Overview
National Children and Young Adults Diabetes Programme
The Children and Young Adults (CYA) Diabetes Programme brings together the NHS Diabetes programme and the Children and Young People’s Transformation programme. This joint programme of work has been set up to deliver the commitments outlined in the NHS Long Term Plan, including moving to a 0-25 years’ service model.
Alongside regional teams, the programme aims to support systems to improve CYA diabetes treatment and care. To date, the programme has:
- established a National CYA Diabetes Oversight Group to support the development of national policy and strategy to improve the quality of care for CYA living with diabetes, as well as mobilise key stakeholder organisations
- included diabetes as one of the 5 key clinical areas within the children and young people Core20PLUS5 framework, the national NHS England approach to support the reduction of health inequalities
- worked closely with the National Paediatric Diabetes Audit programme on the publication of system level data (and other key outputs), to support benchmarking and improvement
- funded the Transition and Young Adult Pilot programme to build the evidence-base around effective transition and young adult care, as well as number of projects aiming to reduce inequalities in access to diabetes treatment technology. Learning from these are expected to help inform future models of care
- worked with Getting it Right First Time (GIRFT) to establish a Paediatric Diabetes GIRFT programme to support systems with identifying opportunities for improvement
The RightCare programme was engaged and asked to develop this toolkit to support the CYA Diabetes programme in delivering its key objectives.
About this toolkit
The NHS England National Children and Young Adults Diabetes programme worked in partnership with RightCare to develop this toolkit with the aims of bringing together latest guidance and data in one place and provide key practical actions for improvement. The toolkit was developed in collaboration with a wide range of stakeholders including Diabetes UK, clinicians, lived experience partners and their families/carers, NHS integrated care systems (ICS) programme and commissioning leads.
Accurate and timely diagnosis, optimal treatment and care, self-management tools, and support for mental well-being are essential to ensure people with diabetes can live well and avoid complications. This supports improved population health, reduces unnecessary healthcare activity, and has important wider societal and economic benefits.
Who is the toolkit aimed at?
The toolkit is designed to support ICSs to design, plan, and deliver high-quality treatment and care for children and young adults aged 0-25 years with all types of diabetes.
The toolkit may also be of interest to clinicians, healthcare planners and commissioners in related clinical areas, healthcare public health professionals, those working in local authority or voluntary sector organisations, and those with lived experience of diabetes.
What’s included?
This toolkit includes:
- a general overview of an ICS’s role in delivering high quality care within CYA diabetes services
- details of the key areas of focus and actions to take by ICSs to support in the delivery of CYA diabetes services
- a section on enablers to support commissioning and delivery of high-quality care
- a checklist to help ICSs pinpoint where to focus to improve diabetes treatment and care
- links to key guidance, policy documents, and other useful resources
- appendix 1 provides details of the different diabetes data collections available, and appendix 2 provides links to different data sets and information on levels of granularity for each dataset
How to make best use of this toolkit?
This toolkit is not intended to be read from start to finish. Below are some examples of how you may wish to use this toolkit:
How can I identify where our organisation is doing well and where improvements can be made?
Use the ICS checklist to reflect on current commissioned services and identify where there are opportunities to improve the service across the pathway.
I need more general information on children and young people diabetes services in England?
The introduction section provides useful summary information on national organisations, current priorities within CYA diabetes services and key data, as well as useful links.
What are the key areas of focus and how can we improve these within our organisation?
Use the Toolkit on a page to visit each of the 4 Areas of Focus. This will take you to the actions your organisation may wish to consider to achieve these.
What data is available and where can I find it?
Appendix 1 and appendix 2 provide useful information and links to key data collections for CYA diabetes care.
Where can I find key guidelines?
The reference section includes links to all the key legislative and policy documents, guidelines, and other key resources, such as relevant academic papers.
Where can I find case studies?
The evidence and other resources section located within the references table, includes links to available useful case studies.
Four areas of focus
Diabetes can have a significant impact on the health outcomes and the lives of young people and their families or carers. It is a leading cause of healthcare service usage. Four areas of focus have been identified by the national programme. These have been identified through analysis of national audit data as well as working with children and young people, their families and carers, clinicians, and key stakeholders.
The National Children and Young Adults Diabetes programme four key areas of focus are outlined below:
Address diabetes health inequalities in children and young adults
Children and young people living in the most deprived areas have higher HbA1c levels than those living in less deprived areas. Black and minority ethnic groups also have higher HbA1c levels compared to White children and young people. They are also more likely to experience diabetic ketoacidosis (DKA) and repeat DKA admissions to hospital. Despite this, the same groups are less likely to use continuous glucose monitoring technology.
Reduce variation in treatment, care, and outcomes across health systems
Completion of health checks and achievement of treatment targets is associated with reduced complications. However, rates of health check delivery and treatment target achievement vary across units and within integrated care systems between different areas of the country.
Improve treatment and care for people transitioning from paediatric to adult services
Outcomes at transition age are shown to decline, with spikes in diabetic ketoacidosis (DKA) and repeat DKA admissions. In addition, there are also drops in key health check completion and treatment target achievement within this age group.
Improve treatment and care for children and young adults with Type 2 diabetes
Type 2 can often be prevented. If diagnosed in children and young adults it is an aggressive condition and associated with an earlier onset of complications and co-morbidities compared to Type 2 diagnosed later in life (after 40 years of age). However, young people living with Type 2 diabetes have lower health check completion rates compared with those living with Type 1 diabetes. Children of non-white ethnicity and those living in the most deprived areas are over-represented in the Type 2 population.
Introduction
NHS England regional clinical leads
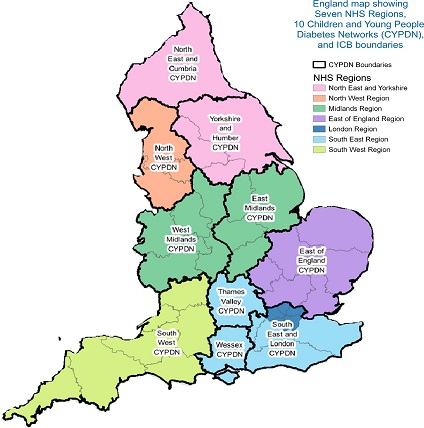
There are NHS England regional CYA diabetes clinical leads within each NHS England region. They provide leadership for improvement in children and young adults diabetes care. The clinical leads are supported by a programme team in each NHS England region. NHS England regional boundaries are colour coded on the map (see figure 1 below).
CYP Diabetes Network
CYP Diabetes Networks (CYPDNs) are collaborative groups whose membership includes local paediatric diabetes clinical teams along with other stakeholders with the aim to share best practice to improve children and young people diabetes care.
Each network has a Clinical Lead and a CYP network manager. Experts working in front-line diabetes services and young people with diabetes are also involved in the networks. CYP Diabetes Network boundaries are shown as black lines on the map, with networks labelled with black and white text (see figure 1).
Figure 1: Children and young people diabetes network map
The map shows different regions in England, each labelled with a specific Children and Young People Diabetes Network (CYPDN). The map is color-coded to distinguish between the regions. Here are the regions and their corresponding CYPDNs:
- North East and Cumbria CYPDN (purple)
- North West CYPDN (orange)
- Yorkshire and Humber CYPDN (pink)
- West Midlands CYPDN (green)
- Thames Valley CYPDN (yellow)
- South West CYPDN (light green)
- Wessex CYPDN (light blue)
- South East and London CYPDN (cyan)
- East of England CYPDN (light purple)
- Midlands CYPDN (dark green)
The map also includes boundaries for NHS regions and integrated care boards (ICBs).
Outcome data
Prevalence
There were 75,180 people aged 0-25 years with diabetes in England in 2022/23. 79.8% had Type 1 diabetes, 14.9% had Type 2 diabetes and 5.3% had other types of diabetes. Of these almost 44% (32,673) were cared for within Paediatric Diabetes Units. For those with Type 2 diabetes, 29.9% of 16 -18 year-olds and 69.4% of 19-25 year-olds were cared for within primary care (see the NDA annual report).
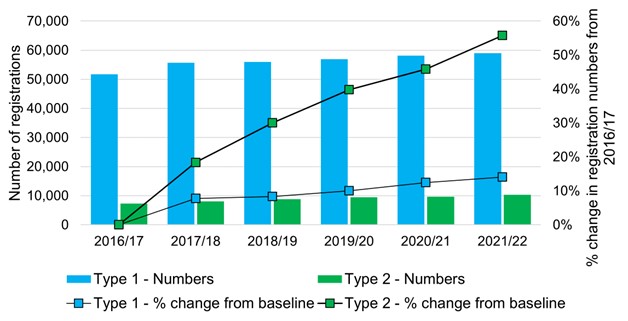
There has been an increase in the prevalence of diabetes over time. Figure 2 shows from 2016/17 to 2022/23, there has been just over a 16% increase in the number of children and young people with Type 1 diabetes, and just over 54% increase in the number with Type 2 diabetes (National Diabetes Audit annual reports in National Clinical Database Repository (NCDR). This has important implications for workforce planning, as ensuring adequate staffing is key to the provision of high-quality care. To support ICSs in managing the increased prevalence of diabetes, key considerations related to appropriate system leadership and workforce are included within the enablers section of this document.
People with a learning disability are at greater risk of developing diabetes than the general population. A recent review of available research shows 8.5% of people with a learning disability have Type 2 diabetes. For young people with a learning disability (15-24 years), a recent Learning from lives and deaths – people with a learning disability and autistic people (LeDeR) deep dive report indicates that the rate of Type 2 diabetes is approximately 16 times higher than for their peers without a learning disability (Baksh et al, 2023). Furthermore, in children and young people aged 5-24 years with Down’s Syndrome, the incidence rate of diabetes was also 4 times more common (Aslam et al, 2022).
Figure 2: Number of diabetes registrations (0-25 years) and percentage change from 2016/17 by year and diabetes type
The chart shows the number of Type 1 and Type 2 diabetes registrations for individuals aged between 0 – 25 years old, along with the percentage change in registration numbers from 2016/17 to 2022/23. The data shows an increase in the prevalence of diabetes over time, with a 14% increase in the number of children and young people with Type 1 diabetes, and just over 54% increase in the number with Type 2 diabetes.
Source: National Diabetes Audit annual reports for 2016/17 to 2022/23 (the most recently available) in NCDR (record level). Note about data: Registrations from the NDA audit reports include data from both GP practices and specialist services. The numbers here will not include patients who have indicated they don’t want their data shared with NHS Digital, a small number of non-submitting practices, and some incomplete/poor coding.
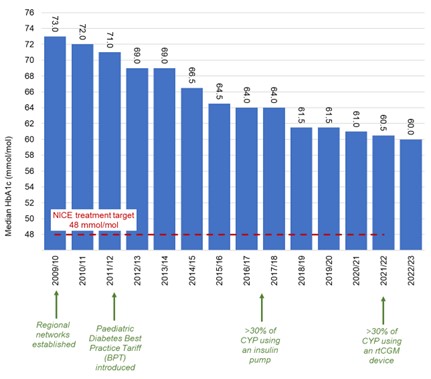
HbA1c
HbA1c is a marker of raised blood glucose. It is expressed in ‘mmol/mol’. A HbA1c target level of 48 mmol/mol or lower is defined as the ‘treatment target’ for children and young people by NICE. Reaching this will minimise the risk of developing long‑term complications related to diabetes.
Multiple drivers, including the introduction of the Best Practice Tariff in 2010/11, has seen the median HbA1c in children and young people with diabetes (Type 1 and 2) fall steadily nationally since 2009/10.
Despite this, the median HbA1c is still higher than the treatment target. Variation exists between ICSs and paediatric diabetes units, with the median HbA1c in children and young people with Type 1 diabetes within individual PDUs ranging from 53.0 mmol/mol to 70.3 mmol/mol (see figures 3 and 4 below).
ICSs can access relevant data from the National Paediatric Diabetes Audit (NPDA). Key considerations for ICSs in reviewing data on HbA1c and care process completion is included within the enablers section on data.
Figure 3: Median HbA1c for children and young people with Type 1 diabetes in England 2022/23 by ICS (NPDA report)
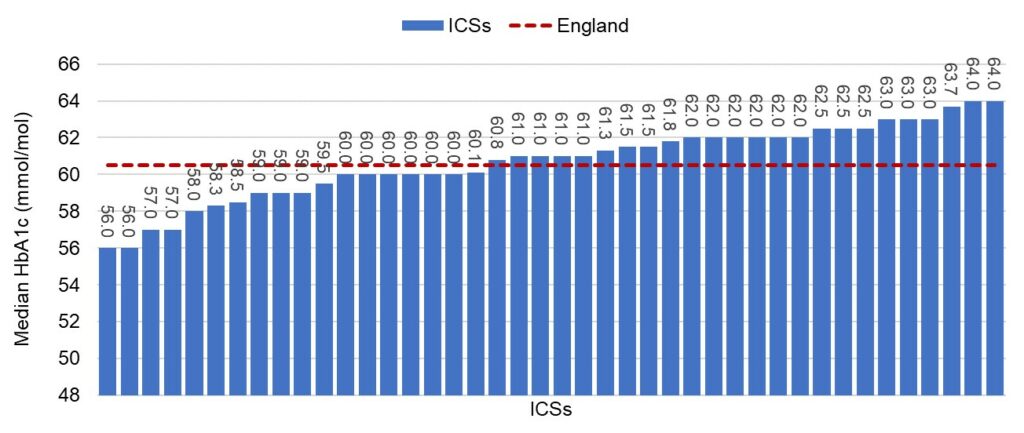
The bar chart shows median HbA1c levels for children and young people with Type 1 diabetes for each ICS in England, in 2022/23. The chart shows a range from 56.0 millimoles per mole to 64.0 millimoles per mole. The median across England is shown as 60.5 millimoles per mole.
Source: National Paediatric Diabetes Audit – data files | RCPCH
Figure 4: Median HbA1c for children and young people with all types of diabetes in England, 2009/10 to 2022/23 (NPDA report)
NICE target: NG18, Recommendation 1.2 Type 1 Diabetes
The bar chart shows median HbA1c levels for children and young people with all types of diabetes in England, from 2009/10 to 2022/23 with associated key policy or technological introductions. The chart shows the median HbA1c level steadily dropping, from 73.0 millimoles per mole in 2009/10 to 60.0 millimoles per mole in 2022/23. The NICE treatment target is noted as 48 millimoles per mole.
Source: NPDA – data files | RCPCH
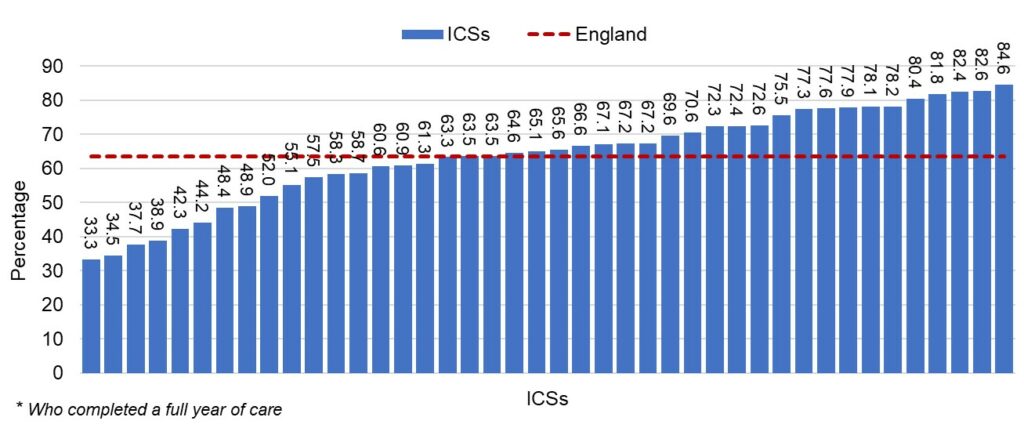
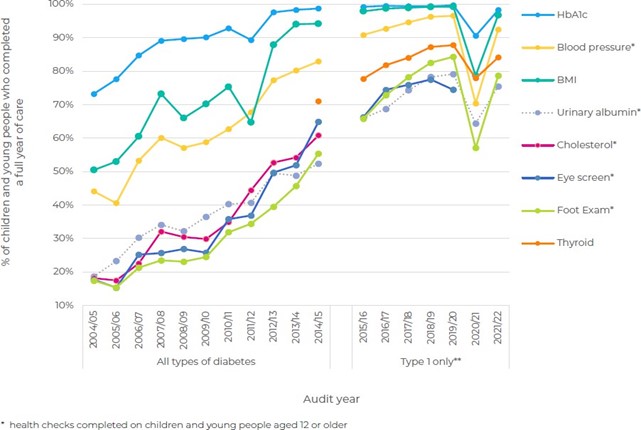
Care processes
NICE recommends that people with diabetes receive key health checks (or ‘care processes’) completed annually. Higher completion of these health checks is associated with better glycaemic management. Undertaking these annual health checks is associated with reduced premature mortality, emergency admissions, and risks of developing diabetes complications and associated care costs (McKay et al, 2021a; Gunn et al, 2021a; Gunn et al, 2021b; McKay et al, 2021).
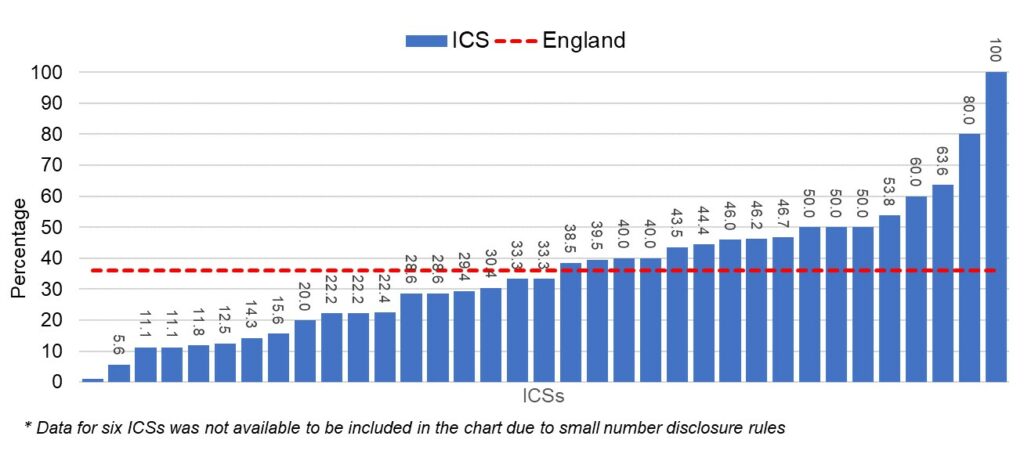
For children and young people with Type 1 diabetes, variation in completion rates exists between each of the individual care processes and within specific geographies, representing an opportunity for improvement. Latest figures (NPDA, 2022/23) show only 63.4% of children and young people aged 12 and over with Type 1 diabetes received all 6 health checks and the variation between ICSs was from 33.3% to 84.6%. ICSs can access relevant data from the NPDA (see figure 5).
Early-onset Type 2 diabetes is a more aggressive condition than older-onset Type 2 diabetes. Despite this, completion of the key annual health checks (‘care processes’) remains low compared to completion rates in adults. Only 36.0% of those with Type 2 diabetes aged 12 and over received all six care processes. Latest results from the NDA 2021-22 young people with Type 2 diabetes report suggest children and young people with Type 2 diabetes are less likely to have completion of all care processes compared to adults (aged 40 plus years). The latest detailed NDA data also shows that those with a learning disability (all ages) were less likely to receive all key care processes.
Figure 5: Percentage of children and young people aged 12+ with Type 1 diabetes* who received all 6 key health checks in 2022/23 by ICS
*6 key health checks for Type 1 diabetes in children and young people aged 12 and above are: HbA1c, BMI, blood pressure, thyroid test, albuminuria screening and foot checks.
The bar chart shows the percentage of young people aged 12 and over with Type 1 diabetes who received all 6 key health checks in 2021/22, broken down by ICS. The chart shows variation in completion rates, ranging from 33.3% to 84.6%. Only 63.4% of children and young people with Type 1 diabetes received all of the 6 key health checks.
Figure 6: Percentage of children and young people aged 12+ with Type 2 diabetes who received all 6 key health checks in 2022/23, by ICS
*6 key health checks for Type 2 diabetes in children and young people aged 12-18 are: HbA1c, BMI, blood pressure, cholesterol, albuminuria screening and foot checks
The bar chart shows the percentage of young people aged 12 and over, with Type 2 diabetes, who received all 6 key health checks in 2022/23. The data is broken down by ICS. The chart shows variation in completion rates, ranging from 0% to 100%. Completion rates of the key health checks remains low for children compared to rates in adults. Only 36% of young people with Type 2 diabetes received all 6 key health checks.
Source: National Paediatric Diabetes Audit – data files | RCPCH
Relevant to area of Focus 2: reduce variation in treatment, care, and outcomes across health systems
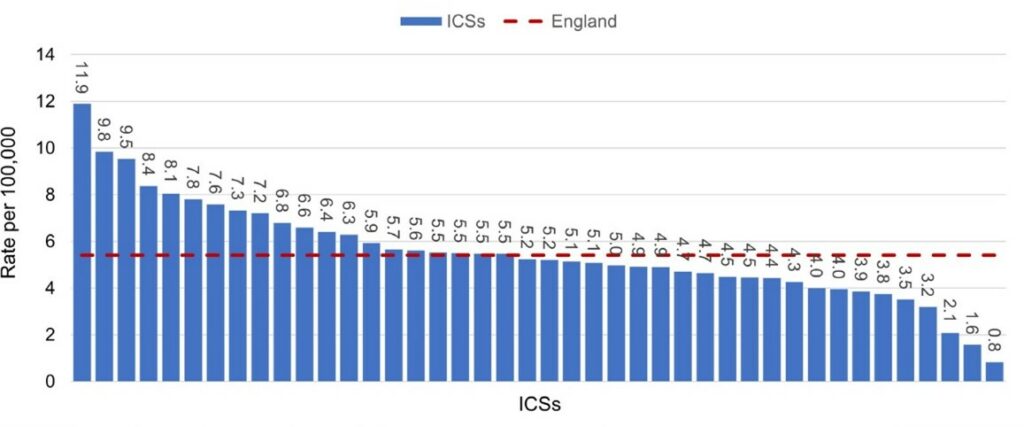
Diabetic ketoacidosis
Diabetic ketoacidosis (DKA) is a serious acute complication of diabetes that requires emergency in-patient management. It can be life threatening and may need to be managed in an intensive care setting.
Some people with undiagnosed diabetes may not be aware they have diabetes until they reach the stage of DKA for the first time (‘DKA at diagnosis’). Analysis from the National Paediatric Diabetes Audit admissions and complications reports, 2011-2020 show a steady increase in DKA at diagnosis across the audit years, with the rate increasing from 29.3% in 2015/16 to 38.5% in 2019/20. Supporting awareness amongst clinicians and the public of early signs and symptoms of diabetes is important to reduce rates of DKA at diagnosis.
People with a known diagnosis of diabetes can also experience DKA. DKA in this situation is often preventable and therefore may reflect a need for services to better engage, educate and support the individual with their diabetes care and management. Analysis from the NPDA showed that lower rates of admission with DKA, not at diagnosis, were associated with lower HbA1c and use of real time continuous glucose monitoring (rtCGM) in children and young people with Type 1 diabetes.
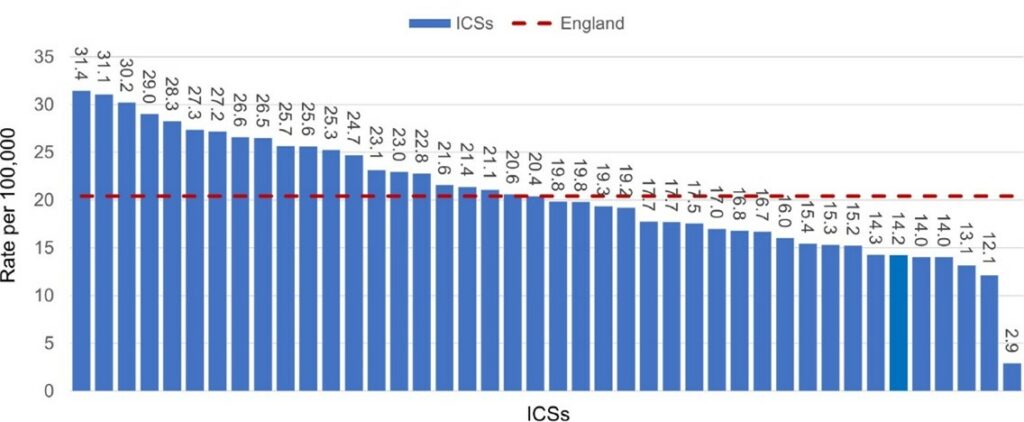
Variation in emergency admissions for DKA exists between ICSs and paediatric diabetes units for both DKA at diagnosis and DKA in those with a known diagnosis of diabetes (see figures 7 and 8).
Key considerations for systems to support reductions in DKA admissions are included within Area of Focus 2.
ICSs can access relevant local data on DKA admissions from the Children and Young People’s Transformation Programme dashboard, available on the NHS England Applications platform.
Figure 7: DKA emergency admissions for children and young people with a new diagnosis of diabetes, 2022/23
The bar chart shows the number of DKA emergency admissions for children and young people with a new diabetes diagnosis in 2022/23, broken down by ICS. The chart shows a variation in admissions from 11.9 per 100,000 to 0.8 per 100,000.
Source: All graphs National Paediatric Diabetes Audit (NPDA)
Figure 8: DKA emergency admissions for children and young people with an existing diagnosis of diabetes, 2022/23
The bar chart shows the number of DKA emergency admissions for children and young people with an existing diabetes diagnosis in 2022/23, broken down by ICS. The chart shows a variation in admissions from 31.4 per 100,000 to 2.9 per 100,000.
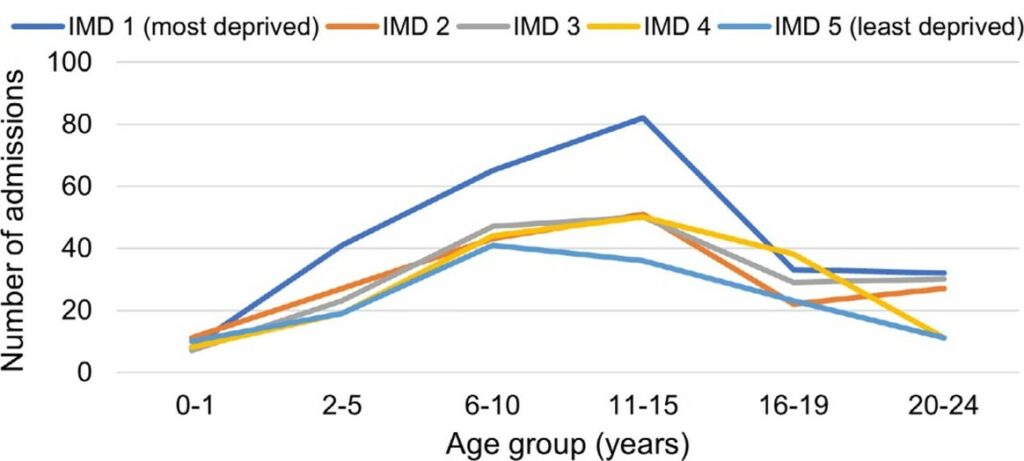
Transition and young adult care
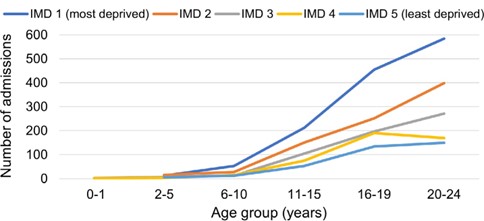
Diabetes outcomes are seen to particularly decline at the age when children and young adults with diabetes are transitioning to adult care. This is where the highest rates of diabetic ketoacidosis (DKA) admissions and repeat DKA admissions are observed. In addition, DKA emergency admissions with an existing diagnosis of diabetes, has a clear social gradient which gets steeper with age, as shown on the graphs (see figures 9 and 10).
A GIRFT report into diabetes care found that transition and young adult services are often unavailable or under-resourced. This may result in young people becoming disengaged, leading to avoidable harms. The GIRFT report found that if clear transition pathways were implemented there would be a reduction in DKA admissions in 18–25-year-olds.
Analysis of data on young people at transition age shows that median HbA1c, and the proportion of people achieving HbA1c treatment targets, deteriorates steadily between the ages of 15 and 20 years old. In addition, completion of most annual NICE recommended care processes decreases between the ages of 17 and 20 years and then plateaus.
Key considerations for systems to support improving care for those transitioning from paediatric to adult care are included within area of focus 3.
Figure 9: Diabetic ketoacidosis emergency admissions in patients with a new diagnosis of diabetes (2022/23)
The line chart shows the number of emergency DKA admissions for patients with a new diagnosis of diabetes in 2022/23. The data is split into deprivation quintiles and 6 different age ranges (0-1, 2-5, 6-10, 11-15,16-19, and 20-24). The chart shows a consistently higher number of emergency DKA admissions in the most deprived quintile in those aged 2-5, 6-10 and 11-15 years old compared to the other deprivation groups.
Figure 10: Diabetic ketoacidosis emergency admissions in patients with an existing diagnosis of diabetes (2022/23)
The line chart shows the number of DKA emergency admissions for patients with an existing diagnosis of diabetes in 2022/23. The data is split into 5 deprivation categories and 6 different age ranges (0-1, 2-5, 6-10, 11-15,16-19, and 20-24). The chart shows a consistently higher number of DKA admissions in the two most deprived quintiles across the age groups of 6-10, 11-15, 16-19 and 20-24 years.
Source: CYP transformation DKA dashboard
Inequalities
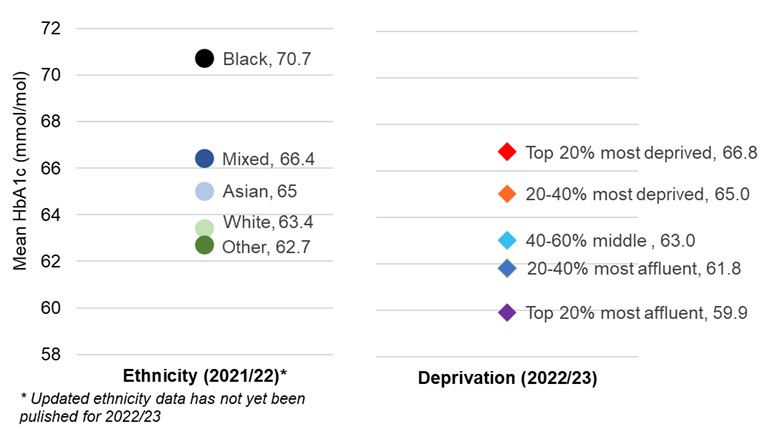
HbA1c levels have been higher in Black children compared to White children since 2005/06, and data between 2013/14 and 2022/23 shows persistently higher HbA1c levels in those living in more socio-economically deprived areas. For example, NPDA data in 2021/22 showed that median HbA1c for black children and young people was 70.7 mmol/mol, compared to 63.4mmol/mol in white children and young people. For children and young people in the most deprived 20%, HbA1c was 67.6mmol/mol compared to 60.1mmol/mol for those in the least deprived 20% (see figure 11).
Figure 11: Inequalities: Mean HbA1c for children and young people Type 1 diabetes in England and Wales
The chart shows the mean HbA1c levels for children and young people with Type 1 of diabetes in England and Wales. The data is split by ethnicity and deprivation. The chart shows that in 2021/22 Black children have the highest median HbA1c levels from the different ethnic groups. In 2022/23 those from the most deprived socioeconomic group also have the highest median HbA1c levels compared to those from the least deprived groups.
Source: NPDA Annual report 2021-22, Care processes and outcomes, Appendix 1 – full audit analysis
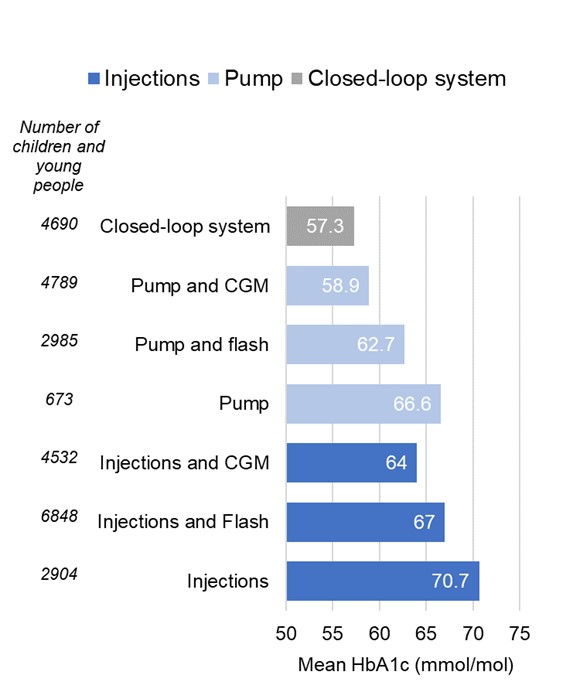
A key factor in improving glycaemic management, and reducing DKA emergency admissions, is diabetes treatment technology such as continuous glucose monitoring devices and insulin pumps. These are recognised by NICE to be cost- effective (see the resource impact report for CGM), help achieve target HbA1c levels, reduce the risk of long-term complications and associated care-costs, and improve the quality of life of those living with diabetes. Recent data shows that children and young people who were using a hybrid closed-loop system had a significantly lower mean HbA1c compared to those using insulin injections (see figure 12).
Figure 12: Mean HbA1c for children and young people with type 1 diabetes using different combinations of treatment regimen and glucose monitoring 2022/23
The chart shows the mean HbA1c levels for children and young people with Type 1 diabetes in 2022/23, using different combinations of treatment regimen and glucose monitoring. The data shows that children and young people who were using a hybrid closed-loop system had a significantly lower mean HbA1c compared to those using insulin injections.
Source: NPDA Annual report 2021/22
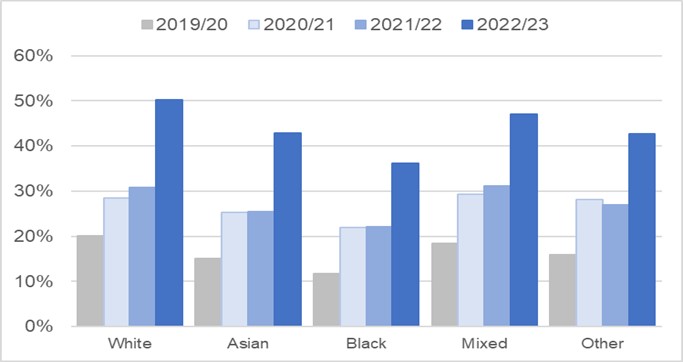
Despite an overall increase in uptake of treatment technology, national audit data shows clear health inequalities by ethnicity and socioeconomic deprivation. Usage is lowest in children and young people from socially deprived areas and those from ethnic minority backgrounds. For example, in 2022/23, only 38.8% of children and young people in the most deprived quintile used insulin pumps, compared to 50.7% of children and young people in the least deprived quintile. Only 36.2% of Black children were on continuous glucose monitors, compared to 50.2% of White children. ICSs can access relevant data from the NPDA. Key considerations for ICSs to support more equitable access to treatment technology is in area of focus 1.
Figure 13: Percentage of children and young people with type 1 diabetes using CGM by ethnic group, 2019/20 to 2022/23
Chart showing the percentage of children and young people with type 1 diabetes using CGM by ethnic group between 2019/20 to 2022/23. The data shows that those from Black and Asian ethnic groups with Type 1 diabetes had consistently lower usage of CGM pumps compared to White children over the 4 year time period.
Ethnic Group
White | Asian | Black | Mixed | Other | |
|---|---|---|---|---|---|
|
2019/20 |
20.2% |
15.1% |
11.7% |
18.5% |
16.0% |
|
2020/21 |
28.4% |
25.3% |
21.9% |
29.3% |
28.1% |
|
2021/22 |
30.8% |
25.4% |
22.2% |
31.1% |
26.9% |
|
2022/23 |
50.2% |
42.8% |
36.2% |
47.0% |
42.7% |
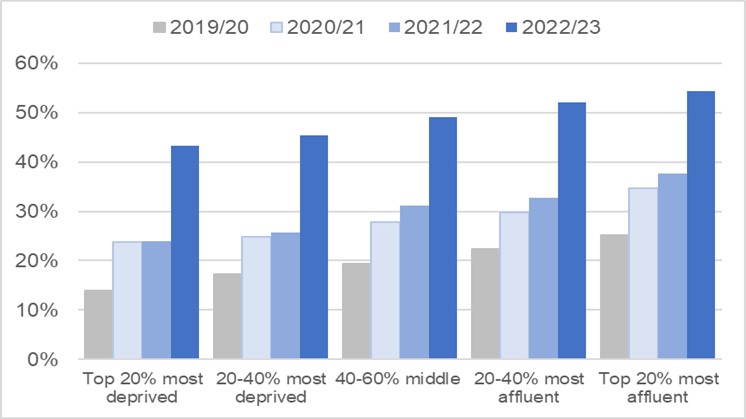
Figure 14: Percentage of children and young people with type 1 diabetes using CGM by deprivation quintile, 2019/20 to 2022/23
Chart showing the percentage of children and young people with type 1 diabetes using continuous glucose monitors by deprivation quintile between 2019/20 to 2022/23. The data shows that those from the lowest socioeconomic quintiles had consistently lower usage of continuous glucose monitors compared to those from the least deprived quintiles.
Deprivation quintile
Top 20% most deprived | 20-40% most deprived | 40-60% middle | Top 20% least deprived | 20-40% least deprived | |
|---|---|---|---|---|---|
|
2019/20 |
14.0% |
17.3% |
19.3% |
22.3% |
25.2% |
|
2020/21 |
23.8% |
24.9% |
24.9% |
29.8% |
34.7% |
|
2021/22 |
23.9% |
25.7% |
25.7% |
32.7% |
37.7% |
|
2022/23 |
43.3% |
45.3% |
49.0% |
52.1% |
54.4% |
Source: NPDA Annual report 2022-23, Report on care processes and outcomes
Relevant to Area of focus 1: address diabetes health inequalities in children and young adults
Type 2 inequalities
Early-onset Type 2 diabetes (defined as diagnosis under the age of 40 years-old) is an often preventable and more aggressive condition when compared to older-onset Type 2 diabetes. It is associated with more rapid disease progression, early development of complications and a significant reduction in life expectancy (Sattar et al, 2019; Kaptoge et al, 2023).
Whilst the majority of people with early-onset Type 2 diabetes are White, there are higher proportions from ethnic minorities in the young onset cohort compared with the older onset cohort. 93.5% children and young people with Type 2 diabetes were classified as overweight or obese based on their BMI, compared with 41.7% of children and young people with Type 1 diabetes (NPDA 2022/23). For young people aged 15-24 years with a learning disability, a recent LeDeR deep dive report indicates the rate of Type 2 diabetes is approximately 16 times higher than for their peers without a learning disability (Baksh et al, 2023).
Despite the more rapid progression of diabetes complications in those with early-onset Type 2 diabetes, the completion of NICE recommended care processes remains low compared to completion rates in older adults. The latest Young People with Type 2 Diabetes report showed that only 26.7% of children and young people with Type 2 diabetes aged 0-25 received all care processes, compared with 51.6% of those aged 60-79.
In addition, when co-morbidities and complications are identified, treatment rates are low. For example, 42.3% of children and young people with Type 2 diabetes had high blood pressure, however only 5.9% were offered anti-hypertensive therapy. A quarter of children and young people with type 2 diabetes had albuminuria, an early marker of kidney disease, however only 3.4% received treatment (NPDA spotlight).
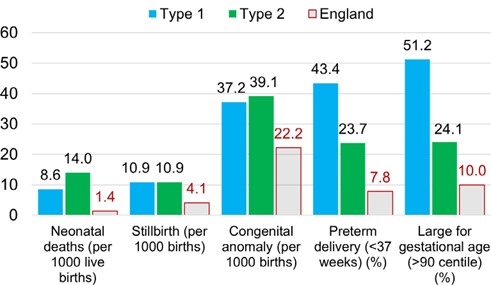
Pregnancy and diabetes
Around 1 in 7 women who give birth in the UK each year either have diabetes before they get pregnant, or develop gestational diabetes during their pregnancy (IDF Atlas 2021). While most will go on to have healthy babies, diabetes in pregnancy is associated with pre-term delivery, birth weight extremes, increased rates of congenital anomaly, stillbirth, and neonatal death (Murphy et al (2021)).
Women with pre-existing diabetes have considerably more adverse pregnancy outcomes than those women who do not have diabetes in pregnancy. This is related to a lack of support to prepare for pregnancy, namely in achieving the HbA1c treatment target of 48 mmol/mol or lower, low rates of prescribing folic acid during pregnancy which helps reduce the risk of birth defects such as spina bifida and missed opportunities to access safe, effective contraception for women who may be sexually active but not planning a pregnancy, which is particularly important given 45% of pregnancies are unplanned.
Latest National Diabetes in Pregnancy (NPID) Audit data show that only 36% of women with early-onset type 2 diabetes achieved the NICE recommended early pregnancy target HbA1c of <48mmol/mol and experienced increasing rates of serious adverse pregnancy outcomes compared to previous years (2022 6.6%, 2021 4.9%, 2020 and previous years 5.5%) (see figure 14).
Figure 15: Maternity and birth outcomes: pregnancies in diabetes compared to England overall, 2021 and 2022
Bar chart showing maternity and birth outcomes for women in England with diabetes, for 2021 and 2022. The data shows that women with Type 1 diabetes have higher rates of pre-term deliveries and babies who are large for their gestational age. In women with Type 2 diabetes, there is a higher rate of neonatal deaths and babies born with a congenital anomaly.
Notes about the data: The latest NPID audit data covers the time period from 01/01/2021 to 31/12/2022.
The England figures for neonatal deaths and still births are taken from the Child and infant mortality statistics in England and Wales, 2021. Congenital anomaly data is taken from the National Congenital Anomaly and Rare Disease Registration Service (NCARDRS) Congenital Anomaly Official Statistics Report, 2020. Preterm delivery is taken from the OHID child and maternal health profile, 2019-21.
Source: NPID Audit 2021 and 2022.
RightCare toolkit on a page
Enablers
Funding
The planning and funding of diabetes treatment and care for children and young adults is the responsibility of ICBs. NHS England is responsible for determining allocations of financial resources to ICBs. Total annual budgets given to ICBs cover the majority of NHS spending, including the costs of delivering diabetes care. In addition to this core allocation, several financial incentives exist.
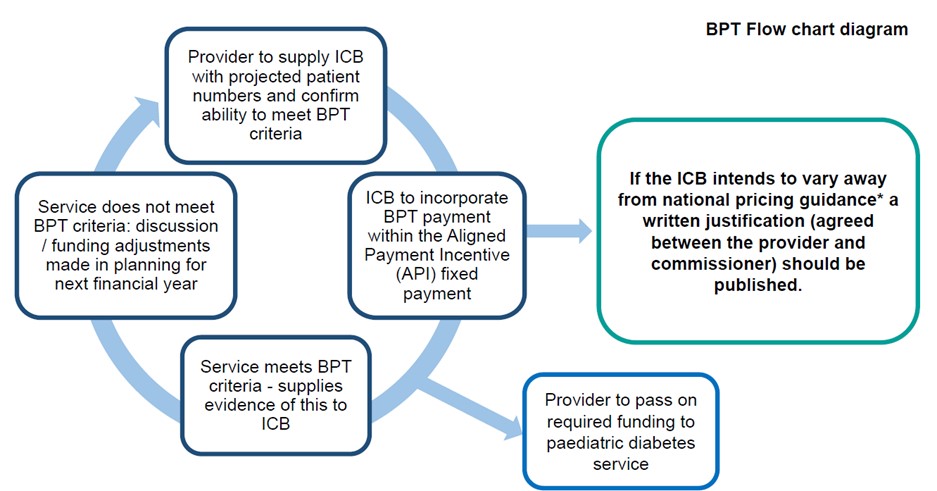
Paediatric best practice tariff
Best practice tariffs (BPTs) were first introduced in 2010/11. They are designed to incentivise high quality, cost-effective care with the overall aim of reducing unwarranted variation in clinical quality and to spread best practice.
BPTs cover services that have high volumes of activity, significant variation in practice, or significant impact on patient outcomes. BPTs support areas of care where there is a strong evidence base and clinical consensus on best practice.
The paediatric diabetes BPT is an annual payment per patient for a year of care. It aims to support clinical services to deliver consistent, high-quality care to children and young people with diabetes, aged 0-19 years.
The level of funding that hospital trusts can achieve through the BPT reflects the estimated funding that services will require to meet the BPT specification, with a particular focus on the cost of the workforce and training.
To qualify for the BPT payment, providers must demonstrate that they meet all the specified criteria, found in the BPT guidance documents.
Content within this toolkit is aligned to the BPT criteria. The implementation of the BPT criteria is expected to reduce overall care-costs through incentivising consistent quality diabetes care.
BPT covers:
- outpatient care from the date of discharge from hospital after the initial diagnosis until the patient is transferred to adult services up to the age of 19
- inpatient care for any admissions related primarily to diabetes, after the initial diagnosis, up to the age of 19
BPT does not cover:
- cost of insulin pumps and associated consumables
- cost of CGM systems when used continuously for therapeutic purposes
- routine prescriptions for insulin, blood glucose testing (including flash glucose scanning/FreeStyle Libre) and ketone monitoring issued in primary care
BPT payment scheme 2023-25
The way the Paediatric diabetes best practice tariff works changed in 2023/24 (see figure 15). The following steps set out how the BPT should now work locally, as set out in national guidance (NHS England » 2023-25 NHS Payment Scheme annex C).
- ICB and hospital trust agree a fixed payment for the year to fund the delivery of paediatric diabetes care. This fixed element should be based on an assessment of expected paediatric diabetes patient numbers and whether the provider is likely to deliver best practice criteria, as set out nationally.
- Finance teams within hospital trusts confirm to paediatric diabetes service leads that the paediatric diabetes BPT payment has been received by the trust. The department receives the funding to support the availability of the necessary workforce and training to achieve the nationally set criteria.
- ICB and hospital trusts review achievement of the BPT criteria at the end of the financial year based on evidence supplied by the trust. Where best practice was not achieved, this should be discussed and a plan put in place, or funding adjustments made, in the next financial year/planning process. No in-year payment adjustments should be made.
Figure 16: Best practice tariff flow chart diagram
*For example, if the ICB does not intend to pass on the full best practice tariff (BPT) quantum for the projected number patients.
Flow chart showing how the best practice tariff payment works from 2023/24 based on the criteria in Annex C of the 2023-25 NHS Payment Scheme guidance documentation.
The steps are:
- The healthcare provider gives the ICB an estimate of patient numbers and confirms they can meet the best practice tariff standards.
- The ICB includes the best practice tariff payment as part of a fixed payment system known as the aligned payment incentive (API). If the ICB decides to diverge from the national pricing guidance, they must provide a written justification for this decision, which is agreed upon with the provider and then made public.
- The funding is passed to the provider, who then uses it to finance specific services, like paediatric diabetes care.
- At the end of the year there are two possible outcomes a. If the service meets BPT standards: the provider needs to show evidence of this to the ICB and no adjustments are made or b. If the service does not meet BPT standards: the provider and ICB will discuss what went wrong and make funding adjustments for the next financial year.
System leadership
High quality diabetes treatment and care is clinically effective, safe and provides a positive patient experience, with benefits including improved health outcomes and reduced healthcare activity and costs in the long-term. The role of the ICS is to provide oversight and support to providers, creating the right conditions for high quality care, using all the levers at its disposal. This includes effective planning, leadership, partnership working, and quality governance.
Planning and governance
Children and young adults’ diabetes should be reflected in system strategic plans. This should span the full pathway – from prevention of Type 2 diabetes to improving diagnosis and treatment for children and young adults living with all types of diabetes in primary, community, and secondary care services.
Commissioning, service planning and improvement initiatives can be enabled by a population health management approach – using local prevalence and outcomes data, which takes appropriate account of health inequalities (see area of focus 1 and area of focus 4).
Designated clinical and managerial leads at ICS level
Having designated clinical and managerial leadership in the ICS will enable effective engagement with services and support improved communication, closer working and sharing of good practice between paediatric, young adult and adult teams, as well as between primary, community and secondary care. Having specific individuals whose role it is to regularly review data across the pathway of care to identify improvement opportunities will support the delivery of high-quality care.
Key considerations
Key considerations for system leadership include to:
- engage with lived experience partners and their families/carers
- review data regularly (see appendix 2) and use it to inform review meetings, service planning and commissioning, seeking context from service leads
- develop local networks and join regional networks
- support services to Make every contact count (MECC)
- ICS to participate in the forthcoming CYA Diabetes GIRFT programme
- collaborate with ICP partners on cross cutting issues that require a partnership approach such as lifestyle and healthy weight support for children and families, contraception and sexual health services, youth worker support, the provision of individual healthcare plans and family support
- report to ICS governance groups on key quality metrics and improvement initiatives
- apply the paediatric diabetes best practice tariff and use other financial and contractual levers (see enablers section on funding)
- log quality risks in ICS quality risk registers and present risks to System Quality Groups where appropriate
- consider Diabetes UK leadership programme
Data
National diabetes data for children and young adults comes from 2 main sources – the National paediatric diabetes audit and the National diabetes audit.
National paediatric diabetes audit (NPDA)
All paediatric diabetes units (PDUs) submit data about people with all forms of diabetes under the care of a consultant paediatrician up to the age of 24, although most paediatric services do not continue to care for people beyond 18 years of age. This includes data on HbA1c levels, health checks, patient education, psychological well-being, and assessment of diabetes related complications including acute hospital admissions. The NPDA publishes an annual annual report and has an online tool to help make the data more interactive and accessible at PDU, network and at former CCG level.
National diabetes audit (NDA)
The NDA integrates data from both primary and secondary care settings. The NDA Core Audit annual and quarterly dashboards include data on care process delivery, treatment target attainment and structured education. The data is available at ICS, PCN and GP practice level. The Adolescent and young adults audit includes data for those age 15-25 with Type 1 diabetes. The data is available at region and ICS level, with the dashboard refreshed annually. The Young type 2 diabetes audit, includes data for those up to age 40 with Type 2 diabetes. Data is available at region, ICS and PCN level and can be accessed via the Young people with type 2 diabetes dashboard and will be updated annually.
Further information on these datasets and other national reports is available at appendix 1. Details of all available metrics and where to find data is available at appendix 2.
Some ICSs already collate local data through business intelligence functions and have ICS level dashboards which may draw from national and/or local data. This will continue to advance as new initiatives such as the Federated data platform come online. Systems should regularly consider refreshing data sources and data presentation.
Key considerations
Key considerations for data include to:
- read national audit and quality improvement reports to understand key themes and trends (see appendix 1)
- review key diabetes metrics and consider how the services in your ICS compare to regional and national averages (see appendix 2)
- look for disparities in care and outcomes that may lead to or reflect health inequalities in socio-economically deprived groups with protected characteristics
- check that local services are regularly uploading data into the NPDA data capture system and the NDA specialist services data collection, with consideration given to the ability of teams to collect accurate data
- encourage local services to regularly review audit and other service level data and key diabetes metrics to inform plans to address unwarranted variation
- ask services to inform the ICS if they receive an outlier status letter from the NPDA and work with them to understand how any quality issues will be rectified
- support the inclusion of diabetes metrics (national and / or local data) in ICS population health dashboards
Workforce
The prevalence of Type 1 and Type 2 diabetes in children and young people is increasing. The NPDA annual report recommends that multidisciplinary diabetes team staffing increase proportionately to reflect this. As part of the RCPCH National Diabetes Quality Programme (NDQP), 132 peer reviews were conducted across participating services between 2018 to early 2023. From these peer reviews the most common recommendations were for increases in MDT staffing including dietetic, medical, psychological, paediatric diabetes specialist nurse, and administrative provision. The NDQP also looked at serious concerns raised within services and found that services that had MDT clinic appointments and MDT training had smaller numbers of serious concerns identified. See Impact report 2023 from the National Diabetes Quality programme.
The Best practice tariff (BPT) for paediatric diabetes stipulates that patients should be offered a minimum of 4 clinic appointments a year, with a recommendation of 30 minutes per appointment, with a MDT. Sufficient staffing is required to deliver this and to support the provision of high-quality care. As well as this, the BPT criteria includes the requirement that patients must be offered at least one additional appointment per year with a paediatric dietitian with training in diabetes.
The NHS Long Term Workforce Plan includes reforms around working and training differently, enabling innovative ways of working with multidisciplinary teams so staff can spend more time with patients.
Key considerations
Key considerations for workforce include to:
- align paediatric diabetes Best Practice Tariff payments to the latest data on patient numbers
- work with service leads to review patient numbers and staffing ratios regularly and identify any gaps in multi- disciplinary teams
- ensure there is appropriate administrative and IT support for data recording and audit participation
- review the local workforce to ensure there is an appropriate level of staffing to support delivery of high-quality care to children and young people with diabetes
- review the capability and competencies of MDTs to ensure that professionals are being supported to develop key skills
- encourage services to support staff to attend regular training on the use of new diabetes-related technologies and treatments (such as insulin pumps, CGM and hybrid closed loop systems)
- support services to participate in regional/ national networks for peer support and quality improvement (refer to the system leadership enabler section)
Areas of focus
Area of focus 1: addressing diabetes health inequalities
The Health and Care Act 2022 identifies a range of ICB obligations in relation to health inequalities. This includes a duty on an ICB that it: “must, in the exercise of its functions, have regard to the need to (a) reduce inequalities between persons with respect to their ability to access health services, and (b) reduce inequalities between patients with respect to the outcomes achieved for them by the provision of health services”.
NHS England has a legal duty to annually assess the performance of each ICB in each financial year. The NHS Oversight Framework provides the basis for this assessment. Reducing health inequalities is part of this, aligning to the priorities set out in operational planning guidance and the legislative changes.
NHS England has developed the ‘Core20PLUS5’ approach to inform action to reduce healthcare inequalities at both national and system level. The approach defines a target population – the ‘20% most deprived (CORE20)’ – and identifies ‘5’ focus clinical areas (PLUS5) requiring accelerated improvement. Within CORE20PLUS5 for Children and Young People, diabetes has been identified as one of the 5 key clinical areas.
The 2 key objectives for the Core20PLUS5 approach in diabetes are to:
- Increase access to real time continuous glucose monitors and insulin pumps across the most deprived quintiles and from minority ethnicity backgrounds.
- Increase the proportion of those with Type 2 diabetes receiving all recommended care checks.
For more information see the CORE20PLUS5 infographic for Children and Young People.
Theme
Equitable services
Context
Data demonstrates that children and young people with diabetes do not always have equitable access to diabetes care or outcomes, with unwarranted variation seen related to age, socio-economic status and ethnicity. People who experience socio-economic deprivation face multiple challenges and barriers which may impact on their ability to access care and self-manage long term health conditions.
Equitable access to technology
There are persistent inequalities in the use of diabetes treatment technology. NPDA data from 2022/23 shows that rtCGM use is 43.3% within the most deprived quintile, compared to 54.4% in the least deprived quintile, whilst usage amongst Black children is 36.2% compared to 50.2% in White children.
For insulin pumps, usage amongst White children is 47.5% compared to 33.0% in Black children, and in the most deprived quintiles it is 38.8% compared to 50.7% in the least deprived quintile.
Risk factors associated with Type 2 diabetes
The number of children and young people with early-onset Type 2 diabetes is increasing. Whilst the majority of people with early-onset Type 2 diabetes are White, there are higher proportions from ethnic minorities in the young onset cohort compared to the older onset cohort. The younger onset cohort with Type 2 diabetes are also more likely to be from deprived areas compared to their older onset peers. (National Diabetes Audit 2021-22, Young People with Type 2 Diabetes) (published December 2023. A recent LeDeR deep dive report has shown that for young people with a learning disability (15-24 years), the rate of Type 2 diabetes is approximately 16 times higher than for their peers without a learning disability (Baksh et al, 2023).
Theme
Equitable services
Actions
- Use the available health inequalities metrics data (see Appendix 2) to understand variation in care and outcomes for different groups in your area.
- Offer training for staff to support teams to identify and address health inequalities.
- Facilitate implementation of the 2 specific Core20PLUS5 objectives for diabetes in children and young people.
- Consider the diversity of the population and whether services can adapt the delivery of care or service models based on key factors such as language, religion, cultural norms, practices, and beliefs.
- Ensure services make available reasonable adjustments for disabled children, for example autistic children and young people and those with a learning disability, or both.
- Support release of staff time to work with families who have particular needs, taking account of health inequalities and associated factors which may have an influence on condition management.
- Ensure clear referral pathways are in place for equitable access to mental health and well-being services.
Equitable access to technology
- Review commissioning policies for diabetes glucose monitoring technology in line with NICE guideline NG18, with the objective of minimising barriers such as completion of individual funding requests.
- Analyse data on diabetes treatment technology usage and determine if there are inequalities based on age, ethnicity, or deprivation (see Appendix 2 on where to find data and see the NPDA).
- Ensure children and young people with diabetes are offered a choice of clinically appropriate diabetes technology that meets their individual needs, for example the needs of young children or disabled children including those with a learning disability or autism.
Risk factors associated with Type 2 diabetes
- Work with ICSs on a prevention strategy to ensure that there is a focus on obesity in children and young adults, as obesity is a key risk factor for early-onset Type 2 diabetes (a diagnosis of Type 2 diabetes in those aged under 40 years old).
- Work with ICSs to support them to increase the proportion of children and young people with Type 2 diabetes receiving annual health checks, as per the Core20PLUS5 objective.
Area of focus 2: reduce variation in treatment, care, and outcomes across systems
Theme
Quality oversight
Context
Rates of health checks delivery, treatment target achievement, access to treatment technology, DKA admissions, rates of complications, patient and family experience and pregnancy preparedness vary across units and between different areas of the country.
Timely and accurate diagnosis
A failure to diagnose diabetes can lead to life threatening diabetic ketoacidosis (DKA) and this can develop particularly quickly in children and young people. There has been a steady year-on-year increase in DKA at diagnosis rates in children and young people from 29.3% in 2015/16 to 38.5% in 2019/20. Differentiating between Type 1, Type 2 and monogenic diabetes is challenging in young people, with specialist input and investigations required to achieve an accurate diagnosis.
Structured education and peer support
People living with diabetes need to make frequent decisions and choices about how to manage their diabetes, often supported by parents and carers, particularly in childhood and adolescence. There is evidence (NICE [QS209], Statement 2, Steinsbekk et al (2012), Tai et al (2021)) of the benefit of structured education and peer support for young people and families.
First year of care
A positive experience of care for people that are newly diagnosed with diabetes and their families is a strong foundation for future clinician- patient engagement and supported self-management. Optimising the management of diabetes in children and young adults from as early as possible after onset can reduce the incidence, and delay the impact of, the longer-term complications associated with diabetes.
Preventing hospital admissions
Outpatients’ services should have very low DKA hospital admission rates in already diagnosed patients. If there are admissions where the primary cause is for diabetes, this is a signal that there could be improvement opportunities in outpatients’ treatment and care services, for example in education, self-management, and use of technology.
Retinopathy
Diabetic eye screening services are nationally commissioned and delivered by a provider framework. Diabetes professionals may not have access to screening results. Retinopathy screening has the lowest completion rate of all the care processes.
Dental care
Poor periodontal health has a bidirectional link with glycaemic management in people living with diabetes. There is also a correlation between living with obesity and dental caries (decay), relevant in Type 2 diabetes.
Treatment technology
Evidence demonstrates the positive impact of continuous glucose monitoring technology on achieving the HbA1c treatment target, however access is variable by geography, socio-economic status, and ethnicity (also see Area of Focus 1 – Health Inequalities).
Mental health and well-being
3 in 5 people with diabetes experience emotional or mental health problems as a result of their condition (Diabetes UK 2017). Type 1 Diabetes related Disordered Eating (T1DE), is a condition where people with type 1 diabetes restrict their insulin intake to lose weight. It can give rise to an increased rate of both acute and chronic diabetes complications and can lead to a 3-fold increase in risk of death.
Theme
Quality oversight
Actions
- Regularly review key metrics using local and national data. As a minimum, review care process completion, HbA1c (mean and achievement of NICE treatment target), use of diabetes treatment technology, DKA admissions (new and established patients), rates of diabetes complications, patient and family experience and pregnancy preparedness. Review the data cut by age, deprivation, ethnicity, learning disability where available.
- Review national audit and quality reports to identify key themes and trends.
- Participate in the forthcoming CYA Diabetes GIRFT Programme.
Timely and accurate diagnosis
- Regularly review national and local diabetes data to understand DKA at diagnosis rates and assess variation across the locality. Where rates of DKA at diagnosis are particularly high, further investigation is warranted to understand what is driving it – for example, missed opportunities to identify diabetes in primary care, or the need for a local public awareness campaign.
- Raise awareness in primary care of the challenges of correctly classifying diabetes type in young people, with training and robust pathways in place for prompt access to specialist diabetes services.
- Encourage services to ensure training is undertaken in identifying rarer types of diabetes in children such as monogenic diabetes. Many trusts have monogenic diabetes champions to support appropriate screening and testing.
- Consider whether services have access to diagnostic investigations such as Type 1 antibody tests and testing for monogenic diabetes.
Structured education and peer support
- Undertake a system level review of the provision of structured education programmes and their uptake. This should include a review of uptake of nationally funded products: Digibete (0-25-year-olds with all types of diabetes), My Type 1 (aged 19+ with Type 1 diabetes) and Healthy Living (aged 19+ with Type 2 diabetes), as well as locally commissioned services. Provision should include a mix of face to face and digital provision, recognising that preferences will differ amongst the target population. Other structured education resources are also available such as Seren, DAFNE, DESMOND and DEApp that children and young people can be signposted to.
- For those using technology such as insulin pumps to help manage their diabetes, this therapy needs to be supported by a device specific education programme to ensure optimal use.
- Consider local promotion of peer support networks such as Diabetes UK Together Type 1 or other local support networks where available.
First year of care
Encourage services to develop a first year of care pathway for Type 1 diabetes. See Appendix 6 for the first year of care pathway produced by The Children and Young People National Diabetes Network.
Preventing hospital admissions
- Review rates of admissions for established diabetes patients, looking for any increases or spikes
- Ensure services provide sufficient education and support to people with diabetes on how to spot the warning signs and symptoms of DKA.
- Ensure services are pro-actively reviewing their DKA admissions data to identify patients who may require additional support in managing their condition to prevent further admissions.
Retinopathy
- ICSs are encouraged to link with their local diabetic eye screening provider/s to develop a standard operating procedure/ process to ensure screening results can be sent to the appropriate children and young people clinical teams within the ICS.
- Encourage services to speak to patients about the importance of attending retinopathy screening. Children (aged 12+) who have had an abnormal eye screen should be screened again the following year and not biannually.
Dental care
Work with dental commissioners to support access to dental care for children and young people with diabetes due to their increased risk of periodontal disease, recognising that children and young people with diabetes may require a more frequent dental recall interval.
Treatment technology
- Ensure commissioning policies align to NICE NG18 which states that all children and young people with Type 1 diabetes, and children and young adults with Type 2 meeting specified clinical criteria should be offered real-time continuous glucose monitoring.
- Where technology is commenced in paediatric care (such as insulin pumps), systems should consider how policies support this technology still being available when the person transitions to adult care.
- Implement the NICE Technology Appraisal TA943 Hybrid closed loop system for managing blood glucose levels in Type 1 diabetes.
Emotional care and well-being
- Ensure services are adequately staffed to meet the NICE guidance recommendation that children and young people (aged up to 18) with diabetes have access to annual psychological screening and timely psychological support when needed and appropriate to emotional, social, cultural, and developmentally appropriate needs
- Consider what non-clinical support CYA can access such as dedicated youth workers and peer support groups.
- Develop integrated diabetes and mental health models of delivery, building on the learning from nationally funded Type 1 Disordered Eating (T1DE) pilot areas.
Area of focus 3: improve treatment and care for those transitioning from paediatric to adult services
Theme
Preparation for transfer and transition
Context
Transition refers to the time when a young person moves from one diabetes service to another. Often this is from a paediatric service to an adult service, however it can also refer to moves between different adult services, including to primary care settings, as well as moves across geographical locations.
Integration of paediatric and young adult services
Diabetes outcomes are seen to particularly decline at the age when children and young adults with diabetes transition to adult care, where the highest rates of diabetic ketoacidosis (DKA) admissions and repeat DKA admissions are observed. A recent GIRFT report found that transition services are often unavailable or under-resourced. This may result in young people becoming disengaged, leading to avoidable harms. Provision of a coordinated transition is particularly important where children and young adults have multiple long-term conditions and/or a learning disability.
Young adult care
Ensuring that young adult services are tailored to meet the needs of the young people using them will help to maximise service engagement.
Contraception and planning for possible pregnancy
Young women with diabetes may become pregnant during this period with an increased risk of stillbirth and neonatal morbidity. The major modifiable risk factor for this is poor glucose management at the start of pregnancy (NPID, Murphy et al (2021)). As pregnancies are often not planned in this age group, support to achieve HbA1c treatment target and facilitating access to contraception is key.
Theme
Preparation for transfer and transition
Action
Review whether diabetes services have clear policies and pathways for transition.
Integration of paediatric and young adult services
- Review whether paediatric and adult services routinely deliver joint clinics together and have a period of crossover (more than one joint appointment) for the person moving between services. Consideration around the funding of adult teams is needed to enable this.
- Ensure there are clear protocols and processes in place regarding discharge policies (where services are encouraged to retain young people and take appropriate measures to engage recurrent non-attenders), high HbA1c policies, and appropriate processes for transfer of any ongoing mental health care.
Young adult care
Review whether services:
- Offer dedicated clinic time and/or space for young adults (18-25 years old) that are separate from routine diabetes clinics for older-aged adults.
- Tailor service delivery to young adults and families with specific support needs such as learning disabilities, considering where reasonable adjustments can be made when required
Contraception and planning for possible pregnancy
- Work with services and those with lived experience to understand whether contraception and sexual health services are easily accessible.
- Support services to provide information about how diabetes affects pregnancy and how pregnancy affects diabetes. This should include the importance of glucose management in reducing the risk of adverse outcomes such as miscarriage, stillbirth, and congenital malformation.
- Ensure service pathways include considerations for women with diabetes who may become pregnant (such as contraception, folic acid, prescription, and medication review).
- For those planning pregnancy, consider what specialist services are in place to ensure diabetes care and pre-pregnancy health is optimised.
- Ensure service pathways enable women to access appropriate antenatal care when a pregnancy is confirmed whether planned or unplanned.
Area of focus 4: improve treatment and care for children and young adults with Type 2 diabetes
Theme
Prevalence
Context
The number of CYA developing Type 2 diabetes is growing each year and there has been an increase of 21.8% in those aged under 25 years over the last 4 years (2017/18 – 2021/22).
People with early onset Type 2 diabetes are more likely to be female and the latest National Diabetes in Pregnancy (NPID) Audit data show that only 36% of pregnant women with type 2 diabetes achieved the NICE recommended early pregnancy target HbA1c of <48mmol/mol.
Healthy lifestyle support
Being overweight or obese is the major modifiable risk factor for a diagnosis of Type 2 diabetes and most (93.5%) children and young people with Type 2 diabetes cared for within paediatric diabetes units were classified as overweight or obese (NPDA 2022/23). Complications from Excess Weight (CEW) clinics for children have been rolled out across the country aimed at children and young people with severe obesity and/or complications arising from obesity. The clinics use a holistic approach to treating conditions related to obesity. Children and young people will be able to access CEW clinics following a referral from secondary or tertiary care. This link contains more information around the clinics including the referral criteria
People aged 0-25 years old with Type 2 diabetes are less likely to receive all 8 care processes compared to older adults with Type 2 diabetes. Those aged 0-18 years should be cared for in a specialist paediatric diabetes service (NICE NG18). Whereas most (69.4%) of the 19-25 years age group are under the care of general practice.
High quality care and support
A lack of confidence and awareness of treatment options for CYP with type 2 has been identified amongst the paediatric profession, with many units seeing fewer than 5 patients a year. The Type 2 Diabetes and the Young (T2Day) programme aims to improve care for people with Type 2 diabetes aged 18-39 years by introducing treatment reviews that are additional to usual routine care. The additional reviews will provide an opportunity to address any missed care processes and will aim to provide high quality care by addressing key elements:
- classification of diabetes type
- contraception and planning for possibility of pregnancy
- optimisation of glycaemia, cardiovascular risk, and weight
- psychological well-being and unmet social needs
Theme
Prevalence
Actions
- Review the number of children and young people with Type 2 diabetes living in your area (available at ICS level) via the Type 2 Diabetes Dashboard.
- Review OHID Public Health Profiles annual data on percentage prevalence of those overweight and obese (available at place level).
Healthy lifestyle support
- Work with stakeholders in the ICS and ICP (including Local Authorities) to take a population health management approach to addressing overweight and obesity in children and young adults – with a particular focus on high prevalence areas and groups, and the presence of Tier 1 and Tier 2 services.
- Map relevant local supporting services available for CYA with type 2 diabetes (such as weight management services, peer support, mental health, or social support services) and ensure providers are signposting appropriately.
- Work with CEW clinics, where present, to map pathways and ensure that interdependent services are joined up (such as diabetes services). Not all ICSs currently have a CEW clinic, therefore requiring some ICSs to work across larger boundaries.
High quality care and support
- Regularly review key diabetes metrics using local and national data. As a minimum, review care process completion, HbA1c (mean and achievement of NICE treatment target), rates of diabetes complications, patient and family experience and pregnancy preparedness. Review the data cut by such as age, deprivation, ethnicity where available (see Appendix 2 on where to find data).
- Review the capability and competencies of specialist paediatric MDTs to ensure that staff are being supported to develop key skills to care for children and young people with Type 2 diabetes. This could include training and or participation in peer support networks (see the enablers section on workforce).
- Consider the role of Additional Roles (such as clinical pharmacists, health and well-being coaches, social prescriber, and advanced practitioners) in enhancing the care of young adults with type 2 diabetes in primary and community settings.
- Commission delivery of the Type 2 Diabetes in the Young (T2Day) programme, adapted to suit local needs. This should include referral of cases identified in those under 18 years to specialist services and provision of additional treatment reviews for those aged 18-39 years.
Appendices
Appendix 1: data collections
National Diabetes Audit (NDA)
The NDA is one of the largest clinical audits in the world and integrates data from both primary and secondary sources. It is a mandatory NHS collection, funded by NHS England and NHS Wales. General practices and specialist services have their data extracted via the General Practice Extraction Service (GPES), whilst secondary care and structured education providers submit their data manually via the Clinical Audit Platform.
The NDA provides a comprehensive view of diabetes care in England and Wales. It measures the effectiveness of diabetes healthcare against NICE Clinical Guidelines (NG17) and NICE Quality Standards (QS208 and QS209) with the aim to answering the following questions:
- Is everyone with diabetes diagnosed and recorded on a practice diabetes register?
- What percentage of people registered with diabetes received the 9 National Institute of Health and Care Excellence (NICE) key processes of diabetes care?
- What percentage of people registered with diabetes achieved NICE defined treatment targets for glucose management, blood pressure and blood cholesterol?
- What percentage of people registered with diabetes are offered and attend a structured education course?
- For people with registered diabetes what are the rates of acute and long-term complications (disease outcomes)?
The audit collects data on all ages from primary care, but does not collect data from paediatric specialist units, which is delivered separately via the National Paediatric Diabetes Audit.
Commissioners can use the interactive National Diabetes Audit dashboards to drill down into the data relating to the provision of care and services for people with diabetes in their area.
The key audit products for children and young adults’ diabetes care are:
- the NDA Core Audit dashboards – Annual and quarterly dashboards with data on care process delivery, treatment target attainment and structured education. The data is available at ICS, PCN and GP practice level
- the Adolescent and Young Adults Audit (AYA), includes data for those age 15-25 with Type 1 diabetes and can help identify any areas of improvement for the provision of care and services during transition from paediatric to adult based clinical The data is available at region and ICS level and the dashboard is refreshed annually
- the Young Type 2 Diabetes Audit, includes data for those up to age 40 with Type 2 Data is available at region, ICS and PCN level and the dashboard will be updated annually
National Paediatric Diabetes Audit (NPDA)
The purpose of the NPDA, is to provide information that leads to an improved quality of care for those children and young people living with diabetes.
The National Paediatric Diabetes Audit is funded by NHS England and NHS Wales, commissioned by the Healthcare Quality Improvement Partnership (HQIP), and managed by the Royal College of Paediatrics and Child Health. It started from 2003 and is currently commissioned until 2025.
Paediatric Diabetes Units (PDUs) across England and Wales submit data about the care received by children and young people using their services. The effectiveness of that care is measured against NICE guidelines and includes HbA1c targets, health checks, patient education, psychological well-being, and assessment of diabetes related complications including acute hospital admissions, all of which are vital to monitoring and improving the long-term health and well-being of children and young people with diabetes.
The audit’s aims are to:
- monitor the incidence and prevalence of diabetes amongst children and young people receiving care from a PDU in England and Wales.
- establish whether recommended health checks are being received by children and young people with diabetes.
- enable benchmarking of performance against standards of care specified by the National Institute for Health and Care Excellence (NICE) guidance at PDU, regional, CCG (England), Health Board (Wales) and national
- determine the prevalence and incidence of diabetes-related complications amongst children and young people with diabetes.
The latest audit report (2022/23) included all 171 PDUs in England and Wales and captured information on 31,615 children and young people with all forms of diabetes up to the age of 24 years under the care of a consultant paediatrician.
The NPDA has an online reporting tool to help make the NPDA data more interactive and accessible at PDU, regional network, ICS, and previous clinical commissioning group (CCG) level. NPDA Online (rcpch.ac.uk).
The NPDA also collects Patient/Parent Reported Experience Measures (PREMs) data from paediatric diabetes units and produces local and national reports.
Quality and Outcomes Framework (QOF)
Information on system performance against the QOF indicators can be found at QOF 2021-22 | NHS Digital.
Quality Improvement Programmes
A quality programme for children and young people’s diabetes ran between 2018- 2023 and was delivered by RCPCH at PDU level. The impact report from this programme provides a source of data and learning. National Diabetes Quality Programme – Impact report 2023 | RCPCH
The NDA QI collaborative is a National programme provided as part of the National Diabetes Audit contract. Relevant reports with key learning are listed below:
Getting It Right First Time (GIRFT)
GIRFT is a national programme designed to improve medical care within the NHS by reducing unwarranted variation.
The adult GIRFT diabetes workstream published a national report in 2020, that focused on improving services for people with type 1 diabetes and improving inpatient care and foot care for everyone living with diabetes.
The national report has recommendations which are relevant to children and young people around transition from paediatric to adult services, specialist support for young adults on insulin pumps and around psychological support needs to manage their condition.
National CYA GIRFT programme
To provide a national mechanism for identifying and supporting systems and units to address variation, a dedicated CYA Diabetes GIRFT programme is being established.
The programme will use a core set of metrics to be developed at unit, system, and region level, to inform the GIRFT visits and to build an understanding of how variation presents between PDUs and ICSs. It will undertake a series of system level ‘gateway reviews’ to explore the causes of unwarranted variation and identify opportunities for addressing them.
The programme will cover care and outcomes for those with diabetes up to the age of 25 and run for 2 years initially. The focused visits will be at system level supporting the engagement of both paediatric and adult services, as well as supporting involvement of commissioners and key local decision makers to best influence change and improvement. This will also allow for assessment of transition care, and variation in outcomes associated with the move from paediatric to adult care.
Visits will be undertaken at system level (ICS) initially, with the opportunity for additional follow up visits at PDU level in subsequent years where the need is identified. It is expected that engagement with this programme will serve as a mechanism for Trusts to evidence their compliance with the BPT. Data and analysis developed as part of this programme will be embedded in the Model Health System database as a mechanism for units and systems to further assess and benchmark their position nationally in relation to key metrics and measures.
Appendix 2: data resources
The data for the key children and young adult diabetes metrics comes from different sources and reflects the different setting in which care is delivered. It includes routine primary care data, national survey d
Prevalence data
How many children and young adults are living with diabetes (type 1 or type 2) within your area?
| Where to find the data | Geography level | Diabetes level | Age breakdown available |
|---|---|---|---|
| NDA core and Annual dashboard Region, ICS, Sub ICS | Region, ICS, Sub ICS | Type 1 and Type 2 | 12-19; 20-29 age splits presented |
| National Paediatric Diabetes Audit – data files ICS level data file For data by deprivation: use the ‘unit, region national’ data file | Unit, ICS, Region, and Network level | Type 1 and Type 2 | 0-24 years cared for in paediatric services |
How many children and young people are there with Type 1 diabetes by age band, sex, ethnicity, and deprivation?
| Where to find the data | Geography level | Diabetes level | Age breakdown available |
|---|---|---|---|
| NPDA – data files Refer to file npda_2022-2023 ICS data. For Deprivation refer to file NPDA 2022-23 unit, region and national data file. | ICS | Type 1 | 0-24 years cared for in paediatric services 0-15 years (split presented) |
Care process completion
How does your rate of care process completion (for all and individual health checks), compare to other ICSs within the region and nationally?
| Where to find the data | Geography level | Diabetes level | Age breakdown available |
|---|---|---|---|
| NDA core and Annual and quarterly dashboards NDA type 1 dashboard – Microsoft Power BI | Region. ICS, Sub ICS | Type 1 and Type 2 Type 1 | 19-25 years (split presented) |
| Adolescent and young adults dashboard | Region and ICS level | Type 1 | 15-25 years, individually or combined |
| Young Type 2 dashboard (coming Summer 2023) | Region, ICS and PCN | Type 2 | 0-40 years |
| NPDA results online | Unit, ICS, Region, and Network level | Type 1 and Type 2 | 0-24 years cared for in paediatric services |
HbA1c (mean and achievement of NICE treatment target)
How does the mean HbA1c of children and young adults with diabetes your system compared to other ICSs within the region and nationally?
How does the proportion achieving the HbA1c Treatment Target (58mmol/mol) in your system compared to other ICSs within the region and nationally?
| Where to find the data | Geography level | Diabetes level | Age breakdown available |
|---|---|---|---|
| NDA core Annual and quarterly dashboards – TT achievement and HbA1c levels NDA Type 1 dashboard Microsoft Power BI | Region. ICS, Sub ICS | Type 1 and Type 2 Type 1 | 19-25 years (split presented) |
| Adolescent and young adults dashboard | Region and ICS level | Type 1 | 15-25 years, individually or combined |
| Young Type 2 dashboard | Region, ICS and PCN | Type 2 | 0-40 years |
| NPDA results online – Median HbA1c | Unit, ICS, Region, and Network level | Type 1 and Type 2 | 0-24 years cared for in paediatric services |
Usage of diabetes treatment technology
Is usage of diabetes technology equitable between the most and least deprived groups and by those from ethnic minorities in your area?
| Where to find the data | Geography level | Diabetes level | Age breakdown available |
|---|---|---|---|
| NPDA usage of: Flash CGM Insulin Pumps Hybrid Closed Loop Splits for insulin pumps and CGM are available by deprivation and ethnicity | Unit, ICS, Region, and Network level | Type 1 | 0-24 years cared for in paediatric services |
| NDA Type 1 dashboard Microsoft Power BI – usage of flash, CGM, Closed loop system, insulin regimes and pump usage Adolescent and young adults dashboard – Insulin pump usage | Region, ICS, and sub-ICS Region, ICS | (>19 years), (19-25 years split presented) 15-25 years, individually or combined | |
| All prescribing data is published on the BSA website Prescribing data | NHSBSA | Various | Type 1 | All ages |
DKA Admissions
What are the rates of DKA at diagnosis? And DKA in established patients?
| Where to find the data | Geography level | Diabetes level | Age breakdown available |
|---|---|---|---|
| NPDA annual reports and NPDA results online | Unit, ICS, Region, and Network level | Type 1 and Type 2 | 0-24 years cared for in paediatric services |
| Adolescent and young adults’ dashboard | Region and ICS level | Type 1 | 15-25 years, individually or combined |
Rates of diabetes complications
What proportion of children and young adults are achieving the NICE recommended treatment targets in your area?
| Where to find the data | Geography level | Diabetes level | Age breakdown available |
|---|---|---|---|
| NDA Type 1 dashboard Microsoft Power BI – Blood pressure TT achievement and statin usage | Region, ICS, Sub ICS | Type 1 | 0-24 years cared for in paediatric services |
| Young Type 2 dashboard – (Blood pressure TT achievement) | England, ICS, Sub ICS | Type 2 | 0-40 years |
| NPDA online – micro and macrovascular disease risk factors NPDA Type 2 spotlight report – full range of risk factors/ co-morbidities/ complications | Unit, ICS, network, and region National, region | Type 2 | 0-24 years cared for in paediatric services |
| QOF – nephrology/ CVD/ HTN QOF 2021-22 | NHS Digital | Practice level | All types | Adults |
Patient and family experience
What do children and young people and their families think of local paediatric diabetes services?
| Where to find the data | Geography level | Diabetes level | Age breakdown available |
|---|---|---|---|
| NPDA PREM: National Paediatric Diabetes Audit (NPDA) PREM report | RCPCH Link to data tables | Unit, ICS, Region, and Network level | All types combined | 0-24 years cared for in paediatric services |
Pregnancy preparedness
How well prepared for pregnancy are women with diabetes living in your region?
How does the quality of antenatal care, and pregnancy outcomes compare between local provider trusts and your region?
| Where to find the data | Geography level | Diabetes level | Age breakdown available |
|---|---|---|---|
| National Pregnancy in Diabetes audit dashboard (2018-2020) | Region and Provider level | Type 1 and Type 2 | All ages of or women with diabetes who are pregnant or planning pregnancy |
Excess weight and obesity
What percentage of children in your area are overweight or obese?
| Where to find the data | Geography level | Diabetes level | Age breakdown available |
|---|---|---|---|
| OHID Public Health Profiles: Obesity Profile – OHID (phe.org.uk) | National, region, LA | N/A | Reception: age 4-5yrs Year 6: age 10-11yrs |
Appendix 3: QOF indicators relevant to young adult diabetes care
Descriptor | |
|---|---|
|
DM006 |
The percentage of patients with diabetes, on the register, with a diagnosis of nephropathy (clinical proteinuria) or micro-albuminuria who are currently treated with an ACE-I (or ARBs). |
|
DM012 |
The percentage of patients with diabetes, on the register, with a record of a foot examination and risk classification: 1) low risk (normal sensation, palpable pulses), 2) increased risk (neuropathy or absent pulses), 3) high risk (neuropathy or absent pulses plus deformity or skin changes in previous ulcer) or 4) ulcerated foot within the preceding 12 months. |
|
DM014 |
The percentage of patients newly diagnosed with diabetes, on the register, in the preceding 1 April to 31March who have a record of being referred to a structured education programme within 9 months after entry on to the diabetes register. |
|
DM017 |
The contractor establishes and maintains a register of all patients aged 17 or over with diabetes mellitus, which specifies the type of diabetes where a diagnosis has been confirmed. |
|
DM020 |
The percentage of patients with diabetes, on the register, without moderate or severe frailty in whom the lastIFCC-HbA1c is 58 mmol/ mol or less in the preceding 12months. |
|
DM021 |
The percentage of patients with diabetes, on the register, with moderate or severe frailty in whom the lastIFCC-HbA1c is 75 mmol/ mol or less in the preceding 12months. |
|
DM023 |
The percentage of patients with diabetes and a history of cardiovascular disease (excluding haemorrhagic stroke) who are currently treated with a statin. |
|
DM033 |
The percentage of patients with diabetes, on the register, without moderate or severe frailty in whom the last blood pressure reading (measured in the preceding 12months) is 140/90 mmHg or less (or equivalent home blood pressure reading). |
|
NDH002 |
The percentage of patients with non-diabetic hyperglycaemia who have had an HbA1c, or fasting blood glucose performed in the preceding 12 month. |
Appendix 4: care processes
Key health checks
Health checks (care processes) for children and young people with diabetes are essential for early recognition of complications. There are different health checks depending on which type of diabetes has been diagnosed and dependent on age (see figure 17).
The graph below (see figure 18) shows the percentage of children and young people who completed a full year of care recorded as receiving individual health checks between 2004/5 and 2021/22. This data is from the NPDA 2021/22 care processes and outcomes annual report.
Comparisons of completion rates prior to 2015/16 should be reviewed with caution as they included both Type 1 and Type 2 diabetes.
However, given that most children and young people reported to the audit have Type 1 diabetes, the improvements in completion rates are likely to reflect real improvements in health check completion and/or completeness of data submitted to the NPDA.
The below graph (see figure 18) shows that the decline in health check completion rates recorded in the 2020/21 audit has largely reversed, although each rate remains below its pre-pandemic peak.
Figure 17: Recommended care processes for children and young people with diabetes
Type 1 (12 years and over) | Type 2 (Under 12 years) | Type 2 (12 to 18 years) | Type 2 (19 years and over) |
|---|---|---|---|
6 key health checks: HbA1cblood pressure albuminuria BMI thyroid test foot check Also: eye check | HbA1c blood pressure albuminuria BMI cholesterol
| HbA1c blood pressure albuminuria BMI cholesterol foot check eye check | HbA1c blood pressure albuminuria BMI cholesterol foot check eye check smoking status creatinine |
Figure 18: Percentage of children and young people who completed a full year of care recorded as receiving individual health checks between 2004/5 and 2021/22.
Line chart showing the percentage of children and young people who completed a full year of care recorded as receiving individual health checks between 2004/5 and 2021/22. Percentages largely increased each year for each health care type (HbA1c, blood pressure, BMI, urinary albumin, cholesterol, eye screen, foot exam, thyroid). A noticeable decline can be seen for each health check in 2020/21, this has since reversed but each rate remains below its pre-pandemic peak.
Appendix 5: different types of technology
Continuous glucose monitors
A continuous glucose monitor, or CGM, is a small wearable device that measures glucose levels in real-time. It uses a sensor to continuously send information to a handset or compatible mobile phone so that patients can see what their current levels are and whether they’re heading up or down. Patients can also set alarms to signal if their glucose levels are going too high or too low and see their glucose trends over time.
Patients attach a CGM directly onto their skin, usually on the upper arm or stomach. A short wire from a sensor goes under the skin and senses how much glucose there is in the fluid between the blood vessels and cells (interstitial fluid). A transmitter then beams this information to a receiver, which might be a handset, a compatible mobile phone or compatible insulin pump.
With real time CGM patients can see glucose readings at any time. Some CGMs are intermittently scanned, commonly called ‘flash’ glucose monitors, and allow patients to scan a sensor attached to their body to get their latest glucose readings.
Sensors are changed every 7 – 14 days depending on the brand. Patients should always have a blood glucose meter and test strips as a back-up.
Insulin pumps
Insulin pumps are electronic devices that release pre-programmed amounts of rapid acting insulin regularly through the day and night. This acts like basal or background insulin. Patient can change the delivery of insulin according to any activity they do, the carbohydrate or fat content of food consumed or to bring down high glucose levels.
Patients wear the pump all the time.
There are 2 types of insulin pump:
- A ‘tethered’ pump uses a fine tube to connect the pump to the cannula; the pump is worn in a pocket or clipped to a belt.
- A patch pump or micro pump has no tubing or a very short tube, and the pump is usually stuck on to the skin. Patients will still need to carry pen and cartridge insulin as a back-up, so they can do insulin injections if needed.
Hybrid closed loop systems
A hybrid closed loop system (HCL) is where a continuous glucose monitor (rtCGM) and an insulin pump ‘talk to each other’ through a computer program (algorithm). Some of a patient’s insulin doses are adjusted automatically in response to their glucose levels, as glucose is monitored all the time by the rtCGM. Patients’ will still need to tell the system when they eat.
HCL systems can help prevent or minimise hyper and hypo situations. The algorithm will stop insulin delivery if it thinks a patient is going below target. This is usually set between 5.5 and 6.1mmol/l. Patient will still need to carry pen and cartridge insulin as a back-up, so they can do insulin injections if needed. HCL systems are only recommended if they are procured at a cost-effective price agreed by the companies and NHS England.
Appendix 6: newly diagnosed patients: first year of care pathway
At diagnosis. Patient centred sessions
- Explanation of diabetes and treatment*
- Practical skills*
- Food, CHO awareness and diabetes*
- Glucose targets, Insulin, Food and physical activity*
- Hypo management*
- Promote positive and consistent messages regarding diet and body image
- Diabetes at home and school
- Diabetes during illness/DKA
- Preparing for home (consider advance technology as per national guidance)
* = Essential prior to discharge/at diagnosis Diabetes team to map the above on current education package and knowledge assessment check list using verbal, written and video resources. Family to be provided with emergency contacts (out of hours etc)
Within the first week (Diabetes team)
- family provided with any relevant diabetes resources
- ensure expectations are given to recording blood glucose, insulin and food data (diary or electronic)
- check biographical details
- check family email address
- set up download account, link to any relevant apps and bolus advisor apps
- set up to relevant education apps (e.g Digibete, DeApp)
- signpost to emotional resources (JDRF, MindMate, DUK, Digibete)
- give details regarding next appointments
- allocation of named nurse or key worker
- psychology contact – phone, leaflet, meet and greet if possible
- school care plan completion, training of school staff and contact made with school – ensure completion before returning to education (as per local guidance)
- education on glucagon and training (if not completed at diagnosis)
Within first 2-6 weeks
Follow the core clinic components plus:
- MDT clinic review
- dietetic review
- meet diabetes team psychologist
- level 3 CHO Counting (if not already achieved)
- Set up to relevant education apps (e.g Digibete, DeApp)
- review of screening blood results taken at diagnosis
- explanation of routine diabetes care/ annual review/ retinal screening/ HbA1c/ clinic targets/ time in range/ understanding of DKA/ discussion around complications of diabetes
- information on DLA
- pre-emptive discussion around remission phase and changing insulin requirements
At 3 months: OPA (HbA1c)
Follow the core clinic components plus:
- how to assess and optimise time in range (if applicable)
- advanced education of diabetes management
- discuss HbA1c targets
- discuss the impact of diabetes on the relationship with food and activity
At 6 and 9 months: OPA (HbA1C)
Follow the core clinic components plus:
- explore data review and support/ encourage changes based on self-analysis (if possible)
- patient centred/led discussion
- introduce Goals of Diabetes (or equivalent) and annual review
- review education, knowledge and understanding
- pre-emptive discussion around remission phase and changing insulin requirements
At 12 months: OPA (HbA1C)
Follow the core clinic components plus:
- explore data review and support
- encourage CYP/ families to identify 2 relevant educational refreshers e..g CHO counting, hypo management
- discuss and complete annual care processes – follow up with a discussion around complications of diabetes
- review education on sick day rules and ketone testing
- dietetic review
- promote positive and consistent messages
Underpinning the newly diagnosed first year of care pathway are the ongoing care elements shown below
On-going support between MDT clinics
Examples include:
- telephone contacts by named nurse and dietitian
- joint CDSN/Dietitian review
- electronic or written data review – blood glucose, insulin and food data
- introduction to data review and support – Set expectations of regular self-review of downloading
- follow up with school (as required)
- school menus – consideration of CHO counting at school (as per local guidelines)
- follow up with healthy eating, CHO counting, fat and protein and glycaemic index
- exercise and physical activity
- check emotional wellbeing
- support for travel/staying away from home
- information on relevant peer support groups
Core clinic components
- Celebrate successful behaviours!
- MDT clinic review
- Data review including HbA1c targets, time in range
- Discuss data review and support accordingly (including dietetic review)
- Check ability to share data remotely
- Consider advanced technology as per national guidance
- Check wellbeing and identify any changes – emotional support resources
- Promote positive and consistent messages regarding diet and body image – use available resources
- Promote healthy lifestyle including food and activity
Diabetes care, aims and objectives
- HbA1c ≤ 48mmol/mol (by 6 months and maintained)
- average 14 day glucose < 8mmol/l (sensor data)
- standard Deviation < 3.0 (sensor data)
- time in range (4-10mmol/L), (based on 70% sensor usage)
- ensure patient centred/led care
- work in partnership with the CYP and their family
- to discuss at each clinic and consider options to facilitate target achievement:
- technology use incl. pump therapy, FGS/CGM, Hybrid closed Loop
- education required (developmental/ age appropriate)
- promote regular data review by CYP/families
- extra appointments/referrals (for example, social care, psychology)
- injection and infusion sites
- early help referral
Celebrate successful behaviours! (Not specifically achieving targets)
References and useful links
NHS England
- NHS Long Term Plan 2019
- Paediatric diabetes best practice tariff
- Diabetes Transition Service Specification (2016)
NICE
All NICE products on diabetes
- NG17: Type 1 diabetes in adults: diagnosis and management
- NG18: Diabetes (type 1 and type 2) in children and young people: diagnosis and management
- NG28: Type 2 diabetes in adults: management
- NG43: Transition from children to adults’ services for young people using health or social care services
- TA943: Hybrid closed loop systems for managing blood glucose levels in type 1 diabetes
- QS167: Promoting health and preventing premature mortality in black, Asian, and other minority ethnic groups
- QS208: Type 1 diabetes in adults
- QS209: Type 2 diabetes in adults
Useful links
- Diabetes UK
- JDRF: Improving lives. Curing Type 1 diabetes
- NHS Futures: The National Diabetes Programme. Children and Young Adults with Diabetes
- NHSFutures – National RightCare: https://future.nhs.uk/NationalRightCare/grouphome
- NHS England: Model Hospital
Enablers
Funding
Guidelines
Evidence and other resources
See section within this toolkit on the Best Practice Tariff
See section within this toolkit on the Quality and Outcomes Framework NHS England.
Quality and Outcomes Framework – Guidance for 2023/24 QOF quality improvement case studies
System leadership
Guidelines
NHS England
Evidence and other resources
NHS England
Changing healthcare cultures – through collective leadership, The Culture and Leadership Programme
See Appendix 2 on data resources and also refer to the NPDA and NDA dashboards.
Office for Health Improvement and Disparities (formerly PHE): Making Every Contact Count (MECC): practical resources
Data
Guidelines
NHS England
Evidence and other resources
Refer to the NPDA and NDA dashboards.
Nottingham and Nottinghamshire Integrated Care System: PHM Diabetes Pack RCPCH. NPDA results online, Interactive reporting tool for the NPDA.
See Appendix 1 on data collections and Appendix 2 on data resources
Healthcare Quality Improvement Partnership:
- NPDA Report on care and outcomes 2022/23
- National paediatric diabetes audit admissions report 2015-2020
Workforce
Guidelines
NHS England:
Evidence and other resources
NHS England:
- Paediatric diabetes best practice tariff (2023/25)
- Service level demand and capacity planning
- e-learning for healthcare
Diabetes UK:
- Training and Competencies resources
Royal College of GPs:
- Learning Hubs – Diabetes Hub e-learning resources
Area of focus 1: addressing diabetes health inequalities
Equitable services
Guidelines
NHS England:
- Guidance for NHS commissioners on Equality and Health Inequalities legal duties
- Equality Frameworks and Information Standards
- Core20PLUS5 – An approach to reducing health inequalities in children and young people
- National Healthcare Inequalities Improvement Programme
- Reasonable adjustments
- Sensory friendly resource pack
NICE:
Evidence and other resources
Digibete: A video platform and app to help young people, families, and communities to manage their diabetes. See links for specific resources for Type 1 and Type 2 Diabetes UK: Tackling Inequality Commission Report (2023)
The Association for Young People’s Health (AYPH): Understanding the experiences of young people with type 1 diabetes from communities that experience marginalisation (2023)
Children North East Poverty Proofing©:
- Common Themes Poverty Proofing© Paediatric Diabetes Care (2023)
- Poverty Proofing© Paediatric Diabetes Workforce Guide
Baksh, R. A., Gulliford, M., Chauhan, U., Sheehan, R., Strydom, A. Onset and Care of Type 2 Diabetes Mellitus in People with a Learning Disability – A LeDeR deep dive (2023, KCL unpublished report).
Equitable access to technology
Guidelines
NICE:
Evidence and other resources
Risk factors associated with Type 2 diabetes
Guidelines
NICE:
Evidence and other resources
Kings College London:
- Addressing health inequalities through co-developing the Healthy Eating and Active Lifestyles for Diabetes (HEAL-D) programme
NHS England:
Area of focus 2: reduce variation in treatment, care, and outcomes across systems
Quality oversight
Evidence and other resources
- See Appendix 2
- James Paget University Hospital’s Paediatric Diabetes Team case study. A start to our QI journey: High HbA1c support clinics at JPUH
Timely and accurate diagnoses
Guidelines
NICE:
Evidence and other resources
- DiabetesGenes – Information for patients and professionals on research and clinical care in genetic types of diabetes
- RCPCH: National Paediatric Diabetes Audit (NPDA) Hospital admissions and complications reports 2011-2020
- CYP transformation programme dashboard
- See Appendix 2 DKA at diagnosis metrics Diabetes UK: 4Ts awareness campaign
Structured education and peer support
Guidelines
NICE:
Evidence and other resources
- Digibete: A video platform and app to help young people, families, and communities to manage their diabetes. See links for specific resources for Type 1 and Type 2
- Structured Education Programmes: DAFNE for T1 and DESMOND for T2.
- Diabetes UK
- Learning Zone has free online courses for adults but some specifically for parents and carers of children with type 1 diabetes
- Diabetes UK Together Type 1 programme; and Local Support Groups.
First year of care
Guidelines
Evidence and other resources
See Appendix 6 or visit the National Children and Young People’s Delivery Network website for more details.
Preventing hospital admissions
Evidence and other resources
See Appendix 2 on data resources and also refer to the NPDA and NDA dashboards. See Appendix 2. DKA in established patient metrics.
Retinopathy
Guidelines
NICE:
- GID-NG10256. Diabetic retinopathy (Guideline in development, expected publication Feb 2024)
- NG18 Diabetes (type 1 and type 2) in children and young people
GOV.uk:
Evidence and other resources
NHS England:
FutureNHS:
- Diabetic Eye Screening page (sign up and login in required)
Dental care
Guidelines
NHS England:
NICE:
Evidence and other resources
NHS: Find a dentist
Office for Health Improvement and Disparities (formerly PHE). The relationship between dental caries and body mass index – child level analysis
Treatment technology
Guidelines
NICE:
- NG17 Type 1 diabetes in adults: diagnosis and management
- NG18 Diabetes (type 1 and type 2) in children and young people: diagnosis and management
- NG28 Type 2 diabetes in adults: management
- Quality statement 4: Continuous glucose monitoring in type 1 diabetes
- TA943 Hybrid closed loop systems for managing blood glucose levels in type 1 diabetes
Evidence and other resources
See Appendix 2
NHS England. Decision support tool: making a decision about managing type 1 diabetes
RCPCH Audits. National Paediatric Diabetes Audit (NPDA) Report on Care and outcomes 2021/22. (Case study: Supporting families to adopt using a closed loop system)
Mental health and well-being
Guidelines
NHS England. Adult Eating Disorders: Community, Inpatient and Intensive Day Patient Care – Guidance for commissioners and providers
The Royal College of Psychiatrists. Medical Emergencies in Eating Disorders: Guidance on recognition and management. College Report CR33
Evidence and other resources
NHS England. The 6 principles of good peer support for people living with Type 1 diabetes
Sachar A, Breslin N, Ng SM. An integrated care model for mental health in diabetes: Recommendations for local implementation by the Diabetes and Mental Health Expert Working Group in England. Diabet Med. 2023; 40:e15029. doi:10.1111/dme.15029
Area of focus 3: improve treatment and care for those transitioning from paediatric to adult services
Preparation for transfer and transition
Guidelines
NHS England:
- NG43 Transition from children’s to adults’ services for young people using health or social care services
- QS140 Transition from children to adults’ services
Evidence and other resources
Child Health Clinical Outcome Review Programme. The Inbetweeners – a review of the transition from CYP into adult health services
Quality Improvement Collaborative: Report on the National Diabetes Transition Audit (NDTA)
Colver A, Rapley T, Parr JR, McConachie H, Dovey-Pearce G, Le Couteur A, McDonagh JE, Bennett C, Maniatopoulos G, Pearce MS, Reape D, Chater N, Gleeson H, Vale L. Facilitating transition of young people with long-term health conditions from children’s to adults’ healthcare services – implications of a 5-year research programme. Clin Med (Lond). 2020 Jan;20(1):74-80
Doncaster and Bassetlaw Teaching Hospitals. Case Study: How does one solve a problem like transition – the ups and downs…
Integration of paediatric and young adult services
Guidelines
Evidence and other resources
NHS England. Integrated care resources
Young adult care
Guidelines
Evidence and other resources
NHS England. Adolescent and Young Adult Type 1 Diabetes Audit (2017-21) pages and interactive dashboard
Royal Liverpool and Broadgreen University Hospitals NHS Trust (2018). Young Adult Diabetes: Engaging to improve; outcomes of the young adult clinic restructure
Holman N, Woch E, Dayan C, Warner J, Robinson H, Young B, Elliott J. National Trends in Hyperglycaemia and Diabetic Ketoacidosis in Children, Adolescents, and Young Adults With Type 1 Diabetes: A Challenge Due to Age or Stage of Development, or Is New Thinking About Service Provision Needed? Diabetes Care. 2023
Contraception and pregnancy planning
Guidelines
NICE:
- NG3 Diabetes in pregnancy: management from preconception to the postnatal period
- QS109: Diabetes in pregnancy, quality statement 1: Preconception planning
Evidence and other resources
International Diabetes Federation – IDF Diabetes Atlas 2021
Area of focus 4: improve treatment and care for children and young adults with Type 2 diabetes
Prevalence
Guidelines
Evidence and other resources
Refer to the NPDA and NDA dashboards.
See Appendix 2 Office of Health Improvement and Disparities (OHID): Public Health profiles
Healthy lifestyle support
Guidelines
NICE:
Evidence and other resources
Walsall Healthcare NHS Trust. NICE Fellowship project to facilitate the implementation of NICE guidance PH38 via the utilisation of Tier 2 and Tier 3 weight management and lifestyle-intervention programmes for the prevention of type 2 diabetes
T2DAY: Type 2 diabetes in the young
Guidelines
NHS England: NHS rolls out world-first programme to transform diabetes care for under 40s
Evidence and other resources
Misra S, Gable D, Khunti K, Barron E, Young B, Kar P, Valabhji J et al., 2022, Developing services to support the delivery of care to people with early-onset type 2 diabetes, DIABETIC MEDICINE, Vol: 39
Misra S, Ke C, Srinivasan S, Goyal A, Nyriyenda MJ, Florez JC, Khunti K, Magliano DJ, Luk A. Current insights and emerging trends in early-onset type 2 diabetes. Lancet Diabetes Endocrinol. 2023
Yamamoto JM, Hughes DJF, Evans ML, Karunakaran V, Clark JDA, Morrish NJ, Rayman GA, Winocour PH, Hambling C, Harries AW, Sampson MJ, Murphy HR. Community-based pre-pregnancy care programme improves pregnancy preparation in women with pregestational diabetes. Diabetologia. 2018 Emerging Risk Factors Collaboration. Life expectancy associated with different agesat diagnosis of type 2 diabetes in high-income countries: 23 million person-years of observation. Lancet Diabetes Endocrinol. 2023