Introduction
Effective care navigation requires careful consideration and planning. This guide is for general practice teams who are seeking to improve the care navigation processes in their organisation.
Care navigation is a commonly used term that means different things to different people. It is sometimes used interchangeably with ‘signposting’, ‘triage’ or ‘digital triage’. Throughout this guide, we use the term ‘care navigation’ to cover all these meanings. Care navigation describes any process where patients:
- contact a practice for help
- provide information about their query
- are assessed and prioritised based on need
- are allocated to the most suitable person, team or service to help them
This guide has been developed by the national Primary and Community Transformation and Improvement team. It has involved extensive consultation over a long period of time and takes into account perspectives from many general practice staff members. If you have a question or feedback about this guide, you can email the team at england.pctgpip@nhs.net.
How care navigation can help
General practice faces significant challenges due to increasing demand and complexity of work.
Care navigation can help if:
- patients are complaining about access
- you are experiencing high staff burnout and turnover
- you are running out of appointments too early in the day
- patients who need your service are not accessing it
- patients are not getting to the right person first time
- you are struggling to prioritise continuity of care
- you want to make the most effective use of your team
This guide helps you to understand and improve each aspect of your care navigation approach in 5 sections: understand, plan, prepare, implement and sustain. You can use the supporting project plan for improving care navigation alongside this guidance.
Benefits of effective care navigation
Care navigation is a critical part of the modern general practice model, which supports a safer, more equitable and more sustainable general practice.
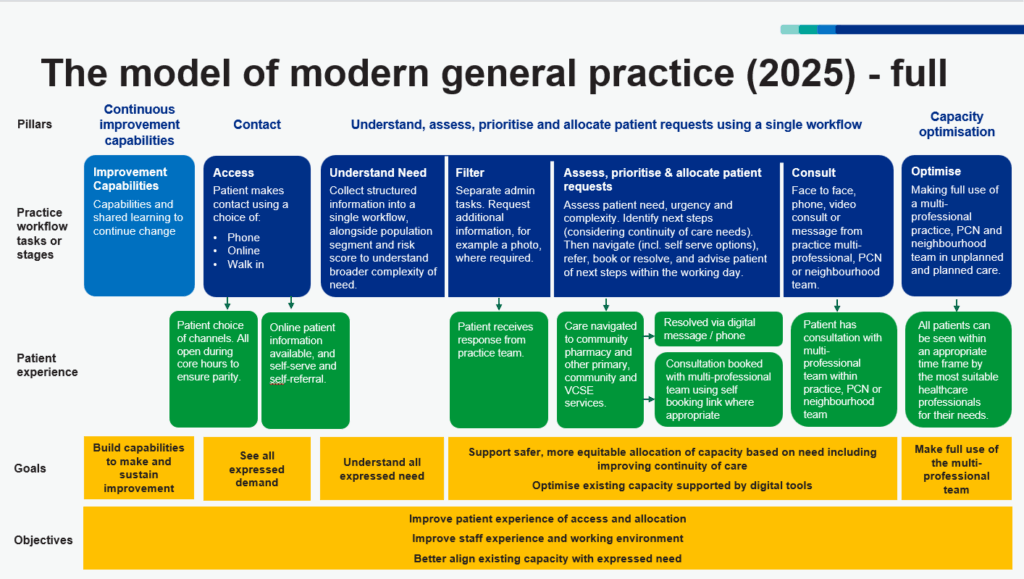
Figure 1: Modern general practice model (updated August 2025)
Figure 1 shows the model of modern general practice. The model’s objectives are to improve patient experience of contact, assessment and allocation, improve the working environment for staff and better align capacity with need.
Patients have a choice of 3 contact routes to general practice: phone, online and walk in. The practice collects structured information from the patient when they make contact. The patient’s needs (including continuity of care) are assessed and they are then allocated to an appropriate healthcare professional or service for their needs within an appropriate timeframe and using an appropriate consultation modality.
The assessment considers the:
- right timeframe
- prioritisation
- best way to communicate with the patient
- most suitable mode of consultation, for example face to face or phone
- need for continuity of care
This is a move from ‘first come, first served’ to a fairer and safer model for patients which puts you back in control of your work. You and your patients will feel the benefits of:odel for patients which puts you back in control of your work. You and your patients will feel the benefits of:
- a safer process
- a fairer process for patients
- a more efficient use of your patient-facing team
- better use of your multi-professional team
- time freed up to focus on proactive care rather than reactive care
Related guidance
This guide is 1 of 5 modern general practice ‘how to’ guides available on the resources page for the national General Practice Improvement Programme. The other 4 are:
- how to align capacity with demand in general practice
- creating highly usable and accessible GP websites; includes supporting patients who choose to use online channels
- how to improve telephone journeys in general practice
- how to improve care related processes in general practice
This guidance supports practices that want to improve their care navigation process. You can follow the guidance end to end if you want to create an entire care navigation process from scratch. If you already have a care navigation process in place but want to improve or add certain elements, you can simply dip into the relevant sections.
1. Understand
Benefits and key steps
Many of the elements of the modern general practice model will reflect what you are already doing. By carefully assessing your current situation, you can save valuable time later. This helps you:
- recognise what’s working well
- understand your existing problems in greater depth
- prioritise your actions
- feel in control
The key steps in the understand section are to:
- complete the assessment tool for modern general practice
- map your existing processes
- understand current staff experiences and perspectives
- understand current patient experiences and perspectives
- measure your demand and capacity
- audit your avoidable appointments
- review your starting point
Assessment tool for modern general practice
Completing this assessment tool for modern general practice will help you:
- examine your care navigation process
- understand what you are doing well
- identify areas for improvement
- prioritise your improvement activities
We recommend completing this assessment before starting any improvement work, to clearly establish the point from which your work should begin.
Start using the assessment tool for modern general practice.
Top tip
The assessment tool for modern general practice is flexible and works for your unique practice and patient population. It’s not a rigid set of rules, but a guide to help you understand your current situation.
Map your existing processes
To understand ‘how things get done around here’, it is helpful to create a process map. Your process map should detail all the steps in a patient’s journey through your practice. This guide to conventional process mapping can help if you’ve not done this before or would like a reminder.
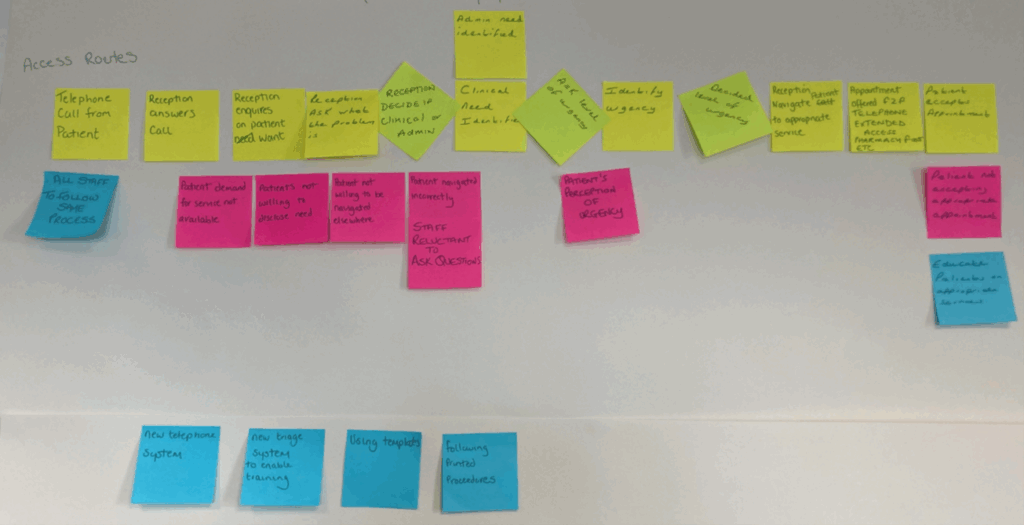
Figure 2: A process map created in a practice
The photograph in Figure 2 is of a process map created in general practice. It shows the process starting with a patient contacting the practice by telephone, through to being allocated an appropriate appointment for their need.
This care navigation process mapping tool may be a useful starting point.
Things to consider when mapping your existing access and allocation processes are:
- involve both staff and patients in the creation of your map
- start at the point the patient contacts the practice
- finish when the patient is allocated to the appropriate person or service
- identify all your patient contact channels and create a separate map for each process to start with. They may come together at some point
- decide what level of detail will help you most
- add timelines to show how long each step in the process takes. This will help you check that each patient contact channel is managed equally
- include how and when you currently:
- gather and record information
- prioritise patients into appointments
- manage continuity of care
- allocate patients to available options to meet their need
- communicate with patients throughout the process
Review the map you have created and consider:
- where does the process work well?
- where is it inefficient?
- where is it difficult for patients to navigate, especially the more vulnerable?
- where can it be improved?
- what rules or assumptions are being followed as part of this process?
- are any steps missing or duplicated?
- how do staff experience this process?
- how do patients experience this process?
Involve the staff who are currently care navigating in the creation of your process map. They will be able to tell you what really happens and how it feels to undertake the process. They may also give you ideas for how the process could be improved, both for themselves and for the patients.
Current staff experiences
Knowing the needs of your staff at each stage of your care navigation process is key to success. They understand the details of how and why they do what they do and the impact any changes will have on them. Capturing the experiences and perspectives of your staff will help you understand any barriers to implementing a new process. It will also help you gain buy-in from staff, which in turn will help get buy-in from patients.
Current patient experiences
Making your care navigation process useful and usable to patients means they are more likely to use them as intended. Engage with patients at the start to understand what they need from the care navigation process. This will:
- flag any potential issues you may not have considered
- shape what to include in your patient communications and how your patients like to be communicated with
Include patients who are more likely to struggle to access your practice. If your process works well for them, it is more likely to work for everyone. You can involve your patient participation group, conduct a short survey or hold an open session.
When engaging patients:
- explain the situation from your perspective
- be honest about your concerns
- listen carefully to their concerns and perspectives
- respect their opinions
- make the process of engagement as easy as possible
- think carefully about the questions that only your patients can answer
Top tip
Questions that only your patients can answer might include:
- What do they find frustrating or confusing about the current system and why?
- What concerns do they have about contacting the surgery online? Why might they be reluctant to use online channels? Would they want to contact the surgery in different ways for different purposes?
- How could each part of the care navigation process be made easier for them to engage with?
Measuring demand and capacity
Measuring demand
To improve your care navigation system, you must understand the total demand coming into the practice each day. Demand will vary depending on the day of the week and the hour of the day, so it is important to break the data down to this level.
When thinking about the demand your care navigators must manage, consider exactly what they do. For example, if they manage every request that comes into the practice, you should measure the total number of:
- phone calls answered (available through your cloud-based telephony)
- online contacts received (available through your online consultation system)
- patients attending at the front desk (you will need a manual tally)
However, if your care navigators only manage requests for help for a medical problem, you should measure the number of:
- phone calls from patients requesting an appointment or help for a medical problem
- online contacts requesting an appointment or help for a medical problem
- patients attending at the front desk requesting an appointment or help for a medical problem
Exactly what you measure will depend on how your practice works. These measures need to reflect the demand your practice is meeting.
Top tip
Patients should be able to contact the practice through any of the contact channels (phone, online or walk in). However, to manage the demand sustainably you need to record all information about patient requests in a single digital template and/or pass them through the same workflow. This avoids running multiple, parallel workflow processes. It means practices can assess and allocate the demand equitably and safely with a full view of the incoming need and practice capacity. It also helps to build up good data on the nature of all demand and which role or service patients were allocated to.
Evidence shows that total demand is predictable and finite. When you improve your contact channels so they are easier for all patients to use, even those who might have previously struggled, they are more likely to use them. This means that in some cases there may appear to be additional demand. In reality the extra demand was always there but was not expressed due to difficulty with access for some patients. The good news is that practices using online access as part of an improved care navigation process have found this perceived increase is temporary and will settle. The evidence shows a shift from phone to online contacts rather than an ‘opening of flood gates’.
Top tip
When changing your care navigation process, you need to allow a buffer for unmet demand in your calculations of total demand. We recommend adding 10% to your measurable demand. Hold your nerve, demand will settle into a predictable pattern once the unmet demand has filtered through.
Measuring capacity
You need to understand the capacity you have to meet the demand. Capacity should include your care navigators and your clinical workforce.
Decide how many requests an hour your care navigators can manage. Base this on the number of requests they could realistically handle in a standard or average day and use it to calculate your care navigator capacity. The number of requests handled an hour may vary depending on who is doing your care navigation, their experience and the complexity of the requests they are dealing with. Remember to factor in the flexibility of your care navigator capacity, including annual leave requirements and sickness levels. Demand will likely fluctuate across the day or week, so you should review how to match your capacity to peaks in demand.
Similarly you need to decide how long each type of appointment needs to be and from this calculate your exact clinical capacity. This is covered in ‘Align your appointment book’ in section 3: Prepare. Remember to count numbers of appointments. Numbers of sessions does not provide sufficient granularity to be meaningful.
There is further information in the How to align capacity with demand in general practice guide.
Audit your avoidable appointments
An audit of potentially avoidable appointments can help you understand the effectiveness of your care navigation processes, where improvements can be made and where additional services or roles may be beneficial.
Ask all your clinicians to assess every appointment they undertake over 1 to 2 weeks. This should include face-to-face, phone and written consultations. They should record:
- whether they were the best person to deliver that appointment
- if they weren’t, who was? (clinicians should answer this question as if they had access to every available role or service, even if that role or service is not currently available in their practice)
- whether the urgency and mode of consultation was appropriate
- whether continuity of care was required or beneficial in that appointment and whether the patient received this
Review your starting point
It is important to understand all the information and data you have gathered before planning your next steps.
The assessment tool for modern general practice and your current state process map will show:
- if you have all the elements required for effective care navigation
- how well you manage these elements
- if all your contact channels (phone, online and walk in) are open during your contracted hours for both clinical and admin requests
- what needs to be added or removed to improve your process
Your staff and patient perspectives will reveal:
- what matters most to your patients
- how your process flows
- how it feels to be part of that flow
- what works well already
- what may need to change to create a better experience
From your data collections you will have quantified the total demand on your care navigators, your current available capacity and your avoidable appointments. From this you will understand:
- whether there is enough capacity to safely meet demand
- whether there are times in the day or week when demand drops and capacity exceeds demand
- how you can plan your staffing through the day or week
- whether you need to make better use of the skills in your multi-professional team
- whether you need to make better use of external services
Take these findings into the ‘plan’ section of this guide.
2. Plan
Benefits and key steps
You should create a detailed plan to keep your work on track and focused. This should include:
- where you are going and what good will look like when you get there
- resources you need for the journey: both digital tools and a good understanding of the skills and capacity you need
- actions to take and activities to engage everyone along the way
- clinical safety considerations
- equity, efficiency and effectiveness elements
The key steps in the Plan section are to:
- involve both admin and clinical staff in planning to generate commitment and a sense of ownership
- involve patients in planning
- map a proposed new care navigation process
- consider what you need digital tools to do
- ensure you are creating a consistent patient experience
- review how you capture information from patients
- plan how to make decisions about allocation of patients
- assess the need for urgency versus continuity of care
- complete a skills matrix for the staff in your practice
- create a directory of services identifying the external services available to your patients
- check your proposed new process is safe for patients and staff
- define how you will measure the success of your changes
Involve staff in planning
When planning improvements to your care navigation, staff need to understand why change is needed and what the benefits will be for them and for patients. It’s vital to create a space where everyone can share what is important to them in this change and by bringing perspectives together in a way that is meaningful to all and creates a shared purpose. This will encourage the team’s ownership of and commitment to the change.
Identify the skills you think you need to make the improvement. These may vary depending on exactly what you are trying to do.
It is useful to identify staff who have skills in:
- improvement leadership – for example, quality improvement and change management
- planning practice changes and project management
- measuring success and improvement
- extracting and analysing data from your digital systems
- clinical safety
- training frontline staff in customer service skills
Many staff have useful experience from outside general practice. You may discover some untapped potential in unusual places. Identifying an administrative and a clinical champion can help. So can involving a representative group of staff in the improvement work.
Creating your care navigation process with both clinical and administrative staff gives all roles the opportunity to:
- express their views
- contribute suggestions
- identify any inconsistencies or workarounds in place
- identify the impact any proposed changes may have
- identify how they can improve their use of digital tools
Before you begin, ensure you have buy-in from your senior practice leaders. They need sufficient understanding of the purpose and the benefits to give the go ahead for the planned improvements.
Top tip
NHS Impact has more information on creating a shared purpose.
Involve patients in planning
By now, you should have asked your patients for feedback on their experience in accessing your practice.
You should now ask a representative group of patients what they think you need to do to improve your process. We recommend that this group work closely with the staff doing the improvement work.
Map a proposed new process
Effective care navigation should:
- require that there is available access through all contact channels during contracted hours
- allow patients to choose the contact channel they use
- review all patient requests consistently using the same, single process, from the first to the last contact of the day
- provide equitable management of patient requests based on patient need
- enable maximum use of all available staff and services to appropriately manage each patient’s need
- use digital tools to increase efficiency and effectiveness and reduce pressure on phone lines
- be safe
We recommend that you map your desired new process, starting from when the patient contacts the practice and ending when they are allocated to the correct service to meet their need.
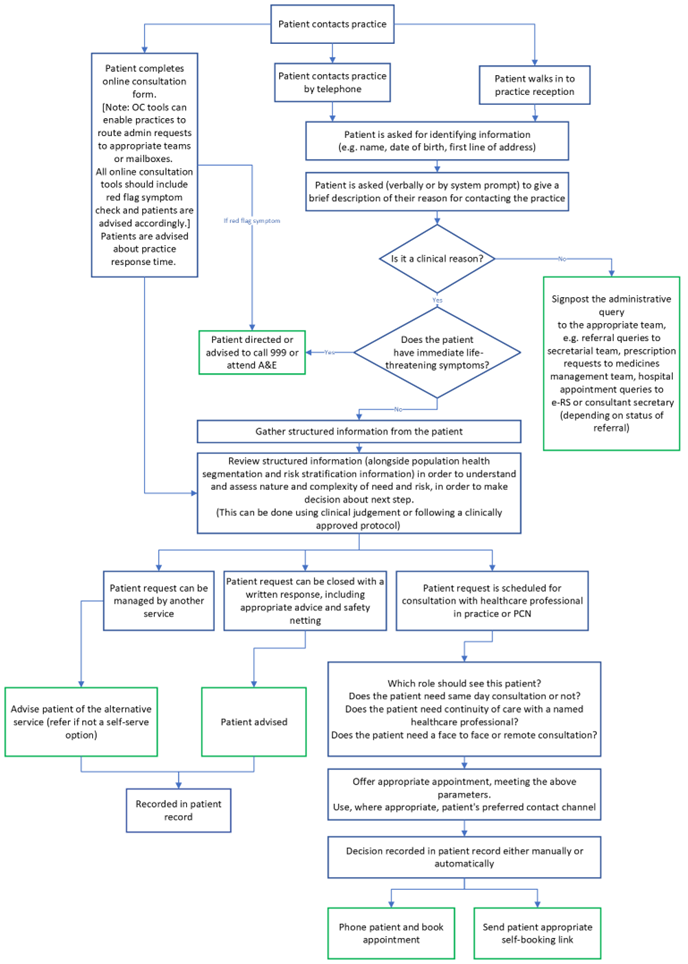
Figure 3: Example new process map, created using Microsoft Word
Figure 3 is an example of a high-level process map for managing all patient requests in a single way. It maps the steps from contact, through care navigation based on patient need, to outcome (which may include a general practice appointment or a referral to a more suitable service. You can use this example of a care navigation process diagram as a starting point.
You should consider the resources required to manage this process.
Choosing your digital tools
The digital tools that can support and enhance care navigation are:
- those that link to an online consultation tool, for example GP websites and the NHS App
- online consultation tools
- cloud-based telephony
- messaging tools
- tools that generate self-booking links for patients to choose and book an appropriate appointment
- tools that help identify patient complexity, for example population health segmentation and risk stratification tools
When mapping the steps in your process, consider checking what functions your online consultation or messaging tools offer to see if they meet your requirements.
The NHS England Step-by-step guide to improving general practice website online journeys can help you improve your GP practice website for patients.
Online consultation tools
Online consultation tools:
- provide patients with a means of requesting clinical and administrative help from their practice. These range from a simple form where patients can type a request, to more complex questions that follow preset pathways
- support practice staff to collect structured information on a patient’s presenting problem and how urgently it needs to be managed
- provide practice staff with the functionality to manage patient requests
We have extensively researched what patients and general practice staff need from online consultation tools (available on Futures which requires a login). Our report assesses and benchmarks 15 of the most used online consultation tools. It looks at their patient usability and accessibility and the features that matter most to practice staff.
Patients need online consultation forms to:
- be straightforward to access; in their preferred channel (web, app, etc)
- be straightforward to find and start; clearly labelled and ideally without the need to register or login
- be straightforward to understand what is required of them; no more reading than necessary, using written content that meets NHS guidance
- be straightforward to complete; questions written in plain English with no medical jargon, they can express all their needs easily and clearly
- set clear expectations; patients need to understand what will happen with this information and when and how they will receive a response
- be highly accessible; a patient’s end-to-end journey must be fully accessible
- be highly usable; journeys should be consistent with NHS design standards
Online channels should be managed in the same way as phone and walk in to increase confidence for those patients that choose to use them. Online channels that are accessible, easy to use and open during core hours will relieve pressure from managing phone lines and free these up for those who really do need to call the practice. The need to manage more channels can feel worrying to practices but you should remember that demand is finite.
Top tip
Test the whole online journey yourself on your mobile phone as this is the device most patients will use.
Phone systems
The functions in cloud-based telephony can enhance your care navigation by helping you to direct patients to the right place or person. These functions include:
- recorded messaging
- call routing
- call transfer
- dashboard data
- ‘call back’ function; patients may find it more convenient to be called back than wait on hold
How to improve telephone journeys in general practice has guidance on understanding and using practice call data, optimising your telephony, using telephony for continuous improvement and working at scale with telephony.
Top tip
Care navigators can find that access to phone headsets and dual screens is a big help to them.
A headset with a noise reducing microphone helps to cancel out any background noise for those on the call. You may need to check your phones have a USB port to connect the headset to.
Messaging and booking tools
Messaging tools provide important functions that support care navigators to:
- receive further information or actions from a patient for assessment or ahead of a consultation
- send a patient a link to self-book an appropriate appointment
- keep patients informed about what is going on and what to expect
- manage specific administrative requests, for example sending fit notes
Some of these functions can be provided by an online consultation tool and some require a separate messaging and booking tool.
Top tip
We recommend creating shared messaging templates for common processes. These can often be created by a primary care network (PCN) and then shared throughout the network.
Creating a consistent patient experience
The care navigation process begins with the patient contacting the practice for help. Consider carefully what information you need to share with the patient every time they contact the practice. This information should be clear and consistent across every contact channel.
Key messages may include:
- when you get in touch, we’ll ask what you need help with
- any information you share is confidential
- we will use the information you give us to agree the right person to help you
- however you choose to contact us, we may offer you a consultation face to face at the surgery, by phone or by text or email
Think about how your website or online consultation tool explains how patients should request help from the practice. Does that match what practice staff tell patients when they phone or walk in?
Top tip
The written content templates for GP websites have been developed with practices, the NHS Content team and have been tested with patients with low digital confidence and low levels of literacy and confidence in English.
Capturing structured information
This step enables you to filter, navigate and prioritise requests based on need. It increases your ability to close requests with a message or book the right consultation first time. It also helps clinicians to be ready with the right information to meet the patient’s need.
Structured information can be captured by:
- the patient or their carer completing an online form
- staff using a digital template on behalf of a patient (over the phone or in person)
Whichever capture method is used, the same structured information should be consistently collected across all contact channels. This supports patient choice and access needs. Information should be saved in the patient record, using appropriate codes where possible.
Across all channels, patients should be asked:
- patient’s age and sex and, if not the patient, who is providing the information, for example a carer?
- what problem do you need help with? What are your symptoms?
- how long have you had this? Is this a problem you’ve asked us about before?
- is it getting worse stayed the same or getting better?
- have you tried anything already?
- have you seen anyone about this in the practice or somewhere else?
- is there anything you want to tell us? Any ideas, worries or things you are expecting?
- would you prefer a consultation face to face or by phone, video or message?
- would you prefer to receive help from a particular healthcare professional? If so, who?
- are there times when you are not available?
- do you have any particular communication needs? For example, interpreter required, limited access to digital or phone (communication and access needs should be coded)
- confirmation of the patient’s phone number and if they have consented to receiving text messages if needed
You may find you need more information to assess and prioritise some requests. You may need to go back to the patient for this. As well as helping you, this can also reduce the number of times a patient needs to visit or contact the practice.
The practice can request or receive further information by:
- asking the patient to complete a standardised digital template, for example, for a suspected urinary tract infection
- sending the patient a text with a link to upload a photograph
- ordering tests prior to clinical review
Top tip
Patients are often reluctant to describe their problem when in person in a busy reception area. Some practice receptions give patients access to the online consultation tool available in reception so they can provide this information in privacy.
It may be helpful to record phone messages that patients hear when they call your practice, before they are connected to a call handler, and to have call scripts for staff to follow when speaking to callers. You can use these example phone messages and call scripts to get you started in creating these.
Making a decision about allocation
Once you have the structured information from the patient, you will need to decide where to allocate the request and with what urgency. All patient requests need to be reviewed consistently using the same, single process.
You should record your allocation decision for safety, accuracy and training purposes, where possible SNOMED coded, and in your online consultation tool or clinical system.
The things for you to consider as a practice, in deciding allocation are the:
- information gathered from the patient
- urgency
- patient’s view of urgency
- need for continuity of care
- complexity of health needs
- appropriate type of healthcare professional
- mode of consultation
- patient’s individual needs and circumstances, for example their age, specific conditions, vulnerability, access to digital or a mobile phone
Using population health segmentation and risk stratification tools
Some practices are using population health segmentation and risk stratification tools to refine their care navigation approach. Segmentation divides the patient population into groups with similar complexity of healthcare needs. It can be done using clinical judgement alone or supported with population health segmentation and risk stratification digital tools. Some tools code the individual patient’s segment or risk level into their notes.
Table 1: Patient groups
| Patient need group (PNG) | Level of need |
|---|---|
| 1. Non-user | Low |
| 2. Low need child | Low |
| 3. Low need adult | Low |
| 4. Multi-morbidity, low complexity | Low |
| 5. Multi-morbidity, medium complexity | Moderate |
| 6. Pregnancy, low complexity | Moderate |
| 7. Pregnancy, high complexity | Moderate |
| 8. Dominant psychiatric or behavioural condition | Moderate |
| 9. Dominant major chronic condition | Moderate |
| 10. Multi-morbidity, high complexity | High |
| 11. Frailty | High |
Table 1 is an example of a tool that segments the population based on healthcare needs. All patients are allocated to one of the 11 patient need groups, or segments. Patients can move between segments if their healthcare needs change. The segments are grouped into low, moderate and high need. This is one example of a segmentation tool that some practices are using; there are several different tools available for practices to use.
Including the use of linked-data into the tools, which incorporates GP, hospital, community and other data, gives a more accurate picture of a patient’s need group. For example, allowing data relating to a hospital event to be included in the calculation. Using the Shared Care Record data to determine the patient need group is an example of using linked-data and is being used in a number of parts of the country.
The patient need group in the patient’s record is used as part of the decision making for allocation (right service or healthcare professional and particularly whether the patient needs continuity of care). This approach can support more effective decisions around care navigation, triage and capacity planning within your multi-professional team.
Segmentation and risk stratification tools must be used alongside clinical judgement to support frontline staff with decision making. If any team member is concerned or unsure about a patient in any need group, they must be able to access support from an experienced clinician in the team. Embedding the use of these tools should be included in your clinical safety risk assessment and comply with information governance standards. See the digital safety requirements in the Safety considerations section below.
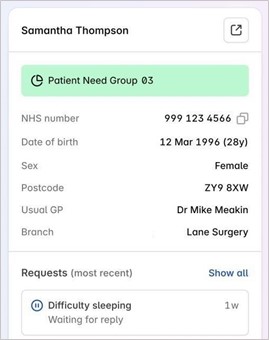
Figure 4: A screenshot of a test patient’s need group or segment within an online consultation tool inbox
Figure 4 shows how the patient need group of a patient can be displayed within an online consultation tool inbox, using fabricated names and information. It shows that the patient is in a green segment in this case the patient need group (PNG) 3, which identifies them as a low complexity need adult. It also shows who their usual GP is in case continuity of care is needed.
Figure 5: A screenshot of a patient’s need group within one of the GP IT clinical systems (EMIS)
Figure 5 shows how the patient need group (PNG) can be displayed within a clinical system. In this example, the patient is in PNG 4 so has multi-morbidity, low complexity need.
Further information is available from:
- the NHS Learning Hub modules on segmentation and stratification
- the Population Health Academy on Futures (login required) which has recorded talks from primary care networks and places that have used these tools for both reactive and proactive care
- your local integrated care board (ICB) analytical team if you require support in adopting a segmentation and risk stratification tool
Assessing urgency versus continuity of care
To provide a safe service, you need to decide what the level of urgency is for each request.
Some known red flag symptoms signal a serious condition. These include chest pain, weakness on one side of the face or body and severe shortness of breath. For compiling a list, NHS 111 red flag symptoms can be a helpful place to start.
Urgency may also relate to a patient’s need for an emergency supply of a medication for a life-threatening condition, such as insulin and anti-epileptics.
Next, you must agree with your clinicians how urgency should be assessed, especially if non-clinicians are doing the assessment. You will need clear rules and guidance to help decide if someone needs seeing today, this week or can wait beyond a week. Check the patient agrees with the suggested time frame. If there is any doubt or discrepancy between the practice’s and patient’s view of urgency, refer the case to a clinician.
Your chosen method to assess level of urgency must be as safe as possible and not overlook any worrying symptoms or signs.
Alongside the need to decide the level of urgency sits consideration of a patient’s need for continuity of care. Research shows that continuity of care can significantly reduce reattendance rates in general practice and improve outcomes for patients.
A balance needs to be struck between urgency and continuity of care, but it is possible to achieve both. While all patients arguably benefit from continuity of care, first consider which ones may benefit most. Then, consider if continuity of care must rest only with a GP. Could it be shared with an alternative practitioner or a small team? An alternative approach may help to achieve continuity, even in urgent situations.
The Safety considerations section below gives guidance on designing a safe process for assessing urgency and supporting continuity of care.
Complete a skills matrix
With the wider variety of roles now available in general practice, it is important to understand what skills your practice staff have. A skills matrix will identify what skills are common across each job role and those of a specific practitioner. This activity should also involve all your Additional Roles Reimbursement Scheme (ARRS) staff. A skills matrix template tool is available to download.
Compare the skills you currently have in your practice with those identified as needed in your avoidable appointment audit. Do they match or do you have gaps? Consider how to close those gaps. You could upskill existing staff or recruit new ones.
You can use the skills matrix to update your internal Directory of Services. It details who does what in the practice, giving staff up-to-date information about the practice staff who patients can be navigated to. Decide how you will make this directory accessible to all practice staff.
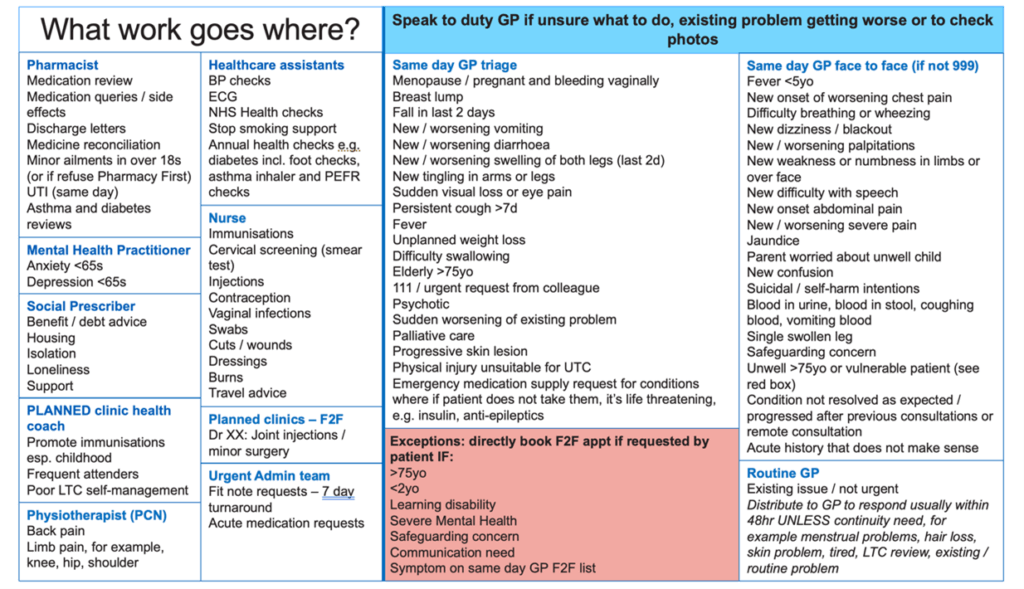
Figure 6: An example of a practice skills
Figure 6 shows a template that supports care navigation. It lists practice professionals who patients can access, the type of support they provide and their expertise. You can adapt this What work goes where? template for use in your practice.
Create a Directory of Services
External services can include:
- other primary care services, for example community pharmacy, dentistry, optometry
- secondary, tertiary and community health services, for example, minor injury units, urgent care centres, district nursing
- other statutory services, for example social care
- other commissioned services, for example drug and alcohol teams, public health services such as weight management, sexual health, Department for Work and Pensions, housing
- community and voluntary sector, for example food banks, Citizens Advice Bureau, HomeStart for parents, carers support services
- other local voluntary, community, faith and social enterprise organisations
The NHS Service Finder is a directory of NHS services and from it you can get accurate, real-time information to help signpost patients to available services. Your local ICB Directory of Services lead can add local NHS services to NHS Service Finder or update entries as required.
Where no information is given about a service in NHS Service finder – for example, it is a non-NHS services – we recommend collating this information into an external directory of services. To avoid duplication, check if such a directory has already been developed by your social prescriber, health and wellbeing teams or local council.
This directory should give staff access to up-to-date information on the services you can navigate patients to, and include:
- a brief description of the service
- its location, opening times, contact details
- how referrals should be made, for example self-referral, completion of a form/template by the practice, by phone
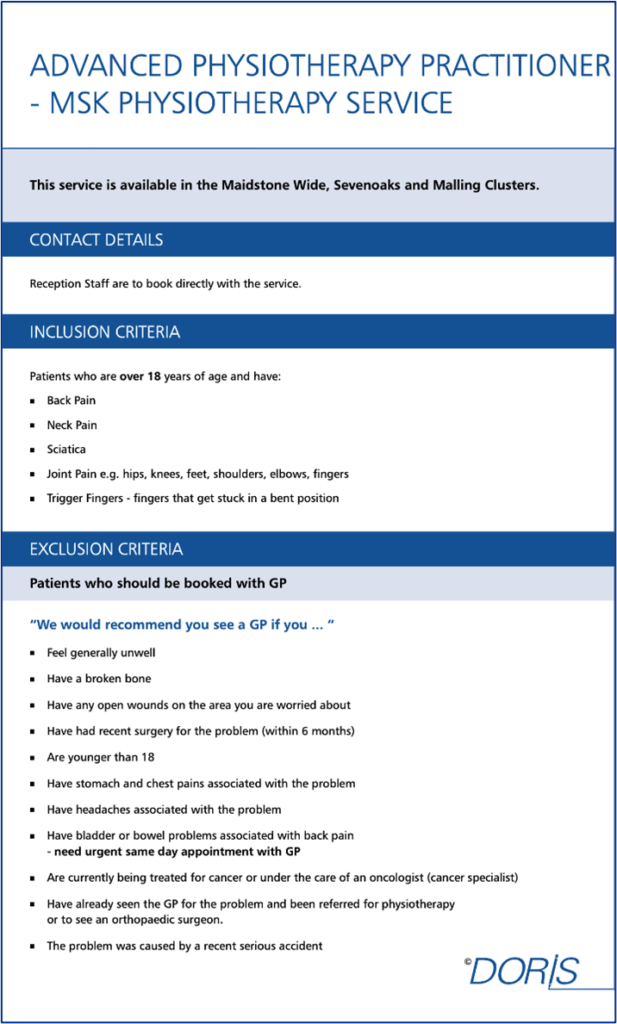
Figure 7: An example of a Directory of Service entry
The example entry shown in Figure 7 identifies which patients and conditions are suitable and not suitable for referral or signposting to an advanced physiotherapy practitioner.
Top tip
It is not practical for most practices to create and maintain this directory on their own. We recommend that this is done at a wider level, preferably integrated care system, place or neighbourhood level. If this is not possible, it should be done at primary care network (PCN) level as a minimum.
Safety considerations
We know all practices want to deliver a safe service. It is essential to give careful consideration to safety at this planning stage.
Digital safety requirements
Any organisation that instals and uses a digital system is responsible for its safe implementation. This includes:
- managing the clinical safety risks
- managing the system’s information governance
- completing the clinical safety risk assessment
- completing the data protection impact assessment
- ensuring the system meets the national Digital Technology Assessment Criteria (DTAC). This includes checking that the product has been correctly considered under the Medical Device Regulation
- ensuring the system meets the national specified capabilities to support digital pathways
- ensuring the system meets patient and general practice staff needs from online consultation systems (available on Futures which requires a login)
If you are using a digital system chosen by your ICB, it should support you with its safe implementation to fulfil these criteria. You will need to consider the mitigations for any risk and adapt these depending on how you work as a practice. This will ensure the procured digital systems meet user needs and are implemented safely. For more procurement advice see the NHS England National Commercial and Procurement Hub.
If you are using a digital system not chosen by your ICB, you are responsible for its assurance and safe implementation.
You can find a breakdown of responsibilities for your ICB and practice when procuring digital solutions on Futures (login required).
In either case, when implementing a digital tool to support care navigation, your practice must:
- update your data protection impact assessment and privacy policy
- work with your integrated care board (ICB) to mitigate clinical safety risks
- collaborate with your ICB clinical safety officer to complete and review a clinical safety risk assessment DCB0160 and update your clinical safety risk management activities as part of a dynamic approach to clinical safety
- ensure that patient access to digital services is integrated into your practice safeguarding plans, policies and procedures and your practice has a named information governance lead (or Caldicott Guardian)
- make sure patients know if decision making is being automated (where a person is not involved in the process) and agree to it. They must have the option to have a decision reviewed manually
- update your safeguarding and chaperone policies to include remote consultations
- use professional judgement to decide whether requesting a photograph is necessary for the provision of patient care. Should be stored in the patient’s clinical record or will a written description of the image suffice? Use guidance on how to manage intimate images for remote consultation
Further information can be found in:
Top tip
Templates of a hazard log to support you to complete the clinical safety risk assessment (DCB0160), as well as a digital triage clinical risk summary are available on Futures (login required).
Additional safety strategies
In addition to the digital safety requirements, consider:
- having measures in place to protect those who are vulnerable or susceptible to controlling or coercive behaviour
- ensuring all staff know how to identify and escalate incidents and concerns. Adapt existing processes for recognising, analysing and learning from incidents
- providing patients with the opportunity to share their information and communication needs and flagging these in their medical record. This includes those with a disability or sensory loss
- adding steps to your care navigation process to regularly check patients’ information and communication needs
Designing safe processes
When designing safe processes, follow a reliable design method.
The principles of reliable design are to:
- make it easier to do the right thing
- make it harder to do the wrong thing
- spot and stop errors
To make it easier to do the right thing in care navigation, you need a clear, standardised process. All staff and patients should be able to follow with minimal training. There should be little room for interpretation of what is required, for example, your practice skills matrix as described in Complete a skills matrix section above.
To make it harder to do the wrong thing in care navigation, find and fix potential error points. For example, most clinicians would agree that in the following situations a senior experienced clinician should review the patient face to face and prioritise continuity of care if:
- a patient has contacted the practice 3 times about the same problem
- a patient has accessed multiple services about the same problem in a short period of time, for example 111 or A&E
- there is escalating parental concern
- a condition has not resolved as expected or has progressed after a previous remote consultation(s)
- a patient has an acute history that does not make sense
- a patient has complex needs (including a complex family or carer situation), severe mental illness, palliative care, multi-morbidity, is frail or vulnerable
- a patient is high risk but does not engage with reviews or screening
- a patient has specific communication or information needs, for example sensory impairment, language challenges, a learning disability
This is not a comprehensive list. You should ask your senior GPs to review this list and add to it as necessary.
This approach should be applied even if the patient’s problem seems trivial. If a patient contacts the practice many times about the same problem and is signposted away each time, this could be an error point. A serious health issue may be missed. This error will be easier to spot if:
- this interaction is recorded in the clinical notes
- you ask patients if they’ve sought help for the problem before or seen anyone else about it
Make sure you include robust safety-netting when directing patients away from your practice. Ensure patients know what to do next, what to do if symptoms get worse or what to do if they don’t hear from anyone. Don’t assume that they will know.
Running a search for repeat contacts can help you establish whether this is a repeating pattern of behaviour that can be mitigated in future.
To spot and stop errors, including near misses and serious incidents, requires vigilance. This must be based on a shared purpose among all staff. It also relies on a strong learning culture with people feeling supported to openly raise concerns.
You can find out more about safe, reliable design by watching the Safe, reliable processes webinars available on Futures Primary Care Improvement Connect (requires login).
Setting up your success measures
All improvement work should be driven by data. Give some thought to how you will evaluate the success of your changes. Measure from when you start implementing your care navigation process so you can see early where it is working and where it may need improvement.
There are a range of measures you can use. Examples are:
- an audit of potentially avoidable appointments
- number of referrals to Pharmacy First
- number of recommended referrals to Pharmacy First declined by the patient
- number of referrals to a social prescribing link worker
- number of appointments signposted to the wider multi-professional team, not including GPs
- number of reattendances within 2 weeks for the same issue
- number of patient complaints about access
- specific measures from the staff survey
- percentage of patients who need continuity of care but do not receive this
Top tip
Ensure your online consultation system and telephony system provide you with the data you need to understand demand, demand patterns, need and navigation outcomes.
It is important to set a clear aim and outline the outcomes you expect from improving care navigation in your practice.
Some practices analyse outcomes by population demographics, deprivation, age, ethnicity, disability and inclusion health groups. This can help you to understand the impact of changes on health inequalities.
Outcomes you may look for through measurement are:
- reduction in avoidable appointments with the practice and with GPs
- improvement in provision of continuity of care
- reduction in complaints about access
- improvement in staff wellbeing – reduced sickness or burnout, greater joy at work
- reduction in call waits from reducing overall phone demand through increasing use of online channels, self-referral and self-service options
- increased use of Pharmacy First services
- improvement in local patient experience measures in the Friends and Family Test, patient experience survey or your own survey of patients
- improvement in experience of access across different patient groups
- all contact channels being open throughout contracted hours
- all requests, regardless of channel, are care navigated
- increase in urgent requests that receive same day access
Everything you do should seek to serve the outcomes you have set.
Top tip
When collecting data, involve staff early. Decide together what data to collect and how. This will ensure the data collection is possible, practical and consistent and you only need to collect the data once.
Top tip
At the start of implementation there may be an increase in call length, and therefore, call wait times. To make it easier to implement a new care navigation process, it may be best to tackle call wait times first. See the guides: How to align capacity with demand in general practice and How to improve telephone journeys in general practice.
3. Prepare
Benefits and key steps
You now need to put everything in place to help you deliver your plan and prepare for a stress free go live. This will be straightforward for some aspects but others will need to be tested to find any issues.
The benefits of preparation are:
- a practice team who can best meet the needs of your patients
- patients who are more prepared for the change
- external services that are supportive of the change
- a reduction in failure demand (avoiding duplication and decreasing avoidable work)
- creation of a more transparent process
- confidence that the changes you’re proposing will succeed
The key steps in the Prepare section are to:
- decide whether you are looking to take a small steps or big bang approach
- create and test a single process to manage all patient requests irrespective of their entry point. This includes testing your phone and messages, structured information capture, urgency and continuity assessment
- ensure you have the team you need. Review and refine your internal directory
- engage with the external services you have identified. Refine your external directory as a result of this engagement
- document your new process along with the rules governing it. This can be done in the form of a protocol or a standard operating procedure
- align your appointment book to reflect your new process
- train all staff in ‘how things will be done’
- guide your patient facing team in how to have effective communication
- inform patients of the proposed changes, what they can expect and how they can be involved
Small steps or big bang?
The answer will be down to your preference and what feels doable. Both approaches can work and the advice in this guide works for both.
You may prefer to start small by creating a process to manage the most common requests in your audit of avoidable appointments. You can develop your rules, processes and directories of service based on these alone. Then use learning from testing these to build your care navigator scripts.
Alternatively, you may prefer to build a comprehensive package and launch it in one go.
Testing the elements of your care navigation process
You have now created a new process to manage patient requests and care navigate your patients. You should now test each of its elements to see if they all work as intended (both as an individual element and as part of the whole process) before you go live.
Draw up a programme of testing for all the elements you have updated or devised. This may include phone and message testing, capturing the decisions about allocation testing, and urgency and continuity assessment testing.
This testing step should involve undertaking rapid, short cycle tests of change. They will help you to identify and fix major issues in a controlled way. Practices that make time for this step find go live is a much smoother process because they have resolved many issues in advance.
When testing each element you should:
- Identify the scale and nature of the test. Some tests can be ‘done in the background’, involving your staff and perhaps some digital test patients. Some will need to be carried out in a live setting with real patients. Which scenario would work best for this element? How many times do you need to run the test to generate meaningful results?
- Be clear what you want each test to tell you. What is your aim for this test? What do you think is going to happen?
- Carry out the test and document what happens. What measures do you need to record and how will you record them?
- Think about what the results are telling you. Do you get the results you expected? Were they good enough or could they have been better? Were there any mitigating circumstances that may have influenced the results you got?
- Decide on your next steps. If your results were good, what could you test next? If they were not good, why? How could you improve the element to get better outcomes?
Involve both staff and patients in this testing phase. Their feedback will help you decide how successful each test was.
Top tip
This guide to improving services using quality improvement provides background and tools to support this step.
Phone and message testing
You have planned how to communicate with your patients, for example your phone message, and what is written on your online consultation tool. Now you need to optimise them.
Develop a process for collecting and collating feedback from both patients and practice staff.
Ask your patient focus group to offer their perspective. They can give you feedback on different messages and language. Test different phone messages in different scenarios and decide which are most effective.
Top tip
Many of the new cloud-based telephony systems have auto voices, both male and female. Type in the message and the auto voice will read it out.
The NHS Content guide can help you ensure your messages to patients are clear.
Decision capture testing
Testing how you have planned to capture decisions will check that this captures all the elements required to make good decisions when allocating a patient to a particular solution for their need. You can run your test using digital test patients, but you will get more robust results if you test with real patients in real scenarios.
Figure 8: Example of a SystmOne template (currently being tested at a practice in Wiltshire) for recording the care navigation decision
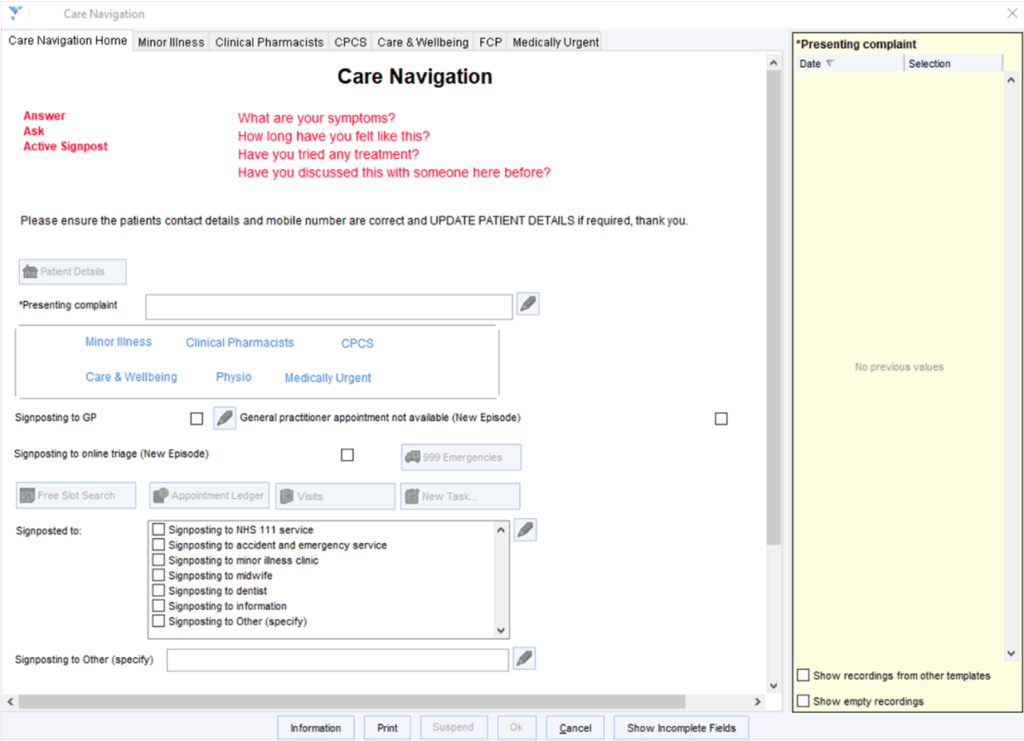
Figure 8 shows an example of a capture template built in SystmOne to record decisions made during the allocation activity. It includes tabs to make signposting simpler for care navigators. SNOMED codes are embedded to allow the information to be searchable for monitoring purposes.
When testing your decision capture method, consider how robust the codes you have embedded in your template are for:
- safety: for example, how many times has a patient been care navigated for the same problem?
- monitoring: for example, what percentage of the time is the decision capture method used?
- optimising your workforce: for example, how many patients are navigated to the mental health practitioner?
- workforce management: for example, how many patients are being navigated correctly?
Top tip
Creating templates in your clinical system is relatively straightforward. Have a go! Your clinical system provider can provide training and many ‘how to’ videos are available online. Someone in your practice, primary care network or locality may also be able to show you how. Look at other template providers for ideas. You can design and amend easily before publishing them for use.
Urgency and continuity assessment testing
You need to test that your planned approach to assessing the level of urgency for each patient request, and their need for continuity of care is fit for purpose.
You can do this with a small test group; for example, by checking the accuracy of outcomes over time for all requests received by 1 care navigator over 1 day or all care navigators over half a day. Run the assessment on each request received, then check the accuracy of the outcomes over time. This may be done by asking the clinicians to whom the patient was navigated. They should assess the urgency and need for continuity of care at the point of consultation. This should match the level of urgency assigned by the care navigator. You could also check for reattendance rates over the subsequent week or two.
You will need to repeat this test a few times, and with different staff to identify any differences between them. Be aware that y success rate may not be 100% but do not be disheartened by this. You are looking to achieve standardisation across staff and a safe level of accuracy.
If you are testing on real patients, you should provide clinical oversight for this activity.
Optimise your team
Once you have your new process, you should review what skills you need in your team. These may or may not be the same as the skills you already have (as identified in the ‘plan’ section). If they are not the same, the (ARRS) skills matrix tool might help you see what you need to close that gap.
Figure 9: Screenshot from the Additional Roles Reimbursement Scheme (ARRS) skills matrix (from Futures courtesy of NEY regional team)

Figure 9 is showing the skills a first contact physiotherapist brings. You can search the skills matrix by skills or by role.
You should also review your current appointment durations and consultation mode options. A move to GP appointments longer than the traditional 10 minutes may be appropriate if your GPs are seeing more complex patients, and use of group or remote consultations may be more efficient. Always remember safety considerations when making these decisions.
Take time to understand your capacity data and compare this with your avoidable appointment data to identify gaps in your workforce. You may have too many staff with certain skills and not enough of those with others. Consider how you can close any gaps by asking the following questions:
- Do you need to recruit different staff or can you upskill existing staff?
- Is there any capacity in your PCN for additional roles?
- How urgent is your staff requirement?
- Do you need to solve this before you change your care navigation process or can it be done over time?
Top tip
You may be concerned that extending the length of appointments will mean you have fewer appointments to offer. It is worth considering how many patients need to be seen multiple times due to a shorter appointment time not meeting their needs. You could test longer appointment times with one of your GPs, measuring your re-consultation rate before and after the change.
Engage external service providers
You will have identified the external services of greatest value to your patients during the planning stage. It can be helpful to get to know these service providers and build relationships with them. Understanding the scope and ethos of their service can boost your care navigation success. Informing them of your population needs and care navigation process will help build a strong foundation for integrated neighbourhood working.
Document ‘how things will be done’
Once you have tested your new process and its supporting resources, agree your final standardised process, including the rules governing it.
You will need to capture this process in a ‘how things will be done’ document (a protocol or standard operating procedure). This document should be developed in line with the Safety considerations section above and must be signed off by a senior clinician.
It should cover the structured information that needs to be gathered, how to manage all requests from all channels in a single process and how to escalate issues and get support. You will also need to capture how you will regularly monitor the processes for efficiency and safety.
All staff should easily be able to access this document.
Standard processes for clinical and admin requests
As a minimum this document should include:
- a list of common clinical and admin requests
- a standardised process for dealing with those requests
- a way of assessing the severity and urgency of the current patient’s need
- how to demonstrate and take into account the complexity of the patient’s broader needs
For clinical requests, the document should include:
- clear instructions to enable allocation of the patient based on the symptoms or conditions they describe
- recommended urgency of appointment, for example same day, this week, within 2 weeks
- most appropriate mode of appointment (face to face or remote)
- duration of appointment needed
- any specific requirements for appointments, for example before 2pm if phlebotomy; patient to bring inhalers with them if attending an asthma check; interpreter needed
- most appropriate professional by role (for example, GP, practice nurse, Health Care Assistant). It can be a named professional, depending on the skill mix within the practice or by particular patient request
- continuity of care needs and with whom, for example patient’s usual clinician or small team; the clinician consulted in the last 6 months; the clinician who ordered the test; the patient’s preferred clinician
It should also include information for navigating patients to:
- self-serve options where appropriate, for example online repeat prescription ordering
- services within general practice, for example additional roles in the practice or PCN
- services outside general practice, for example Pharmacy First, sexual health services
For navigation of administrative requests, the document should describe a clear distribution route in the practice and agreed turnaround times, for example 7 days for fit notes, 2 weeks for insurance reports.
Processes for supporting patients with specific needs
Instructions should be provided for supporting patients with specific needs, complexities or multi-morbidities, such as those patients who:
- are vulnerable
- have a disability, impairment or sensory loss
- are young children
- are frail and complex
- are pregnant
- have specific communication and information needs or contact preferences (including barriers such as language, literacy, digital access and understanding of the health system)
- have severe mental illness
- are receiving palliative or end of life care
- present frequently
- are care home residents
- are high risk but do not engage with reviews or screening
What to do when problems arise
The document should contain troubleshooting instructions:
- who to approach for support
- what to do if the patient declines the choice being offered
- what to do when the appointment book is full; this should not include turning off any patient contact channels during contracted hours
Top tip
If you are struggling to bring this document together, review your high-volume requests. Choose some requests that require allocation within the practice and some that don’t (for example, referring minor illness to Pharmacy First for patients who fit the referral criteria and have low complexity of need). Think about all the steps required to ensure these requests are managed in the right way and what resources you need to do this well. Ensure you think about ways in which this process could go wrong as well as how it could go right.
Align your appointment book
From your data on demand, capacity and avoidable appointments, you can estimate the number of appointments you need to meet demand.
Ensure your appointment book reflects your new process. When redesigning your appointment book you should consider the:
- total number of appointments needed on each day of the week. Remember to factor in known adjustments, such as increased demand before and after bank holidays
- spread of appointments across the day. For example, if you have a large working population you may need to offer more appointments early in the morning, over lunchtime or in the evening
- proportion of routine versus on-the-day appointments needed each day
- spread of clinical appointments by type of healthcare professionals across the week and the duration of appointments
Most patients do not need to be seen on the day they contact you.
The number contacting your practice probably peaks first thing in the morning, but this should ease as you improve online access and implement a responsive care navigation process.
A well structured appointment book should be flexible enough to meet the day’s demands and to offer contact types that suit each patient’s needs. Setting rigid times for each appointment type may waste capacity and add stress to clinicians.
For help redesigning your appointment book and rota to fit your care navigation model, see the guide How to align capacity with demand in general practice.
Top tip
Things that can help make your appointment book work for you:
- turn off automatic text messaging reminders to patients for triage slots
- align appointment book slots with associated GP Appointment Data (GPAD) categories
- align the permissions on your Additional Roles Reimbursement Scheme (ARRS) smartcards
- agree how you will view and manage your clinical workflow, for example viewing all clinical requests within your online consultation system or within your GP IT clinical system
Train your staff in ‘how things will be done’
All staff can undertake care navigation, irrespective of their role. They should all receive training in this to feel confident and capable in conducting the process safely and effectively and for the patient to have a consistent experience regardless of who it is handling their enquiry.
NHS England national care navigation e-learning training is available until September 2025. For more information, email napc@napc.co.uk.
ICBs may offer training locally and many practices provide their own training and support to first-line staff.
Your training should provide:
- a full understanding of each element of the new process for managing patient requests and care navigation and an opportunity to trial it. You can use ‘test patients’ and team simulations to build staff familiarity with the process, test the patient journey and check IT and logins work
- guidance on how the process should be delivered: the roles and responsibilities and its associated rules or protocols
- guidance on how to escalate an issue if there is a problem
- competence in using the digital systems involved and how to get support from the supplier. Digital suppliers can train staff to use their software, provide you with a point of contact and will explain how to report incidents or issues
- team and peer-led training (confident users support others) and person to go to for support and queries, including advice from a senior clinician
Top tip
To understand what to include in your training programme, ask your reception team what they worry about. Addressing these worries should give your team more confidence.
Effective patient communication
Your care navigation staff will also need training in and opportunity to practise customer service skills such as:
- careful listening
- demonstrating empathy and patience
- being adaptable, yet consistent
- providing the patient with information to support them to make an informed choice
- maintaining personal resilience
Reinforce the message of ‘our team’. It builds patient trust and reduces conflict.
Some practices have found the following approaches help engage patients.
At the start of a conversation you can:
- explore the patient’s query with them in a positive way. This will boost confidence, reduce frustration, and improve dialogue, enabling better care navigation
- say ‘If you can tell us more about your enquiry, we can direct you to the right person within the team. Would you mind sharing some information with us? This information is entirely confidential’
- use open questions to let patients share information in their own words, encourage conversation and boost engagement. For example, Why? How? What?
- use ‘we’ and ‘us’ to promote the consistency of your practice team message
- say ‘Our staff are using a process that the GPs have designed and agreed on.’
- say ‘Did you know you can now fill out an online form to ask for help to save you waiting on the phone? You can ask us for help in the same way as when you call us’
- say ‘you can now go straight to a physiotherapist for help with that problem’
- suggest a particular patient can be seen by a member of the wider team, if your practice protocol says this. This may widen patient choice of time and date and reduce their waiting time.
- say ‘I understand you may be uncomfortable telling me. I can reassure you our conversation is confidential. If you prefer, you can fill out the online form yourself. I can send you the link now if you like?’
- be clear about what happens with the information. For example, ‘the information will be passed directly to the doctor.’
- say ‘Dr [insert name of GP] has asked me to help you, to ensure you don’t have to wait long to see or speak with someone…’
- say ‘The reason we can’t do that is…’
- say ‘I’m sorry we didn’t do that…’
- say ‘Thank you for…’
- avoid phrases like ‘we are experiencing high demand’. They can frustrate patients and spark conflict
Towards the end of a conversation you can:
- say ‘Do you have any questions or concerns about the information and options we have spoken about?’
- use a reassurance message at the end of each conversation. For example, ‘Please come back to us if you have any questions or concerns’). This helps build the patient’s confidence. It shows them how care navigation can work for them
- make sure you communicate what the patient can expect to happen next, as well as how and when they will hear back
Top tip
You can use the phone messages and call script examples as a starting point.
Care navigation should guide a patient to the most suitable person or service to meet their needs but whether or not to follow this advice will be the patient’s choice. Patients need to have enough information to make the best choice for their needs. Careful communication can help ensure they do.
Inform patients of the changes
Your patients need to be kept informed of how things are changing and engaged in the new process. Consider the following in your engagement strategy.
- use your text messaging service to inform patients about the new way of working
- provide a message on your phone system about what patients should expect, for example to explain why they may be asked for a little more information than before
- use the written content templates to explain clearly on your website what patients should do in different situations and what to expect when they contact you online. These templates have been tested with patients for clarity and meet the NHS recommended reading age of 9 to 11 years
A consistent message across the different channels is key to success. You should use all relevant channels to promote the new process and do so using consistent messages. These channels include:
- verbal touchpoints – staff
- text messaging
- the practice website
- physical touchpoints – practice posters and screens, leaflets
- letters
Top tip
Your website should provide a clear and concise explanation of when to use the online consultation tool. GP website guidance has advice on making the online consultation tool link easy to find for patients.
When explaining any new process to patients, be sure to emphasise what they are gaining from the change.
4. Implement
Benefits and key steps
At some point you will need to press ‘go’ or nothing will change. Whether you are taking a small steps or big bang approach, this is the point at which it becomes real.
Last-minute checks, troubleshooting and support will keep things running smoothly. They will ensure you get all the benefits of an improved care navigation process, including:
- prioritising care based on need, providing safer and more equitable care
- ensuring patients can access care from the right healthcare professional, in the right way, first time
- increasing appointment availability throughout the day by reducing potentially avoidable appointments
- allocating appointments fairly across your staff
- empowering patients to use self-serve and self-referral services where appropriate and available
- improving patient and carer experience, enabling more personalised care
- improving staff experience and wellbeing
- improving efficiency and reducing failure demand
The key steps in the Implement section are:
- last minute checks before you start
- go live
- monitoring your progress and managing any issues
- staff support
- patient support
Last minute checks
You may find the following list of last minute checks helpful:
- Confirm the go live date and work towards it. This should ideally be not until you can expect to have a full team. Avoid launching a new system on a Monday or Friday.
- Clear the appointment book before moving to a new operating system. Some practices have provided extra clinical cover leading up to or for the first few weeks after ‘going live’ to work off any backlog.
- Ensure that protocols and processes work as intended. Staff should be clear about their roles and responsibilities. Use audit, feedback, reporting and incident monitoring.
- Ensure you have adequate support available for the first few weeks of running your new process. This support may be technical, for staff or for patients.
- Be clear how you will know that your go live is going well.
- Think about all the ways in which it could go wrong so you are fully prepared. Ask your staff and patient group what they are worried about and address their concerns.
- Also consider how you will:
- manage extra patients who need to be seen after you have run out of appointments
- deal with errors, for example a patient is navigated to an inappropriate service
- deal with complaints or unhappy patients
Go live
Implement your new process!
Senior staff should be available to observe, troubleshoot and support for at least the first few weeks and see this as their priority.
Any new process will not be perfect right away. Check in with your staff regularly throughout the first few weeks. Encourage them to provide honest feedback on how things are going.
Consider asking members of your focused patient group to support patients to navigate the new process. Regularly check in with them.
Have the phone numbers for phone and digital system support to hand when going live. If you are moving to a new phone or digital system as part of your care navigation process launch, it would be best to have on-site support for at least the first few days.
Monitoring progress and managing issues
Measure your progress using your agreed measures.
Collate and record issues as they arise. Some you may be able to solve straight away; others will be trickier. Do track them as this may help you avoid similar traps in your next improvement step.
Celebrate with your team when things go well. Change is difficult for people and positive reinforcement helps.
Be honest with staff and patients when things go wrong. If possible, involve them in finding better solutions.
Staff support
In any change process it is vital to support staff who are taking on new roles, particularly in the early stages of implementation. How you do so will depend on how quickly you are launching and individual factors in your practice.
Support may include:
- quick, daily team meetings
- regular clinical meetings
- having an experienced floor walker on ‘go live’ day
- having a named clinician for immediate support each day; all clinicians must be consistent in their approach, speed and effectiveness in offering support
- whiteboards to gather less urgent queries and dedicated time to review and respond
- structured approaches to reviewing episodes of care recorded for training and monitoring
- built-in safety checks; is the care navigation process doing what it’s supposed to?
- peer-to-peer support, for example through a team chat and/or care navigation champions
The care navigation process should ensure staff have immediate support when they need this, and provide ongoing learning and development opportunities.
Top tip
When starting to use your care navigation rules and process, consider having your most skilled and experienced care navigator ‘floating’ among the team to support them and answer queries. In some practices this may be a GP and in others the practice manager, a care co-ordinator or care navigation champion.
Patient support
Patients need support to understand and navigate their way through a new process. Keeping patients up to date and involved will lay a good foundation and, when you go live, be patient with your patients.
Encourage feedback from patients as a fundamental part of learning from users what works and what may need further review.
Top tip
Having your patient group in the waiting room can be very valuable during a big change. They can explain the benefits of the change to their fellow patients and support them with any practical elements if needed.
If your online consultation tool has a login, send your patients a text message before going live to encourage them to sign up for an account in advance.
5. Sustain
Benefits and key steps
General practice is ever changing, so improvement work within needs to be continuous. Responding quickly to any change in context can be less work than waiting and planning big improvement projects from scratch.
By sustaining progress you:
- preserve a clear understanding of where you are, from monitoring and evaluating
- maintain control, from deciding where you want to be using horizon scanning
- are always flexible, from keeping your staff and patients ready and engaged
The key steps in the Sustain section are to:
- continue ongoing checks to ensure you are maintaining your improvement in care navigation
- review your care navigation processes regularly to ensure they still work as intended and are safe
- develop your staff to keep them involved and engaged
- maintain patient engagement
- horizon scan to prepare for changes in general practice; consider how you may need to adapt
Ongoing evaluation
Continue to evaluate your process. Improvement work can succeed in the short term but dissipate over time as focus wanes and interest grows elsewhere. Staff may return to previous ways of working. Starting again to implement improvement is time and energy consuming.
However, once you feel your process is working, you can measure and evaluate less frequently; from measuring daily, to weekly for a few months, then monthly. For continued success we recommend you measure and evaluate quarterly as a minimum.
Regular process review
Continuing to record and troubleshoot problems as they arise is a useful activity. Develop a method for regular review of your process. This should include:
- clear responsibilities for undertaking any review activity. Who will do what?
- a timetable: when will review activity take place? Ideally, this should be weekly at first, then monthly as things settle and issues become less frequent
- a risk assessment to mitigate potential problems
- review of your phone and digital systems to ensure they continue to act as efficient enablers of the process
- updating your staff skills matrix as you upskill staff or to reflect turnover
- review of the external directory of services. Add any new services that become relevant to your patients. You may need to request service additions if your practice does not hold the directory
- review of contractual requirements that may impact on your process
Use this review to check that the rules and processes are still fit for purpose. Keep an eye on the outcomes you want to see. If the practice circumstances change, do these also need to change?
Staff development
You will need a plan for the ongoing training and mentoring of staff and allow time for this. This should cover all practice requirements – your rules, processes and technology – and reflect staff needs and feedback. Make sure this training is staff led.
Ongoing patient engagement
Early on some patients may be uneasy about your new process. Maintain regular, clear and honest communication with your patients and make it easy for them to give feedback. Be curious about their position and perspective. Never assume you know what’s best for them – always ask them. Remember, if patients do not use your systems as intended, this is a sign they need improving.
Horizon scanning
Once your care navigation process is working well, consider how you can maintain your progress and whether you can improve further – for example, by expanding the success across your PCN or locality. Sharing protocols and having a shared directory of services saves time for individual practices. A shared telephony and triage hub may be worth exploring.
How to improve care navigation in general practice: Bakhai M, Fox Z, Croney L, Drew J, Graham E, Hudson M, Joyce J, Koffman O, Mata Cervantes G, Vallely D.
With thanks to all the general practice staff who helped test and develop this guidance. We appreciate the time they spent sharing experiences, expertise and reflections. Their perspectives and feedback have been invaluable in shaping this guidance.
This guidance was prepared by NHS England’s Primary and Community Transformation and Improvement team as part of the national General Practice Improvement programme.
If you have any questions or feedback, please get in touch: england.pctgpip@nhs.net
Publication reference: PRN01858i