Foreword
It has been inspiring to work with NHS colleagues locally, in systems, and nationally on Growing occupational health and wellbeing together. Following an initial review in 2021, wide consultation was undertaken with service-users, leaders and managers, and occupational health and wellbeing professionals, leading to the co-design and launch of the strategy in summer 2022.
This report reflects the progress made over this past year by individuals, teams, and policy supporters, both inside and outside the NHS. I want to thank everyone deeply for prioritising the work necessary to achieve such strong momentum in the first year of this major change initiative. Many people have invested generous personal time and it has been a privilege to chair the Growing Occupational Health and Wellbeing National Steering Group that has provided counsel and direction to the programme.
Growing occupational health and wellbeing together reflects a cultural change in reducing the health inequalities for NHS staff by tackling the significant inconsistency and variation of approaches across our country’s largest employer. Better care for NHS staff delivers improved patient outcomes, better organisational efficiency, and improved performance against regulatory targets. This has been evidenced in many reviews for over a decade (NHS health and well-being review, 2009). The NHS workforce faces the same health demands as the general population, in addition to recovering from the effects of the acute phase of pandemic. The improved capacity and capability of employee occupational health and wellbeing services and professionals is needed if we are to meet the challenges ahead.
I recognise how much has been delivered in less than a year, yet this report also highlights more ahead that needs to be done. My aspiration is that this time “it’s different”. It is vital that the momentum achieved to date is not lost among the noise of wider initiatives. I applaud each of you who are contributing to making Growing occupational health and wellbeing together a reality, to continue to drive better care for staff, and enable better care for our patients.
Dr Steven Boorman CBE, Chair of the Growing Occupational Health and Wellbeing National Steering Group.
Executive overview
Growing occupational health and wellbeing together is the NHS strategic roadmap to grow and improve occupational health and wellbeing (OHWB) services, our multi-professional workforce, and increase the impact it has over the next five years. This will improve the health and wellbeing of our healthcare workforce, which in turn will lead to improved patient care.
NHS England is committed to supporting and empowering our stakeholders to make growing OHWB together a reality, in their local context. This ‘Look back, Look forward’ report showcases the journey, investment, and progress we have made over the past year since the launch of our strategy. It also provides insight into where we need to continue to invest to support our healthcare system, organisational and OHWB leaders to fully realise our shared vision in their local contexts, where they are in the driving seat for local change.
Looking back across 2022-23
John Drew, Director of Staff Experience and Engagement, NHS England.
Growing OHWB together relies on local, flexible implementation of the strategy, led by local leaders and OHWB professionals. Appreciating that the first year of the strategy needed national investment, this last year focused on supporting local healthcare system, organisational and OHWB leaders to ‘level up’ OHWB, while also learning from examples of outstanding practice. This initial investment by NHS England was designed to enable leaders and OHWB professionals to sustain the momentum for growing OHWB together across the future years of the strategy and begin to demonstrate impact in their local context.
In brief, during 2022-23 we have:
Raised the profile and professional identity of OHWB services in the NHS:
Through co-design with over 1,000 stakeholders and launching the strategy, identifying the vision to grow OHWB as an integrated, multi-professional, strategic partnership service that improves the health and wellbeing of our people, to enable them to pass good care onto our patients. We were able to integrate this vision into strategic levers including a mandate for action in the NHS Priorities and Operational Planning Guidance 2023-24, the new NHS Long Term Workforce Plan, and by working with partners such as the CQC to begin embedding our shared vision into strategic quality and assurance levers. We also worked through communities of practice and networks to help them to identify their own local vision for OHWB, to help local leaders and the OHWB community to realise what growing OHWB together means for them in their local context and services. The inception of our national Growing OHWB steering group enabled us to bring together national bodies who play a key partnership role in advancing OHWB, enabling us to work together in implementing the strategy in the NHS, and potentially beyond.
Empowered the development of OHWB services:
Through working with integrated care systems (ICS) and organisational leaders, communities of practice and providing targeted investment that enabled innovation in OHWB services, and subsequently capturing and sharing this practice. We were able to identify exemplary practice in integrated OHWB service development, some of which is already demonstrating significant return on investment that can be spread more widely, for example, significantly reducing sickness absence and saving millions of pounds a year. To support all organisations, we worked to enable the development of good OHWB strategy and service development, through embedding the NHS Health and Wellbeing Framework to support the creation of needs-driven OHWB strategy and services. We developed new resources and development opportunities to help OHWB leaders to embrace service improvement and advance the quality of services through engagement with the quality kite mark standards such as SEQOHS. We also developed a prototype ‘directory of services’ for good OHWB in the NHS to support service improvement, and good commissioning.
Developed our multi-disciplinary OHWB workforce, and wider NHS leader, manager, and teams’ competences in improving health and wellbeing:
This included empowering over one hundred OHWB leaders through formal NHS Leadership Academy programmes and offering leadership development workshops to hundreds more of the OHWB community. We also invested in growing the OHWB nursing, physician, and management workforce capacity by training 114 established NHS clinicians through OH fast-track qualifications, enabling them to safely extend their practice into the OH environment and advance their career pathways into NHS OHWB services. We empowered wider NHS leaders, managers, and teams to take ownership of creating localised wellbeing cultures through scaling and spreading the NHS Leader and Manager Wellbeing programme and implementing new Improving Team Wellbeing Guides. We continued implementation of the new roles of the Health and Wellbeing Guardian and Health and Wellbeing Champions, which supported establishing the strategic voice of OHWB at board level and increased wellbeing support at team-based levels across healthcare.
Advanced OHWB impact and practice:
We identified and shared best practice across our NHS at community of practice events, created online resources including a dedicated Growing OHWB community website, and crafted/shared best practice case studies. This inspired our community by demonstrating that the growing OHWB together vision was no longer just an ambition, but in fact already being delivered across various settings and demonstrating a good return on investment. However, our future challenge is how to replicate this practice and ensure equitable levels of OHWB provision across all parts of our NHS. We also undertook research to better understand and advance contemporary areas within the growing OHWB together strategy. This included how we maximise the wider contributions of both Allied Health and HROD professionals as part of a multi-professional integrated team, and how we can maximise the use of OHWB digital and technology longer-term.
Looking forward to 2023-24 and beyond
The four themes of the growing OHWB together strategy and the actions within each theme outline the future we want to create, and act as our long-term success measures for the strategy. A key success measure for growing OHWB together is that NHS leaders and OHWB professionals are taking ownership of and progressing the strategy in their local context. This is now recognised as a mandate within the NHS Priorities and Operational Planning Guidance 2023-24 and the new NHS Long Term Workforce Plan. Growing OHWB together also aligns to and is supportive of national Government ambitions to expand the impact of Occupational Health across all sectors, as outlined in the Occupational Health: Working Better consultation. Therefore, for 2023-24 and beyond, the call to action remains the same. We must continue to empower NHS system, organisational, and OHWB leaders to grow OHWB services and professions to meet their local need, to improve the health and wellbeing of our workforce, and ultimately pass that wellbeing onto our patients.
As we move into year two of the strategy, NHS England will continue to support the implementation of the growing OHWB together strategy in different local contexts. This will require continued collaboration through working with our national strategic partners, supporting integrated care boards (ICBs) and organisational leaders to own and champion the strategy locally, and ongoing development of our OHWB multi-professional workforce to be in the ‘driving seat’ for change. It will also involve progressing the initiatives and practice from year one of the strategy, to encourage adoption, scale and spread.
For 2023-24 and beyond, this will mean our collaborative focus will be on:
Growing the strategic identity of OHWB, by:
- Empowering ICB and organisational leaders to advocate and act on growing OHWB together in their local context, strategically supported by their OHWB professionals being in the driving seat for change.
- Working in partnership with national bodies to access resources and support.
- Embedding OHWB within strategic performance, quality, and assurance mechanisms, such as the way staff health and wellbeing is monitored.
Growing OHWB services across systems, by:
- Enabling the creation of needs-driven health and wellbeing strategies across healthcare systems and organisations.
- Supporting service development of ‘in house’ and/or good commissioning of external OHWB services across local contexts.
- Enhancing the quality of OHWB services, including adoption of the recently enhanced SEQOHS quality standards.
Growing our OHWB multi-professional workforce and wider NHS leader, manager, and teams’ competence in improving health and wellbeing, by:
- Working with national partners to work toward a multi-professional OHWB workforce plan, spanning various sectors, and aligned to the new NHS Long Term Workforce Plan.
- Developing our multi-professional OHWB workforce capacity and capability, including both professional/clinical competence, and in leadership and service improvement.
- Empowering all NHS leaders, managers, and teams to take ownership of improving their health and wellbeing and creating a culture of wellbeing.
Growing OHWB impact and evidence-based practice, by:
- Sharing good practice in OHWB, that demonstrates the future vision within growing OHWB together is already here in many places, and encouraging adoption, adaptation, scale and spread.
- Enabling OHWB leaders to make better use of data and metrics to demonstrate impact, return on investment, develop needs-driven services, and maintain oversight of quality of services.
- Translating into practice our research to understand how we advance contemporary areas within growing OHWB together, including enhancing OHWB digital/technology, and maximising AHPs and HR/OD contribution as part of the multi-professional workforce.
1. Introducing Growing occupational health and wellbeing together
1.1. Overview of Growing occupational health and wellbeing together
Growing occupational health and wellbeing together was launched in 2022-23 as the NHS five-year strategy to grow the occupational health and wellbeing (OHWB) multi-professional workforce and services that support our NHS people and keep them safe, healthy, and empowered to pass good care onto our patients. It has been co-designed with over 1,000 people across healthcare including OHWB professionals, national experts, integrated care system (ICS) leaders and organisational leaders, and importantly our healthcare managers and employees as our ‘service users’ of OHWB.
Growing OHWB together is a deliverable within the NHS People Plan and has since become a mandate for action within the 2023-24 NHS priorities and operational planning guidelines and the new NHS Long Term Workforce Plan. It is directly endorsed by the NHS Expert Advisory Group for Health and Wellbeing and supported by members of the national Growing OHWB Steering Group, including: DHSC/DWP, Council for Work and Health, Society and Faculty of Occupational Medicine, CIPD, National School of OH, NHS Employers, NHS Health at Work Network, Social Partnership Forum members, and Trade Unions.
The strategy will benefit every member of our healthcare workforce, by keeping them well throughout their career and supporting their diverse health and wellbeing needs, having been built on the design principle that different people need different things at different times.
1.2. Vision and strategic drivers
Growing OHWB has a vision of:
‘Improving the health and wellbeing of our NHS people by growing our Occupational Health and Wellbeing services and people to be trusted, strategic and integrated partners’
The Growing OHWB vision is supported by four drivers, which are split into underpinning areas of collaborative action, framed as such to demonstrate the need for NHS England to empower all levels of the NHS to fully realise these. These also act as our long-term success measures for the strategy. The four drivers and supporting areas for collaborative action are as follows:
1.1. Integrated OHWB
1.2. Strategic voice of OHWB
1.3. A trusted and proactive brand
1.4. Collaborative action and visible investment in OHWB
Driver 2. Growing our OHWB services across systems
2.1. Inclusive, needs-driven, and well-resourced OHWB
2.2. Integrated service user pathways
2.3. Common service development framework
2.4. Service innovation
2.5. Quality improvement
2.6. Maximising technology and digital
2.7. Integrated Care System (ICS) collaboration
2.8. Improving access for smaller healthcare organisations and primary care
Driver 3. Growing our OHWB people (i.e. workforce)
3.1. Multidisciplinary OHWB workforce planning
3.2. Attractive career pathways and talent management for OHWB professionals
3.3. Credible and accessible OHWB education and training
3.4. Empowered OHWB leaders
3.5. Empowered OHWB workforce
3.6. Developing all NHS managers in supporting employee health and wellbeing
Driver 4. Growing our OHWB impact and evidence-based practice
4.1. Using data to demonstrate the impact of OHWB
4.2. Driving OHWB practice
4.3. Demonstrating the value of OHWB
4.4. Driving the OHWB market
4.5. Demonstrating the impact of this strategy
1.3. How we are supporting and enabling Growing occupational health and wellbeing together
INSERT IMAGE – need text description.
List showing how 33 integrated care boards across England have engaged with enhancing their health and wellbeing offers.
London
- South West London: enhanced health and wellbeing – primary care system – inclusive system
- North East London: enhanced health and wellbeing
- North Central London: primary care system
- North West London: inclusive system – growing occupational health and wellbeing – civility and respect.
South East
- Kent and Medway: enhanced health and wellbeing
- Surrey Heartlands: enhanced health and wellbeing – inclusive system
- Buckinghamshire, Oxfordshire and Berkshire West (BOB): enhanced health and wellbeing – primary care system
- Hampshire Isle of Wight: enhanced health and wellbeing – primary care system – inclusive system – growing occupational health and wellbeing
- Frimley: inclusive system – violence prevention and reduction
- Sussex: violence prevention and reduction – civility and respect.
Midlands
- Herefordshire and Worcestershire: primary care system
- Derby and Derbyshire: primary care system – inclusive system
- Leicester, Leicestershire and Rutland: civility and respect
- Coventry and Warwickshire: growing occupational health and wellbeing.
North West
- Lancashire and South Cumbria: enhanced health and wellbeing – inclusive system – violence prevention and reduction
- Greater Manchester: enhanced health and wellbeing – primary care system – inclusive system – growing occupational health and wellbeing
- Cheshire and Merseyside: enhanced health and wellbeing – primary care system.
North East and Yorkshire
- North East and North Cumbria: enhanced health and wellbeing – growing occupational health and wellbeing – violence prevention and reduction
- West Yorkshire: enhanced health and wellbeing – inclusive system – violence prevention and reduction – civility and respect
- South Yorkshire: enhanced health and wellbeing – primary care system – inclusive system
- Humber and North Yorkshire: enhanced health and wellbeing – primary care system.
East of England
- Hertfordshire and West Essex: enhanced health and wellbeing – inclusive system – civility and respect
- Suffolk and North-East Essex: enhanced health and wellbeing – inclusive system – violence prevention and reduction
- Norfolk and Waveney: enhanced health and wellbeing – primary care system – inclusive system
- Bedfordshire Luton and Milton Keynes: primary care system
- Mid and South Essex: inclusive system – civility and respect
- Cambridgeshire and Peterborough: enhanced health and wellbeing.
South West
- Bath and North-East Somerset: inclusive system
- Bristol, North Somerset and South Gloucestershire: enhanced health and wellbeing – primary care system
- Cornwall and IoS: civility and respect
- Devon: enhanced health and wellbeing
- Dorset: enhanced health and wellbeing – inclusive system
- Somerset: enhanced health and wellbeing – primary care system – inclusive system.
Growing OHWB together is a collaborative strategy with implications for all levels of the healthcare system. To be successful, it must be locally driven and fully realised by ICB and organisational leaders, and OHWB professionals in their local contexts through flexible local implementation.
NHS England is supporting local ICB, organisational and OHWB leaders through a centre of excellence model, where we co-design the future direction of travel together, and then identify and spread good practice to support leaders in their local context. We can also support initiatives nationally, where it makes sense to benefit from national economies of scale on behalf of all our stakeholders.
This centre of excellence, collaborative and supportive way of working was developed through the consultation and co-design of growing OHWB together, where it was identified that there is currently very limited capacity and skills in strategic OHWB across all levels of the healthcare system. Therefore, we are working with all levels (i.e., national, system, organisational, OHWB professionals, managers/employees) to ‘level up’ capabilities to meet our collaborative ambition within growing OHWB together.
This approach has been met with praise from NHS ICS/B leaders, healthcare organisation leaders, and national body and partners. It is also seen as best practice by our devolved nations partners (Wales, Scotland, Northern Ireland) across the UK, who are working with us to learn from this approach.
2. Look back: Our journey during 2022-2023
In this section, we look back at our journey and achievements during 2022-23, which represented the first year of growing OHWB together. Our strategy and programme of work is new, and therefore this describes the ‘start up’ journey and investment we have made during year one.
Where applicable, impact data and case studies are shared, which will be tracked and built upon in subsequent years when we gather further impact data on the strategy at local system / organisational levels. Progress and successes relating to each of our four strategic drivers are explored at national level, and then regional system/organisational progress is also shared, with stakeholder insights and case studies threaded throughout.
2.1. Growing the strategic identity of OHWB
The co-design and launch of the growing OHWB together strategy marked a shift in the identity of OHWB services and related professions, and how the NHS thinks about them. It helped us to set the aspiration for OHWB to become a trusted, strategic, and integrated partnership of services and multi-professional workforce, who all work together to support improving the health and wellbeing of our healthcare workforce, which in turn empowers them to pass good care onto patients.
Shifting the identity of OHWB in the NHS requires long-term culture change. The first year represents the very start of our collaborative journey, which focused efforts on co-design and dissemination of the vision with our system and organisational stakeholders and creating partnerships with national bodies that role model the need to work together strategically to realise the vision. We also established ways to integrate our future desired state for OHWB in the NHS into strategic performance, quality, and assurance mechanisms, moving growing OHWB together toward a mandate, and not just a call to action.
2.1.1. Co-designing and launching the strategy and new identity for NHS OHWB
“We have started to shift the identity of OHWB in the NHS to become a trusted, strategic, and integrated partnership of services and multi-professional family, working together to improve the health and wellbeing of our healthcare workforce, which in turn empowers them to pass good care onto patients”.
Dr Shriti Pattani, National Clinical Expert in OH and Wellbeing, NHS England.
Growing OHWB together was launched at in summer 2022, at an event attended by hundreds of NHS stakeholders. The strategy is available on the NHS England website and further resources for the OHWB community can be found on the Growing OHWB NHS Futures community platform.
The strategy formally set out the shift we want to make in the profile and identity of OHWB, toward being a trusted, strategic, and integrated group of services and multi-professional family of people, all working together to support the improved health and wellbeing of our healthcare workforce. ‘Integration’ represents the unique aspect of how we want to think about OHWB, moving away from siloed and unconnected services, where our employees as our patients/service users must navigate them independently, toward an integrated service and multi-professional workforce model who all work together to proactively and holistically support improving the health and wellbeing of our workforce.
The strategy was co-designed over six months with input from over one thousand stakeholders including our multi-professional family of OHWB professionals, national bodies and OHWB experts, ICS and organisational leaders, and importantly our healthcare employees and managers as the service users of OHWB. The co-design approach and emphasis on the need to realise the strategy flexibly and locally has empowered all those who lead on improving the health and wellbeing of the healthcare workforce with a long-term roadmap and ‘call to action’ to work together to achieve this. The impact of this iterative large scale co-design approach meant that our OHWB professionals are in now in the driving seat to take improving OHWB services forwards. Furthermore, this national and large-scale approach of collaboration and co-design effectively ‘crowdsourced’ and created a social movement, where ‘Growing OHWB’ is increasingly becoming not just a strategic priority, but a collaborative model where people see themselves within the ambition and feel a personal attachment to realising this vision.
“The Growing OHWB Together strategic programme has been helpful in validating our local level direction of travel, in particular transitioning to have a strong proactive, preventative element to our model. Our approach continues to be informed by this important strategy.”
Giles Wright, Associate Director of Workforce, Cambridge University Hospitals NHS Foundation Trust.
“Growing OHWB for the first time provides the entire NHS with a collaborative and flexible direction of travel to improve the health of our NHS workforce.”
Integrated care system executive Leader.
2.1.2. Integrating OHWB into strategic assurance, quality, and performance mechanisms
Whilst the growing OHWB together strategy outlines our collaborative roadmap toward our future desired state for OHWB in the NHS, we also recognise that this is one of many competing agendas for ICBs and NHS organisations to advance locally. To work toward this becoming a strategic priority for the NHS, we have started to incorporate Growing OHWB into a variety of strategic assurance, quality, and performance levers. The long-term impact of this will support improving the OHWB of our healthcare workforce as it becomes a mandate for action, rather than an aspiration. This year we have focused on:
- Growing OHWB together as part of 2023-24 NHS priorities and planning guidance and NHS Long Term Workforce Plan: We have ensured that growing OHWB together features as a call to action within the 2023-24 NHS priorities and operational planning guidance and the NHS Long Term Workforce Plan, which both reference the strategy as a priority to support our NHS workforce experience and improve retention. This means that ICBs and organisations across their systems are now required to develop their OHWB services and professionals to support our NHS workforce, acknowledging that this will support recovery of our core patient facing services, improve productivity, making progress in delivering the key NHS Long Term Plan ambitions and continuing to transform the NHS for the future.
- Working in partnership with the CQC to integrate OHWB into the enhanced assessment framework: We have worked collaboratively with the CQC as part of their consultation to evolve their single assessment framework. We have contributed toward a variety of evidence that has supported increasing the presence of OHWB as part of CQC assessments and quality statements. Long-term, this will mean that employee health and wellbeing will become a more explicit and measurable quality indicator, where healthcare organisations must demonstrate that they are equally prioritising this against other quality indicators. Improving employee health and wellbeing will be integrated throughout the new five quality domains including: Governance, management and sustainability; Workforce equality, diversity and inclusion; Partnership and communities; Shared direction and culture; and Capable, compassionate and inclusive leaders.
- Enhancing Safe Effective Quality Occupational Health Services (SEQOHS) framework: SEQOHS represents the standards endorsed by the Faculty of Occupational Medicine (FOM) that are associated with high-quality occupational health services across both public and private sectors. These standards are currently being re-developed to ensure that they are fit for the future with emphasis on outputs and outcomes, simplification, and benefits. We are working with FOM on enhancing the standards to align them with growing OHWB together and maximising the NHS specific domain in the standards to ensure that they encourage OHWB services delivered for our NHS workforce to develop in line with our future vision. The 2023 SEQOHS standards have been launched in draft and are due to be released later in 2023.
2.1.3. National Growing OHWB Steering Group
The Growing OHWB Steering Group was established as an expert group chaired by Dr Steve Boorman and has membership from partner organisations who support improving employee health and wellbeing across the health systems including; Department of Health and Social Care / Department of Work and Pensions joint businesses unit, NHS Trade Unions, NHS Health at Work network, Faculty of Occupational Medicine, Society of Occupational Medicine, Chartered Institute of Personnel and Development, NHS Employers, National School of OH, and is led and hosted by NHS England.
The group has been instrumental in steering the design of growing OHWB together and providing expert advice and guidance to support successful design and delivery. This group has since evolved into a partnership group, acting as a forum to bring together national stakeholders to work together to support implementation, role-modelling the ‘togetherness’ principle of the strategy at a strategic national level in how we cannot achieve the vision alone, and need to work collaboratively at all levels of the healthcare system to realise our joint ambition.
“Growing OHWB Together has contributed to great progress in ensuring a focus on NHS staff health and wellbeing. Considering the retention and health and wellbeing challenges of NHS staff, the importance of this strategy has never been greater.
Post pandemic, there has never been more need for an evidence-based approach to improving staff health and wellbeing, and we know there is a direct link between the health and wellbeing of NHS staff, and patient safety. Investment fits with wider Government ambition to tackle ill health issues in the workforce, highlighted in the Autumn statement, the work and pensions Parliamentary committee, and the Spring Budget.
Growing OHWB together activity is a key part of the NHS People Plan and People Promise and welcomed as a mandate for action for Integrated Care Systems and NHS organisations as part of 2023-24 NHS priorities and operational planning guidance”.
Nick Pahl, CEO of the Society of Occupational Medicine, and Steering Group member.
In this last year, a considerable amount of work and support has been provided to upskill the OHWB workforce both clinically and managerially, which has empowered teams to consider the needs of their service and the vision for improvement and collaboration.
It is recognised that this strategy still has several more years to embed, and that OHWB services in England are striving to keep on that journey to improve the experience for staff and ultimately patient care”.
Hilary Winch, Chair of the NHS Health at Work Network, and Steering Group member.
2.1.4. Growing OHWB collaborative support and regional implementation
We worked collaboratively across all seven regions of NHS England to align and support design and implementation of the growing OHWB together work programme, appreciating the need to support local implementation in a way that takes account of local context. This was achieved through a community of practice, and by regional NHS England teams creating local OHWB networks to support their local healthcare leaders to advance practice.
Regional teams also worked with their local system stakeholders in different ways to gain momentum and adapt growing OHWB together aspirations to meet local needs. This flexibility of local implementation is a distinctive aspect of the strategy, recognising that one size does not fit all, and flexible models of delivery are vital. More information on regional progress is found in section 2.5. regional perspectives.
Case study: Be Well Midlands
‘Be Well’ is an example of how Midland’s region is creating a system-wide approach to improving health and wellbeing. During 2022-23, this regional strategy was co-designed to improve the wellbeing of the people working in health and social care. Using a collaborative approach across all 11 ICSs and using a ‘Big Conversation’ platform, this enabled stakeholders to co-design their regional approach. These insights were translated into actionable solutions to shape how resources are deployed to improve the wellbeing of the region’s healthcare professionals. The strategy focuses on five drivers:
- People before policy: Develop managers to lead with people first, using their compassion to apply policy based on individual circumstances (regional priority).
- Support managers and leaders: Leadership development programmes that focuses on how managers can develop a culture for others to thrive (regional priority).
- Permission to look after our own health and wellbeing: Create a regional workforce plan which incorporates an amalgamation of ICB workforce and operating plans to feedback to colleagues what action is being taken to increase capacity (regional priority).
- Increase opportunities for flexible working: Undertake baseline assessment of systems and status of collaborative banks and use to support with gaps and progress in developing a collaboration across providers (system priority).
- Health Inequalities: Existing health and wellbeing offers will be re-marketed to support with attracting colleagues from under-represented staff groups from needs assessment (system priority).
More information can be found on their website: bewellmidlands.org
2.1.5. Collaboration across the UK
Acknowledging that growing OHWB in the NHS is a UK-wide and complex challenge, we have worked with the four UK devolved nations and formed a working partnership to share practice and collaborate with strategic leaders across England, Wales, Scotland, and Northern Ireland. Whilst in its infancy, this partnership working demonstrates the underpinning ‘togetherness’ value within the Growing OHWB together strategy.
2.2. Growing OHWB services across systems
Growing OHWB Ttogether identified that OHWB services require the same level of investment in service development that patient facing services do, the only difference being that our employees are effectively our patients. To enable this during the first year of the strategy, we were able to begin levelling up investment to support OHWB service development.
We continued to promote and apply the NHS Health and Wellbeing Framework as the strategic toolkit for senior organisational and system leaders to undertake a needs analysis of their workforce health and wellbeing needs and use this to create their health and wellbeing strategy and improvement plan. We captured inspirational case studies that evidenced the impact of the Framework, which led to gaining a Society of Occupational Medicine award for this work.
We also continued investment in supporting the enhancement of OHWB services across ICSs and in organisations through communities of practice. This included working with four Growing OHWB Trailblazer systems to support them and learn from them in creating system-wide services. We also continued our support to ICSs to enhance their health and wellbeing offers through innovative pilots. We captured and shared case studies on how these enhanced OHWB services are demonstrating increased return on investment and can be scaled/spread.
We began to articulate what a good OHWB service comprises of in the NHS, by creating a pilot ‘Directory of Services’. This captures both core mandatory services and evidence-based and needs-driven services that a good OHWB service may offer within their NHS organisations. The impact of this will help both the improvement of in-house OHWB services and inform good commissioning of external OHWB services.
Recognising the need for good quality OHWB services is critical. We supported 12 NHS services to rapidly work toward gaining SEQOHS quality kite mark accreditation. We also worked with the Faculty of Occupational Medicine to support enhancement of the SEQOHS quality standards.
2.2.1. NHS Health and Wellbeing Framework
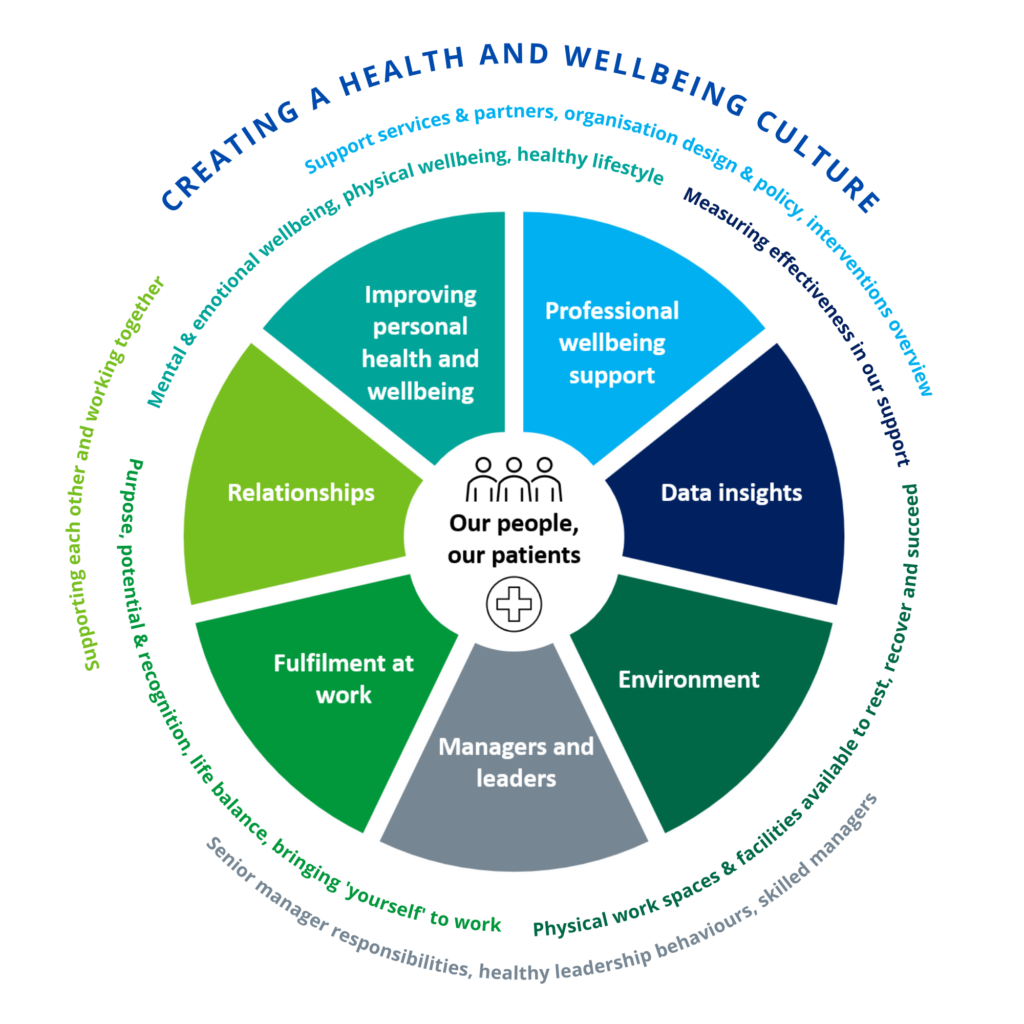
The NHS Health and Wellbeing Framework was enhanced and re-launched in 2021 to better support boards and health and wellbeing leaders to create a culture of wellbeing, through a variety of diagnostic, evidence based, and strategic development tools. It also paved the way to inform growing OHWB together, identifying good integrated multi-professional OHWB services are needed to realise a proactive and preventative wellbeing culture. During 2022-23, the impact of our NHS Health and Wellbeing Framework was recognised through a Society of Occupational Medicine award.
To further embed the Framework as the mechanism for NHS organisations and systems to create their wellbeing culture, we worked with 24 trailblazer organisations and ICSs to support them in using the Framework. At the same time, we captured a variety of learning and impact case studies that support healthcare leaders with their journey of getting started with the Framework. We also developed an impact evaluation report with the 24 trailblazers, outlining shared learning to offer board leaders and Wellbeing Guardians, HROD directors and OHWB leaders insight and support with using the Framework successfully.
Further work we have undertaken to support embedding the Framework across the NHS includes:
- Delivering practical learning sessions across regional teams focussing on each of the seven elements of the Framework. Evaluation demonstrated that these sessions reached over 700 OHWB professionals, who stated that learning from trailblazers on using the Framework in practice, advice from external experts and supporting each other as a community of practice across geographical boundaries, has helped them to advance their local ambitions.
- Providing bespoke ‘consultancy style’ support and bespoke sessions for different leadership communities, including supporting the People Promise Exemplar sites.
- Sharing the Framework and the impact it has had on supporting improving employee health and wellbeing across wider sectors, including national and regional conferences, NHS ‘Do OD’ conference, the national CIPD wellbeing conference, the global Work and Health conference.
2.2.2. Creating a service development framework for OHWB services
During the co-design of growing OHWB together, we identified that OHWB services had not benefitted from the same service improvement support as our wider patient facing services had, despite equally being clinically/professionally driven services. We also identified that there is currently no detailed description of what constitutes a good OHWB service in the NHS, meaning that it is difficult to design and develop in-house, and/or commission external quality services. In response to this, we have begun the development and piloting of a variety of resources, working with an expert design group, and engaging with over 200 stakeholders.
We have developed a pilot ‘directory of services’ for OHWB, which outlines the elements of a good OHWB service as mandated by legislation and national guidelines, as well as the added value services that are shaped by local insight and workforce need. The first copy of our OHWB directory of services has been shared with stakeholders and is currently being tested out in a variety of forums to improve in-house delivered OHWB services and inform the commissioning of OHWB across organisations and shared services across ICSs.
We also began co-designing an OHWB service development framework and principles for good service improvement that will provide practical guidance to developing services in organisations and across systems, to flexibly encompass the diverse delivery models needed across the NHS. The framework is based on good service improvement methodology and provides a roadmap for future development, designed to support services at whatever stage they are at on their service development journey.
Both the pilot OHWB directory of services and service development and improvement support can be accessed by signing up to the Growing OHWB community NHS Futures site. Whilst in their infancy, the directory of services and service development support are paving the way to inform and enable OHWB service leaders and commissioners to develop their services, through good quality service improvement methodology, throughout the lifetime of growing OHWB together, and beyond.
2.2.3. System and organisational Trailblazer community of practice
We identified several ICSs and organisations who were ready to advance their ambitions to grow their OHWB services across a large system footprint at pace through a strategic readiness process and worked with them as a community of practice to offer targeted support and resources. In return, these trailblazers have worked closely to inform the design, learning and best practice within the Growing OHWB together strategy, demonstrating to others that it can be, and is being achieved.
“Case studies demonstrate the significant impact and return on investment that OHWB trailblazers are making, which if scaled and spread will not only improve the health of our NHS workforce and keep them in work, but also save millions of pounds which can be invested back into patient care”.
Trailblazers focused on realising their vision of a multi-professional workforce and integrated services across systems by being needs driven and based on local workforce intelligence, and an ambition to offer faster and equitable access to OHWB support to staff. They achieved this through redesigning services to target preventative support for high impact workplace health and wellbeing issues.
Case studies demonstrate how these Trailblazers have advanced the evidence base for growing OHWB services as outlined in the strategy, through both process and impact evaluation, where some services have demonstrated strong return on investment and cost savings, through improved wellbeing and reduced sickness. This learning is being shared across healthcare leaders and the OHWB community, to support scale and spread.
The following case studies demonstrate the significant impact and return on investment that OHWB trailblazers are making, which has the potential not only improve the health of our NHS workforce, keep them safe healthy and in work, but also save millions of pounds which can be invested back into patient care.
Case study: Hampshire Isle of Wight Integrated Care System (HIOW) system wide OHWB services
HIOW is a Growing OHWB Trailblazer. They focused their collaborative efforts on creating system wide integrated and multi-professional OHWB services that supported large scale health improvement reaching 20,000 people in their healthcare workforce across all partner organisations. They used the NHS Health and Wellbeing Framework to scope the workforce needs and developed an investment plan based on this. Since then, they have created new needs-driven, system-wide OHWB services which have included: increased access for primary care, system wide menopause services, a system-wide staff physiotherapy service, and an innovative Employee Disability and Neurodivergent Advice Service (EDNA). In a short space of time, these services have led to over 8,300 face-to-face engagements with staff to improve their health.
Since the launch of the systemwide physiotherapy service in July 2022:
- Over 2,700 referrals were actioned via self-referral or OH, which has enabled early interventions and rapid access to musculoskeletal services.
- 68% of clients surveyed reported the service had stopped them needing support from their GP, which leading to estimated savings of between £68k-£137k to primary care in the costs of GP appointments, as well as freeing up appointments for the wider community.
- 93% of individuals would recommend the service to a colleague, where 83% of individuals using the service reported it has had a positive impact on their health and wellbeing.
EDNA demonstrates an innovative, needs-driven service within OHWB. Whilst in its infancy since launch in December 2022, it has seen 238 new referrals and 61 follow-up appointments, demonstrating a high demand. 82% clients stated that support from EDNA is helping them stay in their role and supporting retention, 45% said that EDNA has stopped them taking time off sick, and 36% felt that EDNA had meant they hadn’t needed to see their GP.
“I love my job now as I am less stressed and am now getting more done. I have accomplished lots in the past 6 weeks in my role!” EDNA client
These innovative needs driven OHWB service approaches are growing from strength to strength, demonstrating the power, economy-of-scale, and impact of system wide collaborative OHWB service development in a relatively short space of time.
Case study: Manchester University NHS Foundation Trust integrated multi-professional services
Background
With the support of the national Growing OHWB programme and aligned to the integrated multi-professional services drivers, Manchester University’s NHS Foundation Trust (MFT) Employee Health and Wellbeing Service (EHW) have been able to accelerate the development of existing musculoskeletal (MSK) services provided to their 28,000 staff, by enhancing and delivering a range of innovative MSK services. These services have ensured that all staff benefit from a comprehensive and consistent model of care, which support MFT’s ongoing Wellbeing Strategy and contribute to high levels of employee engagement, increased productivity and a significant reduction in operational costs – all of which ultimately benefit patients.
Return on investment
MFT’s MSK service model has three core components; the Rapid Access (Self-Referral) Advice and Treatment Service, Absence Support Service and the MSK Ill-health Prevention and Education Programme. By providing timely and appropriate MSK services for staff, the EHW Service has been able to demonstrate a positive and significant impact on reducing MFT’s MSK conditions absence costs and as a consequence an increase in workforce productivity. Trust absence data for the past 3 years shows that since the implementation of the Absence Support Service in May 2022, the upward trend in MSK absence has been reversed with the length of MSK absences now reduced by 11-days per absentee, on average. MSK sickness absence costs for the Trust have reduced from £23,000 per day to £17,000 per day, with a cost saving of £180,000 per month, which is estimated to have saved £2.16m per year.
User feedback
The MSK Service is highly valued staff and managers as demonstrated by ongoing feedback – the service regularly receives a 4.7/5 ‘Star’ Rating. Testimonials from service users demonstrate the impact and benefits:
“I was seen within 5 days of self-referring. The practitioner was very good at explaining the cause of my pain and restriction to my movement in relation to both work and leisure activities. The exercise programme I was given made a huge difference to both my work and home life. I was able to return to some of my theatre lists that I had been unable to do, and I was stronger and has much less pain and restriction than when I started …
… I was also quicker at performing work tasks and in addition my mood was improved due to physical improvement and from the better understanding they gave me of my condition and how to support it. Without this EHW Physiotherapy service I would not have been able to return to my full work duties nearly as quickly as I did without further time off work. I am forever grateful”. Consultant, Manchester Royal Infirmary.
Scale and spread:
The Growing OHWB programme has enabled extensive engagement with other trailblazers and OHWB leaders across the country. MFT have been able to share best practice and lessons learned with respect to OH service enhancement and development. With the support of the National and Regional teams, MFT have been able to share their learning, as well as highlight barriers and challenges detailing the steps being taken to overcome them. This approach has assisted other organisations and systems to review and develop their own MSK service offers to address the impact of MSK conditions on the NHS workforce.
2.2.4. Wider continued support for enhancing health and wellbeing services across systems
As part of our wider work to enhance health and wellbeing services across systems and since the programme first launched in 2020-21, we have continued to work with 33 of the 42 ICSs across England through various service enhancement programmes. These include:
- Enhanced health and wellbeing programmes across ICSs
- Primary care system health and wellbeing pilots
- Inclusive health and wellbeing pilots
- Health and Wellbeing Trailblazers
- Civility and Respect
- Violence Prevention and Reduction
During 2022-23, we continued to support these enhanced wellbeing services pilots through a community of practice model. Evaluation findings have demonstrated that systems have taken collaborative and inclusive approaches to understanding local workforce needs and providing a range of tailored health and wellbeing support offers which are reflective of the pressures their workforce are facing. Projects have identified that some of the key enabling factors to fostering success have been the clear leadership and governance in addition to the broader stakeholder engagement. The programme has been recognised as promoting a culture of joint working across the system to promote health and wellbeing for the wider workforce across different organisations.
INSERT IMAGE – do we need this map?
2.2.5. Safe Effective Quality Occupational Health Service (SEQOHS) accreditation support
We have been working in partnership with the NHS Health at Work Network to increase the number of SEQOHS accredited NHS OHWB services in England by:
- providing active support to NHS OHWB Services seeking full SEQOHS accreditation.
- providing advice and facilitating the sharing of good practice with those NHS OHWB services pursuing their 5-year re-accreditation.
- supporting NHS OHWB Services to understand the implications of any changes to the existing SEQOHS accreditation standards.
The SEQOHS support project was promoted at the regional community of practice meeting leading to follow up meetings with individual OHWB services. There are currently 12 OHWB services who are being supported to rapidly gain full SEQOHS accreditation.
2.2.6. Supporting primary care
Further work was conducted in 2021/22 to support the wellbeing of colleagues working across primary care and bring them into the wider NHS family. A national working group was established to develop a joint plan, outlining the priorities to focus on in 2022/23 to enhance the health and wellbeing of our primary care workforce. While this is a complex landscape, we have been able to work with primary care partners to flexibly adapt and adopt national initiatives such as wellbeing conversations, reducing violence against primary care staff, and Wellbeing Guardians. We also supported primary care workforce with workshops to improve their health and wellbeing and continued sharing supportive resources. We have identified case studies where primary care health and wellbeing models aligned to Growing OHWB have been successfully created, to share with wider stakeholders for consideration toward adopt, adapt, scale, and spread.
Cambridgeshire and Peterborough Integrated Care System: A primary care occupational health (OH) and human resources (HR) service
The Cambridgeshire and Peterborough Primary Care OH and HR Service pilot was designed to deliver an enhanced Occupational Health and Wellbeing service to c.3800 people working in Primary Care in the area, including independent Community Pharmacies, General Practices and GP Federations. Primary care sites were set up on a portal, offered training and support to engage with the health and wellbeing services through a variety of promotional material. Highlights include:
- 56% of primary care sites made an Occupational Health referral in the first year.
- Over 80 health checks in the first year have been delivered to primary care staff.
- Quarterly People Pulse Survey to staff involved, the first of its kind in the country.
- Introduced HWB champions in primary care, and developing a People Plan action plan for primary care in their area.
This approach demonstrates innovative ways of supporting increased and equitable access of OHWB across primary care.
2.3. Growing our OHWB multi-professional people and wider workforce
The ambition within growing OHWB together identifies our need to rapidly grow our multi-professional OHWB workforce. Furthermore, health is everyone’s business and to effectively create a proactive and preventative culture of health and wellbeing for our healthcare workforce, we need to empower leaders, managers, and team members to improve their own health and wellbeing.
During 2022-23, we focused on rapidly investing in ‘levelling up’ both the capacity and capability of our OHWB multi-professional workforce, in addition to empowering leaders, managers and teams to create a local health and wellbeing culture.
We supported increasing the capacity of our OH clinical workforce by taking 29 doctors, 30 nurses and 55 managers through professional development qualifications to enable them to effectively and safely practice in OH. We also supported the leadership development of our multi-professional OHWB community through taking 114 professionals through formal NHS Leadership Academy development courses, whilst also offering a variety of bite-size learning courses to 100’s of other OHWB professionals on various needs-driven leadership topics, with wider resources available on the Growing OHWB community website.
Recognising that leaders and managers play a key role in creating a local wellbeing culture, we created, piloted, and began scaling and spreading a new NHS Leader and Manager Wellbeing programme designed to support leaders to improve their own wellbeing, and go on to improve the health and wellbeing of their diverse team members. This is being scaled through developing local faculties of trainers in NHS organisations, so that this can be sustainable long term.
To develop and empower teams to improve their wellbeing, we co-designed and launched new team health and wellbeing guides, enabling them to undertake a self-facilitated journey across various evidence-based topics that will enable them to improve their own health and wellbeing, and create a local culture of wellbeing.
We continued to support implementation of Health and Wellbeing Guardians and Health and Wellbeing Champions, to improve reach of health and wellbeing advocacy and support at both strategic board-level, and local team-levels.
We also undertook various research to improve understanding of how we can begin to widen our multi-professional OHWB family of roles, seeking to understand how we can maximise the contribution of Allied Health Professionals in improving employee health and wellbeing, and also the evolving health and wellbeing lead role to act as an organisational tactical and strategic enabler in creating and leading integrated OHWB services and offers. This resulted in partnership work with CIPD aligned to the new HROD future professions map to create new qualifications for HROD professionals wishing to work in OHWB.
2.3.1. Developing our occupational health and wellbeing leaders
Growing OHWB together puts our OHWB multi-disciplinary workforce in the driving seat of leading the enhancements of their services. To empower them to take up this challenge, we have invested a variety of leadership development offers to upskill them to effectively lead their teams, develop their services, and enable innovation in OHWB to drive forward the transformation of services.
We enabled 92 of our established OHWB leaders to take part in bespoke cohorts of the NHS Leadership Academy Rosalind Franklin programme tailored to the OHWB community. Evaluation demonstrated that the programme was hugely impactful for these leaders, who stated that the programme provided them with the confidence to deal with complex problems and tackle the huge challenges in recovering employee health and wellbeing post pandemic by redesigning service delivery. It allowed them the opportunity to focus on creating change, enabling them to become more competent, compassionate, and inclusive leaders and managers, whilst maintaining their resilience.
To encourage talent pipelines, we also supported 16 of our aspiring OHWB leaders to engage with the NHS Leadership Academy Mary Seacole programme. Excellent feedback identified that participants felt it prepared them to take on a formal leadership position within OHWB. They stated the programme empowered them to lead successful teams, that champion compassionate patient care.
“The development journey I experienced was phenomenal, which in turn has benefited my department and my Trust workforce as a whole.”
“The programme was valuable in helping focus on creating change, dealing with complex problems and maintaining resilience.”
“This training provided new skills and knowledge around leadership that enabled me to offer better leadership to the team and service.”
“It empowered us in our formal leadership position to transform teams for success and to champion compassionate patient (i.e. our staff) care.”
Participant testimonials from the professional OHWB leadership development offers.
2.3.2. Increasing capacity of the occupational health clinical and managerial workforce
Growing OHWB together identified that we do not have enough core occupational health professionals to meet the health and wellbeing needs and demand from our NHS workforce. During 2022-23, we rapidly ‘levelled up’ our core occupational health workforce by investing in qualifications for existing clinicians who want to move their careers into occupational health and wellbeing services.
We funded 29 places for physicians on the Royal Society of Public Health Diploma in Occupational Health Medicine intensive online training course, designed for existing qualified physicians and GPs looking to extend their practice into occupational medicine in the NHS. The programme was positively evaluated, where 92% of participants felt the course was excellent or good with 100% stating that they could apply the learning to practice and seek to move their careers into occupational medicine.
We also funded 30 places for nurses on the Diploma in Occupational Health Practice, to support established nurses seeking to extend their practice into NHS occupational health teams. Participants rated the course well and shared how the course helped them in improving the knowledge, skills, and confidence to work in occupational health practice. We were also able to share case studies on the impact of these courses on our clinicians careers. Both qualifications will enable these 59 physicians and nurses to undertake their professional qualifications in occupational health practice.
Demand for these qualifications outstripped supply, where we had over 70 physicians and 140 nurses apply, demonstrating a strong pull for wider clinical professionals to embrace a career in occupational health and wellbeing.
Our approach was seen as exemplary by the Department for Work and Pensions / Department of Health and Social care who are looking to expand the occupational health workforce across all sectors as part of Health is Everyone’s Business. We are partnering with them to expand and sustainably replicate this approach nationally across wider sectors, encouraging careers into occupational health and supporting the retention of our clinical workforce.
We also empowered 55 professionals to undertake the Certificate in Managing Occupational Health Services award to support them moving into the management of occupational health services by building on their professional training. Participants stated that the course was invaluable in providing a solid grounding to help them to drive forward quality occupational health in their workplace.
“I have increased my knowledge and understanding of Occupational Medicine and improved my clinical practice … It has been very beneficial in building the foundations of my potential future career in Occupational Medicine.”
“It has deepened my knowledge, which I am now able to demonstrate in the workplace … reinforced the benefits of pursuing an OH career for me … I gained a deep appreciation and understanding of what people in need of OH services are experiencing, as well as a great respect and admiration for the professionals of Occupational Health.”
“Energising and thought-provoking course. All OH people should be encouraged to attend to improve their practice.”
Testimonials from the professional OH physician, nurse, and management qualifications.
2.3.3. Bespoke workshops and resources to upskill OHWB professionals
We recognised that not all OHWB professionals have the capacity to engage in a long-term development programme. We put our OHWB people in the driving seat and asked them to identify the key leadership and improvement skills they need to better lead their services, and delivered a series bespoke ‘bite-sized’ learning workshops to address their knowledge gaps. These were in: building your business case, influencing strategically, business acumen for leaders, and using data effectively.
The workshops were attended by 208 participants and were well evaluated, where 77% of participants felt they helped them to become more effective in practice and 84% felt well prepared to apply their knowledge, learning and skills back at the workplace. Workshop resources are available on our Growing OHWB community website.
“It gave me knowledge and insight into areas and activities to improve my leadership skills.”
“This bite size learning and networking is refreshing – an easy commitment to make and spark ideas.”
Testimonials from bespoke OHWB workshops.
2.3.4. Establishment of a Growing OHWB alumni community
Participants who engaged in the professional development offers identified that networking and peer support was a huge benefit to engaging in the courses. To enable this, we established a Growing OHWB alumni community or practice network to enable them to continue to engage and support each other with peer support.
The community has been co-designed with colleagues from our alumni, is chaired by a Consultant and Head of Occupational Health and Wellbeing, and is designed to offer:
- A safe, confidential space to share your leadership journey, practice, and challenges
- Learning and development
- Networking and peer support
Future alumni sessions will be co-designed to ensure the needs of our OHWB community alumni are met and are supported to continue to embed their learning in practice, as champions for recognising the ambition within growing OHWB together.
“The Alumni group has been useful for sharing best practice – it helps me to drive this agenda forward.”
Testimonials from the OHWB alumni community of practice.
2.3.5. Evolving the NHS Health and Wellbeing lead role in partnership with CIPD and AHSN
The role of the ‘health and wellbeing lead’ has increasingly become common in the NHS over the past several years, often acting in a leadership capacity and bridging the gap between HROD and OHWB professions. Yet, we identified lack of understanding around a common role profile, competencies, and talent pathways.
We partnered with the Health Innovation Oxford and Thames Valley to undertake research into those who lead NHS staff wellbeing in organisations and systems, with work towards professionalising health and wellbeing leadership as a career in the NHS.
Engaging with over 500 health and wellbeing professionals, we found the commonality of this emerging role was acting as the ‘tactical enabler’ to bring together all elements of an integrated employee health and wellbeing strategy, services and offers. Yet, there is currently no formal training or career pathway for these individuals they often come from a variety of professional routes, most often HROD and wider OHWB backgrounds. We also started to identify common competencies and career pathways that will help us to develop this as an established role within the NHS.
Spring boarding from this research and as part of aligning to NHS HROD Futures and our partnership with CIPD and work with them on the new CIPD professions map which now includes wellbeing as speciality, we were able to identify an opportunity to initiate the creation of a development programme for all wellbeing lead professionals from an HROD background. We are in the process of working together to engage with subject matter experts to create this programme, which will help solidify professional training and career development for health and wellbeing leads. This programme will be available later in 2023-24.
2.3.6. NHS leader and manager wellbeing programme
Leaders and managers form part of our OHWB multi-professional family by extension, as they are critical in creating a proactive and preventative culture of wellbeing for their teams to thrive, so that they can pass this wellbeing and care onto our patients. Yet, we still need to build leaders and managers capability in supporting the health and wellbeing of their diverse teams. Equally they too need support to improve their own personal wellbeing.
The new NHS Leader and Manager Wellbeing Programme was designed to address this. After hugely positive evaluation and feedback from a national pilot, we were able to begin scale and spread of this programme during 2022-23. To maximise impact, reach and long-term sustainability, we began offering the programme in different formats, one that supports direct national entry for senior leaders to empower them to improve their own wellbeing and role model it for their teams, and secondly a local ‘train the trainer’ offer, designed to train OHWB and HROD professionals in local organisations across their ICS to roll the training out themselves directly to support their frontline organisational leaders.
As part of this pilot year, we have trained 160 senior leaders and 26 local faculty trainers who have begun delivering local programmes within their own organisations and have developed plans to rapidly widen the local faculty over the next two years to make this approach sustainable. As leaders and managers impact the health and wellbeing of their large diverse teams, we predict the reach of this pilot year alone has supported an improved wellbeing culture for over 10,000 healthcare people, which will continue through a butterfly effect.
“I thoroughly enjoyed the course and am looking forward to introducing many of the practices explored in my work and personal life, and with my team.”
“It was a wonderful experience being a part of the course and sharing it with such an amazing group of people to improve our wellbeing, and our teams.”
Testimonials from participants on the NHS leader wellbeing programme.
2.3.7. Empowering teams to improve their health and wellbeing
Ongoing research demonstrates that good teamwork and social wellbeing contributes to good work and good health. Whilst redesigning the NHS Health and Wellbeing Framework, stakeholders asked for a resource that supports teams and team leaders to self-facilitate improvement to their health and wellbeing, in a simple, fun, and engaging way. This was further supported by the North West Leadership Academy Healthy Leadership Behaviours Framework and research.
In response to this, we co-designed a new suite of Looking After Your Team’s Wellbeing Guides in collaboration with people across over 100 NHS and social care organisations, piloted and enhanced by 18 organisations, and finally launched during January 2023. The new guides draw inspiration from the NHS Health and Wellbeing Framework, and the Healthy Leadership Framework. They are a simple toolkit to help NHS and social care managers and their teams engage with and embed the principles of wellbeing, and promote wellbeing culture in their local settings.
The guides are designed around a ‘choose your own journey’ model, where teams are encouraged to start with the getting started, diagnostic and goal setting guides, and then choose their most relevant next guide to work through based on their needs analysis, such as improving physical emotional and mental wellbeing, or improving team social wellbeing. Insights, inspiration, and further learning resources are also captured, which will be expanded over time and made available on our Growing OHWB community website.
Whilst in its infancy, early evaluation and early feedback from teams using the guides and strategic partners such as trade unions demonstrate highly positive feedback.
“We now have protected time as a team, a dedicated one hour where we focus together on health and wellbeing. We try to do different things which focus on both mental and physical aspects of health.”
“The team has improved cohesion, by just knowing people are not on their own in their views and issues. It is also motivating that the Trust is promoting this – the team felt it was really positive.”
“It is good to have the options of the tools to use, as one size doesn’t fit all. This gives options for light touch or a deep dive into a topic”.
“This guide helps move things forward. It empowers people to ask questions, take action and to feel valued.”
“We developed a positivity post-board which both patients and staff can see. Patients are seeing that we care about staff and each other.”
Testimonials from teams using the team wellbeing guides.
2.3.8. Wellbeing conversations
The NHS People Plan sets out the ambition that all healthcare employees should have a health and wellbeing conversation. To support NHS organisations with the local realisation of this ambition, we are continuing to support managers in facilitating wellbeing conversations, and a national training programme was launched in which resulted in 3,635 managers undertaking conversation training.
Evaluation demonstrated the training improved managers understanding, skills and confidence in facilitating these conversations in a meaningful way and support their team members to improve their wellbeing through action planning. This subsequently positively impacted team morale, feeling valued, reassured, listened to, and resulted in improved working relationships. Managers also indicated that the training helped to improve their own sense of personal wellbeing. A train the trainer model was adopted to make this approach sustainable, where 88 facilitators were trained during 2022-23.
The wider impact of managers trained and conducting meaningful wellbeing conversations has been demonstrated through the NHS people pulse, where individuals who identified they had undertaken a conversation was positively corelated with how they perceive the organisation supports their health and wellbeing.
“It gave me the opportunity to reflect on my own wellbeing and recognise what I may have been neglecting. It reminded me of the importance of taking care of myself in order to be able to take care of others”.
Testimonials from wellbeing conversations evaluation.
2.3.9. Health and Wellbeing Guardians
Part of the vision within growing OHWB together is to increase the strategic voice of OHWB. The new role of Health and Wellbeing Guardians is pivotal to this, acting as the champions for OHWB at board-level leadership and holding the organisational leaders to account for improving the health of their workforce.
During 2022-23, 96% of NHS provider organisations reported that they had a health and Wellbeing Guardian in post. As a new strategic and board-level assurance role in OHWB, we continued to support the Guardians to understand how they could make an impact through regional networks and national communities of practice.
We engaged Guardians to evaluate the progress and impact of their role through a mixture of formal research and evaluation. Guardians reported:
- A positive move throughout the year towards achieving long term wellbeing culture change through the wellbeing guardian function.
- Greater focus on holding leaders in the organisation to account to improve health and wellbeing of their workforce.
- An ever-increasing focus on getting the best out of corporate data to support the staff health and wellbeing agenda.
- Increased focus on responding to operational challenges and a greater focus on “cure”.
During 2022/23 wellbeing guardians provided feedback in several areas where the national team were able to act and implement change. We worked with the Guardians to capture their voice and influence national health and wellbeing strategy through networking, evaluation, and journalling platforms. For example, this resulted in them influencing our partnership work with the Care Quality Commission (CQC) to enhance focus on employee health and wellbeing during inspections, and the development of new health and wellbeing resources which focus on support suicide postvention.
Impact evaluation and ongoing co-design work with the Guardian community also identified the need to support the evolution of the Health and Wellbeing Guardian guidelines to both simplify their strategic assurance function, in addition to widening their reach across NHS system organisations and primary care. Work was undertaken to evolve, update and expand the Wellbeing Guardian’s guidance to make it relevant to all areas of the NHS. Extensive stakeholder engagement was undertaken with Wellbeing Guardians and organisational leaders across primary care, secondary care and with integrated care boards (ICBs) to help evolve the national guidance to suite the different organisational context needs. This has resulted in new guidelines which will be released early in 2023-24.
“HWB was higher on the agenda during the pandemic. Now, as the conversation moves to recovery, I am concerned that the conversation will move on to focus exclusively on productively and reduction in agency. We need to keep HWB high on the agenda in light of the cost-of-living crisis and potential impact on suicide rates”.
Non-Exec Director, Health and Wellbeing Guardian.
“My organisation has long had a strong wellbeing offering, but we have revisited the entire programme over the last six months and re-established the strategy, based on feedback and learnings. It has been a very powerful exercise and we have benefitted from the fresh look at what we are doing and where the gaps are”.
Non-Exec Director, Health and Wellbeing Guardian.
2.3.10. Health and Wellbeing Champions
Health and Wellbeing Champions create supportive wellbeing cultures at team/colleague level. We have progressed a programme to support NHS organisations in rolling out Health and Wellbeing Champions at local level, which included developing champions through a long-term development programme, e-learning, wider training/qualifications and sharing supportive resources through our national Champion community of practice.
During 2022-23, we grew and supported our national network of over 2,500 Champions across the NHS covering a range of roles, grades, demographics, and sectors. 22 development sessions have been delivered, supporting Champions to learn more about specific wellbeing topic areas, including menopause, financial wellbeing, and mental health. We also supported 450 Champions to undertake the RSPH Level 2 Award in Understanding Health Improvement to formally recognise their role in health championing, and wider bespoke development programmes including the Money Charity’s financial wellbeing training programme, and various bespoke workshops into becoming menopause champions.
To understand the value and impact of embedding Health and Wellbeing Champions across the NHS, a survey was circulated to over 3,000 Champions seeking their views on their role and their impact. Responses demonstrated that Champions are supporting the creation of local cultures of wellbeing through implementing drop-in sessions, wellbeing weeks, advocating, signposting, creating resource packs, newsletters, buddy initiatives, wellbeing groups and various other team-based wellbeing activities.
2.4. Growing OHWB impact and evidence-based practice
Growing impact and practice are core enablers within the Growing OHWB together strategy. This last year, we identified a variety of best practice in advancing OHWB services that demonstrate how it is possible to achieve the ambitions within the strategy. We have worked with partners to create research into advancing practice which includes growing our multi-professional workforce and the use of data and technology. We have also helped our OHWB professionals to better understand how they can maximise the use of data to help them to evidence the impact of their services locally.
2.4.1. Capturing, sharing, and advancing good practice
A range of resources that capture innovative work and examples of good practice have been developed to demonstrate that the ambitions within growing OHWB together are not only achievable – they are also being implemented across various settings. However, this also highlighted that our biggest challenge is how this practice is not being evenly distributed.
To support the adoption of good practice, case studies have been developed and shared on our website though mixed media designed to be simple and engaging. Wider case studies and best practice have been created and shared throughout our partnership networks, including NHS Health at Work and NHS Employers.
Appreciating the need to advance core occupational health clinical practice, we also worked collaboratively with the NHS Health at Work Network to support identifying, sharing, and advancing clinical practice through the creation of a new online best practice repository. A good practice expert reference group was established to continually review identified good practice and to provide quality assurance and clinical oversight. The online good practice OH repository is published on the NHS Health at Work website.
2.4.2. Researching growing our multi-disciplinary OHWB clinical workforce
Growing OHWB together recognises the importance of creating an integrated and multi-professional OHWB workforce, if we are to successfully realise the ambition within the strategy. However, we identified a gap in our knowledge around how wider clinical professionals and Allied Health Professionals could effectively contribute to this multi-professional family, and the obstacles hindering the future expansion of the OHWB workforce.
To address this, we collaborated with the London Centre for Work and Health to conduct research that scopes and assesses opportunities for growing a multidisciplinary OHWB clinical workforce with an emphasis on the role and utility of Allied Health Professionals from different disciplines, and other emerging clinical roles. A cross-sectional workforce survey of NHS OHWB teams was conducted to explore OHWB workplace composition, skills set, internal staff development, training, and supervision, and OHWB services delivered. A series of semi-structured focus group sessions involving OHWB leaders and other key stakeholders were undertaken along with a review of existing research studies involving training of health and non-health staff to deliver OHWB interventions and support.
Interim findings highlight a growing allied health professional workforce and novel job roles in OHWB multi-professional teams, including for example: physiotherapy, mental health and psychology, occupational therapists, OH technicians, health and safety, phlebotomy, health and wellbeing advisors, social prescribers and social workers, paramedics, vocational rehabilitation, dietetics, and ergonomics. This supports the necessity of a multi-professional OHWB team, identifying that collaborative interdisciplinary case management and care packages can add value to improving the holistic wellbeing of the workforce. Most importantly, there is appetite and enthusiasm among leaders to explore further opportunities for growing the allied health professional workforce which will assist in improving the health and wellbeing of our workforce. To enable this, we need to strengthen career pathways and talent pathways in OHWB as a multi-professional service. The final research report and recommendations will be available in summer 2023.
2.4.3. Research into growing OHWB technology and digital
Advancements in technology and digital are identified as core to enabling a good quality, future focused and data driven OHWB service, however we know that this landscape is complex and not fully realised. We undertook research into how we can maximise the use of technology and digital innovation opportunities within OHWB services by reviewing the current OHWB state, working with stakeholders to co-design a future desired state, and exploring how we can get there.
During an initial discovery phase, an analysis of the current OHWB technology ecosystem was undertaken, engagement sessions were held with 110 stakeholders and technology champions at national, regional, and local level through workshops and interviews.
This research has identified ways to maximise existing OHWB workflow and patient database systems, as well as the ways that wider digital technology can advance practice. The report is currently being finalised and will inform the future direction of travel and investment for the Growing OHWB technology improvement driver during 2023-24 and beyond.
2.4.4. Improving how we use OHWB data
Good use of data in OHWB is critical to developing needs driven and quality services, as well as demonstrating the impact, return on investment, and business cases to expand services. However, our OHWB professionals identified that they need more support in how they maximise the use of data to achieve this.
To bridge this gap, we provided a variety of training and development to our OHWB professionals in how to maximise the use of data, both day-to-day and when developing services. We have also promoted the use of the NHS Health and Wellbeing Framework diagnostic tool in undertaking a strategic needs analysis to inform local wellbeing strategy and investment in OHWB services and interventions. We also began to demonstrate how OHWB can start to develop strategic metrics and data to understand the health of the workforce, through new health and wellbeing domains within the Model Health System.
2.5. Regional perspectives
Regional teams within NHS England supported local dissemination and various programmes of work to progress the ambition within growing OHWB together locally. Collaboratively, they focused on:
- Regional communities of practice which bring together local OHWB and HROD leaders and professionals, to support them to drive improvements in OHWB locally, share practice, and offer peer support.
- Scoping OH and wellbeing services across four of the regions. This provided baseline data that is helping to inform an understanding of both OHWB workforce and services at both regional and national levels, and where to invest in next.
- Implementation of the Health and Wellbeing Framework through national workshops based on the elements of the framework, as well as supporting local organisations in using the Framework through bespoke interventions.
Specific achievements across several of our regions and their local ICSs and organisations are detailed below.
2.5.1. South East
The focus of Southeast region was socialising and raising awareness of the Growing OHWB strategy and its impact on workforce availability across all six integrated care systems. This included:
- Several events with stakeholders and people leaders across November and December 2022.
- Creating connections and collaboration to begin enabling communities of practice to work together to improve OHWB.
- Co-designed and established Southeast Menopause Network enabling menopause friendly environments across provider organisations.
A variety of good practice was identified across ICSs and regional organisations, including:
- Hampshire and Isle of Wight ICS: We embraced the Growing OHWB vision in many ways. We developed a rapid access to musculoskeletal services via self-referral or occupational health referrals. A central online people portal was created to access wellbeing information, tools and techniques which supports a large portfolio of self-help advice and guidance. A Health and Wellbeing Support Service was also developed as a confidential personal consultation support service for people who are looking for guidance related to their wellbeing. The service employed trained health advisers (fitness, coaching, mental health) to support our people and help them to reach personal solutions which work best for them.
- Dartford and Gravesend NHS Trust: Following the Growing OHWB vision of integrated multi-disciplinary services, we streamlined wellbeing by combining OH with HWB. This resulted in deeper, more rounded wellness provision and reduced sickness levels and healthier lifestyles amongst staff members. The multi-disciplinary approach afforded better outcomes for staff rather than separate OH and HWB services.
- Kent and Medway NHS and Social Care Partnership Trust: Increasing access is a core part of Growing OHWB. We delivered a ‘talking wellness’ bus service, which helped to increase opportunities for staff to increase access to services and promote staff wellbeing more generally with particular emphasis on our harder to reach groups in our community, including staff from an ethnic minority background, men, and medical staff.
- Sussex Community NHS Foundation Trust: We used the Health and Wellbeing Framework diagnostic tool to engage with staff across various team to develop initiatives linked to musculoskeletal support and coping with stress.
- Buckinghamshire, Oxfordshire and Berkshire West ICS: We delivered data driven collaboration though our Enhanced Occupational Health and Wellbeing intervention to support our people. We developed a health and wellbeing website, kindness into action programme, and rolled out restorative just culture training.
- Royal Berkshire NHS Foundation Trust: We opened the ‘The Oasis’ Staff Health and Wellbeing Campus which included environmental improvements to enable wellbeing improvements across our facilities.
2.5.2. South-West
The focus for the South West region during 2022-23 was raising awareness of the growing OHWB together strategy and creating momentum, through:
- A launch event held in November 2022, with a follow up event in March 2023.
- A review of current occupational health provision across the region to enable a better regional understanding of OH.
- Creating connections and collaboration to begin enabling local networks to work together to improve OHWB.
A variety of good practice and progress was identified across ICSs and regional organisations, including:
- University Hospitals Dorset NHS Foundation Trust: We focused on musculoskeletal related issues which resulted in 20% of the workforce being supported and great feedback around enabling people back into work.
- Gloucestershire Integrated Care System: We are reviewing OHWB at system level, including with voluntary sector and local government to identify need and gaps to develop system level provision.
- Gloucestershire Health and Care NHS Foundation Trust: We finalised our health and wellbeing strategy and are now working on the Implementation plan. The South West OH Health at Work Network group are working collaboratively to support a large South West OH contract starting in April 2023 – with lots of sharing of best practice.
- Cornwall Partnership NHS Foundation Trust: The team undertake proactive outreach to teams out in the community and use absence information as a guide to the wellbeing interventions that are needed.
- Southwestern Ambulance Service NHS Foundation Trust: The health and wellbeing team meet monthly with HR business partners to identify absence themes and then engages with specific teams to discuss and provide support. We are working with the South West Health at Work network to develop a new model of OH for the service.
- Dorset Healthcare University NHS Foundation Trust: Wellbeing and OH work proactively together and undertake physical outreach into teams. They run wellbeing sessions at team away days and support managers to develop wellbeing plans. We reached 34 community sites and plan more for next year.
- University Hospitals Bristol and Weston NHS Foundation Trust: We are proud that our ‘health check’ offer is now a substantive, collaborative offer delivered jointly by Occupational Health and Corporate Workplace Wellbeing teams.
- Royal United Hospitals Bath NHS Foundation Trust: We rolled out health checks on site for staff, initially focused on estates and facilities.
- Dorset Healthcare University NHS Foundation Trust: Improvement in relationships between OH and service leads within the trust, positive feedback.
2.5.3. Midlands
Midlands region used 2022-23 to support creating a regional strategy called ‘Be Well Midlands’, owned by all 11 integrated care system (ICS) stakeholders to improve the health and wellbeing of all healthcare employees, with 5 underpinning improvement drivers to focus on at regional and system level over the next several years. They also:
- Supported the NHS health and wellbeing framework implementation with stakeholders through collaborative workshops.
- Grew and supported a Health and Wellbeing Guardian network as the strategic voice for OHWB.
- Enhanced scoping work to fully understand all OHWB services current state, which achieved a 100% return rate and informed future local enhancement projects to promote holistic services.
A variety of good practice was also identified across their local ICSs and organisations, specifically around how tackling health inequalities and promoting flexibly working, which included:
- Leicester, Leicestershire and Rutland ICS: We implemented ‘event-in-a-box’ roadshows for colleagues working across health and care shared resources and information on relevant health and wellbeing initiatives accessible to the workforce. This removed barriers around access and provided additional capacity needed to reach front-line staff who would not normally be able to access health and wellbeing initiatives. Furthermore, an Arts and Heritage project designed for health and social care staff from ethnically diverse backgrounds consisting of uplifting and affirmative workshops as an opportunity to share their experiences of working across the system as a member of the BAME community.
- Black Country ICS: ‘SiSu’ Health Booths have been introduced as a way of reinforcing a culture that wellbeing and allowing our people quick access to available resources. The booths sit within public environments and will give immediate insights into an individual’s blood pressure, height, weight and risk factors.
- Lincolnshire ICS: We developed case studies with real life experiences of managing health and wellbeing and flexible working. We worked with Timewise at system level to promote flexibility and inclusive workplaces with a view to retaining talent, and progressed initiatives such as collaborative banks across providers and working towards Timewise Flexible Accreditation. We also developed documentation in different languages / formats which support and encourage engagement from individuals with protected characteristics.
- Coventry and Warwickshire ICS: A deep dive was undertaken into improving communication approaches about health and wellbeing offers to reach staff across the system. Our interactive Health Kiosk project helps tackle health inequalities, providing organisational level data capturing information on individuals age, sex but also on ethnicity. The information will help identify the health and wellbeing of staff across various demographics and ethnicity which will help implement wellbeing measures to take health inequalities. Furthermore, our innovative ‘Project 1000’ aims to recruit nurses and will include learning and approaches to support flexible working.
- Northamptonshire ICS: We promoted targeted health and wellbeing offers to the male workforce who are currently underrepresented. We also undertook work to better understand why they may not be accessing the service and what can be offered to increase engagement with this staff group.
- Birmingham and Solihull ICS: We targeted health and wellbeing communications to attract staff from underrepresented groups and developed a project for training and the promotion of team rostering across the system for flexible working.
- Staffordshire and Stoke on Trent ICS: We promoted resources and support available to all groups via activities of the Staff Psychological Wellbeing Hub as well as through a virtual staff wellbeing week.
2.5.4. North West
The North West supported the advancement of growing OHWB together in partnership with its local stakeholders, supported and driven by local system and organisation leaders. Work included:
- Engagement of Leaders in Health and Wellbeing: Over 5,650 staff from across the region attended various training/development offers. The North West Wellbeing Guardian Network was facilitated with bespoke sessions including, Growing OHWB Strategy, Regional Retention Strategy, Civility and Respect. Engagement with Health and Wellbeing Managers and ICB System leads on the challenges leading to co-creation of events. There was active promotion of the national health and wellbeing offers across the systems and organisations through our 2 weekly People Experience newsletters, North West NHS Futures pages, 6 weekly Community of Practices, HRD newsletters and via emails.
- Health and Wellbeing Framework Implementation: Sessions provided an overview of the Framework and best practice guidance to embed the use of the Framework to support the development of their wellbeing strategies. An evaluation and stocktake across the North West to understand how the Framework is also being used to obtain case studies and identify further support required.
- Promoting Growing OHWB strategy and delivery: A North West OH scoping exercised reviewed service provision to gain a regional baseline. An OHWB Delivery Group was established with representation from all three ICSs. This was supported by the development of an OHWB delivery plan identifying actions across regional, system and organisations. Engagement events were held with the HROD Network providing overview of the strategy and regional priorities for implementation. There was a Growing OHWB Engagement Event held on attended by 72 stakeholders, which supported the development of a regional delivery plan.
- North West HRD Network focus on holistic wellbeing: The regional HRD Network have commissioned the development of Holistic Wellbeing Guidance which underpins a shift in how the region approaches attendance. A ‘Wellbeing Community’ concept will bring together the wide variety of roles that exist within secondary care organisations to support colleague wellbeing. Activities include, identifying all roles within secondary care organisations that are part of the wellbeing community, development of a resource pack highlighting the purpose of each role, the positive impact the role can have on our colleagues, how each role can support other members of the Wellbeing Community and initiatives to support community members in their role. Embedding this approach will be taken forward through a social-movement methodology.
- Development of estates to improve wellbeing: Work was supported across various provider trusts to explore how improved estates (i.e. the environment we work in) can contribute to enhanced staff wellbeing. This created a warmer and more inviting environment for all staff, leading to an enhanced perception of wellbeing.
- Cost of living and financial wellbeing: Appreciating that financial wellbeing is an important part of a holistic employee wellbeing service, this formed a focus of support this year. Scoping with 40 leaders was undertaken to understand what various organisations do to support financial wellbeing. An Insight report was prepared to guide ways to support colleagues in need. Two cost of living sessions were run, supported by financial wellbeing resources throughout the year. Cost of Living Exchange organised and facilitated in November 2022.
2.5.5. North East
The North East region focused efforts on beginning to understand a baseline of OHWB services, health inequalities and improving attendance:
- Health inequalities and attendance: A scoping report was developed which set out to; explore and set out the links between attendance and health inequalities, set out what the evidence points to in supporting attendance, showcases what has been put in place to innovate in this area, and make recommendations and commitments to inform future investment in future years. The recommendations included:
- Create and embed a preventative health and wellbeing approach that is rooted in organisational culture to support attendance, with strategic and practical steps.
- Create insight using the Index of Multiple Deprivation (IMD) analysis to better understand workforce need.
- Develop more targeted interventions and proportionate universalistic approaches to support attendance.
- Personalise the employment experience supporting managers to do this well.
- Regional scoping: Work has begun to undertake a regional scoping of OHWB services, following the model that wider regional teams undertook. This will support understanding of baselining of service provision and inform future support/investment.
2.5.6. East of England
East of England region focused on creating a support network for OHWB professionals, and also baselining existing provision:
- OHWB leads steering group: This was formed to support OHWB leads across the region and has started to meet monthly. It enabled a space for leads to connect, share and learn from each other. ‘Growing our OHWB people’ was a specific focus area of the Growing OHWB together strategy that the group focused on.
- Regional service scoping: As part of a regional scoping to understand a baseline of OH services across the region, private sector OH providers were also engaged to understand the details of provision.
2.5.7. London
London region utilised a health and wellbeing subgroup of the regional People Board to drive the OHWB agenda. The region has focused on enabling ICS level change to create integrated and shared OHWB services and share the learning from these new models.
There has been a focus on how to best use data, and the power of the staff survey in driving change in improving employee health and wellbeing. The Health and Wellbeing Framework has been used as a tool to promote wellbeing strategy design and development.
3. Look forward: Strategic priorities for 2023-24 and beyond
We are stronger together and growing OHWB together is built upon stakeholder co-design, appreciating that we all need to contribute to make it a reality. This section outlines our strategic priorities for 2023-24 and how NHS England will support our stakeholders. They are based on extensive and ongoing engagement with national partners and experts, regions and ICS/B leaders, organisational leaders, and our OHWB multi-professional community.
A key success measure for growing OHWB together is that NHS leaders and OHWB professionals are taking ownership of and progressing the strategy in their local context. As we move into year two of the strategy, NHS England will continue to work to empower local leadership of the growing OHWB together strategy, and flexible realisation of the strategy in different local contexts. This will require continued collaboration working with our national strategic partners, support to integrated care board (ICB) and organisational leaders to own and champion the strategy locally, and ongoing development of our OHWB multi-professional workforce. It will also involve progressing the initiatives and practice from year one of the strategy, to encourage adoption, scale and spread.
For 2023-24 and beyond, this will mean our focus will likely be on, but not limited to:
Driver 1: Growing the strategic identity of OHWB
Focus area | How we will support this |
|---|---|
| 1.1. Empowering ICB and organisational leaders to advocate and take action on growing OHWB together in their local context, strategically supported by their OHWB professionals being in the driving seat for change. | Working through regional offices to support ICB leaders, Chief People Officers and Health and Wellbeing Guardians to understand growing OHWB together and what they can do to actively champion the strategy in their local context, in line with the 2023-24 NHS Priorities and Planning Guidelines. Empowering OHWB professionals to be in the ‘driving seat’ to strategically support their senior leaders in creating and advancing health and wellbeing strategy, through ongoing support and local networks / communities of practice. |
| 1.2. Working in partnership with national bodies to align resources and support. | As part of our Growing OHWB steering group, working collaboratively with national body partner organisations to align our resources and strategic messaging to support implementation of growing OHWB together. This includes support from, DHSC/DWP, SOM, FOM, CIPD, National School for OH, NHS Employers, the Health at Work Network, Council for Work and Health, and Trade Unions. |
| 1.3. Embedding OHWB within strategic performance, quality, and assurance mechanisms. |
In addition to supporting the Growing OHWB requirements within the NHS Priorities and Planning Guidelines, this will include working with strategic partners to embed the vision and ambition for OHWB service and professionals within quality, performance, and assurance mechanisms. This will include for example, continued work to integrate this into regulatory frameworks (such as continued work with the CQC to embed OHWB in their new oversight framework) and quality improvement mechanisms (such as revising the SEQOHS standards). |
Driver 2: Growing OHWB services across systems
Focus area | How we will support this |
|---|---|
| 2.1. Enabling the creation of needs driven health and wellbeing strategy across healthcare systems and organisations. |
Continued dissemination of the NHS Health and Wellbeing Framework resources to enable leaders and OHWB professionals to undertake a needs analysis of their local workforce health and wellbeing needs, turn this into local strategy to improve workforce wellbeing, and inform a resourcing plan to enhance OHWB services and offers. |
| 2.2. Supporting service development and/or good commissioning of OHWB services across local contexts. |
Sharing and further refining the new OHWB ‘directory of services’ guidance to support local leaders and OHWB professionals to develop and/or commission needs driven OHWB services. Developing our OHWB community in service improvement techniques, aligned to NHS quality and service improvement methodology, to empower them to lead local service transformation to meet local need. This will also include ongoing work to support increasing access to OHWB services for our primary care workforce and smaller healthcare organisations. |
| 2.3. Enhancing the quality of OHWB services. |
Working with FOM to ensure that the revised SEQOHS quality standards for OHWB services are representative of Growing OHWB for NHS delivered services. Supporting NHS delivered OHWB services to meet SEQOHS standards and demonstrate a good quality level of service provision. |
Driver 3: Growing our OHWB multi-professional workforce – and wider NHS leader, manager, and teams’ competence in improving health and wellbeing
Focus area | How we will support this |
|---|---|
| 3.1. Working with national partners to explore and develop a multi-professional OHWB workforce plan, spanning various sectors, and aligned to the new NHS Long Term Workforce Plan. |
Appreciating that the OHWB workforce spans across NHS, wider public and private sectors, this will require work with various national agencies to explore the development of a multi-professional OHWB workforce plan to grow our professions. This must meet the needs withing NHS Growing OHWB, as well as wider government policy as part of the recent chancellor’s budget and health is everyone’s business governmental policy. This must also be aligned to the new NHS Long Term Workforce Plan. |
| 3.2. Developing our multi-professional OHWB workforce capacity and capability, and in leadership and service improvement. | This will require ongoing development of our multi-professional OHWB workforce and will require national partnership working with other agencies as part of the Growing OHWB steering group to support this workforce development. This will include both growing clinical/professional competencies to increase capacity and capability within professional OHWB and HROD services, and also growing OHWB competency in leadership and service improvement skills to empower them to be in the driving seat of growing OHWB together. It will also include the development of new roles and development for AHPs and HROD professionals to maximise their contribution to the integrated and multi-professional OHWB team. |
| 3.3. Empowering all NHS leaders, managers, and teams to take ownership of improving their health and wellbeing and creating a localised culture of wellbeing. |
We will continue to empower leaders, managers, and teams to create local cultures of wellbeing. For leaders and managers, this will include ongoing development of the Health and Wellbeing Guardian role to act as the strategic voice of wellbeing. For wider leaders/managers, this will be through continued development and support to understand and support the health and wellbeing needs of their teams in a proactive and preventative way. We will continue to support creating wellbeing cultures at team level through ongoing guidance to support teams in improving their wellbeing together, and the role of the Health and Wellbeing Champion to encourage colleague support. |
Driver 4: Growing OHWB impact and evidence-based practice
Focus area | How we will support this |
|---|---|
| 4.1. Identifying, sharing, scaling, and spreading outstanding practice in OHWB, demonstrating that the future vision within growing OHWB together is already here in many places, and encouraging adoption. |
We will continue to work with ICBs, NHS organisations and OHWB professionals to identify, share and spread best practice in OHWB as aligned to the Growing OHWB four drivers. This will both demonstrate that the vision within Growing OHWB is becoming a reality and inspire others to adopt/adapt/scale existing practice. This can be achieved through ongoing sharing of best practice through communities of practice at national / regional levels, capturing and sharing case studies, and maximising use of engaging mixed media on our website, collaboration platforms, and bulletins to the OHWB community. |
| 4.2. Enabling OHWB leaders to better use data and metrics to demonstrate impact, return on investment, develop needs driven services, and maintain oversight of quality of services. |
We will continue to work to help OHWB professionals and our senior leaders to understand how we can use data to demonstrate the impact of OHWB and also to drive needs-driven service improvement. This will be through ongoing support and guidance into using data and metrics to manage quality day-to-day service operations, demonstrate impact and return on investment, health surveillance to align workforce wellbeing to business needs, and capturing need to evidence the case for change and service development. |
| 4.3. Translating into practice our research to understand how we advance aspects of newer areas within growing OHWB together, including enhancing OHWB digital/technology, and maximising AHPs and HROD as part of the multi-professional workforce. |
We will continue to support research into newer areas of the Growing OHWB strategy, to ensure that we fully understand these areas before advancing them with our partners. For this year, it will likely focus on implementing recommendations into research that we have started to undertake into advancing and maximising the use of OHWB digital systems and technology, and also how we maximise the contribution of AHPs and HROD colleagues as part of a multi-professional OHWB integrated team. |
Publication reference: PRN00530

