with a learning disability. It provides insight and feedback to our teams and works to co-produce policy guidance and service improvements. In 2023/24 the group advised on areas including the Reasonable Adjustment Digital Flag, the National Framework and Operational Guidance for autism assessment services and improving the quality of inpatient mental health care and crisis support in the community.
Through the Learning Disability and Autism Forum, we shared key national campaign information in more accessible language to widen reach, help raise awareness, explain complex messages, and help improve services. We used social media, monthly update email bulletins and a newsletter. For example, we gained valuable insight and feedback from sharing a survey around medication, the findings have been used to make improvements for people, their families, and carers.
Appendix 5: Sustainability
Scope
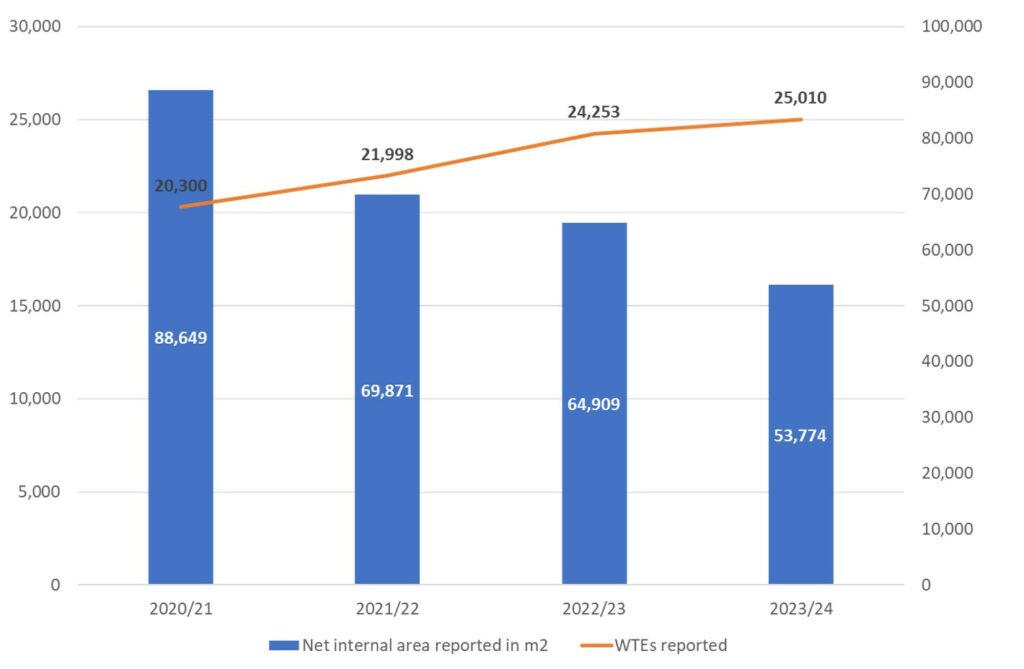
All reporting in this section covers NHS England and CSUs. Reflecting the merger of NHS England, NHS Digital and Health Education England, all historical figures have been restated to include the information from all legacy organisations.
Each trust and ICS have their own Green Plan and will report their sustainability performance separately. Sustainability across the wider NHS continues to be led by the Greener NHS.
Summary
This report summarises our progress against the Greening Government Commitments (GGCs) and the NHS ambition to be net-zero by 2040.
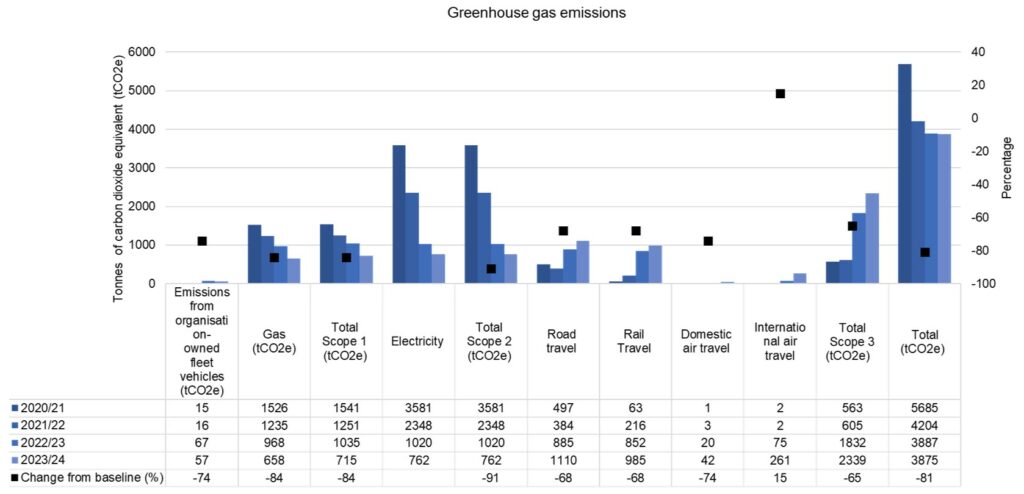
We continued to maintain a significant reduction in greenhouse gas emissions compared with the 2017/18 baseline year. We are currently 81% below baseline, against a target of 44% by 2025.
A decrease in the size of the reportable estate over the last 12 months has resulted in lower gas, electricity, and water consumption, as well as a reduction in the amount of waste generated.
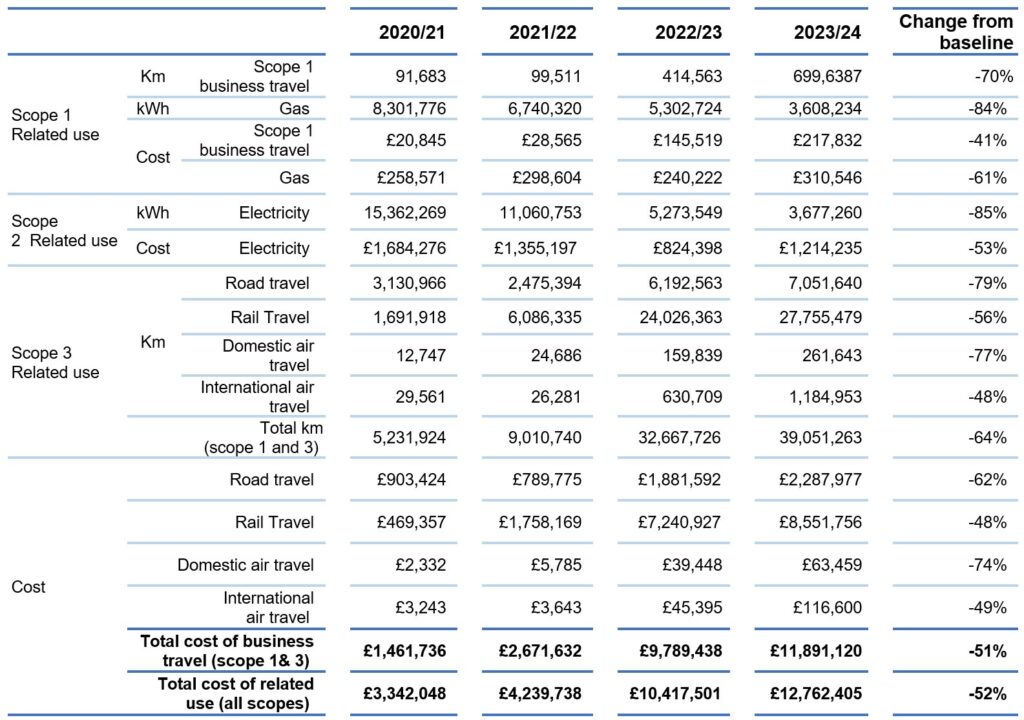
We remained below the annual targets we set for business travel emissions during the reporting period. However, as we increase the amount of face-to-face working across the organisation, the rate at which business travel is increasing will be monitored closely to assess the environmental impact.
We have also made progress with reducing paper consumption and increasing the proportion of zero-emissions fleet vehicles. Areas for improvement include the recycling rate, which is below target, and the removal of Consumer Single Use Plastics (CSUP) from our estate. The number of CSUP items increased this year as staff spent more time working on-site in our offices. We will continue working with suppliers to remove CSUP items and replace them with sustainable alternatives.
Reporting for multi-occupancy buildings
We are reporting on the proportion of the NHS PS buildings occupied by NHS England and CSUs. Approximately 45% of our estate is included in this reporting. Where we are a tenant of a government department, energy, waste, and water information will be reported in their respective annual reports and published on their websites.
Provision of data
The process of merging historical data highlighted some gaps in data provision across the legacy organisations. Wherever possible, we have used available data to make informed estimates based on averages per WTE. We estimated the proportion of the former Health Education England estate that is reportable by using the average of the proportion of the NHS England and NHS Digital reportable estate. We have highlighted where relevant if it hasn’t been possible to provide meaningful estimates.
It has also been necessary to estimate data where there have been gaps in the information provided. This includes:
- Missing energy, water, and waste information for some of the estate. Gaps have been estimated based on averages per Net Internal Area.
- Paper data was available for part of the year. We used the average amount of paper printed per WTE to estimate the total figure for the whole year for NHS England. This average was also used to estimate paper usage for CSUs when actual figures were not available.
- CSUP is estimated for the CSUs using the average per WTE for NHS England.
We continue to work with suppliers to improve the provision of data and data quality.
Mitigating climate change: working towards net zero by 2040
2021-25 GGCs headline target: Reduce the overall greenhouse gas emissions from a 2017/18 baseline and reduce direct greenhouse gas emissions from the estate and operations from a 2017/18 baseline.
2021-25 GGC sub targets: Reduce the emissions from domestic business flights by at least 30% from a 2017/18 baseline and report the distance travelled by international business flights.
Contextual information
Greenhouse gas emissions (figures have been rounded to the nearest whole number).
Related use and cost
Air travel (the flight data for Health Education England has been estimated based on average per WTE)
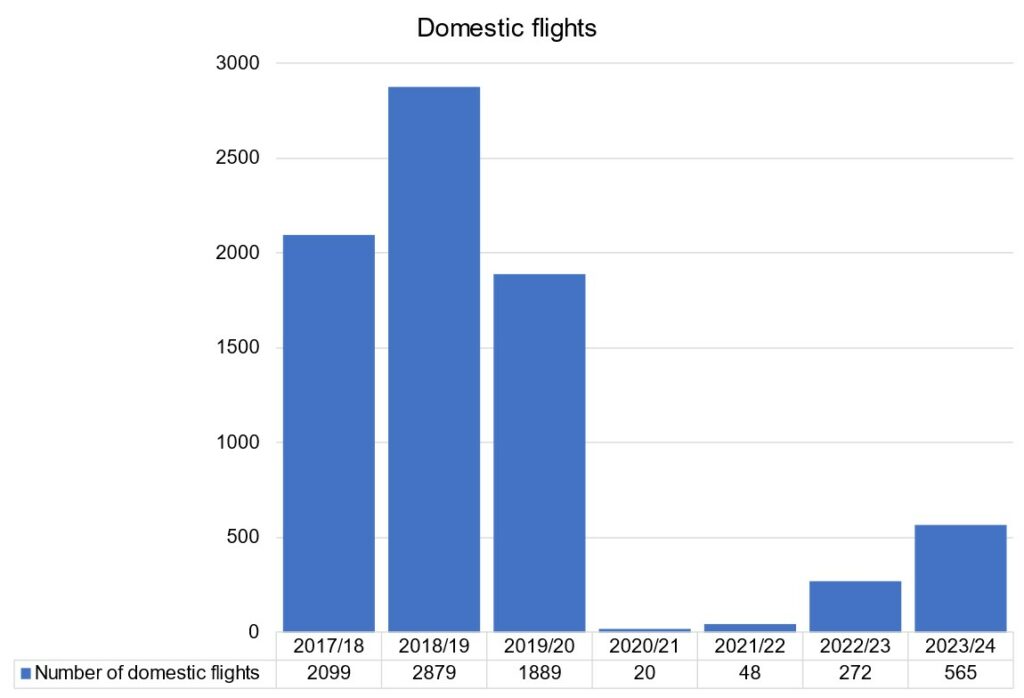
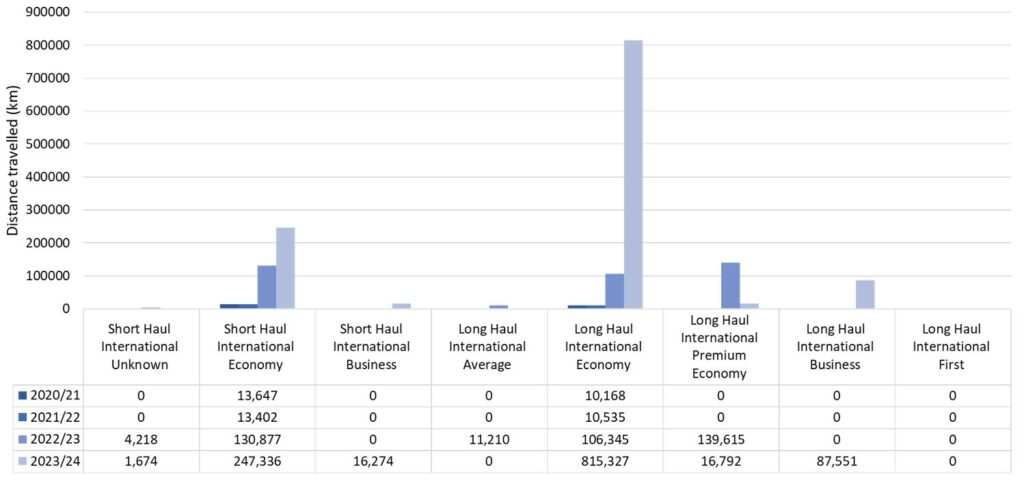
All flights have been categorised as short-haul or long-haul international flights.
We have not accounted for flights departing from and arriving to international destinations separately. Work is ongoing to reduce the number of both domestic and international flights.
Car fleet
2021-25 GGC sub target: Meet the government fleet commitment that 100% of the government car and van fleet will be fully zero emission at the tailpipe by 31 December 2027. This commitment covers vehicles which are leased by employees through the employer’s salary sacrifice scheme.
Zero emissions vehicles against 2027 targets
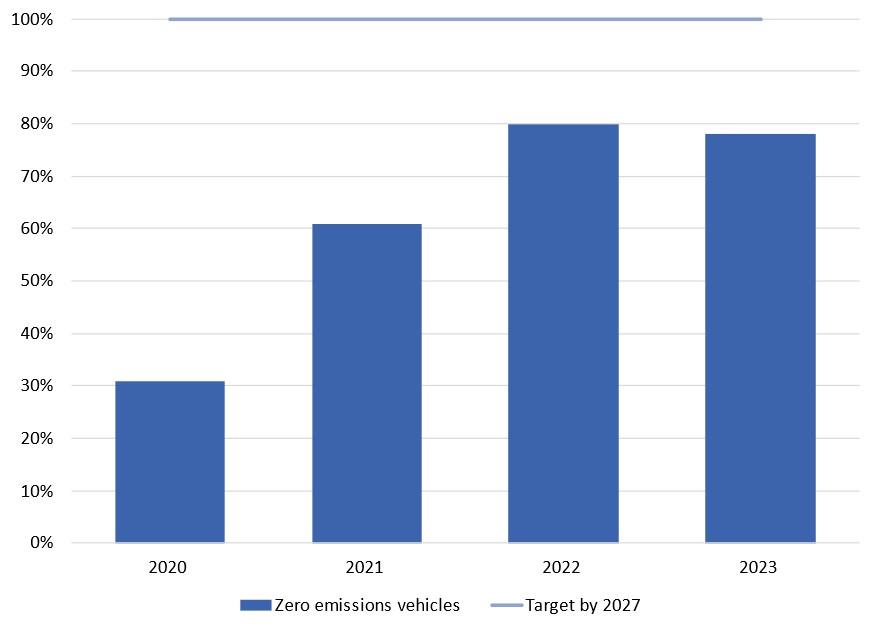
We exceeded the 2022 target to ensure that at least 25% of the fleet was ultra-low emissions vehicles ((ULEV) CO2 emissions below 50 g/km at tailpipe) and by the end of December 2022, 92% of vehicles were ULEV. On 31 December 2023, 93% of fleet vehicles were ULEV.
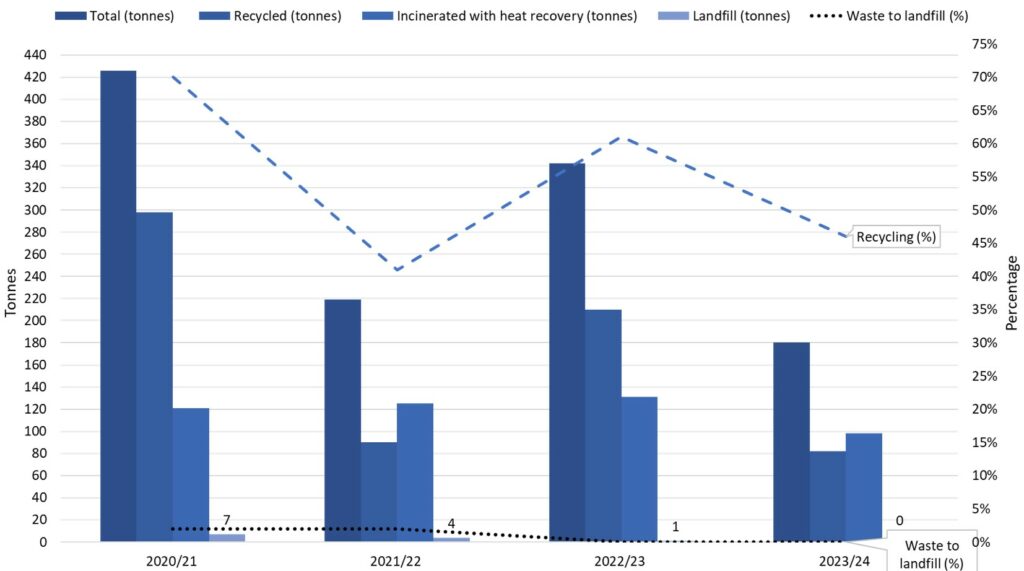
Minimising waste and promoting resource efficiency
2021-25 GGC headline target: Reduce the overall amount of waste generated by 15% from the 2017/18 baseline.
Sub targets:
- reduce the amount of waste going to landfill to less than 5% of overall waste
- increase the proportion of waste which is recycled to at least 70% of overall waste
- reduce government’s paper use by at least 50% from a 2017/18 baseline
- remove CSUP from the central government office estate
- report on the introduction and implementation of reuse schemes.
Minimising waste and promoting resource efficiency
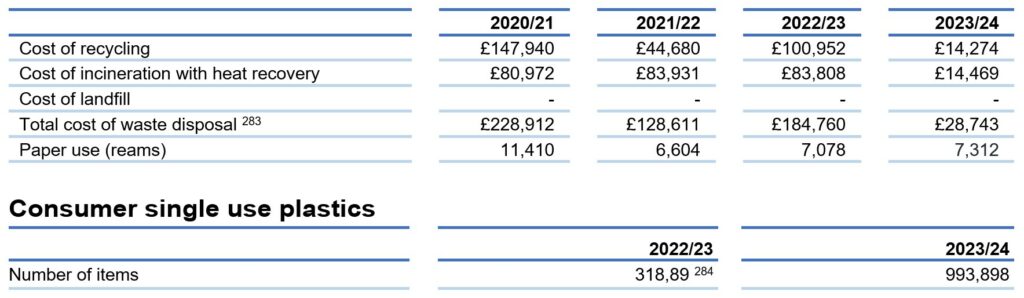
* The cost of waste disposal was not broken down by waste stream in 2019/20 and 2020/21
Consumer single use plastics
| 2022/23 | 2023/24 | |
| Number of items | 318,89 * | 993,898 |
* This figure has been re-stated to correct an error in the NHS England figure reported.
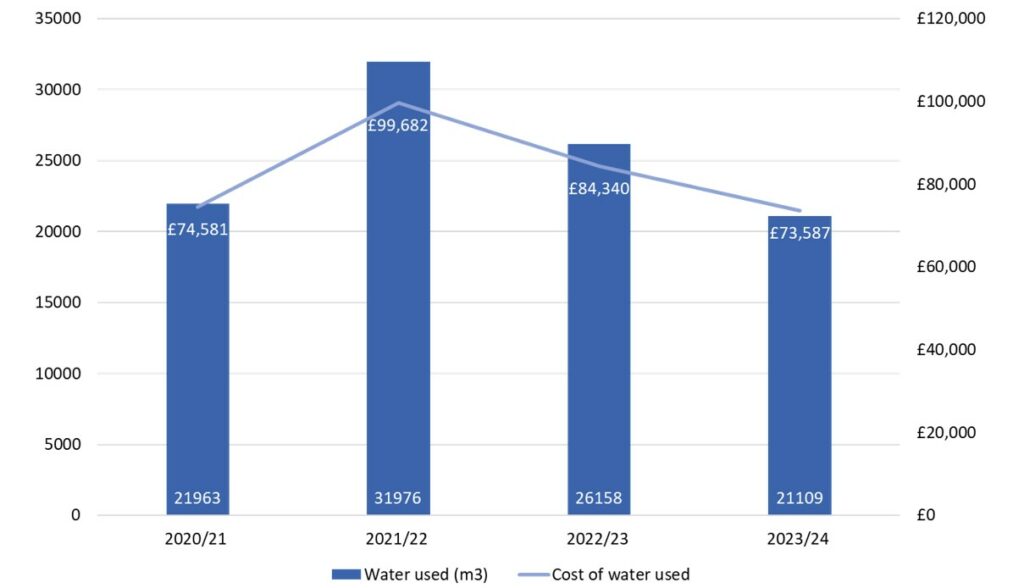
Reducing our water use
2021-25 GGC headline target: Reduce water consumption by at least 8% from the 2017/18 baseline.
Sub targets:
- ensure all water consumption is measured
- provide a qualitative assessment to show what is being done to encourage the efficient use of water.
Utilities, including water, are the responsibility of the landlords we rent offices from. Our NHS Property Services sites are not metered, and data is supplied based on best estimates. NHS Property Services are moving to a single supplier for water, which will allow them to manage water supply and consumption more easily.
Sustainable procurement
Our policy is set out in the published net zero supplier roadmap, with supporting guidance aligned to Procurement Policy Note (PPN) 06/20 on the Social Value Model implementation, and PPN 06/21 on Carbon Reduction Plans. This is furthered by our Evergreen Sustainable Supplier Assessment tool that supports suppliers to understand how to align with our net zero and sustainability ambitions. Modern Slavery eradication aligned to PPN 02/23 is in development.
Net zero and social value buying guides have been produced to support the development of specific category strategies and Government Buying Standards have been included in these guides where relevant.
Nature Recovery and Biodiversity action planning
We do not own any natural capital or landholdings.
Adapting to climate change
Business continuity management identifies our priorities and prepares solutions to address disruptive threats, including those which may be the result of climate change and extreme weather events.
Reducing environmental impacts from ICT and digital
We maintain the use of ICT equipment for as long as possible. When items become obsolete, we work with other organisations to process our ICT waste responsibly and sustainably. This may be through approved authorised treatment facilities, following waste electrical and electronic equipment regulations or using corporate recycling schemes.
Taskforce on climate-related financial disclosures
Compliance statement
Climate change is considered a principal risk for NHS England and our role supporting the wider NHS. It poses a major threat to our health as well as our planet. The environment is changing, that change is accelerating, and this has direct and immediate consequences for our patients, the public and the NHS.
The UK Health Security Agency Health Effects of Climate Change report notes that “Climate change can increase risks to health directly through greater severity and frequency of extreme weather events such as flooding, drought, heatwaves, or wildfires. Many infectious diseases are highly climate sensitive, and with warmer temperatures we can expect an increased risk of new and emerging infectious diseases in the UK, including those transmitted through mosquito and tick bites. The impact of climate change on individuals will vary, with the worst effects on disadvantaged and vulnerable populations, which could widen health inequalities further.”
Our Greener NHS programme leads the way for the NHS to reduce the impact of climate change on public health and the environment, save money and reach net carbon zero. NHS England’s Green Plan sets out our contribution to the NHS vision to be net zero by 2040 for the emissions we control, and 2045 for the emissions we influence.
We have a Board-approved Green Plan, which outlines how the organisation will contribute to the NHS net-zero ambition, and to the GGCs. The Chief Delivery Officer is the SRO for this. Progress against our Green Plan is monitored by our Executive Corporate Group, which meets every other month.
The Greener NHS national programme
The Greener NHS national programme was launched in 2020, alongside the NHS’ commitment deliver the world’s first net zero health service and respond to climate change, improving health now and for future generations. This programme is important because:
- climate change threatens the public’s health and impacts on the NHS’s ability to deliver high quality care now and in the future
- the NHS’s response to climate change is set to deliver unprecedented health benefits through cleaner air, healthier diets, increased energy security and more liveable communities
- reaching net zero provides opportunities to reduce long-term running costs for the NHS
- there is strong support from the system’s 1.3 million staff, with over nine out of ten supporting the NHS’s net zero ambitions.
The Greener NHS national programme is led by the NHS sustainability board. The programme is delivered in the way that is most appropriate and sensitive to each local context by working carefully through the NHS regions and systems.
NHS Carbon Footprint
The NHS has committed to reducing greenhouse gas emissions under our direct control (the NHS Carbon Footprint) to 3,200 ktCO2e by 2028 to 2032 and to net zero by 2040. The trajectory set out in the ‘Delivering a Net Zero NHS’ report implies a reduction to 4,550 ktCO2e in 2023/24.
Provisional calculated emissions for 2023/24 are 4450 ktCO2e (see table). This data, combined with the evidence of action across the NHS as described below, suggests the NHS is on track to meet the target trajectories for the NHS Carbon Footprint in 2023/24, giving confidence in the ability to meet the commitments in 2028-32 and 2040.
These figures are based on both actual and forecasted data as at end May 2024, and may be subject to revision as final input data is published. Updated figures for 2022/23, based on best available 2022/23 data and methodology, are also included in the table.
Provisional estimate of the NHS Carbon Footprint by emissions source
| (ktCO2e, rounded to nearest 50kt) | Confirmed 2022/23 emissions | Provisional 2023/24 emissions |
| NHS Carbon Footprint, of which: | 4,550 | 4,450 |
| Estates | 2,850 | 2,850 |
| Medicines | 1,150 | 1,000 |
| Fleet and business travel | 600 | 650 |
This progress is supported by targeted action across the NHS, including the following areas:
Medicines
Nitrous oxide is responsible for the largest overall volume of emissions from anaesthetic and medical gases, accounting for at least 80% of total anaesthetic and medical gas emissions in 2019/20. Efforts to optimise the use of nitrous oxide products through leaner supply, decommissioning of manifolds where appropriate, and improved stock management and repairs have led to annual savings of £5 million as well as reduced emissions by over 70kt of carbon compared to 2019/20.
Desflurane is a volatile anaesthetic agent with higher global warming potential than alternative readily available general anaesthetic agents. In January 2023, the Association of Anaesthetists and the Royal College of Anaesthetists supported the NHS England announcement of the decommissioning of desflurane in routine practice. In March 2024 NHS England published guidance on the decommissioning of desflurane, building on the NICE Evidence Summary on desflurane. From 1 April 2024, desflurane is only permitted to be used in specific circumstances and as a result, desflurane now makes up less than 0.5% of all volatile anaesthetic gases used in 2023/24 (down from over 20% in recent years), and almost ninety trusts have now stopped using desflurane altogether. This has reduced costs as well as bringing the overall reduction in emissions from desflurane to 40ktCO2e per year from 2024.
The NHS has been collaborating with key partners to support higher quality and lower carbon respiratory care, embedding clinical recommendations into practice, and offering patients lower carbon inhalers where clinically appropriate, supported by a range of resources developed by Asthma and Lung UK. This work has successfully reduced the national average emissions per SABA inhaler prescribed to below 16.4kgCO2e, down from 24kgCO2e in 2021/22, contributing to a 300 ktCO2e reduction in inhaler emissions in 2023/24 compared with 2019/20.
Fleet and business travel
The NHS Net Zero travel and transport strategy was published in October 2023 and is expected to yield annual operational savings of £59 million a year as well as over £270 million a year in wider health and societal benefits. In January 2024, the London Ambulance Service rolled out a zero-emission double crewed ambulance, as part of a pilot involving 5 ambulance trusts, informing future vehicle design specifications, and ensuring the NHS ambulance fleet is resilient to future changes to availability of internal combustion engine vehicles. The proportion of the fleet meeting low, ultra-low and zero emissions standards is increasing year on year: 2022/23 data suggests the NHS fleet is now 89.3% Local Exhaust Ventilation and 7.2% ultra-low or zero emission vehicles – up from 76.3% and 2% respectively in just two years.
Despite this important progress, the estimate of emissions for fleet and business travel has been driven by increased overall NHS activity, including more ambulance mileage and grey fleet mileage (NHS staff using their own vehicles for work purposes). For example, there were nearly 5% more face to face ambulance responses in 2023/24 compared with the previous year (Statistics » Ambulance Quality Indicators). The progress made in electrifying the fleet will lead to emissions reductions in future years as the national grid decarbonises, as well as delivering significant financial savings due to reduced fuel and maintenance costs.
Estates
The NHS is the UK’s largest single public energy user, with an estimated annual energy cost of nearly £1.5 billion. Tackling these emissions requires initial investment but provides financial savings that can be reinvested into patient care. Over £850 million funding has been secured by NHS trusts through the Public Sector Decarbonisation Scheme which is being invested in heat pumps, solar panels, LED lighting and other energy efficiency measures, reducing NHS energy bills as well as carbon emissions. Progress will be further supported by the NHS Net Zero Buildings Standard which became operational in October 2023, and will ensure the development of sustainable, resilient, and energy efficient buildings that meet the needs of patients now and in the future.
NHS Carbon Footprint Plus
The NHS has also committed to reducing emissions from its Carbon Footprint Plus (greenhouse gas emissions under our direct control as well as the emissions we can influence). An update to the Carbon Footprint Plus estimate will be provided in 2025, and ongoing progress is being supported by targeted action including in the following areas:
Supply chain
Meeting NHS net zero ambitions for the carbon footprint plus requires carbon reduction commitments and action from the NHS’s large and diverse supply chain. The NHS net zero supplier roadmap sets out the steps suppliers must take to align with the NHS net zero ambition between now and 2030. In line with this roadmap, since April 2023 suppliers of all new contracts over £5 million per annum have been required to provide a publicly available carbon reduction plan for their scope one, two and a subset of scope three emissions, with a commitment to reach net zero by or before 2050. In April 2024, this has been proportionately extended to cover all new procurements (NHS England » Carbon reduction plan and net zero commitment requirements for the procurement of NHS goods, services and works). In 2023/24, NHS England also launched the Evergreen Supplier Assessment tool, which supports suppliers to engage with the NHS on their sustainability journey and understand how to align with the NHS net zero and sustainability ambitions.
Clinical transformation
Meeting our net zero emission targets requires carbon reductions across all patient pathways, achieved by adopting a clinical and patient-centred approach to delivering high-quality low carbon care. This approach has ensured that new models of care such as virtual wards, the GIRFT High Volume Low Complexity and elective surgical hub programmes are considering their carbon impact and harnessing their carbon reduction potential. As the NHS continues to offer patients greater flexibility in how they receive their care, increased access with fewer repeat trips will improve patient care while reducing travel emissions.
Supported by the NHS and respective Royal medical colleges, specific net zero initiatives such as the Royal College of General Practitioners Net Zero learning hub and the Royal college of Emergency Medicine GreenED accreditation scheme are equipping a growing number of engaged clinical communities to act on meeting our net zero targets.
In January 2023, a significant milestone was achieved through the collaborative efforts of Trinity College Dublin, the Office of the Chief Dental Officer, and NHS England.
The inaugural release of the Clinical Guidelines for Environmental Sustainability in Dentistry marked a crucial step towards raising awareness, offering guidance to dental professionals, and ultimately mitigating carbon emissions associated with oral health and dental care services.
To support clinical transformation in 2023/24, funding was delivered to support innovation to deliver efficient, high quality, low carbon care through the SBRI Healthcare programme. In total 22 projects were delivered, aimed at addressing critical challenges for the NHS.
Workforce
In partnership with the Carbon Literacy Project and E-learning for Healthcare a new training pathway for NHS staff has been developed that covers climate science, impacts and policy. In 2022/23, the NHS delivered a sharp rise in engagement in training at the intersection between climate change and health; from County Durham and Darlington NHS Trust training more than eight out of ten staff on the topic, to more 50,000 NHS staff engaging with the Building a Net Zero NHS e-learning module.
In December 2023, the Council of Deans of Health together with a wide group of stakeholders across the 4 UK nations developed and published curricula guidance for professional bodies and higher education institutions, supporting the incorporation of education for sustainable healthcare within Allied Health Professions curricula and programmes.
Delivering a net zero NHS
The Greener NHS national programme was launched in 2020, alongside the appointment of the NHS’s first Chief Sustainability Officer, to deliver the world-leading commitment of a net zero national health service. The Health and Care Act 2022 introduced new legally binding duties on all NHS bodies, including NHS England, which effectively made this ambition a statutory requirement.
During 2023/24 NHS England, with support from across the NHS:
- Secured an additional £40 million of DHSC funding to deliver energy efficiency schemes to reduce carbon and energy bills across the estate.
- Continued to support trusts to decarbonise heating including through funding from the Public Sector Decarbonisation Scheme, over £850 million of which has been awarded to NHS organisations in recent years, delivering significant financial savings, as well as reducing carbon and air pollution emissions.
- Implemented the NHS Net Zero Building Standard which became mandatory for construction and refurbishment projects over £25 million from October 2023.
- Continued implementation of the NHS Net Zero supplier roadmap, supporting NHS suppliersto engage with the NHS on their sustainability journey and understand how to align with the NHS net zero and sustainability ambitions through launching the Evergreen Sustainable Supplier Assessment tool and publishing guidance on the requirement for carbon reduction plans or net zero commitments.
- Published guidance to decommission desflurane, a volatile anaesthetic agent with higher global warming potential than alternative, readily available general anaesthetic agents. From 1 April 2024 desflurane is only permitted to be used in specific circumstances. Desflurane now makes up less than 0.5% of all volatile anaesthetic gases used in 2023/24 (down from over 20% in recent years), and almost 90 trusts have now stopped using desflurane altogether.
- Continued to collaborate with key partners to support higher quality and lower carbon respiratory care, embedding clinical recommendations into practice and offering patients lower carbon inhalers where clinically appropriate.
- Achieved a reduction in nitrous oxide waste through improved supply and stock management, enhanced piping systems maintenance, and demand reduction where clinically appropriate that is estimated to save over £5 million each year, as well as deliver carbon footprint reduction of over 70ktCO2
- Published the NHS Net Zero Travel and Transport strategy outlining a deliverable roadmap that is expected to yield annual operational savings of £59 million a year as well as over £270 million a year in wider health and societal benefits, including through reduction of harmful air pollutants which cause poor health via ischemic heart disease, stroke, lung cancer and asthma, placing additional burden on the NHS and widening health inequalities.
- Piloted the use of electric vehicles across the fleet, including double crewed ambulances, rapid response vehicles, mental health, and specialist practitioner vehicles, ensuring the NHS is prepared and resilient to future changes to availability of internal combustion engine vehicles.
These milestones helped the NHS reduce its carbon footprint to an estimated 4.4Mt in 2023/24, ensuring we remain on track against the trajectories set out in the Delivering a net zero NHS report.

