Chief executive’s overview
Welcome to NHS England’s Annual Report and Accounts for 2023/24.
This report covers the operation and performance of NHS England between April 2023 and the end of March 2024. Despite the consistent name, this is effectively a brand new organisation, bringing together the functions of the former NHS England, NHS Improvement, Health Education England and NHS Digital, with a shared purpose to lead the NHS in England to deliver high-quality services for all, and to put workforce, data, digital and technology at the heart of our vision to transform the NHS.
The benefits of bringing together these functions, providing more unified and streamlined leadership to the wider NHS, and releasing significant savings to support front line services, are clear. But it is important to say that a change programme of this size and complexity – unprecedented in the public sector – is not achieved without having a significant impact on colleagues, and I want to put on record my thanks to everyone in the new NHS England who has worked so hard over the past couple of years to make it a success.
They have done that alongside maintaining their primary focus on supporting the wider NHS to manage the significant challenges it has faced. In addition to the ongoing recovery from COVID-19 and the inflationary effects of global economic volatility, local services and systems continued to deal with the operational and financial impact from sustained periods of industrial action.
These, and other pressures, have contributed to a reality for many NHS staff that’s incredibly tough. Lord Ara Darzi’s assessment of the NHS paints a deeply sobering picture of the current performance challenges NHS teams are managing day-to-day across the country. As we all recognise, many people’s experiences of the NHS are a long way from where any of us want them to be.
On average, around 1.6 million people have some kind of contact with NHS services every day. Most will get what they need and have a good experience. But we all recognise what Lord Darzi says in his review of the NHS: that too many people are currently waiting too long for planned appointments, scans and operations; A&Es are too often overcrowded, meaning that patients wait too long to complete their care, or for ambulances to arrive; too many people still find it difficult to get appointments with general practice, community and mental health services; and the quality and safety of care (for example, in maternity and mental health) can too often fall short of what is expected, and sometimes fall short of what is acceptable.
We now have a definitive diagnosis, so it is time for the NHS and Government to work together on the prescription.
In setting out his conclusions, Lord Darzi is unequivocal that the current NHS model is the right one. He is clear ‘a top-down reorganisation’ is ‘neither necessary nor desirable’, and our structures are the right ones to deliver the changes and improvements we all want to see.
Most importantly of all, Lord Darzi shares our hope for the future, in the quality and values of NHS staff, and the ability they have shown time and again to turn things around. Indeed, he shares our view that many of the solutions are already out there, working in parts of the NHS today.
It will take time for the NHS to recover fully from the pandemic and to become a service fit for future generations. That’s why the work that comes next – to develop a 10-year health plan – is so important.
In this we must address the honest assessment of Lord Darzi and the immediate risks to our delivery, including those outlines in this report – a lack of capacity to cope with demand and risks to cyber security.
And in looking to the future, we should continue to learn from what NHS have already achieved in tough circumstances.
Over the last year, due to the hard work and commitment of NHS staff, progress has been made on almost all the ambitions set out in the 2023/24 Planning Guidance, albeit there is still a very long way to go. Record numbers of people were supported by mental health services. Millions more general practice appointments were delivered, alongside the launch of Pharmacy First and a plan to help improve dental access.
Hospitals delivered around a million more elective treatments, and long waits were dramatically reduced, supported by the growing number of surgical hubs, and greater use of the independent sector, now delivering one in ten of every treatments.
Patients received almost two million more diagnostic tests, supported by our growing network of Community Diagnostic Centres, and more than ever before were seen for urgent cancer checks, supported by innovations such as lung scanning trucks, direct referrals from community pharmacy, FIT testing and cytosponges.
And a corner was turned on urgent and emergency care, with 999 and A&E performance improving thanks to the work of local teams to put more ambulances on the road, open more core beds, and extend out of hospital care.
The above are just some of the achievements which give hope, but not complacency. For all the progress we can point to, we all know we could still do far more, far better, for our patients.
As ever, central to delivering these ambitions will be the effort of NHS staff – whether frontline clinicians, or those who work to support them and our patients. While we have seen an expansion in the NHS workforce in recent years, it is against a backdrop of over a hundred thousand vacancies and colleagues in many services and parts of the country feeling stretched, an over-reliance on overseas-trained clinicians and agency staff, and a future in which baked-in demographic changes place ever growing demand on services.
However, in the NHS Long Term Workforce Plan, published in June 2023, we do now – for the first time – have a credible strategy to put staffing on a sustainable footing for the future, and crucially to better support those who work in the health service, so that they in turn can do their best for our patients.
So while I want to once again thank all of my NHS colleagues for their ongoing hard work and dedication, and praise them for the achievements they were able to deliver in 2023/24 in spite of the massive challenges they were up against, more importantly I want to take this further opportunity to restate the commitment we made in the milestone Long Term Workforce Plan to improving culture, leadership and wellbeing – and to making the NHS a better place to work, to build a career, and vitally for everyone to contribute to better health and care for the communities they serve.
Amanda Pritchard, NHS England Chief Executive and Accounting Officer
4 October 2024
Performance overview
About NHS England
We share, with the Secretary of State for Health and Social Care, the legal duty to promote a comprehensive health service in England, in accordance with the National Health Service Act 2006 (as amended by the Health and Social Care Act 2012 and the Health and Care Act 2022).
Our purpose is to lead the NHS in England to deliver high quality services for all and to deliver value to the taxpayer. We set the national direction, allocate resources, ensure accountability, and define the national strategy for supporting and developing people, making the NHS a great place to work.
We run national IT systems and the collection, analysis, publication, and dissemination of data generated by health and social care services to improve outcomes for our patients and communities.
On 1 April 2023, NHS England incorporated Health Education England, the body responsible for the education and training of the health workforce. This completed the formation of the new NHS England which also merged with NHS Digital on 1 February 2023.
How we operate
NHS England is governed by a Board which is accountable to the Government, Parliament, and the public.
Our work is also supported by third party organisations including NHS Business Services Authority (NHS BSA), NHS Shared Business Services (NHS SBS), NHS Property Services Limited (NHS PS) and Primary Care Support England provided by Capita. Additionally, NHS England hosts NHS Interim Management and Support and sponsors the Sustainability Unit on behalf of the NHS.
We also oversee commissioning support units (CSUs). The CSU staff group are employed by NHS BSA but are formally a part of NHS England. CSU activities are included in our report and accounts except where otherwise indicated.
SCCL is the legal entity through which NHS Supply Chain undertakes its procurement services and transacts with customers and suppliers. This is achieved by leveraging the collective buying power of the NHS to support the healthcare system to achieve their financial, operational, and strategic objectives. NHS England is the sole shareholder of SCCL, a UK incorporated company. SCCL’s Articles of Association include a range of matters reserved for shareholder decision.
Most services are commissioned by integrated care boards (ICBs), which are overseen by NHS England. ICBs lead 42 local integrated care systems (ICSs) made up of NHS organisations, primary care professionals, local councils, social care providers and the community, voluntary and social enterprise sector.
Our NHS England Operating Framework sets out how we are supporting systems and providers to lead locally to improve the health of the population, improve the quality of patient care, tackle health inequalities and deliver care more efficiently. It also describes our six longer-term aims:
- longer healthy life expectancy
- excellent quality, safety and outcomes
- excellent access and experience
- equity of healthy life expectancy, quality, safety, outcomes, access and experience
- value for taxpayers’ money
- support to society, the economy and environment
How we measure performance
The NHS Constitution sets out the rights of patients, the public and staff. We measure and monitor performance against a wide range of constitutional performance standards and publish statistics relating to these core constitutional standards on the NHS England website every month.
ICB performance
Legislation requires an annual assessment of performance to be carried out at ICB level.
NHS England has published guidance on the 2023/24 annual assessment process which includes detail on the evidence to inform assessments and the Key Lines of Enquiry that were considered. We will publish a summary of the outcomes of these assessments on our website later in 2024.
In line with the principles of the oversight framework, all ICBs have been allocated into one of four support segments ranging from no specific support needs (segment one) to a need for mandated national support via the Recovery Support Programme (segment four). At the end of the 2023/24 financial year, we saw a slight increase in the number of ICBs in segments three or four; 27 organisations compared with 25 at the end of 2022/23. Two ICBs, Lincolnshire and Norfolk, were successfully supported out of the Recovery Support Programme this year and one ICB, NHS Hampshire and Isle of Wight ICB, entered the programme.
NHS England may use its statutory enforcement powers, including the power to issue directions, where an ICB is failing, or is at risk of failing, to discharge any of its functions. During 2023/24 no directions were given, but NHS England accepted enforcement undertakings from one NHS Hampshire and Isle of Wight ICB. A copy of these undertakings is publicly available on the NHS England website.
ICB annual reports
2023/24 ICB annual reports and accounts were published on their individual websites, links to these can be found on our website.
Provider annual reports
All NHS trusts and NHS foundation trusts (termed ‘providers’) in England publish an annual report and accounts on their individual websites. The results of all providers will be published by NHS England in Consolidated Provider Accounts, by November 2024. These are presented separately from those of NHS England as NHS England is not the parent body of NHS trusts and NHS foundation trusts.
Overview of 2023/24 operational performance
This performance overview provides a summary of NHS England’s performance against its objectives, set by the Government through the mandate and cascaded to the NHS through Operational Planning Guidance,
NHS England began 2023/2024 managing significant pressures. Industrial Action had already led to hundreds of thousands of appointments and operations being rescheduled and it was clear that ongoing action would present significant challenges to the service throughout the year. Alongside this, we were continuing to respond to the build-up of health needs during the pandemic, ongoing high levels of COVID-19 infection, capacity constraints in social care and increased costs due to inflation.
The 2023/24 operational planning guidance outlined three key tasks for the NHS:
- recover our core services and productivity
- make progress in delivering the key ambitions in the NHS Long Term Plan
- continue transforming the NHS for the future
Improvement has been made against the objectives we set. However, performance remains significantly challenged across priority areas, particularly against constitutional performance standards.
In general practice we have again made more appointments available for patients: almost 371 million appointments took place in the 12 months to the end of March 2024, 6.7 % higher than 2022/23. We have continued to grow the Primary Care workforce and 98% of pharmacies have signed up to Pharmacy First since its launch in January 2024.
As part of our Urgent and Emergency Care Recovery Plan we have expanded capacity and the ambition to deliver an additional 5,000 hospital beds was met from January 2024; 600 new ambulances have also been provided alongside a 7.3% growth in the ambulance workforce.
Category 2 ambulance response times were under 34 minutes in March 2023, a reduction of over 13 minutes over the year; 4-hour A&E performance improved for the first time since 2009 (outside the first year of the COVID-19 pandemic) by 2.7% to 74.2% by March 2024. Although progress was made, we note that performance remains below the constitutional standard of at least 95% of patients being admitted, transferred, or discharged within four hours.
Despite the ongoing impact of Industrial Action, we have treated more elective patients during 2023/24, 17.4 million elective pathways were completed – an increase of 1.3 million compared to 2022/23.
Urgent suspected cancer referrals have continued to increase during the year and hit a record high in March 2024, when they were 33% higher than before the pandemic. To meet this demand, treatment activity has also been at its highest level: 340,000 patients received their first treatment for cancer between April 2023 and March 2024 compared to 2022/23.
Despite these record levels of demand for cancer care, the NHS delivered and exceeded on its 2023/24 target to ensure at least 75% of patients received a definitive diagnosis within 28 days of referral. The backlog of patients waiting over 62 days was also reduced. The percentage of patients waiting no longer than 2 months for their first cancer treatment improved from 64.9% in April 2023 to 68.7% in March 2024, however, this remains below the 85% constitutional standard.
In mental health, more people are getting the support they need, with over 5 million people in contact with NHS services for their mental health, autism and or learning / disability, an increase of nearly 300,000 compared to 2022/23.
We have delivered growth in the maternity workforce to better support women and families; the number of midwives has risen by 6.2% to a record high alongside an improved retention rate.
Performance analysis
In this section, we provide detail on the work we have delivered during the year. These key areas of performance relate closely to the objectives set out in our annual business plan and reflect progress made against the aims set out in the Government’s mandate to the NHS.
For more detail on how we delivered against the mandate, see appendix 1.
Primary and community health services
As the NHS came out of the emergency phase of the COVID-19 pandemic, demand for GP services has grown and public satisfaction with access, as measured by the GP annual survey, has declined. The survey* showed 67% of patients had a positive experience of contacting their GP, set against 33% neutral or negative.
*The publication of 2024 survey results marks the start of a new time series for GP Patient Survey, therefore trend data for previous years of the survey is not presented alongside the 2024 results as it would normally be, and the 2024 results are not comparable with previous years.
General Practice expanded capacity to meet the rising demand for care, with 370.7 million appointments taking place in the 12 months to the end of March 2024, including 7.1 million COVID-19 vaccinations. This is 22.1% more than the 2018/19 baseline and 6.7% higher than the 12 months to March 2023. The March 2024 target of an additional 50 million appointments was met in October 2023.
Appointments in general practice
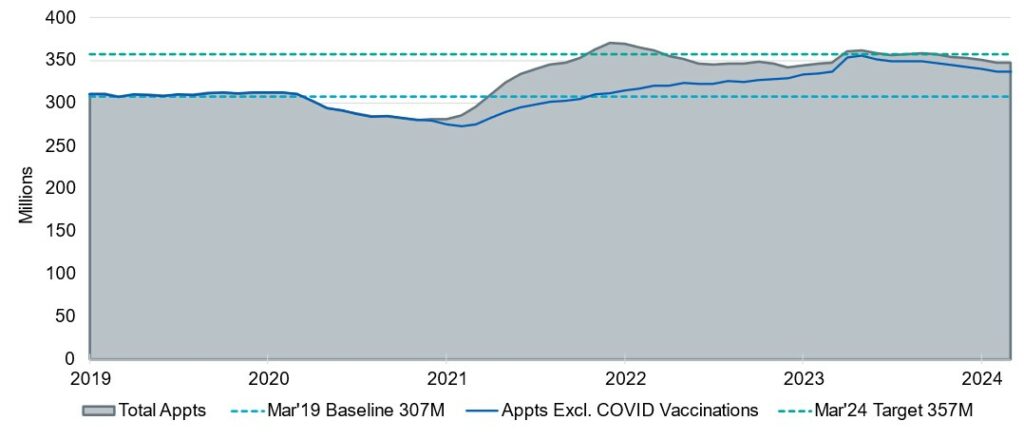
The increase in appointments has been supported by investment in extra staff, with more than 47,843 (December 2023) whole time equivalent (WTE) direct patient care staff in place.
This has been achieved and exceeded the Additional Roles Reimbursement Scheme, in with the Government commitment to deliver 26,000 additional roles in primary care by March 2024. This includes an additional 2,709 WTE doctors in general practice at the end of March 2024 compared to the March 2019 baseline.
By March 2024, we had supported 94% of GP practices to switch to digital telephony, helping to reduce the number of people struggling to contact their practice at 8am.
We also supported over 2,500 GP practices with adopting the Register with a GP Surgery digital service, which enables new patients to register at their preferred surgery online and through the NHS App. At year end, over 20% of all GP registrations were completed using this service, with over a million registration requests processed digitally.
To support access to GP data in wider care settings, we continue to develop technology to allow authorised health and social care workers to access their patients’ GP records. As of March 2024, NHS 111 providers and many care homes can now access GP records through their own provider systems and 90% of GP Practices have enabled functionality to structure GP records data. This gives provider systems even more control over how GP data is presented and used on their own systems.
Community pharmacy
Pharmacy First was officially launched on 31 January 2024. Uptake has been faster and broader than planned, with 98% of pharmacies now signed up. This has been supported by a public campaign to increase patient awareness of the service.
Community Pharmacy Contraception Service and Community Pharmacy Blood Pressure Check services were successfully expanded in December 2023, making it easier for patients to access treatment for common conditions through their local pharmacy.
Dentistry and optometry
Primary care dental services continue to recover from the disruption caused by the COVID-19 pandemic following the lifting of infection prevention control constraints in July 2022, with 82% of contracted units of dental activity delivered in 2023/24. This represents an increase in activity of 2% compared to 2022/23, although remains 10% below pre-pandemic levels. Building on the contract changes announced last year, NHS England published guidance for ICBs on the flexibilities available to them within the current contract to support improved delivery.
The Dental Recovery Plan was published on 7 February 2024, the aim to enable up to 2.5 million additional NHS dental appointments for patients over the next 12 months, including delivery of up to 1.5 million extra treatments. The plan’s three core components are: expanding access; a major new focus on prevention for young children; and developing and increasing capacity of the dental workforce.
Optometry services exceeded pre-COVID-19 activity levels in high street practices. Over 13.7 million sight tests have been delivered, at high street opticians and at home, marking an increase of 7% against the previous year. Over 4 million optical vouchers were redeemed in 2023/24, an increase of 13.7% from the previous year.
Personalised care
We have more than doubled our NHS Long Term Plan commitment, with 5 million people receiving personalised care a year ahead of the target. 10.8 million people have benefitted from a personalised care intervention as of March 2024, supporting patients and giving them more control in managing their long-term conditions.
Urgent community response
UCR teams continued to provide urgent care to people in their homes, avoiding unnecessary hospital admission. More than 83% of patients were seen within 2 hours of referral to UCR in March 2024, exceeding the national expectation of 70%.
Self-referral
Enabling individuals to self-refer into community services rather than having to visit a GP has reduced pressure on general practice. ICSs expanded self-referral routes into community services pathways against a target of 45,000 self-referrals by March 2024, announced in PCARP. This target was achieved one month early, with 57,477 self-referrals in February 2024.
Urgent and emergency care
In January 2023, we published the Delivery plan for recovering UEC services to reduce waiting times in emergency departments and for ambulances. Progress was made by the end of March 2024 against a backdrop of industrial action and an increase in attendances.
4-hour A&E performance was 74.2% (A&E attendances and emergency admissions March 2024 statistical commentary) compared to 71.5% in March 2023*, falling short of the year-end target of 76%, that is still significantly below the 95% constitutional standard.
*No performance data was collected during the period May 2019 to May 2023 for those trusts participating in the UEC Clinical Review of Standards, however the NHS still reported an improvement on last year when accounting for CRS Trial Sites.
The mean category 2 ambulance response time for 2023/24 was 00:36:23, a reduction of 13 minutes and 37 seconds (Statistical note: ambulance quality indicators (AQI)) over the year. Additionally, around 600 new ambulances (double crewed ambulances and mental health response vehicles) were delivered in 2023/24, with the remaining 200 of the 800 commitment to be delivered by end of September 2024. Further to the increases in new ambulances and a 7.3% growth in the ambulance workforce, all 11 ambulance trusts have intelligent, live, digital call-routing systems supporting reductions in long waits for calls.
Average daily A&E attendances for 2023/24 were 71,720, a 3.3% increase on 69,449 in 2022/23 and emergency admissions on 31 March 2024, increased by 6.4% from 1 April 2023.
This improvement was achieved by:
- delivering the target of 5,000 new core (general and acute) beds, in January 2024
- 11,833 new virtual ward beds by March 2024, compared to 9,713 in July 2023. Occupancy also increased to 72% from 64.1% in the same period
- investment to increase ambulance hours on the road by 4%
- 84% of hospitals with type 1 emergency departments now provide same day emergency care seven days a week, with opening hours of a minimum of 12 hours per day.
Improvements in access to 111 services
NHS 111 which received 21.8 million calls in 2023/24 compared to 22.3 million calls in 2022/23, a drop of 2.3%. However, the volume of answered calls increased by 9.1% from 17.1 million to 18.7 million calls. Call abandonment improved to 10.0% in 2023/24 (against 17.6% in 2022/23) and in March 2024 the average call answer time was 00:03:16 down from 5 minutes and 34 seconds in March 2023.
The 111 online service has undergone continuous developments to improve access, accessibility, and user experience. In October 2023, access to 111 online was expanded to all users of the NHS App, further alleviating pressure on telephone-based services, and providing an alternative to the NHS 111 phone service for urgent medical needs. An average of 30% of all 111 activity (across telephony and online) is via 111.nhs.uk, with assessments via the NHS App tripling last year, with more direct digital access to urgent mental health services for patients.
Elective care
Elective care was significantly disrupted by industrial action. An estimated 1.3 million elective attendances/appointments (a combination of inpatient and outpatient rescheduled activity) were cancelled, and many hours were lost due to the disruption. As a result, although the NHS did more activity, with demand high, we did not achieve the goal to virtually eliminate 65 week waits, though they were cut by 48% from 94,400 to 49,000, per our constitutional standard.
During 2023/24, 17.4 million elective pathways were completed from referral to treatment, including more than 3.7 million patient pathways that would otherwise have exceeded 65 weeks within this period. As shown in the following table, progress was also made on reducing the number of patients waiting longer than 18 months (78 weeks) for treatment.
Number of patients waiting longer than 18 months
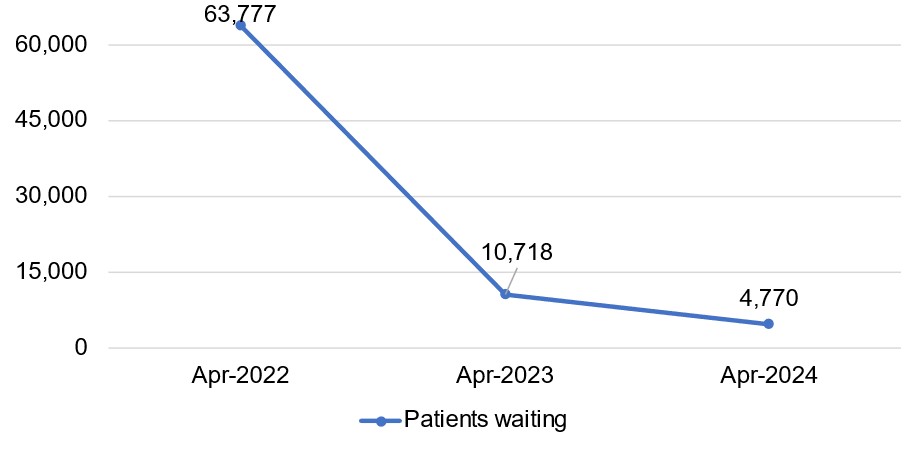
To help patients make choices at the point of referral we improved the information made available to referrers and patients, such as information about waiting times, distance to travel and quality of care. To improve patient choice for those already on an elective pathway, nearly 400,000 patients were proactively offered choice to move provider if they had been waiting over 40 weeks for care and met the relevant criteria.
2023/24 was the second year of the £1.5 billion Targeted Investment Fund (TIF) 2 capital funding agreed at Spending Review 2021, ringfenced to increase elective activity. £509 million was drawn down against a target spend of £600 million, and 23 TIF schemes were completed.
The NHS Constitution sets out that patients should wait no longer than 18 weeks from GP referral to treatment. As of March 2024, referral to treatment 18 weeks performance stood at 57.2%, significantly below the 92% standard.
Mental health
Around 5 million people now contact NHS services for support with their mental health each year, an increase of 0.7 million more than 2018/19.
In 2023/24 the NHS took further steps to improve services, address the long-standing treatment gap and respond to pressures from increased prevalence and demand for mental health services, including:
- during 2023/24, 788,108 Children and Young People aged 0 to 17 received at least one contact from an NHS funded mental health service (94% of the 840,254 target). This is an increase of around 79,000 against the previous year.
- the number of 18- to 24-year-olds having at least one contact with NHS funded mental health services – excluding NHS Talking Therapies – in the rolling 12 months to March 2024 was 234,255, exceeding the NHS Long Term Plan goal of increasing access by 18,000 for 18 to 24 year olds by around 5,000
- Mental Health Support Teams (MHSTs) continue to improve access to mental health services for children. MHSTs now cover 44% of pupils and learners as of Spring 2024
- in 2023/24, 425,625 adults and older adults with severe mental illness received 2 or more contacts, exceeding the target by 15%
- over £500 million was secured for a multi-year capital programme to replace dormitories in the mental health estate with single, ensuite bedrooms. Since the programme started in 2020/21, 43 projects have been completed, eradicating roughly 700 dormitory beds to date, allowing services to provide more therapeutic arrangements for people in inpatient units.
- £150 million of capital investment has been secured for projects to support the mental health UEC Care Pathway. This will fund over 200 schemes, 170 of which will be completed by winter 2024. The schemes include funding for crisis alternatives, making improvements to health-based places of safety, and mental health ambulances, and are expected to improve patient experience and outcomes, as well as reduce pathway pressures
- 58,303 women were reported to have accessed specialist community Perinatal Mental Health (PMH) services and Maternal Mental Health Services (MMHS) in the 12 months to end of March 2024. This is an increase of 7,668 from last year (50,635 in March 2023)
- the NHS Long Term Plan ambition to open 15 specialist gambling clinics by the end of 2023/24 was achieved, providing the capacity to treat 3,000 patients per year across the country
The sector has worked hard to make significant progress in a challenging context. However, there continues to be high demand for services. As a result, a number of areas remain challenged, and work continues with regions and systems to prioritise recovery.
NHS England continues to explore opportunities to improve prevention and early intervention approaches to improve outcomes for Children and Young People with eating disorders. Despite continued growth in demand, services are treating 55% more Children and Young People since the start of the COVID-19 pandemic. By March 2024, 79.1% of routine referrals were seen within 4 weeks and 73.3% of urgent referrals were seen within 1 week, against a 95% standard.
NHS Talking Therapies referral to treatment and recovery standards continued to be met. In the 12 months to March 2024, NHS Talking Therapies services delivered access for 1.26 million people. This is an increase of 41,377 against 2022/23, however a smaller proportion of those completing talking therapies had recovered (50.9% in March 2024 against 51.2% previous year).
The Dementia Diagnosis Rate for March 2024 was 64.8% (63.0% 2022/23), falling short of the national ambition of 66.7%, which has not been achieved since March 2020. However, there has been an upward trend since January 2023, and we anticipate the ambition will be met by March 2025.
Significant progress has been made in expanding the workforce to support mental health service expansions; the NHS secondary care mental health workforce has increased by 32% (around 36,300 WTE) since March 2019, compared to 20% for the NHS secondary care workforce overall (data to December 2023 from NHS Workforce Statistics). Children and Young People Mental Health services staff grew by over 45% between the 2019 and 2022 surveys, though at 16% the vacancy rate for mental health nurses remains high.
Mental health spend
The table below shows that mental health spend*, as a proportion of total recurrent NHS spend that mental health spend, recurrent NHS Mandate funding, and the proportion of recurrent NHS spending on mental health, increased between 2022/23 and 2023/24.
*In this table mental health spend includes: i) ICBs mental health spend from their programme allocations, except for spend on Prescribing and Continuing Healthcare (CHC) as expenditure in these areas were not areas identified within the Long Term Plan for increased investment. NHS England requires ICBs to increase mental health spend from their programme allocations by at least as much as programme allocations grow each year: this is known as the Mental Health Investment Standard. All 42 ICBs met the Mental Health Investment Standard in 2023/24; iii) national transformation funding (known as Service Development Funding) primarily issued to ICBs for new services or used to train new staff for mental health services iii) expenditure on specialised commissioning related to mental health, spent by NHS England. The recurrent NHS baseline shows the element of NHS England’s funding which is agreed to continue year-on-year for service provision. It excludes single-year or short term additions to NHS England’s funding (e.g. to fund a particular Government initiative) and the additional pensions costs for NHS staff which are met centrally.
| 2022/23 £bn | 2023/24 £bn | |
| Mental Health Spend | 12.6 | 13.9 |
| Recurrent NHS baseline | 142.4 | 154.7 |
| Mental Health Spend as a proportion of recurrent NHS baseline | 8.9% | 9.0% |
The recurrent NHS baseline shows the element of NHS England’s funding which is agreed to continue year-on-year for service provision. It excludes single-year or short-term additions to NHS England’s funding (e.g. to fund a particular Government initiative) and the additional pensions costs for NHS staff which are met centrally.
People with a learning disability and autistic people
The number of people on a learning disability register increased by more than 21,000 by the end of 2023/24.
By 31 March 2024, 255,145 people (77.6% of the eligible population) had received an annual health check, exceeding the 75% national commitment. 75% also had an accompanying health action plan, compared with 64% in February 2023.
At the end of February 2023, an autism health check was piloted in four regions to gather learning from the pilots, and, in April 2023, we published a national framework to support improved outcomes in all-age autism assessment pathways.
The Learning from the Lives and Deaths of People with a Learning Disability and Autistic People (LeDeR) programme supported improvements in health outcomes.
The latest data (2022) showed a narrowing of health inequalities, with the median age of death for people with a learning disability increasing by one year. For the first time, the annual LeDeR report included findings about autistic people.
An Information Standard Notice published September 2023 mandates the use of a Reasonable Adjustment Digital Flag in health records from April 2024 to show that a disabled person needs a reasonable adjustment to their care.
At the end of March 2024, there was a significant reduction (of 60% since 2015) in the number of people with a learning disability (who are not autistic) in a mental health hospital. However, the number of autistic people (with no learning disability) in a mental health hospital had increased by 66% since 2017.
National investment of £121 million in 2023/24 supported the delivery of learning disability and autism services, including care education and treatment reviews, community infrastructure and key workers. Keyworker services for autistic Children and Young People at risk of admission to, or in a mental health hospital are now operational in all ICB areas. By the end of 2023/24 keyworkers had supported over 2,600 Children and Young People and our housing capital of £13 million continued to support people with a learning disability and autistic people to leave a mental health hospital.
Health inequalities and prevention of ill-health
The NHS Prevention Programme delivers targeted work to tackle risk factors and their underlying causes, subsequently helping to reduce health disparities and narrow inequalities.
In 2023/24 more than 120,000 people have been referred to the NHS Digital Weight Management Programme.
At the end of 2023/24, 85% of all eligible inpatient and 94% of all maternity services had implemented new tobacco dependence treatment services. The proportion of women who were known to be smokers at the time of delivery was 7.4% in 2023/24, the lowest level on record, but above the current national ambition of 6% or less (Statistics on Women’s Smoking Status at Time of Delivery: England, Quarter 4, 2023/24 – NHS England Digital). Additionally, all 47 patient-facing alcohol care teams funded through the NHS Long Term Plan have delivered increased staffing levels, with 36 achieving optimal staffing rates by the end of December 2023.
Please see Appendix 3: Reducing health inequalities, for more detail on our work to reduce healthcare inequalities in 2023/24.
NHS Diabetes Prevention Programme
Primary care referrals into the NHS Diabetes Prevention Programme reached 1.5 million in 2023/24, with just under 600,000 people joining. The ambition of supporting 120,000 people on the programme in 2023/24 was exceeded by almost 40,000 and an independent evaluation has shown a 37% relative reduction in incidence of those who complete the programme and a 7% reduction in population-level incidence of type 2 diabetes.
NHS Type 2 Diabetes Path to Remission Programme
The NHS Type 2 Diabetes Path to Remission Programme is now available across the whole of England. To date over 20,600 referrals have been made. Early data indicates participants each lose 7.2kg (over one stone) on average after one month, and 13.4kg (over two stone) after three months. This is in line with the outcomes seen in the trials where participants were able to improve their diabetes control, reduce diabetes-related medication and, in around 50% of cases, put their type 2 diabetes into remission.
Non-cancer screening
As at quarter 2 2023/24 national uptake in the NHS Diabetic Eye Screening Programme was at 79.1% and performance has continued above the acceptable target of 75%.
The rates of the NHS abdominal aortic aneurysm (AAA) screening for men living in our most deprived areas continues to improve year on year, particularly since the introduction of inequalities standards for the programme and local interventions.
NHS vaccinations and public seasonal flu programmes
Flu vaccination deployment
18.3 million children and adults received a flu vaccine in 2023/24 with improvements in uptake seen across several cohorts, notably 2- and 3-year-olds and those in long-stay care homes. There was an increase in the levels of co-administration of flu and COVID-19 vaccines, with 35% of adults receiving both at the same time.
COVID-19 vaccination deployment
As of 31 March 2024, the NHS had administered more than 157 million COVID-19 vaccinations in England, with 11.8 million vaccinations given in autumn 2023. The COVID-19 spring 2024 campaign focused on reducing inequalities, improving uptake and co-administration with Shingles where clinically appropriate.
Mpox vaccination deployment
On 10 November 2023, JCVI recommended an ongoing routine vaccination strategy for protection against MPOX to prevent future outbreaks and protect those at risk of exposure.
Polio vaccination
London region has focussed efforts on improving uptake of polio vaccination in high-risk areas to help to reduce risk of outbreak. The risk of outbreak in London has now been reduced and, as no further poliovirus type 2 isolates have been detected for at least a year. World Health Organisation polio status has been reinstated in England.
Maternity and neonatal services
Our national maternity safety ambitions are to reduce the rates of stillbirth, neonatal mortality, maternal mortality, and intrapartum brain injury. Although latest data shows that we are making progress in reducing stillbirth and neonatal mortality, there was a statistically significant rise in maternal mortality for the last triennia (Maternal mortality 2020-2022 | MBRRACE-UK | NPEU).
The Three-Year Delivery Plan, published in March 2023, sets out the steps to meet our objectives and improve outcomes. It includes learning from independent reports into maternity and neonatal services in Shrewsbury and Telford, and East Kent.
A key objective is to grow the maternity workforce so it can better support women and their families. With national and local investment, the number of midwives has risen by 6.2% in the past year to a record high of 23,689 WTE and the number of consultant obstetricians has risen by 5.1% to 1,861 WTE. In 2023/24 we invested to help improve midwife and in March 2024 the leaver rate was 9.9% compared to 11.4% a year before.
Leadership teams from all 150 maternity and neonatal units in England have now started the Perinatal Culture and Leadership Programme, which includes a diagnostic survey and practical support to nurture a positive safety culture.
We have published Maternity and Neonatal Voices Partnerships guidance for trusts and systems to support the embedding of service user voice in improvement work and, to address unwarranted variation in experience, in December 2023, we published What good looks like guidance for the GP maternal postnatal check. Both provide clear, national advice on the delivery of safer, more equitable, more personalised care.
Coverage for the three antenatal screening programmes remained above the achievable thresholds:
- fetal anomaly screening coverage 98.5% at June 2023
- infectious diseases in pregnancy screening for HIV, Hepatitis B and Syphilis at 99.8% at September 2023
- sickle cell and thalassaemia screening coverage at 99.8% at September 2023
September 2023 performance of the three newborn screening programmes’ coverage remained above acceptable thresholds:
- newborn blood spot screening coverage at birth at 97.5%
- newborn hearing screening coverage at 99.1%
- newborn and infant physical examination screening coverage at 96.3%
The in-service evaluation (ISE) for Severe Combined Immuno-Deficiency (SCID) has ended its formal stage. Screening for SCID continues with the same cohort whilst the UK National Screening Committee (UKNSC) awaits and considers the final report.
The ISE for non-invasive prenatal testing rollout within the NHS Fetal Anomaly Screening Programme will end at the end of May 2024. Screening will continue whilst the UKNSC reviews the interim and final report.
Cancer
NHS England has also continued to implement its cancer early diagnosis strategy, contributing to record levels of urgent cancer referrals, with over 3 million referrals seen between April 2023 and March 2024.
The NHS delivered and exceeded its cancer targets by the end of March 2024:
- 3% of people received a definitive diagnosis or ruling out of cancer within 28 days of an urgent referral, against a target of 75%
- the backlog of patients waiting longer than 62 days was at the lowest since April 2020, a reduction of almost 20,000 patients since the post-pandemic peak.
This progress was achieved through new investment in expanding diagnostic capacity, working more closely with the most challenged trusts to provide them with additional support and challenge, and improving the productivity of the more challenged pathways, including:
- increasing the use of faecal immunochemical tests (FIT) in people with symptoms that could be bowel cancer, to help target endoscopy capacity on those who need it most
- expanding tele-dermatology in the skin cancer pathway.
As a result of these strategies, we are diagnosing more people – and a higher proportion of cancers at an early stage than before the COVID-19 pandemic. By March 2024, early diagnosis rates were 2.4% points above the 2019/20 pre-pandemic level and 0.8 percentage points higher than the previous year (based on Rapid Cancer Registration Data). The all-cancer early diagnosis rates have increased across all deprivation quintiles, with the overall gap between the most and the least deprived narrowing compared to pre-pandemic rates (COVID-19 rapid cancer registration and treatment data). The Rapid Cancer Registration Dataset shows that people from disadvantaged areas are now most likely to be diagnosed with lung cancer early.
Cervical Screening Programme
The NHS Cervical Screening Programme helps save around 5,000 lives each year. In November 2023, NHS England set out the ambition to eliminate cervical cancer by 2040.
Screening uses a highly effective test to check for high-risk Human Papillomavirus, which is found in over 99% of all cervical cancers and which may cause abnormal cells to develop in the cervix. These abnormal cells can, over time, turn into cancer if left untreated. 2023/24 data shows that for the higher age cohort (age 50 to 64), coverage is just marginally under the 75% efficiency standard at 74.8%. For the younger cohort (age 25 to 49) it remains lower at 66.6%. The optimal performance standard is 80%.
Bowel cancer screening
The NHS bowel cancer screening programme exceeded the optimal coverage standard of 60%, with latest performance measured at 71.8% at the end of September 2023.
As part of the ongoing extension of FIT kits to all over 50s, the programme started to rollout the kit to people aged 54 in 2023/24. This phase of the age extension will result in around 800,000 more people being eligible for bowel cancer screening each year.
The NHS Bowel Cancer Screening Programme has worked in partnership with the Royal National Institute for the Blind, the Thomas Pocklington Trust and FIT kit supplier Mast Group Ltd to develop a FIT aid to help blind and partially sighted people complete their bowel cancer screening test independently. During 2023/24, in a world first, the NHS started to offer routine preventative bowel cancer screening to thousands of people with Lynch syndrome – a genetic condition which increases risk of developing certain cancers.
Breast cancer screening
In 2023/24, we refined the breast and gynaecological cancer pathways to ensure women with low-risk symptoms, which are unlikely to be cancer, are rapidly directed towards the most appropriate care.
The NHS Breast Screening Programme invitation backlog, affected by the COVID-19 pandemic, was resolved in September 2023 when 97.7% (Q2 (1 July to 30 September 2023) ANNB and YPA screening KPI data – GOV.UK) of women invited were screened within the required 3-year interval. December 2023 performance exceeded the 70% efficiency standard with 70.2% coverage (80% optimal target).
The Breast Cancer Testing programme invited members of the Jewish community, who are more likely to have a genetic mutation which increases the risk of cancer, for screening. The programme has received more than 19,000 registrations so far and has already identified over 100 people with the breast cancer mutation.
Liver health checks
The Community Liver Health Checks programme, which is reducing health inequalities by offering mobile services to those most at risk, delivered more than 36,500 scans and identified more than 2,600 people at increased risk of liver cancer.
Lung health check
By the end of March 2024, the Targeted Lung Health Check programme had invited more than 1.4 million current or former smokers from some of the most disadvantaged areas in the country. Nearly 4,000 people were diagnosed with lung cancer, 75% at stage 1 or 2, compared with the with the overall lung early diagnosis rate of 30% in the 12 months pre-pandemic.
Early diagnosis rates for the most deprived quintile have increased the most from pre pandemic levels (9 percentage points).
Workforce training and education
In July 2023 we published the first comprehensive workforce plan for the NHS, to put NHS staffing on a sustainable footing and to improve patient care.
Our priority for 2023/24 was to start implementing the NHS Long Term Workforce Plan: to grow the workforce; to reform education and training and support workforce transformation; and to improve the culture of working in the NHS.
Growing the workforce
Two of the previous Government’s three manifesto commitments were delivered: the commitment to recruit 50,000 additional nursing staff, was delivered 6 months early; the recruitment of 26,000 additional staff in new roles in Primary Care was delivered a year early; however, the additional 6,000 GPs was not achieved.
NHS hospital and community health service workforce
In total the NHS Hospital and Community Health Service Workforce FTE increased by 64,697 to 1,345,047 people (5.1%), with an increase of clinically qualified staff from 671,943 to 711,117 (5.8%). Retention improved overall across the NHS, with statistics showing the leaver rate reduced from 11.8% in March 2023 to 10.2% in March 2024.
Education and training
The annual survey of students and trainees shows an improvement in the overall experience in the last year by 1.3 percentage points between 2022 and 2023. All groups reflected an improvement in experience between 2022 and 2023, except students in Psychological Professions (although student satisfaction here remains one of the highest overall).
Medical trainee numbers were delivered to plan. The chart below shows the number of trainees in 2023/24, against 2022/23 data.
Number of trainees in 2023/24, against 2022/23 data
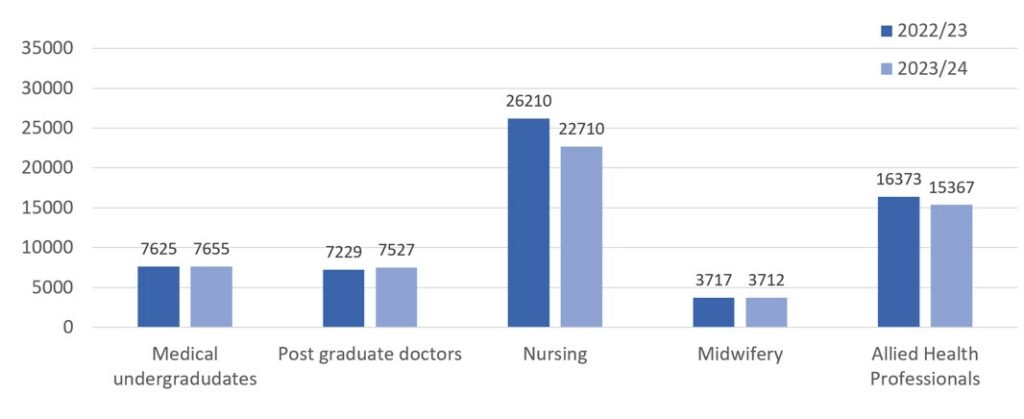
Reform in education and training continues, including the Enhancing Doctors’ Working Lives programme which supports the delivery of activities aimed at enhancing flexibility for doctors in training.
Culture
707,460 people, from 213 NHS trusts and NHS foundation trusts, participated in the 2023/24 NHS staff survey producing the largest response rate to date. Nationally, scores for all elements of the People Promise improved on previous year scores, with notable improvements in the following elements: We are recognised and rewarded, We are safe and healthy, We are always learning, We work flexibly, and We are a team. This year also saw the implementation of the first general practice staff survey in 21 ICBs.
In October 2022, the Preceptorship Framework was launched and embedded. The Preceptorship framework standards for nursing and midwifery provide a supported transition from training to practice for newly qualified staff.
During 2023/24, first and mid-level leadership academy programmes were delivered, with approximately 200,000 enrolments to online programmes. A three-year plan of activity, commencing April 2024, has been developed to continue delivering the Messenger review recommendations.
In 2023, the Fit and Proper Person Test framework was implemented in response to the Kark review, and, in February 2024, we published the NHS Board Leadership Competency Framework and Chair Appraisal framework.
Transforming health and care
We continue to enable the best outcomes for both patients and care providers through driving improvement in services, enabling world-leading research and innovation, and delivering data and digital services on which millions of patients and staff rely every day. In 2023/24, we provided 24/7 support for over 100 national services, ensuring high service availability and resilience.
Transforming NHS services through the NHS App
NHS England has made significant progress in transforming access to healthcare services through the NHS App. By March 2024, 75% of the adult population in England were registered on the app. Integration with patient engagement portals of 82 trusts has facilitated the management of 6 million monthly appointments in secondary care. The app has also played a crucial role in encouraging over 5 million autumn booster bookings (as part of the COVID-19 and Book a Flu Vaccine winter campaigns) and messaging functionalities have saved over £1 million by sending messages securely through the app.
Over 84% of GP practices have enabled record access, providing patients with timely access to information as it is added to their GP record, with this service accounting for over 50% of all app usage traffic. The app now provides information on average wait times and estimated date of treatment for patients referred to NHS acute trusts and patients can now view and order repeat prescriptions through the app, with 13.1% of users utilising this service as of March 2024.
Patient records and digital maturity
In November 2023, NHS England achieved the previous Government’s target of 90% of trusts adopting Electronic Patient Records (EPR) systems, granting authorised clinicians access to crucial patient information. Support and funding have been provided to 160 local EPR projects, with £443.7 million allocated to help ICSs establish essential digital foundations, particularly through electronic records. Health and social care record systems are also being implemented in social care settings, and by the end of 2023/24, 63% of CQC registered adult social care providers had an EPR Digital Social Care Record system in place.
Better use of data
In November 2023, NHS England procured a Federated Data Platform (FDP). The NHS FDP is software that will sit across NHS trusts and ICSs, enabling NHS organisations to bring together operational data, currently stored in separate systems. This supports staff to quickly access the information they need – for example bed availability, the size of elective care waiting lists, or the availability of medical supplies – in one safe and secure environment. To accompany the FDP, we also procured Privacy Enhancing Technology (PET) to support safe data access and use.
Innovation, research and life sciences
Our partnership with the Accelerated Access Collaborative has provided patients with access to proven innovations by bringing together key partners from across government, charities, the NHS, and industry. Work has continued to ensure that the NHS remains a major partner in research and innovation activities, reflecting the aims in the government’s Life Sciences Vision and NHS priorities, and ensuring that recognition of the transformative potential of evidence from research is built into operational and commissioning policies and guidelines for the NHS.
The ICS Research Engagement Network development programme, co-funded with DHSC, has invested £7.2 million to support delivery of local activity across all 42 ICSs to address health inequalities by increasing diversity in research participation.
Through the Innovation for Health Inequalities Programme, we have invested £3.8 million across 39 projects to improve access to National Institute for Health and Care Excellence (NICE) approved innovations for deprived and underserved communities, aimed at reducing health inequalities.
£2.4 million of Small Business Research Initiative (SBRI) Healthcare Award funding has been allocated to research programmes in 2023/24, with the overall total now standing at over £10.3 million.
197 new entrepreneurs joined the Clinical Entrepreneur Programme (CEP) this year and raised £103.1 million on solutions that address frontline challenges, with over 300 CEP alumni retained within the NHS.
In 2023/24 we made major investments in the NHS Research Secure Data Environment (SDE) Network, helping to provide safer and faster access to different types of NHS data across one national and 11 regional SDEs. This has supported over 80 research projects including in genomics, prescribing, primary care, and mental health, with no record-level data leaving NHS England’s environment.
Digital transformation of screening
In 2023/24, NHS England stepped up preparations for the switchover to the new NHS Cervical Screening Management System (CSMS). Improvements to the system will free up more time for frontline staff and ensure all those eligible for a screening appointment are invited on time and followed up as required.
Getting It Right First Time (GIRFT)
The GIRFT programme has expanded its national implementation role with a focus on driving up quality and productivity through various interventions based on clinically led, data-driven peer reviews, with approximately 70 clinical leads across 50 specialties.
GIRFT has supported the elective surgical hub programme and aided struggling trusts and systems through its Decompress Relearn Restart model. Day case surgery rates exceeded national targets, consistently achieving 88% by year-end, and efforts are being made to include unused theatre estate in capacity calculations.
Artificial intelligence in health and care
Aligned with the Government’s Life Sciences Vision to improve clarity on the authorisation and approval pathways for digital health technologies and supported by NICE, NHRA, CQC, and the Health Research Authority, In June 2023 the AI and Digital Regulations Service was launched to provide regulatory advice for developers and adopters of AI and digital technologies in health and care.
As of March 2024, NHS England had allocated £113 million in funding to 86 AI-based projects within the health and care sector. These projects are being evaluated with input from experts in the AI industry, health, and academia, and are being conducted at 408 sites across the UK, encompassing 466 live AI-based trials. 56% of trusts are piloting at least one AI technology product, impacting over 1 million patients in health and care pathways. This work led to the successful deployment of an AI-based decision support service in 95% of stroke networks in England, aiding more rapid identification of patients with suspected strokes.
Digital medicines
Digital medicines initiatives aim to enhance the use of technology and medicines data in the NHS to improve productivity, safety, and patient experience, in relation to how we use medicines in the NHS. Progress has been made in enabling the seamless flow of structured medicines information between NHS IT systems, through the interoperable medicines standard.
The first phase of modernising the Electronic Prescription Service has been completed. This will enable more NHS organisations, particularly in secondary care, to transmit prescriptions to community pharmacies for dispensing. Patients can now view their digital prescriptions through the NHS App and use a digital prescription barcode for dispensing at any community pharmacy.
Infrastructure and core services
During 2023/24 the whole of the Spine infrastructure was moved from physical data centres into the cloud as part of the Spine futures programme. This was accomplished seamlessly while all the live ‘always on’ services were running. Moving Spine to the cloud has resulted in reduced running costs, doubling of Spine capacity, a reduction of our carbon footprint and enabled us to use new security features, strengthening our resilience to potential cyber-attacks.
To support the continued adoption of digital and cloud services, we have supported over 2650 NHS primary and secondary care sites to obtain gigabit capable connectivity. We are also supporting NHS organisations prepare for the scheduled switch-off of the Public Switched Telephone Network, scheduled for December 2025.
We have been rolling out the new National Care Record Service for clinicians to view a summary care record for citizens. The new service now works on mobile devices and browsers and includes new ways of looking up citizen records while meeting new accessibility standards.
Data services – data and analytics operational services
NHS England are now the largest provider of official statistics on health and care. Our flagship Accident and Emergency Statistics is accredited by the Office for Statistics Regulation following assessment on trustworthiness, quality, and value.
Our National Disease Registration Service (NDRS) collects data on patients with cancer, congenital anomalies, and rare diseases. In February 2024 NDRS won the Government Project Delivery Innovation Award for a portal which enables standardised safe submission of data, reducing the burden on the frontline. The portal has been instrumental in enabling linkage of the National Lynch Register with the National Bowel Cancer Screening Programme.
The Model Health System continues to provide a unique benchmarking resource to the NHS, to support quality improvement and productivity. All 368 NHS providers and systems have access with over 58,500 total registered users. The National Competency Framework for data professionals was launched, with more than 500 data professionals and 50 organisations involved in development and testing. Approximately 15% of NHS organisations have now adopted the framework.
Cyber operations
A new unified security team was established to manage the risk to NHS England and support the strategy of making the sector cyber-resilient by 2030. We have provided £38 million to frontline organisations to improve cyber security locally and continue to deliver a range of national cyber services. In 2023/24, we actively monitored over 1.85 million computers and issued 15 high severity alerts, helping protect 367 organisations from the most critical IT vulnerabilities used by cyber criminals.
Emergency preparedness, resilience and response
The COVID-19 response continued into 2023 as a level three incident as part of the transition to recovery. On 18 May 2023, the incident response was stepped down, although it is recognised that COVID-19 and the wider long-term impact of the pandemic will be significant for years to come, and learning from the pandemic response is key.
During 2023/24, incident response arrangements have been activated for several incidents requiring notification to NHS England, which were managed with regional and/or national oversight, including the Coronation of King Charles III in May 2023, a terrorist knife incident in Nottingham in June 2023 and a technical fault at BT that led to a national outage preventing callers accessing emergency 999 voice call services.
Industrial action
The NHS has been navigating continuous industrial action and recovery involving a wide range of health professionals including nurses, ambulance workers, physiotherapists, hospital dentists, junior doctors, and hospital consultants. NHS England has led the national operational response to industrial action and worked with NHS organisations to manage incidents, minimise disruption and support patient care.
Chief financial officer’s report
Introduction
The financial statements for the year ending 31 March 2024 are presented later in this document on a going concern basis (as per Note 1.5 of the accounts) and show the performance of both the consolidated group – covering the whole of the commissioning system – and NHS England as the parent of the group. The group comprises NHS England and the 42 ICBs.
2023/24 is the first full year following completion of the legal merger between NHS England, NHS Digital, and Heath Education England. The new combined organisation has an establishment of around 15,300 whole time equivalent staff compared with approximately 24,300 for the legacy organisations. The new combined organisation will continue the vital functions of the previous organisations, whilst releasing over £400 million to support the front line.
NHS England is required to manage total NHS spending within a fixed revenue limit. The total revenue limit for 2023/24 was £175,017 million.
Funding and allocations
In 2023/24, core funding for the NHS on a like-for-like basis remained broadly flat, in real terms compared to the previous year, increasing by 0.2% including the costs of pay deal adjustments in 2023/24. Funding has been agreed during the year for additional costs, including the higher cost of pay awards where £2.8 billion has been provided to address additional costs of the 2023/24 pay awards which impacted a number of staff groups. £1.7 billion funding for additional costs incurred as a result of industrial action. Additional funding was also agreed for the Primary Care Recovery Access Plan, and delivery of the COVID-19 vaccination and testing programmes.
In January 2023, the NHS England Board approved allocations for the two years from 2023/24 to 2024/25, supporting ICBs to return to longer term financial planning following the emergency financial arrangements in place during the COVID-19 financial regime.
ICB allocations included deployment of an Elective Recovery Fund, made available by the Government to support the recovery of elective waiting lists. The initial targets were reduced in-year in recognition of the service impact of industrial action. Improvements were also made to the formulae through which resources are distributed to ICBs in 2023/24, based on recommendations from the Independent Advisory Committee on Resource Allocation.
From 1 April 2023, all 42 ICBs have taken delegated responsibility for pharmaceutical services, general ophthalmic services, and dental services (primary, secondary and community), and received an additional allocation related to these services.
From April 2024 20 ICBs from 3 NHS England regions have taken delegated responsibility for the commissioning of specialised services.
Operational pressures
Industrial action has continued to create a significant operational and financial pressure on the NHS in 2023/24 with a total of 41 days of strike action by junior doctors and consultants, in addition there were 5 days from other staff groups during the year.
Over the year, ICBs and trusts worked with local authorities to improve discharge processes and increase capacity to support discharge. There was a small reduction in levels of delayed discharges compared to 2022/23, but on average there were still around 12,700 patients per day with delayed discharges.
In 2023/24 we issued capacity funding at the start of the year to support systems to plan ahead of winter to deliver improved urgent and emergency care performance. The funding was focussed on increasing general and acute capacity, virtual ward capacity and utilisation, intermediate and step-down care as well as community beds. This enabled us to improve urgent and emergency care performance despite ongoing high levels of demand.
In spite of these pressures, the NHS has delivered around £7 billion of savings and has made significant improvements in productivity, even with strikes allowing us to improve operational performance in a number of key areas including reducing elective waiting lists, though not by as much as we had planned.
Timeliness of local accounts
In preparing the NHS England group accounts based on consolidation schedules from ICBs, we are reliant on each ICB submitting their audited annual report and accounts to us. We and the Department of Health and Social Care issue directions to NHS bodies on the timing by which these should be submitted.
There are many reasons why a set of audited accounts for a local NHS body may go beyond the deadline: for example, this may reflect illness in the preparer finance team or audit team, or a significant issue may be encountered that takes time to resolve, which may reflect weaknesses in an entity’s preparation of its accounts. Auditors need to be able to complete their work independently of outside influence and take the necessary time to ensure their audit opinion is the right one and supported by appropriate audit evidence. It is also important that there is a properly functioning local audit market to allow audited bodies to hold their auditors to account for delivery. We support the Financial Reporting Council’s current NHS audit market study which will include examining whether this market is functioning effectively.
The vast majority of NHS bodies and their auditors have continued to meet the deadline set for submission of audited accounts. We do not have a backlog of previous years’ outstanding audits affecting a subsequent year. Compliance with the audited accounts deadline for commissioning bodies showed a significant deterioration in 2022/23 compared to historic norms, with the mid-year transition from CCGs to ICBs meaning there was an increased number of bodies to audit. The compliance rate for on-time ICB audited accounts in 2023/24 has significantly improved, and the time taken to resolve cases where the deadline was missed has also reduced. These together have facilitated these accounts being published in October rather than January as in the most recent two years.
A number of actions have contributed to the NHS England group annual report and accounts being published earlier this year:
- an early focus on guidance and training to support the NHS finance community on potential challenges
- more proactively monitoring NHS bodies to ensure they had appointed auditors for the financial year in good time
- a careful focus on the development of the annual report, with early clarity on governance
- timely preparation of national accounts and effective working with the National Audit Office to facilitate detailed audit testing
- a rigorous system of monitoring NHS bodies before and after the audited accounts deadline to support them in managing their audited accounts to completion
- prompt escalation of NHS bodies requiring more support to ensure targeted support from the appropriate part of NHS England to bring resolution of issues and
- planning the expected timing of audited accounts delivery to work out where alternative assurance may be needed nationally and completing this work at an earlier point than previously.
More broadly NHS England continues to work to improve timeliness in financial reporting including:
- encouraging auditors to give clear reporting to audit committees where the preparer’s quality of draft accounts or working papers needs to improve
- working closely with NHS bodies to ensure they appoint external auditors in good time, which helps increase the likelihood of deadlines being achieved
- regular engagement with partners including the Ministry of Housing, Communities and Local Government and the Financial Reporting Council on policy matters affecting the broader local audit system: in particular, the government’s approach of implementing ‘backstop’ dates to resolve backlogs in local government audits has been done with care to minimise potential adverse impacts on the NHS
- contributing to the Financial Reporting Council’s market study into the NHS audit market, including a look at the supply of audit capacity
- working with NHS bodies where financial reporting issues arise to ensure they are able to address findings effectively and
- regular engagement with the audit firms and responding to their feedback to continue to strengthen the NHS financial reporting landscape and working with partners to make sure training and guidance is available for preparers.
NHS England and DHSC have an ambition to return to laying the main national consolidated accounts (being the DHSC group, NHS England group and consolidated provider accounts) before Parliament in advance of the summer Parliamentary recess in July. Achieving this in the years ahead would present challenges for financial reporting in the NHS: it would require the audit community to accept a significantly earlier deadline for audited accounts, better compliance with the deadline by both preparers and auditors, and further streamlining in the national processes for preparation and audit.
14 ICBs were reported by their auditors to the Secretary of State, under Section 30 of the Local Audit and Accountability Act 2014, due to forecasting that expenditure would exceed income during the financial year.
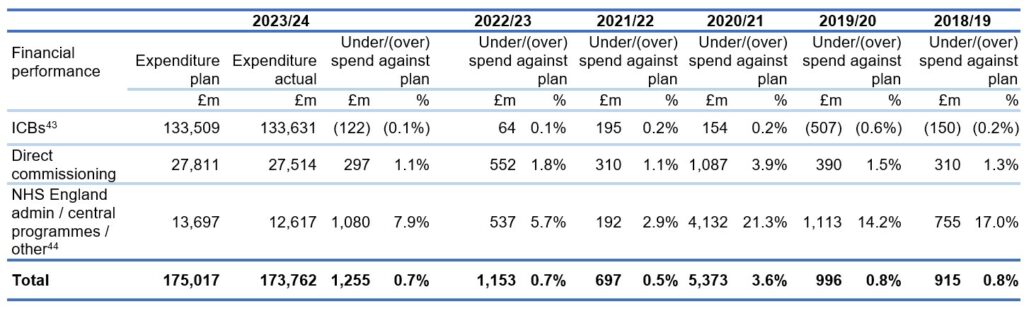
Financial performance
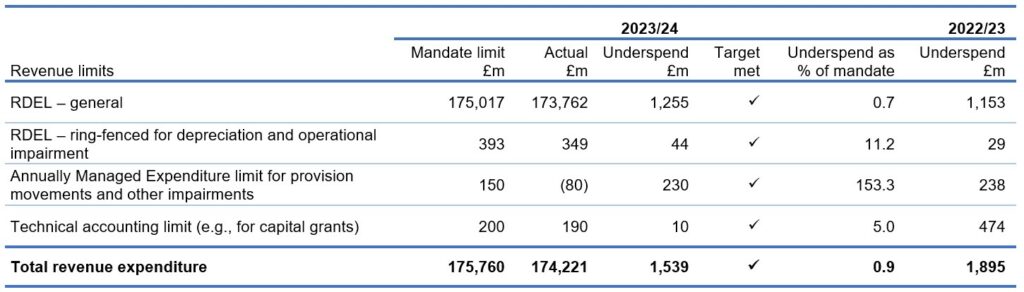
This year, NHS England delivered an underspend of £1,255 million against the revenue resource budget. This planned underspend helped to support the expected overspend in the NHS provider sector and deliver a balanced position across the NHS.
By the end of the year, 15 out of 42 systems either broke-even or delivered an underspend.
Revenue Department Expenditure Limit (RDEL) general (non-ringfenced)
In the mandate, DHSC sets a number of technical financial targets for the NHS England Group, including the core operational limit (general RDEL) described above. These limits are ringfenced, which means that underspends on the other revenue limits cannot be used to support core patient services covered by the general RDEL limit.
2023/24 performance against key financial performance duties
a) Revenue limits
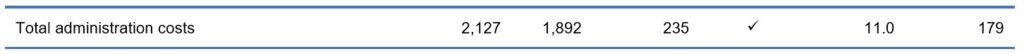
b) Administration costs (within overall revenue limits above)
c) Capital limit

Financial priorities for 2023/24
Our priorities continue to focus on the recovery of core services and productivity. Key to delivery is making sure that the frontline of the NHS has the resources it needs to deliver on our priorities for patients, with a focus on recovering cancer performance, improving emergency care services, improving access to primary care services specifically general practice and dental services and treating as many patients who are waiting for elective care as we can.
We must also recognise the continuing efforts of NHS staff and ensure that colleagues are supported in order that they can continue to deliver their best work for patients.
For 2024/25 we will be working with ICSs to:
- support delivery of system financial plans and for more financially challenged systems to help them recover financial stability over the medium term
- reduction of agency spend as a proportion of the total pay costs for the year
- ensure smooth implementation for the 20 ICBs that have taken delegated responsibility for specialised services and preparation for those taking delegation in 2025/26
- use the specific resources we have been provided with to reduce the number of people waiting for elective procedures, and continue to increase our investment in mental health and primary care services
- continue the journey towards greater system working and integrated care budgets
- maintain spending controls and deliver care as efficiently as we can in the context of ongoing operational constraints, intervening where there is a risk of non-delivery to plan.
Julian Kelly, Chief Financial Officer

