Chief Executive’s overview
The past year has marked a pivotal moment for our National Health Service. Following the Spending Review and with the publication of our 10 Year Plan, we have begun to lay the foundations for a fundamental transformation of healthcare in this country.
The NHS has secured significant investment – £29 billion additional annual funding by 2028/29, alongside record capital investment and £10 billion for digital transformation. Nevertheless, we recognise that investment alone cannot solve the challenges we face. The public’s satisfaction with the NHS is at a record low, and we must rebuild that essential bond of trust.
Our transformation is built on three fundamental shifts that will reshape healthcare delivery. We are moving from hospital to community by creating a new neighbourhood health service that brings care closer to people’s homes. We are transitioning from analogue to digital by modernising our systems to harness technology and improve patient experience, and, we are shifting focus from sickness to prevention, concentrating on keeping people well rather than simply treating illness.
To deliver these changes, we are resetting how we work together across the system. We’re moving away from over-prescription and centrally mandated processes, instead focusing on outcomes rather than inputs. We are creating conditions where local leaders have greater autonomy to meet the specific needs of their communities, while still delivering against clear national priorities.
We have already made important progress, with improvements demonstrated across virtually every performance measure over the last year, despite the challenges posed by industrial action. We have delivered 3.6 million more appointments than last year and diagnosed an additional 187,000 suspected cancer patients within 28 days. Our aim to meet the NHS standard of 92% of patients waiting no longer than 18 weeks for treatment is ambitious but achievable.
These are challenging times, but they also present an extraordinary opportunity to reimagine healthcare. By working together – trusting local leadership, releasing ambition, and embracing innovation – we can ensure the NHS not only survives but thrives for generations to come.
The NHS belongs to us all. It’s our collective responsibility to protect and transform it. I am confident that together we can build an NHS that delivers better care for patients and better value for taxpayers.
Finally, I want to acknowledge the talent and commitment of our NHS England staff across the Country. The coming months will be tough as we navigate organisational changes and heightened expectations. I have met many staff over these first few months in post and seen firsthand their resilience and dedication to making a difference for patients and the NHS. It’s this spirit that gives me absolute confidence that, together, we can rise to the challenges ahead and deliver the transformation our NHS needs.
Sir James Mackey
Chief Executive
Performance overview
Summary
The performance overview section provides a clear and accessible summary of performance during 2024/25. It sets the context for the detailed financial and governance disclosures that follow and helps users of the report understand:
- who we are and what we do, including our mission, values and role within the wider health and care system
- how we’ve performed, highlighting progress against strategic objectives and setting out major achievements and areas for improvement
- why it matters, reinforcing our commitment to transparency, accountability, and continuous improvement in delivering high-quality care for patients and communities.
More detailed performance information, along with additional context, is contained within the performance analysis (link to performance analysis below).
About NHS England
NHS England leads the National Health Service in England, sharing with the Secretary of State for Health and Social Care the legal duty to promote a comprehensive health service, in accordance with the National Health Service Act 2006 (as amended by the Health and Social Care Act 2012 and the Health and Care Act 2022).
Our vision is high quality healthcare for all, and our mission is to:
- drive the delivery of safe and high-quality care in the right place and at the right time for patients
- support NHS staff with the training, data and tools they need to provide the best possible care
- deliver value for money for taxpayers, supporting the health of the population and the wider economy.
Our structure
NHS England is governed by a unitary Board which is accountable to the Government, Parliament and the public. Our Chief Executive Officer, Sir James Mackey, is accountable to Parliament and the Secretary of State for Health and Social Care.
We operate through seven regional teams working directly with systems and NHS providers across the country. Most services are commissioned by Integrated Care Boards (ICBs), which lead 42 local Integrated Care Systems (ICSs) comprising NHS organisations, primary care professionals, local councils, social care providers and community partners.
Organisational changes
In March 2025, the Prime Minister announced significant structural changes affecting the DHSC and NHS England. The government confirmed that NHS England will be abolished with its functions being integrated into the Department. These changes are subject to primary legislation, which will be implemented subject to agreement by parliament.
As part of these changes, the combined headcount across both organisations is expected to reduce by approximately 50 per cent. The objectives for this integration include: reducing administrative processes; eliminating operational duplication; and reallocating resources to support increased frontline clinical staff, including nurses, doctors, and other healthcare professionals.
The changes represent a significant shift in the governance and operational structure of health services administration in England.
Our responsibilities
NHS England allocates £151 billion of funding to local NHS systems and sets the priorities to deliver high quality care and value for taxpayers. We:
- oversee the delivery of safe and effective services across nearly 7,000 NHS organisations
- drive best practice, improvement and innovation through initiatives such as NHS IMPACT (Improving Patient Care Together)
- plan, recruit, educate and train the NHS workforce, providing digital learning platforms used by 3.5 million staff
- use health data to transform services, supporting research and innovation
- negotiate deals for vital products and services, delivering significant efficiency savings
- deliver digital services at scale, including the NHS App (used by 36 million people) and NHS 111 online.
Our history
On 1 April 2023, NHS England incorporated Health Education England, completing the formation of the new NHS England which had previously merged with NHS Digital on 1 February 2023. This streamlining reduced our overall headcount by over 35% and provided nearly £500 million of savings to support frontline services.
Our work is also supported by third party organisations including NHS Business Services Authority, NHS Shared Business Services, NHS Property Services Limited and Primary Care Support England provided by Capita.
Our aims
The NHS England Operating Framework sets out six aims:
- longer healthy life expectancy
- excellent quality, safety and outcomes
- excellent access and experience
- equity of healthy life expectancy, quality, safety, outcomes, access and experience
- value for taxpayers’ money
- support to society, the economy and environment.
How we measure performance
The NHS Constitution sets out the rights of patients, the public and staff. We measure and monitor NHS provider and system/ ICB performance against a wide range of constitutional performance standards and publish statistics relating to these core constitutional standards on the NHS England website every month.
ICB performance
In line with its statutory obligations, NHS England assessed each ICB performance covering the 2024/25 financial year and will publish a summary of each assessment on our website later in 2025. In line with the NHS oversight framework, all ICBs were placed into one of four support segments. At the end of 2024/25 NHS England was providing intensive support via the Recovery Support Programme to four ICBs. During the reporting period, one ICB entered the programme and none left it.
NHS England can use statutory enforcement powers where an ICB is failing, or is at risk of failing, to discharge any of its functions. During 2024/25 no formal legal directions were issued, however NHS England accepted new enforcement undertakings from six ICBs. These were in addition to the existing undertakings in place with NHS Hampshire and Isle of Wight ICB, which were applied in 2023/24 and remain in place. Copies of these undertakings are publicly available on the NHS England website.
Trust performance
During 2024/25, five trusts entered the Recovery Support Programme, with three trusts exiting and one being dissolved as part of an organisational acquisition. There was a small increase in the number of trusts (two providers) in segment four at the end of the reporting period, compared with the same point in the previous year.
There were no instances of NHS England issuing new legal directions this year. Seven trusts agreed new undertakings and a further nine saw existing undertakings superseded by revised measures. Nine trusts had existing undertakings lifted, either due to compliance or discontinuation, leaving 43 trusts with undertakings at year-end (44 in 2023/24).
ICB and provider annual reports
2024/25 ICB annual reports and accounts were published on their individual websites, links to these can be found on our website.
All NHS trusts and NHS foundation trusts (‘providers’) in England publish an annual report and accounts on their individual websites. The results of all providers are published by NHS England in Consolidated Provider Accounts. These are presented separately from those of NHS England, as NHS England is not the parent body of providers.
Overview of 2024/25 operational performance
As detailed in the 2024/25 Operational Planning Guidance, our overall priorities remained:
- Quality and patient safety
- Recover our core services
- Transform the way we deliver care and create stronger foundations for the future.
Against the backdrop of rising costs, unprecedented industrial action, and longer-term underinvestment in capacity, NHS productivity continued to improve. During 2024/25 the acute sector improved its implied productivity by 2.7%, doubling the pre-pandemic rate. This is a measure of how efficiently the NHS uses its resources by comparing increases in activity (outputs) to increases in costs, adjusted for inflation and is calculated using a cost weighted activity method. However, progress against the core performance priorities we set out has been limited. Whilst more people are receiving treatment in A&E within four hours, a growing number have also been waiting longer. In elective care and in primary, community and mental health services, despite seeing record numbers of patients, continued high demand means patients continue to experience difficulty accessing services.
In Urgent and Emergency Care (UEC) our headline objectives were to improve ambulance response times and A&E waiting times. Despite record numbers of patients being seen, and improvements made compared to the previous year, ambitions to reduce average category 2 ambulance response times to 30 minutes and to ensure at least 78% of patients attending A&E were seen within four hours by March 2025 were not met (NHS England » Delivery plan for recovering urgent and emergency care services – January 2023). This is due to several factors, such attendances at Emergency Departments rising by 4.0% in 2024/25 compared to 2023/24 and ambulance incidents increasing by 4.6% in 2024/25. Although the percentage of conveyed patients only rose by 1.6%. The impact of flu pressures was different to 2023/24, and the number of beds occupied peaked higher than previously with almost 5,600 in early January 2025 (January 2024: 2,500). Moreover, difficulties in discharging medically fit patients, to reduce bed occupancy and acute length of stay, provided a challenging environment for UEC services in 2024/25) (National flu and COVID-19 surveillance reports: 2024 to 2025 season – GOV.UK).
For Primary Care and Community Services, operational performance has been challenged against a backdrop of increasing demand for primary care and community services and GP collective action. The NHS saw improvements in experience of access to general practice, including same day appointments, but there remains variation at local level. However, the NHS did not meet objectives on improving community service waiting times or increasing units of dental activity (UDA) to pre-pandemic levels.
In elective care, we are delivering more diagnostic tests and treating more patients. We have outperformed the system specific activity targets, consistent with the national value weighted activity target of 107% with February 2025 showing performance at 121.5%. The NHS made significant progress in reducing long waits for elective care during 2024/25, but it did not fully meet the national target of eliminating waits of over 65 weeks for consultant-led elective treatment by September 2024. In January we published our Elective Reform Plan which sets out how the NHS will reform elective care services and meet the 18-week referral to treatment standard by March 2029.
The NHS exceeded its cancer targets by the end of March 2025. The Faster Diagnosis Standard performance was 78.9% (target 77%), and the 62-day performance was 71.4% (target 70%).
Progress continued against aspects of our maternity delivery plan, with reductions in the rate of brain injury and rates of stillbirth, neonatal death and maternal mortality largely remaining stable. Inequalities in outcomes persist, with women and babies from Black and Asian and the most deprived backgrounds being more likely to experience adverse outcomes.
There were more midwives at the end of the reporting period, with 26,835 whole time equivalents (WTE) in post (1,700 WTE more than March 2024). This comes alongside a sustained decline in leaver and turnover rates.
Performance analysis
In this section, we provide detail on the work we have delivered during the year. These key areas of performance relate closely to the objectives set out in our annual business plan and reflect progress made against the aims set out in the Government’s mandate to the NHS.
For more detail on how we delivered against the mandate, see page 178.
Key performance indicators
| Programme work area | Ambition | Performance |
| Urgent and emergency care | ||
|
Improvement of A&E waiting times, compared to 2023/24, with a minimum of 78% of patients seen within 4 hours in March 2025 |
78% |
75.0% |
|
Improve Category 2 ambulance response times to an average of 30 minutes across 2024/25 |
30 minutes |
35 minutes 22 seconds (mean ambulance response time for 2024/25) |
| Cancer | ||
|
Improve performance against the headline 62-day standard by March 2025 |
70% |
71.4% |
|
Improve performance against the 28-day Faster Diagnosis Standard |
77% by |
78.9% |
|
Increase the percentage of cancers diagnosed at stages 1 and 2 |
75% by 2028 |
60% (March 2025) |
| Diagnostics | ||
|
Increase the percentage of patients that receive a diagnostic test within six weeks |
95% by |
81.6% |
| Elective Care | ||
|
Eliminate waits of over 65 weeks for elective care as soon as possible and by September 2024 at the latest |
Virtual elimination |
22,884 7,380 |
|
Deliver (or exceed) the system specific activity targets, consistent with the national value weighted activity target of 107% |
107% |
121.8% |
|
Increase the proportion of all outpatient attendances that are for first appointments or follow-up appointments attracting a procedure tariff to 46% across 2024/25 |
46% |
45.5% |
| Primary and Community Care | ||
|
Improve community services waiting times, with a focus on reducing long waits for children and young people |
N/A |
67,725 waits over 52 weeks |
|
Increase dental activity by implementing the plan to recover and reform NHS dentistry, improving UDA towards pre-pandemic levels |
N/A |
82% |
|
Continue to improve the experience of access to primary care, including by supporting general practice to ensure that everyone who needs an appointment with their GP practice gets one within 2 weeks and those who contact their practice urgently are accessed the same or next day according to clinical need |
2023/24 baseline |
82.1% |
| Mental Health | ||
|
Increase the number of people accessing transformed models of adult community mental health (to 400,000), perinatal mental health (to 66,000) and children and young people services (345,000 additional CYP aged 0–25 compared to 2019) |
400,000 |
597,374 |
|
660,000 |
63,784 | |
|
840,254 |
829,308 | |
|
Increase the number of adults and older adults completing a course of treatment for anxiety and depression via NHS Talking Therapies to 700,000, with at least 67% achieving reliable improvement and 48% reliable recovery |
700,000 |
667,143 |
|
Reduce inequalities by working towards 75% of people with severe mental illness (SMI) receiving a full annual physical health check, with at least 60% receiving one by March 2025 |
60% |
66.5% |
|
Improve quality of life, effectiveness of treatment, and care for people with dementia by increasing the dementia diagnosis rate to 66.7% by March 2025 |
66.7% |
65.6% |
| People with a learning disability and autistic people | ||
|
Ensure 75% of people aged 14 and over on GP learning disability registers receive an annual health check in the year to 31 March 2025 |
75% |
79.88% |
| Prevention and health inequalities | ||
|
Increase the % of patients with hypertension treated according to National Institute for Health and Care Excellence (NICE) guidance to 80% by March 2025 |
80% |
70.3% |
|
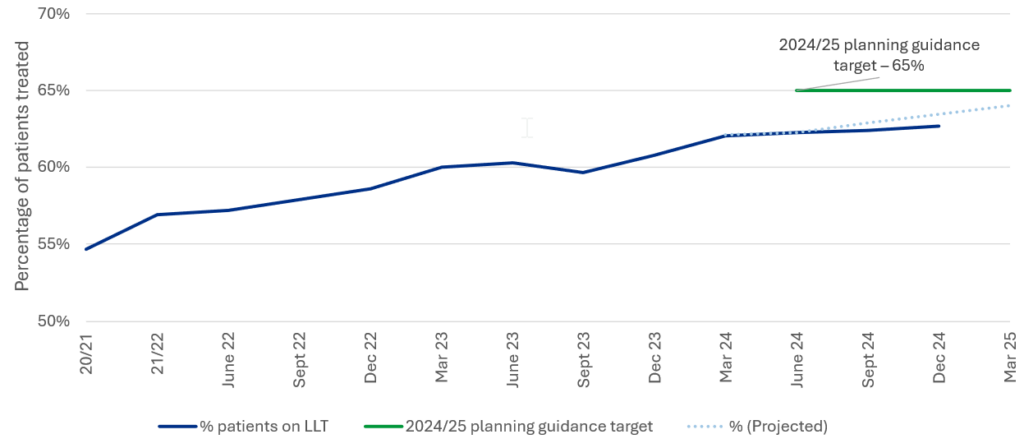
Increase the percentage of patients aged 25–84 years with a cardiovascular disease (CVD) risk score greater than 20% on lipid lowering therapies to 65% by March 2025 |
65% |
63.6% |
| Use of resources | ||
|
Reduce agency spending across the NHS, to a |
<3.2% |
2.3% |
Quality
All NHS organisations have responsibility for the quality of services, and both ICBs and NHS England have a statutory duty to act with a view to securing continuous improvement in quality.
Patient safety
The NHS Patient Safety Strategy is now in its sixth year and continues to deliver its aims, saving an extra 1,000 lives and £100 million in care costs per year from 2024 (NHS England » NHS patient safety strategy – progress update – April 2025).
An estimated 1,500 neonatal lives have been saved through safer care bundle interventions, and 1,900 deaths prevented through the medicine’s safety improvement programme, which has also avoided hundreds of millions in care costs.
In May 2024, NHS England announced the testing and implementation of Martha’s Rule in 143 pilot sites, empowering patients, families, carers and staff to ensure that their concerns are listened to and acted upon. Martha’s Rule is creating a structured way for patients to provide daily updates on their condition and access to an urgent review if their or their loved one’s condition deteriorates, and they are concerned this is not being responded to. In the first six months of implementation, 47% of the 2,389 calls related to acute deterioration; of these 1,298 calls resulted in potentially life-saving escalations of care, of which around a third led to a change in management or treatment.
In 2024/25, we completed the transition of all trusts to real time reporting via the Learn from Patient Safety Events service. This major upgrade made data (and analysis) relating to patient safety events available to all care settings. Around 3 million patient safety incidents were reported during the reporting period, allowing NHS England to identify risks that can be acted on, through National Patient Safety Alerts and collaborating with partners to address safety issues (NHS England » Our National Patient Safety Alerts). This work saves an estimated 160 lives per year and an estimated £13.5 million in additional treatment costs.
By September 2024, we completed the transition of all trusts to the Patient Safety Incident Response Framework, that required a complete overhaul of how NHS providers respond to patient safety incidents, emphasising the health system’s focus on learning for improvement.
The NHS Patient Safety Syllabus is building knowledge, capability and capacity in patient safety through the creation of the first system-wide standardised approach to patient safety training and education. Level 1 and level 2 training is available as e-learning to all NHS staff. Around 1.5 million staff completed level 1 training, including over 70,000 completions by Board members and senior leadership teams and over 850,000 completions for level 2 training by end of 2024/25. In addition to this around 500 staff completed level 3 and 4 training in 2024/25.
NHS IMPACT
NHS IMPACT was introduced to help systems and organisations align improvement approaches by focussing on the most common components of improvement methodologies. This allows systems and organisations to use a shared improvement approach and apply this to the biggest challenges and opportunities they are facing.
NHS leaders have worked with their boards to understand how deeply improvement is embedded in their organisation. This has enabled the formulation of an improvement development plan to demonstrate progress against the self-assessment which organisations have completed.
A suite of resources was shared on the NHS IMPACT website to support organisations to build capability and capacity, including across system partners. Additionally, a series of activities ran throughout 2024/25, to support NHS staff to learn and adopt improvement methods and tools.
NHS IMPACT have established several key improvement networks, to bring together peers from different parts of the NHS to work together on key challenges and issues. To strengthen learning in key priority areas, improvement guides were made available in outpatients, UEC, theatre utilisation and job planning, along with the establishment of learning and improvement networks.
As part of the Clinical and Operational Excellence Programme, learning and improvement networks brought peers together to focus on the development of data-enabled improvements.
Led by 14 acute provider chief executives, these networks collaborate to deliver improvement programmes to improve patient flow, safety and productivity.
Developments have been made to the Model Health System to include analysis related to outpatients, theatres, and UEC improvement.
Insightful Board
Effective NHS boards need to be curious and continually looking to improve how they use the information they receive across all aspects of their organisation’s operations. To support this and to help trust and ICB boards identify the information they need to manage their organisations effectively, in November 2024 NHS England published The Insightful Provider Board and The Insightful ICB Board. Built around six domains linked to capability and organisational priorities, these documents describe approaches to help boards ensure the right behaviours and culture are in place to use data effectively and drive improvement.
Recovering our core services
Urgent and emergency care
We set two national NHS objectives for UEC in 2024/25, focused on a national priority to improve A&E waiting times and ambulance response times. These priorities were two-year ambitions outlined in the Delivery plan for recovering urgent and emergency services, published in January 2023.
The first national objective was to improve A&E waiting times by March 2025. 75.0% (target: 78%) of patients were admitted, transferred or discharged within 4 hours (74.3% March 2024) (Statistics » A&E Attendances and Emergency Admissions). Though the 78% ambition has not been achieved, the NHS did see a record 27.4 million number of patients with 20.2 million seen within 4 hours, an 8.4% increase compared to 2023/24. Performance falls short of the constitutional standard of 95%.
The second national objective for UEC was to improve Category 2 ambulance response times. The mean ambulance response time for 2024/25 was 35 minutes 22 seconds (target,
30 minutes) (Statistics » Ambulance Quality Indicators). Despite this being an improvement on the previous year (2023/24: 36 minutes, 23 seconds), the 2024/25 ambition and the NHS constitutional standard of 18 minutes were not met.
Primary and community services
Primary care and community services had three national NHS objectives for 2024/25:
- Make it easier for people to access primary care and community health services, particularly general practice and dentistry
- Improve timely access to primary care, as outlined in the Delivery plan for recovering access to primary care (published in May 2023)
- Recover and reform NHS dentistry
Implementation of the second year of the Delivery Plan for Recovery of Primary Care has driven improvements to patient access to primary care. Pharmacy First was launched in January 2024 and during 2024/25 2.42 million clinical consultations were delivered by community pharmacy for common conditions. Additionally, there have been 407,329 oral contraception consultations and 3.1 million blood pressure checks conducted by community pharmacies, saving additional capacity in general practice.
By the end of the reporting period, 99.9% of practices had digital telephony in place and more than 700 practices were supported through the Practice Level Support programme, to better manage capacity and demand.
Since October 2024, over 1,000 additional GPs have been recruited by Primary Care Networks, through the Additional Roles Reimbursement Scheme. Supported by this work, 44.2% of general practice patients were seen on same day and 82.1% within two weeks in March 2025. The number of appointments offered in general practice, including COVID-19 vaccinations, increased by 3.69% with 383.4 million appointments offered by March 2025 (previous year: 369.8 million) (Appointments in General Practice, January 2025 – NHS England Digital).
The Health Insight Survey, launched in July 2024, showed how the improvements in access are benefiting patients and their experience of general practice. In March 2025, 72.9% of respondents reported that they found it easy to contact their general practice, (July 2024 when the survey was launched: 60.9%). The percentage of respondents who knew how their request would be managed on the same day as contacting their GP practice was 71.5% in March 2025 (July 2024: 70.3%).
Demand for community services has continued to grow in 2024/25, with an additional
1.75 million referrals to community services recorded during the reporting, compared to the previous year. To meet that demand, there were an additional five million consultations (Community Services Statistics – NHS England Digital). Despite the increase in capacity, the objective to improve community services waiting times – focusing on reducing long waits – has not been met and by March 2025, community service waits of over 52 weeks had increased to 77,712 (March 2024: 40,904). Adult waits of over 52 weeks saw a slight increase to 9,987 in March 2025 (March 2024: 9,208), however waits for children and young people rose markedly to 67,725 in March 2025 (March 2024: 31,696) (Statistics » Community health services waiting lists), an increase driven primarily by rising demand for neurodevelopmental assessments. The increase across all community waiting times was driven by workforce shortages, skill mix limitations, commissioning and contracting issues and inconsistencies in clinical pathways.
The ambition to increase units UDA towards pre-pandemic levels, in March 2025, 82% of contracted UDA had been delivered across 2024/25.
Elective care
We set four national NHS objectives for elective care in 2024/25; all focused on the national priority to improve patient outcomes and experiences by continuing to reduce long waits for elective care.
The 2024/25 priorities and operational planning guidance included an objective to eliminate waits longer than 65 weeks, from consultant-led referral through to elective care treatment, by September 2024 (except where patients choose to wait longer or in specific specialties).
Despite a steady decline in long waits throughout 2024/25 (Statistics » Consultant-led Referral to Treatment Waiting Times Data 2024-25), the NHS did not achieve this. However, by March 2025, the number of patients waiting over 65 weeks had fallen to 7,381, a reduction of 84.9% (March 2024: 48,967).
These long waits now account for less than 0.1% of the total national waiting list. Ongoing surveillance of long waits is continuing in 2025/26, with a national priority for reducing the proportion of people waiting over 52 weeks for treatment to less than 1% of the total waiting list by March 2026.
The second objective, relating to delivery of more routine elective treatment, on a value-weighted basis, was exceeded. By March 2025, year to date performance was at 121.8% against the 2024/25 annual target of 107%. A number of factors can influence the level of value-weighted activity including the types of activity delivered and the complexity of patients being treated. The NHS delivered more outpatient attendances and inpatient spells across 2024/25, with inpatient activity in particular driving value-weighted activity increases in part due to case mix complexity.
The third objective aimed to increase the proportion of all outpatient attendances for first or follow-up appointments that attract a procedure tariff (a set of prices for different healthcare activities) to 46% in 2024/25. Across 2024/25, cumulative performance was at 45.4% and 0.6ppt away from the ambition.
The fourth objective focused on enhancing patients’ experience of choice at the point of referral into an elective care treatment pathway. As of the end of March 2025, 24.7% of respondents to the Health Insight Survey reported being offered a choice of hospital when referred by their general practice within the previous 28 days. This figure shows no change from the baseline recorded when data collection began in July 2024.
The plan for elective care reform was published in January 2025 by the DHSC and NHS England. The plan set out how the NHS will reform elective care services and meet the 18-week referral to treatment standard by March 2029. Ambitions include making elective care increasingly personalised and digital, with a focus on improving experience and convenience, and empowering people with choice and control over when and where they will be treated. The plan includes a range of initiatives and milestone dates which have been included as a way of reaching the ambition by the deadline.
Alongside the publication of the Elective Reform Plan, the NHS and the Independent Healthcare Provider Network established a partnership agreement, the first of its kind for 25 years, outlining plans to work together to reduce the elective waiting list. The NHS and independent sector will work together to encourage long-term relationships and continue to drive patient choice of providers. The independent sector will also aid the elective workforce’s growth, provide training opportunities and offer greater support in the most challenged specialities such as ear, nose and throat, and gynaecology.
Cancer
The NHS delivered and exceeded its cancer targets by the end of March 2025, ensuring that:
- at least 77% of people receive a definitive diagnosis or ruling out of cancer within 28 days of an urgent referral (Faster Diagnosis Standard performance was at 78.9% in March 2025).
- at least 70% of people receive a first treatment within two months of referral or consultant upgrade (62-day performance was at 71.4% in March 2025).
NHS England provided targeted intervention and support to the most challenged providers.
For performance against the 62-day standard, in the most challenged providers there was a 6.8%-point improvement between quarter 4 2023/24 and quarter 4 2024/25, compared to just 2.3% points in providers who were not in receipt of intervention. This approach has reduced variation across the country, with a system-level performance interquartile range of 8.5% points by March 2025 (March 2024: 9.3% points).
28 Day Faster Diagnosis Standard performance 2023/24 to 2024/25
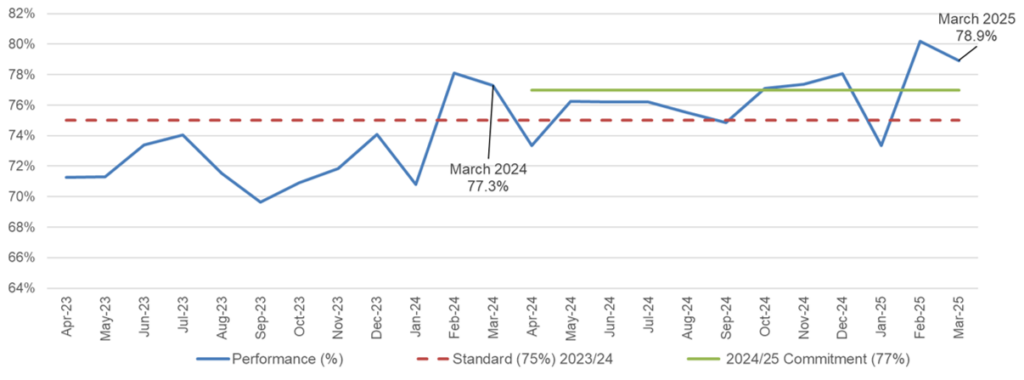
We have also seen benefits from the implementation of key pathway changes. In quarter 4 2024/25, 41% of skin cancer referrals used a tele-dermatology approach in which high quality images are reviewed remotely, and through which most patients can be reassured and discharged. The implementation of faecal immunochemical testing (FIT) into the bowel cancer pathway has reached the target of 80% of referrals being accompanied by a FIT result, supporting an improvement in the Faster Diagnosis Standard performance for bowel cancer from 51% to 64.4% between quarter 3 2022/23 and quarter 3 2024/25.
The NHS cancer early diagnosis strategy aims to give patients a better chance of survival (NHS England » Cancer programme update). The early diagnosis rate has increased by 3.0% points since 2019, including a 1.4% improvement in the 12 months to March 2025, translating to 8,500 more people diagnosed early compared to 2019 (Rapid Cancer Registration Data dashboards – NDRS).
Diagnostics
Timely access to diagnostics was described in the 2024/25 priorities and operational planning guidance as vital for supporting elective recovery and early cancer diagnosis. We therefore set an objective for diagnostics, to increase the percentage of patients that receive a diagnostic test within six weeks, in line with the March 2025 ambition of 95%.
In March 2025, 81.6% of patients received a diagnostics test within six weeks, which is 13.4% below the ambition. However, progress has been made during 2024/25, with an increase from 78% in March 2024, building on gains made after pandemic restrictions were lifted.
The median average waiting time for a diagnostic test dropped to 2.74 weeks in March 2025 (March 2024: 2.9 weeks). This is a significant improvement on pandemic wait times (May 2020: 8.6 weeks) and is almost back to the pre-pandemic average (2019/20: 2.2 weeks) and means that patients are being diagnosed faster, leading to quicker treatment and better outcomes.
The NHS has delivered record levels of diagnostic activity in 2024/25, with every month seeing a new NHS monthly record for diagnostic activity – i.e., diagnostic activity in May 2024 was higher than any previous May. In 2024/25 an average of 2.4 million tests were carried out each month, delivering an 8% increase against the previous year and a 25% increase on pre-pandemic levels (2019/20). In March 2025, almost 2.5 million tests were performed in the 15 key diagnostic modalities (Diagnostics Waiting Times and Activity (DM01) – NHS England Digital), an increase of 9% (March 2023: 2.3 million tests) (Statistics » Monthly Diagnostic Waiting Times and Activity).
Community Diagnostic Centres (CDCs) delivered 6.8 million additional tests in 2024/25, including CT scans, ultrasound investigations, plain film x-rays and pathology tests.
Other investments in endoscopy and imaging capacity resulted in 450,000 other forms of medical imaging and 275,000 additional endoscopies.
The digitisation of diagnostic pathways has resulted in more rapid test acquisition, processing and reporting, which in turn has returned the following benefits:
- Improvement in productivity and improved staff satisfaction.
- Where consultant radiologists and reporting radiographers are using home reporting digital infrastructure for imaging reporting, the clinicians have reported a 9% increase in imaging reporting, working remotely.
- Where trusts have installed MRI acceleration software on MRI scanners, the associated scanners are seeing an average 14% increase in scanning throughput.
- Where trusts have deployed the iRefer clinical decision support tool at referring sites such as general practices and hospital departments, unwarranted test requests for CT, MRI and x-ray were reduced and 5% of imaging test requests were withdrawn by referring clinicians.
- The use of image sharing solutions within imaging networks is expected to reduce unwarranted repeat tests by up to 9%, based on the analysis of test requests for one imaging network.
To mitigate the risk of performance targets not being met, NHS England supports systems to maximise the impact of capital investment and a range of performance improvement initiatives including:
- Capital funding to grow diagnostic capacity, via the Constitutional Standards capital allocation process, including through the roll out of 170 CDCs and additional acute trust equipment (as of July 2025).
- Establishment of digitally enabled diagnostic networks to drive diagnostic service productivity growth and speed up test results.
- Clinically led improvement support for systems to adopt a series of best practice approaches on utilisation, demand optimisation and productivity.
- Support to adopt highly productive straight to test pathways which are speeding up diagnosis and enabling patients to receive all their tests in one CDC visit.
Maternity, neonatal and women’s health
Progress has been made across the four themes of the three-year delivery plan for maternity and neonatal services. These are: listening to women; workforce; culture and standards; and structures. As we enter the final year of the plan, we continue to work towards the following objectives, with a specific focus on narrowing the inequalities in outcome and experience:
- Continue to make progress towards the national safety ambitions (to reduce stillbirth, neonatal death, brain injury, preterm birth and maternal mortality) and increasing fill rates against funded establishment.
- Establish and develop at least one Women’s Health Hub in every ICB by December 2024, working in partnership with local authorities.
With regards to our national safety ambitions, the data shows that stillbirth (State of the nation report | MBRRACE-UK), neonatal death and maternal mortality (Saving Lives, Improving Mothers’ Care 2024) rates have remained largely stagnant, whilst the rate of brain injury (Brain Injury Surveillance Reports | Faculty of Medicine | Imperial College London) has fallen, and preterm birth (Births in England and Wales: linked births – Office for National Statistics) rates have increased. Inequalities persist, with women and babies from Black and Asian and the most deprived backgrounds being more likely to experience adverse outcomes.
During 2024/25, maternal mental health services were established in 41 ICBs, with the remaining ICB becoming operational in June 2025 and 63,748 service users were provided support through specialist Perinatal Mental Health Services.
Version three of the Saving Babies’ Lives Care Bundle brings together evidence based best practice to reduce perinatal mortality across six elements, including smoking in pregnancy.
We have seen a significant and sustained reduction in the smoking-at-delivery rate, with data indicating that, in quarter 4 2024/25, fewer than 6% of women were smoking at delivery. This is the lowest ever recorded rate (Statistics on Women’s Smoking Status at Time of Delivery: England, Quarter 3, 2024/25 – NHS England Digital).
There are now more midwives than ever before, with 26,835 WTE employed as of March 2025, marking an increase of 1,700 (6.7%) over the past 12 months. We have seen a sustained decline in leaver and turnover rates. Leaver rates remain at below 5% levels compared to a peak of over 7% following the COVID-19 pandemic. Based on the March 2025 leaver rate of 4.3%, we are retaining approximately 750 WTE more midwives (over 12 months), compared to when leaver rates were at their peak of 7.3% in 2022.
The obstetric workforce is also growing, and we have established a sustainable training route for obstetric physicians to develop specialist skills to work with women with pre-existing medical conditions, during and after pregnancy.
All 150 maternity and neonatal leadership teams have now taken part in the national culture and leadership programme. Each team is implementing culture improvement plans based on feedback from their staff and we are developing the next phase of this programme, which will specifically address racism and discrimination.
Women’s Health Hub provision was established or expanded in 42 ICBs during 2024/25.
We are planning the publication of a good practice guide to support neighbourhood-level delivery of women’s health services to improve access, experience and outcomes for women and girls, for publication in 2025/26.
Mental health
There were seven national NHS objectives for mental health in 2024/25. These objectives primarily focussed on: access to mental health services for adults; children and young people; access to perinatal services; reducing health inequalities; and reducing the number of people inappropriately placed in mental health hospital out of area placements (OAPs).
Improve access to transformed models of mental health care for adults, perinatal, and children and young people
In 2024/25, NHS England began work to develop and provide a nationally led improvement support offer to help local systems improve access to community mental health services for children and young people. This provided clinical and operational leadership support and helped to drive improvements in the quality and effectiveness of services’ use of data.
Access to adult community mental health services for transformed models of care increased in quarter 4 2024/25 to 597,374 (target: 400,000).
63,784 women accessed specialist community perinatal mental health services and MMHS in the 12 months to the end of March 2025 (target: 66,000).
Performance against this commitment continues to improve through continued support of regions and clinical networks, and through sharing best practice.
In the 12 months to March 2025 an additional 41,000 children and young people aged between 0-17 accessed mental health services against a target of 840,254 (2024/25: 829,308 compared to 2023/24: 788,108).
The number of children and young people with at least one contact from funded mental health service

By March 2025, 73.9% of ‘routine’ children and young people eating disorder referrals were seen within 4 weeks, with 73.1% of urgent referrals seen within one week. Whilst this remains below the standard of 95%, children and young people’s community eating disorder services are now treating almost 40% more children and young people compared to pandemic-era
levels (2019/20: 8,034, 2023/24: 11,174).
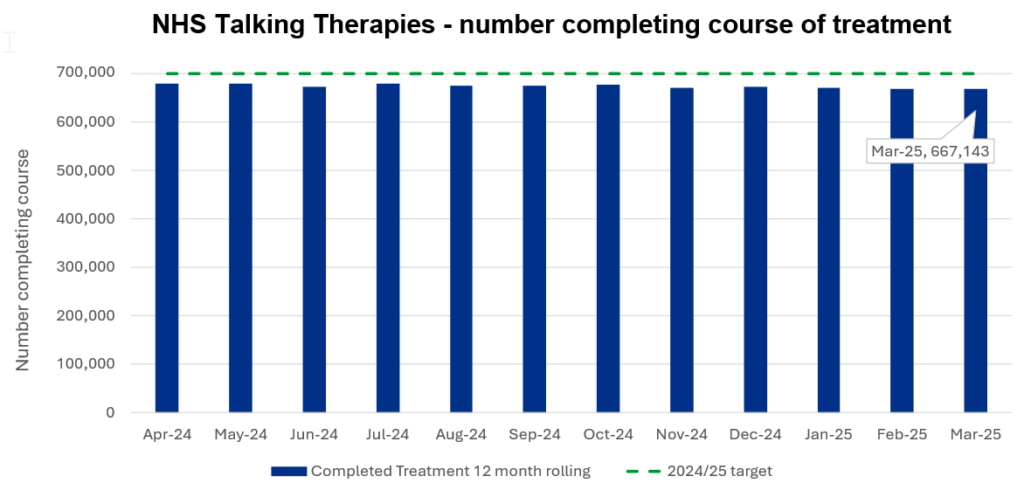
Increase the number of adults and older adults completing a course of treatment for anxiety and depression via NHS Talking Therapies.
NHS England has worked throughout 2024/25 to support the delivery of NHS Talking Therapies, focused on securing workforce training (to enable workforce expansion) and to support providers to increase service capacity. We have supported systems to improve the productivity of Talking Therapies by expanding the use of digital technologies, increasing patient-facing time and freeing up clinical time.
In 2024/25, 667,143 adults completed a course of treatment through NHS Talking Therapies. This is below anticipated trajectories and less than 2023/24 levels due to increased session numbers and workforce growth occurring later in the year than planned, as shown below.
NHS Talking Therapies – number completing course of treatment
Continue to reduce inequalities by working towards 75% of people with a SMI receiving a full annual physical health check.
People with SMI are at higher risk of poor physical health and at significantly higher risk of obesity, asthma, diabetes, chronic obstructive pulmonary disease and CVD – and are significantly more likely to die prematurely compared to the rest of the population. Physical health checks for people with SMI is a key focus area to help address health inequalities and premature mortality.
Physical health check data for quarter 4 2024/25 March 2025, shows 66.5% of registered patients on a GP register with SMI received a full health check, exceeding the minimum standard of 60%.
Improving quality of life, effectiveness of treatment and care, for people with dementia.
The dementia diagnosis rate for March 2025 is 65.6% (national ambition: 66.7%) and, although marginally short of the 2024/25 target, this is an improvement on previous years (March 2024: 64.8%; March 2023: 63%), demonstrating a consistent year-on-year increase in recovery of the dementia diagnosis rate.
We continued to share best practice across NHS regions and promoted resources aimed at increasing dementia diagnosis, particularly in care home settings. We have encouraged the adoption of the RightCare Dementia Scenario to guide best practice for diagnosing dementia and we have supported ICBs by developing resources, including a self-assessment framework, to help designing integrated dementia pathways.
Improving patient flow and eliminating inappropriate Out of Area Placements
The number of people in inappropriate OAPs in adult acute beds actively increased from 396 in December 2024 to 401 by the end of the reporting period (March 2025 target: 181 or less), as shown in the following chart.
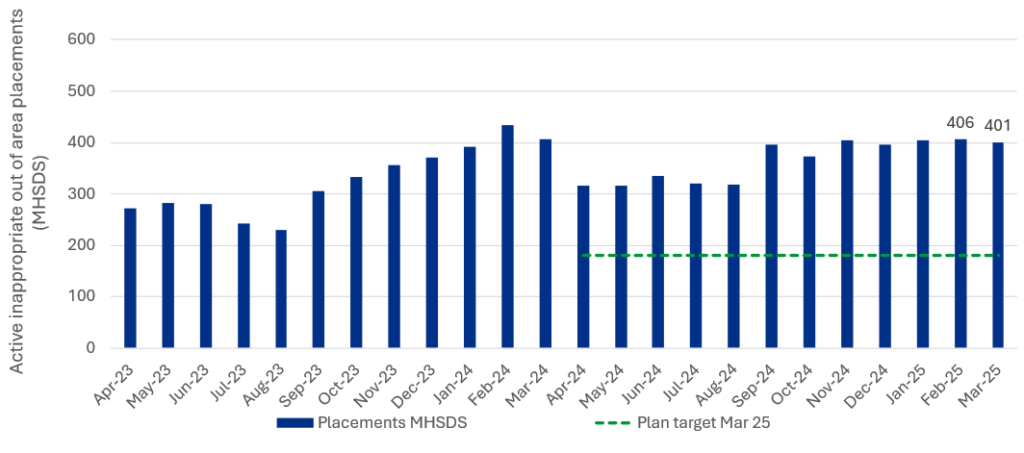
Key challenges driving OAPs include increased demand for mental health services, workforce shortages impacting service capacity, limited local bed availability and quality concerns across mental health services. Additionally, data quality issues persist in both the Mental Health Services Data Set and local data, and further work is underway to investigate and address these data issues.
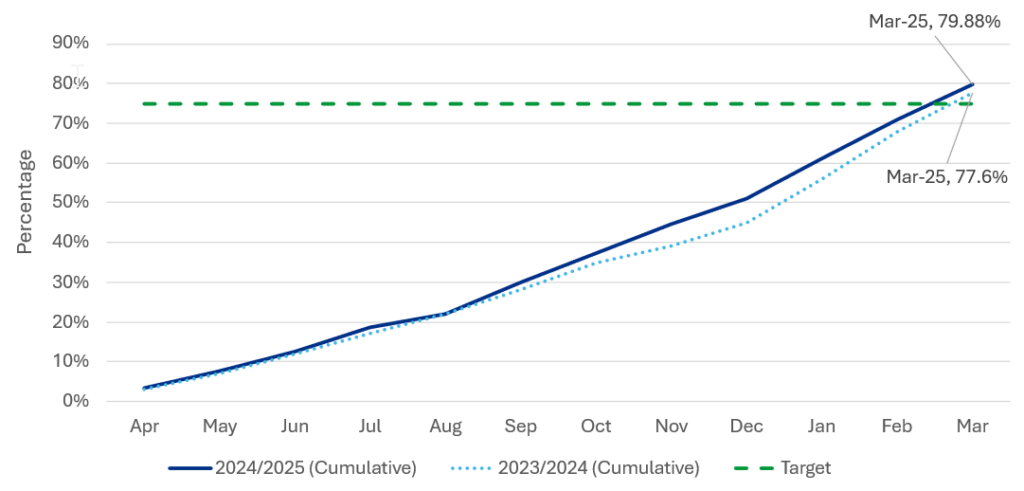
People with a learning disability and autistic people
The NHS made substantial progress with delivering learning disability annual health checks and accompanying health action plans, both of which are key components for managing health inequalities experienced by people with a learning disability. By March 2025, 79.88% of people aged 14 or over, who were on GP learning disability registers, received an annual health check. This exceeds the national ambition of 75% and previous year’s performance (2023/24: 77.55%).
Learning disability annual health checks
Reducing reliance on mental health inpatient care
At the end of March 2025, there were 2,025 people with a learning disability and autistic people in a mental health inpatient setting (baseline at March 2015: 2,910). This represents a decrease of 30% against our NHS Long Term Plan ambition to reduce inpatient numbers by 50% by March 2024. The number of people with a learning disability residing in a mental health inpatient setting decreased by more than 50%, exceeding the national target. However, we have seen the number of autistic people in a mental health inpatient setting increase by more than 130%, including people who were diagnosed as autistic while in hospital.
As of March 2025, there were 223 children and young people (aged under 18) with a learning disability and/or are autistic in a mental health inpatient setting. Keyworker services are in all ICB areas for children and young people with a learning disability and those who are autistic.
In 2024, keyworker services reported that they helped avoid a mental health inpatient admission for over 2,000 children and young people.
There were 1,805 adult inpatients as of March 2025, 340 higher than the quarter 4 system planning target of 1,465.
In 2024/25 we made £124 million available in system baselines to enable the development of community intensive support teams, community forensic teams and 24/7 crisis response for people with a learning disability and autistic people. We made £13 million of housing capital available to support people to leave hospital and we have continued to ensure that national guidance and resources for people experiencing mental illness are reflective of the needs of autistic people and those with a learning disability.
Prevention and long-term conditions
By March 2025, 70.3% of hypertension patients (aged 18 and over) were treated in line with NICE guidance. While no systems met the 2024/25 target of 80% (increase percentage of patients with hypertension treated to NICE guidance to 80% by March 2025), between March 2024 and March 2025 922,436 people were diagnosed with hypertension, and 598,403 people had their hypertension managed to target. As of March 2025 CVD Prevent data shows 494 practices have achieved the target of 80% or more.
Hypertension performance has been adjusted to incorporate home and ambulatory Blood Pressure readings from the June 2024 data period and all future reporting periods. A GP system fix also led to a drop in performance as, prior to this fix, any patients whose diagnosis was recorded at a previous practice were not included in the data. This increase in surfaced diagnoses led to a reduction in achievement against the 80% treatment target, from June 2024 onwards.
The following initiatives have been the driving force behind improving detection and management of hypertension:
- The CVDPREVENT audit, is an extract of routinely held GP data. CVDPREVENT benchmarks performance at general practice, PCN, system and regional level, whilst also highlighting unwarranted variation and health inequalities. These data sets are used both locally and nationally to inform decision making.
- The NHS Quality Outcomes Framework provides the only financial incentive for primary care to drive up performance.
- NHS England provides funding for CVD leadership in every ICB and provides systems with the freedom they need to identify and address local barriers to improvement.
- Dental and optometry sites have been selected to take part in pilots to test the effectiveness of blood pressure checks in wider primary care settings, and funding has been transferred to systems to enable. All sites are now live. A community of practice group has been set up to support sites to share good practice. The pilots will run until summer 2025 and the evaluation partner (South West Health Innovation Network) will report on their findings by Autumn 2025.
In 2024/25, nationally, 63.6% of patients (aged 18 and over and with a CVD risk score of over 20%), were treated with lipid lowering therapies, with seven of 42 ICBs having achieved the 2024/25 target of 65%. By the end of the reporting period, 265,000 (total circa 3,081,000) additional people were identified as being at high risk of CVD and 183,000 (total circa 1,933,000) more people at high risk of CVD were treated with lipid lowering therapy.
Between March 2024 and March 2025 289,383 additional people were identified as being at high risk of CVD and 242,000 more people at high risk of CVD were treated with lipid lowering therapy.
Lipid lowering therapy testing rate
Transform the way we deliver care and create stronger foundations for the future
Embedding measures to improve health and reduce inequalities
Vaccination and immunisation
Preventing between 3.5 million and 5 million deaths worldwide every year, vaccinations help people stay well and avoid hospital stays. Since introducing many of our vaccination programmes, we have seen reduced annual deaths through the targeting of diseases such as polio, where deaths have been virtually eradicated.
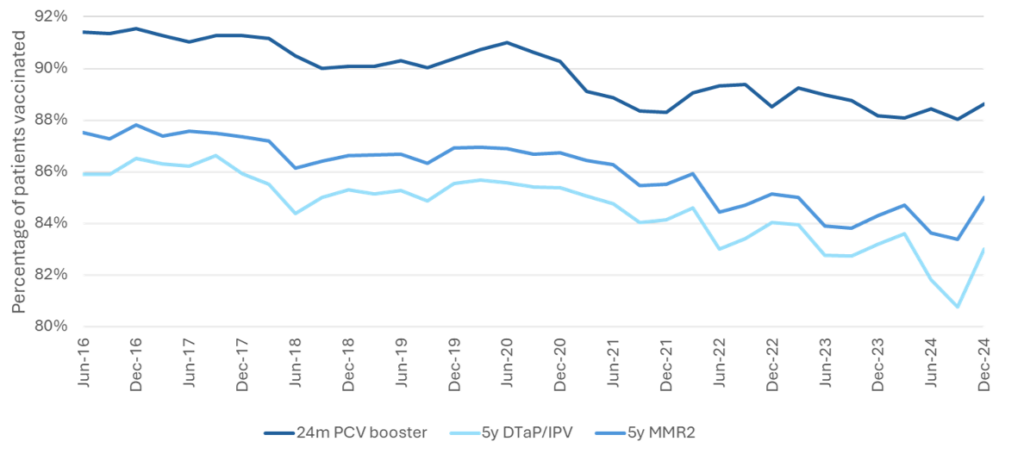
In line with worldwide trends the uptake of vaccines in England has declined over recent years, including for the three key children and young people vaccines (MMR, DTAPIPV and PCV).
The need to reverse these downward trends, and to address vaccine confidence and accessibility, remains the focus. All three vaccine types have minimum 90% and optimal 95% immunisation targets in place.
As of December 2024/25, uptake levels fall short of the minimum target and are down against March 2023/24 levels.
- 5-year MMR2 Booster – 85% December 2024 (March 2024: 84.7%)
- 5-year DTaPIPV Booster – 83% December 2024 (March 2024: 83.6%)
- 24-month PCV Booster – 88.6% December 2024 (March 2024: 88.1%)
Nationally, the largest increase for MMR1 was observed in children aged 15 months to 5 years of age (1.8 percentage point increase) and for MMR2, the largest increase was observed in children aged 3 years and 7 months to 5 years of age (3.6 percentage point increase).
Over 13% of previously unvaccinated children under the age of 5 years were vaccinated with MMR1 during the NHS Catch Up Campaign for missed MMR Vaccines compared to baseline and, for all cohorts, the greatest improvement in uptake was in the most deprived deciles.
The chart below shows the trends of uptake from quarter June 2016 to December 2024.
The RSV vaccination programme was launched in September 2024 with more than 1.8 million eligible people, including older adults and women of child-bearing age (to protect their newborn babies) receiving the vaccination by the end of the reporting period. Early analysis showed a 30% reduction in hospital admission for people aged 75-79 after just three months.
Screening
Screening services seek to detect potential health risks early, enabling timely intervention and improved wellbeing. NHS England commissions 12 screening programmes, from newborn screening to abdominal aortic aneurysm screening for older people. With over 19 million screening tests carried out each year, screening saves thousands of lives and identifies problems early, covering a range of conditions.
Bowel Cancer Screening
The plan to have 64 sites live for bowel screening services for the 50 and 52-year-olds demographic has largely been met. Currently, 47 sites (73%) are live for the 52-year-old cohort, and 38 sites (59%) are live for the 50-year-old cohort. Only two sites remain to go live, and they are scheduled to do so later in the financial year.
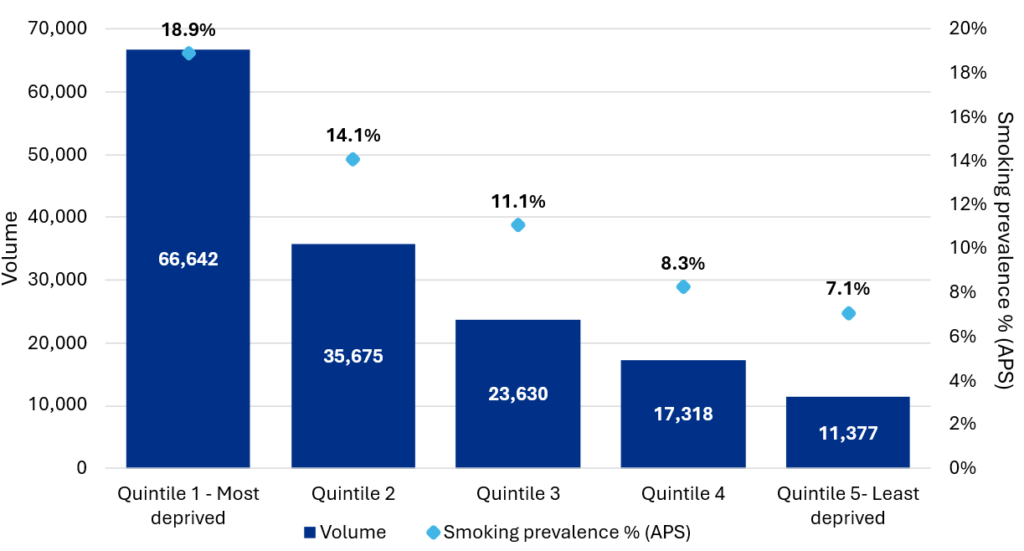
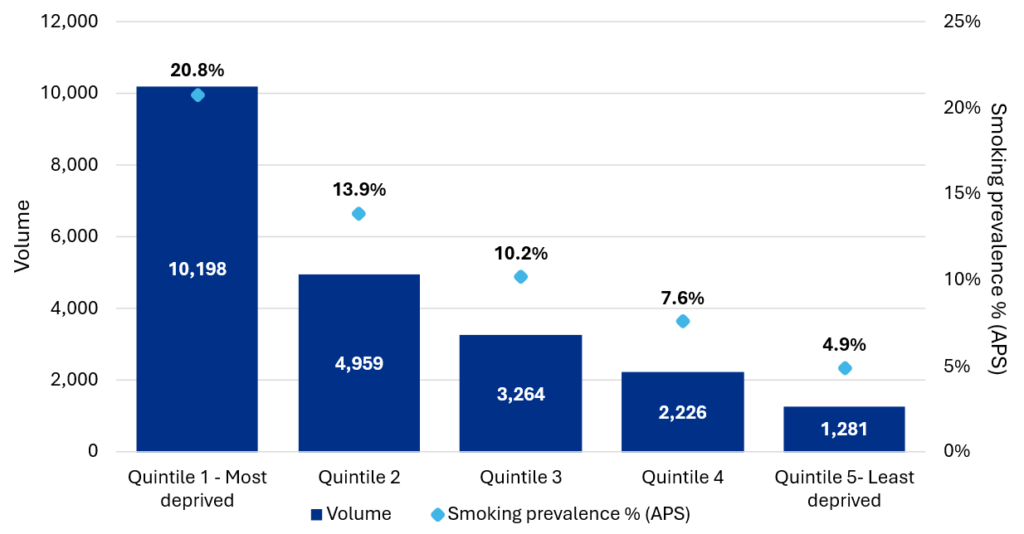
Tobacco dependance
NHS-funded tobacco dependence treatment service have progressed towards universal rollout with 93% of inpatient and 97% of maternity services delivering care to patients at the end of 2024/25. This means that the NHS has supported 121,000 people admitted overnight to hospital and 21,000 pregnant women to make an informed choice about quitting smoking over the 12-month period. This care has focused on those with greatest need with more people identified, seen and engaged in quit attempts from the CORE20 population.
All inpatients seen by tobacco dependence treatment services
Pregnant women seen by tobacco dependence treatment services
Targeted lung health checks
Lung Cancer Screening services expanded in 2024/25, with almost a million people invited to be assessed. 2.6 million people have been invited since 2019, or 37% of the total eligible population. There have been over 7,000 lung cancers diagnosed through the life of the programme, 3,000 in 2024/25 alone. Of this, over 75% were diagnosed at an early stage, increasing the lung cancer early diagnosis rate by 10.2% compared to 2019, and an improvement of 4.4% just in the last year. The lung cancer screening programme has also greatly benefitted those with the greatest need, with the most deprived quintile, who, because of the programme, are now amongst the most likely to receive an early diagnosis
Overall early diagnosis has improved across all deprivation quintiles, a narrowing in the difference between the most and least deprived from 8.5ppt pre pandemic to 6.5ppt (for the 12 months to March 2025).
Digital Transformation Screening – Cervical, Breast and Diabetic Eye
The implementation of the new NHS Cervical Screening Management System, implemented in June 2024, supports automation of breast screening for the National Disease Registration Service.
Work continues to ensure sufficient MRI capacity is in place to enable timely management of very high-risk screening in accordance with national standards, supported by continuous review and strategic planning around MRI diagnostic capacity and demand, including the introduction of new genetic tests for defined populations.
NHS England is introducing state-of-the-art technology to support NHS screening services, with the launch of digital communications utilising NHS Notify services expected in the first quarter of 2025/26. The private beta of personalised HPV home testing is scheduled for completion by the end of the second quarter, followed by a broader national rollout by the fourth quarter.
Supporting our workforce
The NHS Long Term Workforce Plan (LTWP), published in June 2023 set out ambitions for the workforce across three themes: Train; Retain; and Reform.
In January 2025, the overall NHS workforce increased by 2.6% compared to January 2024.
Train
In 2024/25, NHS England advanced its LTWP commitment to expand the clinical workforce through a coordinated student attraction campaign, an educator workforce strategy and other targeted initiatives. The national clearing campaign, delivered in partnership with UCAS, generated a 25% uplift in traffic to NHS Health Careers. These efforts are part of a broader drive to address falling applications to clinical programmes.
Despite some regional progress, overall student recruitment numbers have declined since the peak seen in 2021/22, and applications for clinical programmes continue to fall. Despite the number of new nursing and midwifery student recruits (new starters) in the first half of 2024/25 being 4% lower than 2023/24, they remain more than 10% higher than pre-pandemic levels, and new Allied Health Professional recruits were at their highest recorded level.
We have supported the allocation of an additional 350 medical school places in the 2025/26 academic year. This builds on an earlier expansion of 205 places in 2024/25 targeting new places in under-doctored areas to help ensure medical school places are available where they are most needed.
Retain
Over 774,800 people from 210 provider trusts participated in the 2024 Staff Survey, which is the highest response level to date. Results were similar to the previous year for all elements of the People Promise, with improved employee engagement scores noted following two years of decline.
The Sexual Misconduct Charter launched in October 2024, encouraging NHS providers to adopt a zero-tolerance approach to sexual misconduct in the workplace and to create a culture at work where everyone feels safe. The proportion of staff reporting unwanted sexual behaviour at work remains similar to 2023 – 8.8% from patients/service users and 3.7% from colleagues.
Staff retention continued to improve during 2024/25, with the overall NHS staff leaver rate standing at 10% as of December 2024 one of the lowest levels in over a decade and below the pre-pandemic rate of 10.7% recorded in December 2019. Organisations participating in the People Promise Exemplar Programme reduced leaver rates more significantly than non-exemplar trusts, collectively achieving an 11.8% greater reduction. At a national level, all rates (excluding sickness rates), are consistently reducing or stabilising at all-time lows.
Recommendations from the Kark and Messenger reviews to improve management and leadership in the NHS continued to be implemented in the year. A new programme was launched in September 2024 to transform NHS Management and Leadership over the next 2 years, to develop our leaders, set the right standards and to support talent and career development.
Reform
As part of our commitment to expand the NHS ‘Enhance’ programme to improve generalist skills across the first five years of postgraduate medical education for doctors in training, all Foundation doctors now have access to this programme.
Significant progress has been made in achieving our objective to improve the working lives of doctors in training by reducing duplicative payroll errors. In December 2024 payroll errors had been reduced by over 48% across 27 trusts, with targeted interventions achieving up to a 72% reduction in some cases.
We have worked with the General Medical Council to deliver our commitment to build on the Out of Programme Pause pilot to establish this programme as an accepted part of the training pathway. The pilot allows medical trainees to step out of formal training for up to a year to undertake a patient-facing UK based non-training post. We have invested in more pharmacy technicians, through a two-year apprenticeship, with the first cohort of over 500 set to join the community pharmacy workforce in 2026.
Spend on temporary staffing in the NHS has reduced, with 2.3% (£2.1 billion) of the total pay bill being spent on agency staffing in 2024/25, lower than the target of 3.2% (£2.6 billion), representing a significant cost saving and building on the £451 million reduction in the previous year. We have published several toolkits and have worked with providers and commissioners to support with maintaining strong establishment controls and ensure any significant workforce changes will improve workforce productivity.
Digital and data
We have improved patient care and productivity through digital technology and data, ensuring better outcomes for patients and better staff experience. We operate one of the public sector’s biggest live service technology estates, the “wiring” which connects the NHS and handles billions of transactions on which patients and staff depend every day. We have advanced major initiatives including the NHS App, the Federated Data Platform (FDP), Electronic Patient Records (EPR) and the NHS Research Secure Data Environments Network. Through our NHS IMPACT and Get It Right First Time programmes, we support the front line to standardise care and continuously improve services using improvement science and data driven clinical peer review.
Live services
We operate over 200 live services including everything from systems which protect children, to those which monitor over 1.9 million computers to detect and prevent cyber threats. Spine, the national health information system on which patients and staff rely on every day, securely processed over two billion transactions this year. Our new Digital GP Registration enables online patient registration with local GPs, with over 60% of registrations completed online as of March 2025. The new Record a Vaccination Service simplifies vaccine data recording, with over 600,000 vaccinations logged since its introduction.
NHS App
The NHS App is the digital gateway to the NHS, providing secure and convenient access to health information and appointment bookings. This year, 94% of the population can manage secondary care referrals directly through the NHS App, reducing Did Not Attend (DNA) rates by over 500,000. It also supports prescription management with over 7.2 million patients managing their prescriptions digitally and 4.8 million repeat prescriptions ordered.
NHS Notify, a new service integrated with the NHS App, enables direct communication with patients, driving substantial savings and further reducing DNA rates. We estimate that around £450 million is spent on patient communications by the NHS annually. The NHS App sends unlimited messages for free. The NHS App has saved over 2 million hours of admin time and 890,000 hours of GP time, alleviating pressure on urgent care services.
Improving the digital maturity of frontline services
We improved the digital maturity of trusts nationwide, by aligning providers with the standards set in our What Good Looks Like framework.
By March 2025, 92% of trusts in England have implemented EPR systems, with 40% reaching the highest capability standards. We are working with the remaining trusts to deploy these systems safely. EPR systems improve patient safety and productivity, resulting in a 13% reduction in the cost per episode of care, a 4% reduction in length of stay, and a 17.5% reduction in sepsis mortality.
Recognising pressures in social care, by the end of March 2025 we had supported 77% (April 2024: 66%) of CQC-registered care providers to implement Digital Social Care Records.
This shift is enhancing coordination and continuity of care across the social care system with evidence suggesting at least 20 minutes have been saved per care worker, per shift, as well as time savings across other roles in providers.
Federated Data Platform
The NHS FDP, which was launched in November 2023, integrates operational data to support healthcare professionals with secure information access, enhancing coordinated care and
data-driven decisions. As of March 2025, 72 provider trusts use FDP products and 39 of 42 ICBs have benefitted from the platform.
The FDP has improved elective surgeries, reduced backlogs and ensured timely patient care. By the end of March 2025, the FDP had supported 2.1 million patient pathway (referral to treatment) actions and checks to be completed, helping to ensure patients are treated within NHS recommended target times. Through supporting improved theatre utilisation, on average by more than 8%, an additional 74,996 patients had undergone their procedures in theatres. The FDP has further enabled around 286,000 patients to be safely removed from inpatient and outpatient waiting lists.
The FDP OPTICA product is supporting discharge management in acute settings so that patients are experiencing shorter waits when ready for discharge. An average reduction of 18% in discharge delay days has been observed among patients with the longest stays in hospital, within trusts utilising the FDP OPTICA product.
Cyber
Over the past year, the NHS has bolstered its cyber resilience to counter advanced cyber-attacks and the rapid evolution of artificial intelligence. Our Cyber Security Operations Centre monitors over 1.9 million devices around the clock, preventing numerous disruptive attacks.
We have conducted over 800,000 phishing simulations, launched educational cyber podcasts, and introduced ransomware detection and prevention capabilities. We also issued 160 Cyber Alerts on critical IT vulnerabilities. The Cyber Associates Network, with over 2,800 security professionals, plays a crucial role in sharing information and building cyber capabilities.
Their efforts were vital in responding to the Synnovis pathology attack in June 2024, demonstrating the importance of Cyber Operations in maintaining a secure NHS environment.
Innovation, research and life sciences
NHS England has a legal duty to facilitate and promote research and to promote innovation.
We have continued to support innovation, research, and the life sciences to improve patient outcomes and staff experience, whilst reducing health inequalities.
Research and innovation are more important than ever, playing a crucial role as the NHS seeks to address operational pressures and increase productivity. These factors also mean that frontline staff, researchers, and the life sciences industry report a challenging picture broadly in the health innovation ecosystem. Work has therefore continued to ensure that the NHS remains a partner for research and innovation.
During the reporting period, key activities included:
- Support for over 590,000 people to sign up as research volunteers through the National Institute for Health Research (NIHR) Be Part of Research portal.
- The implementation of the National Contract Value Review process across all phases of clinical trials contributing to a 36% reduction in commercial clinical trial set up times.
- In April 2024, NHS England published guidance to help providers understand research finance, which differs from NHS finance more generally.
- Through the Research Engagement Network Development programme, allocated £4.5 million to ICB-NIHR-VCSE partnerships in all 42 ICBs. This resulted in more than 28,000 people from underserved communities attending Research Engagement Network public-facing events. More than 10,000 people, including 280 community champions, were invited to join research studies.
- Accelerated access to data for research through the NHS Research Secure Data Environment (SDE) Network. SDEs supported over 240 research studies, surpassing the target of 192.
- Supported nine national priority trials through NHS DigiTrials, recruiting 8,000 participants for heartburn research and 400 for melanoma studies.
- Identified 20 Alzheimer’s Disease digital technologies to enter the National Institute for Health and Care Excellence Early Value Assessment process using our Horizon Scanning capabilities.
- Welcomed the latest cohort onto the NHS Clinical Entrepreneur Programme, taking the total number of entrepreneurs supported on the programme to over 1,100. We also launched the first Patient Entrepreneur Programme.
- Appointed 27 fellows to the NHS Innovation Accelerator programme, the largest cohort yet, who will receive mentoring and tailored support to scale their innovations.
- Supported 18 NHS Innovation Sites through the InSites programme, to build capacity and capability for adoption and scale of innovations which map to their local population health needs.
- Undertaken significant system modelling and forward planning activity to support system readiness and pathway transformation needed to adopt innovative new medicines that could impact over 650,000 patients.
- The Digital Trailblazer programme supported 3 NHS Talking Therapies sites through a 100-day challenge to optimise patient-facing digital tools, leading to measurable improvements in access to Digitally Enabled Therapy.
- The SBRI Healthcare competition awarded £1.7 million to nine innovative projects focused on enhancing workplace mental health through digital solutions. Supported over 1,000 innovations and innovators through the NHS Innovation Service an online platform that helps innovators introduce new solutions to the NHS. 172 were also given a route to market.
System working
In 2024/25, NHS England has supported ICBs and their partners to develop their systems to meet their population’s health needs, by providing further clarity on roles and responsibilities of individual organisations, and how systems can organise their decision making to hold each other to account for delivery of shared system plans and system statutory duties.
The publication of The Insightful Board guidance provides advice on what information NHS boards should pay attention to in discharging their duties.
To support systems to meet local population health goals through the development of their place architecture, NHS England has developed a working toolkit to help local areas consider different approaches to accountability, delegation, contracting and commissioning. In January 2025, NHS England also published Neighbourhood health guidelines which set out the core components of a neighbourhood health model that every ICB should be delivering.
NHS England has continued to provide support to ICBs to implement population health management (PHM) capabilities this year. There are now over 12,500 members of the nationally hosted PHM Academy which provides a range of e-learning for neighbourhood teams, good practice case studies and guidance on more technical aspects of joining up data and analysing risk factors. Additionally, there have been 11 peer learning events this year for ICB teams to understand how to implement PHM and learn from international best practice.
NHS England has also supported provider collaboratives during the year, to fully realise the benefits of working at scale and encourage best practice in meeting system priorities. This has included delivery of a programme of webinars, case studies and peer learning sessions.
Independent patient choice and procurement panel
Since 1 January 2024 NHS England has hosted the independent panel for patient choice and procurement (NHS commissioning » Panel reports). The panel has responsibility for:
- reviewing representations from providers about qualification of providers by ICBs for services where the legal rights to choice apply.
- providing advice to relevant authorities about decisions under the Provider Selection Regime.
Cases can be referred to the independent panel where other processes have not resolved the issues. During 2024/25 the panel published advice on six provider selection cases.
Sustainability
The NHS has committed to reducing greenhouse gas emissions (GHGs) under our direct control (the NHS Carbon Footprint) to 3,200 ktCO2e by 2028 to 2032 and to net zero by 2040. Estimated emissions in 2024/25 were 4,350 ktCO2e, down from an updated estimate of 4,450 ktCO2e for 2023/24. Further breakdown is provided on page 194. Progress was supported by targeted action across the NHS during 2024/25, including:
- £900k to support a reduction of nitrous oxide waste, which has been shown to be up to 80% at some sites.
- Increasing electrification across the NHS fleet, with 10% of all vehicles now zero emission.
- Securing over £200 million to decarbonise the estate, through the Public Sector Decarbonisation Scheme, taking the total awarded to the NHS through Public Sector Decarbonisation Scheme to over £1 billion.
- Investing around £90 million in energy efficiency measures, through the National Energy Efficiency Fund.
- The announcement in March 2025 that £100 million would be jointly invested with Great British Energy in solar generation projects across the country.
This estimate, combined with evidence of action across the NHS, suggests that in 2024/25 the NHS was on track to meet our commitments for 2028-32 and demonstrates progress towards our ambitious 2040 net zero target.
Chief Financial Officer’s report
The financial statements for the year ending 31 March 2025 are presented later in this document on a going concern basis (as per Note 1.5 of the accounts) and show the performance of both the consolidated group – covering the whole of the commissioning system – and NHS England as the parent of the group. The group comprises NHS England the 42 ICBs and Supply Chain Coordination Ltd (SCCL).
As part of the merger of NHS England, NHS Digital and Health Education England, NHS England successfully delivered a 35% reduction in its organisational size, resulting in £490 million of savings. In addition, through robust financial management and further efficiencies in central NHS England costs, an additional £306 million in savings was achieved. In total, £500 million of these savings were reinvested into frontline services, directly supporting patient care and system delivery. Across systems, the total efficiency in 2024/25 totalled £8.7 billion.
This represents a 21% increase compared to the £7.2 billion of efficiencies delivered in 2023/24.
NHS England is required to manage total NHS spending within a fixed revenue limit. The total General RDEL limit for 2024/25 was £190,990 million.
Funding and allocations
In 2024/25, core funding for the NHS on a like-for-like basis increased by 0.2% taking account of the funding announced at the Spring Budget. An additional £2.3 billion was allocated to NHS systems to support them in achieving financial balance and breaking even. During the year, further funding was made available to meet emerging and exceptional pressures. This included £5.7 billion to cover the higher-than-anticipated costs of the 2024/25 pay awards, which affected multiple staff groups across the NHS. A further £184 million was allocated to offset the additional costs arising from industrial action, ensuring continued service delivery and mitigating financial risk to providers.
Additional funding was also agreed for technology investment and the ongoing delivery of the COVID-19 vaccination and testing programmes.
ICB allocations continued to include the Elective Recovery Fund, made available by the Government to support the recovery of elective waiting lists. The allocations issued through ERF totalled £6.2 billion.
From 1 April 2024, 20 ICBs in East of England, Midlands and Northwest regions took on delegated responsibility for the commissioning of specialised services, and received an additional allocation related to those services. From 1 April 2025, all 42 ICBs have now taken delegated responsibility for the commissioning of specialised services.
Operational pressures
Over the year, ICBs and trusts worked with local authorities to improve discharge processes and increase capacity to support timely discharge from hospital. There was a small reduction in levels of delayed discharges compared to 2023/24 however challenges remain. On average there were around 12,633 patients per day with delayed discharges, highlighting the continued pressure on flow across health and social care services.
Recurrent capacity funding to support systems to deliver improved urgent and emergency care performance was added to core programme allocations in 2024/25. A&E performance improved from 74% in March 2024 to 75% in March 2025. Latest published figures show that the number of patients in a Virtual Ward (also known as hospital at home) decreased by 1% in the past year, (July 2024: 9,132, July 2025: 9,002).
The NHS has delivered around £8.7 billion of savings and continues to deliver improvements in productivity of around 2%, allowing us to improve operational performance in key areas including reducing elective waiting lists. The waiting list decreased by 120k in 2024/25 and Referral to Treatment Time performance improved by 2.6 ppt.
Timeliness of local accounts
In preparing the NHS England group accounts based on consolidation schedules from ICBs, we are reliant on each ICB submitting their audited annual report and accounts to us. We and the DHSC issue directions to NHS bodies on the timing by which these should be submitted.
There are many reasons why a set of audited accounts for a local NHS body may go beyond the deadline: for example, this may reflect illness in the preparer finance team or audit team, or a significant issue may be encountered that takes time to resolve, which may reflect weaknesses in an entity’s preparation of its accounts. Auditors need to be able to complete their work independently of outside influence and take the necessary time to ensure their audit opinion is the right one and supported by appropriate audit evidence. It is also important that there is a properly functioning local audit market to allow audited bodies to hold their auditors to account for delivery. We welcome the Financial Reporting Council’s publication of its NHS audit market study.
The timeline on which these national accounts are finalised depends on both when the deadline for local audited accounts is set, and compliance with that deadline. For many years prior to 2019/20 the local audit deadline in the NHS was around the end of May. The deadline is set in consultation with the audit firms on what they are willing to sign up to. In recent years the local audit deadline has been around the end of June.
In recent years in the NHS England annual report, we have described NHS England’s limited direct role in NHS audits but detailed the steps we have been taking to improve compliance with the local deadline for audited accounts in the NHS.
More NHS bodies achieved the deadline for submission of audited accounts in 2024/25 than in recent years. 92% of local NHS bodies (being NHS providers and ICBs) met the deadline in 2024/25, the highest proportion since 2019/20. All ICBs submitted audited accounts on time this year, (2023/24: 90%, 2022/23: 74%).
NHS England and the DHSC have worked closely with the Ministry of Housing, Communities and Local Government on the relevant elements of its work to reform ‘local’ audit. In July 2025 MHCLG laid the English Devolution and Community Empowerment Bill before Parliament, part four of which makes changes to the local audit system in England and Wales. The reforms include establishing the Local Audit Office, a body to coordinate local audit with responsibilities including determining the framework for auditors to follow, rules for eligibility to be a local auditor, and inspection and enforcement. Bringing these functions together will help set the foundation to strengthen the audit market. These changes directly apply to audits of NHS trusts and ICBs; the DHSC and NHS England are exploring ways to replicate them for NHS foundation trusts.
As well as reforms to the local audit system, we have continued our broader work to improve timeliness in NHS financial reporting including:
- encouraging auditors to give clear reporting to audit committees where the preparer’s quality of draft accounts or working papers needs to improve
- working closely with NHS bodies to ensure they appoint external auditors in good time, which helps increase the likelihood of deadlines being achieved
- working with NHS bodies where financial reporting issues arise to ensure they are able to address findings effectively
- regular engagement with the audit firms and responding to their feedback to continue to strengthen the NHS financial reporting landscape, and working with partners to make sure training and guidance is available for preparers and
- liaising with broader stakeholders on wider matters that can cause delays in NHS accounts.
NHS England and the DHSC have an ambition to return to laying the main national consolidated accounts (being the DHSC group, NHS England group and consolidated provider accounts) before Parliament in advance of the summer Parliamentary recess in July. Achieving this in the years ahead would require the audit community to accept a significantly earlier deadline for audited accounts than is currently the case. At the present time it is not clear that this is achievable in the short term. We will continue to focus on streamlining processes for preparation and audit of local and national accounts to the extent this falls within our role to seek to facilitate the earlier finalisation of accounts wherever possible.
Financial performance
Revenue Department Expenditure Limit (RDEL) general (non-ringfenced)
The DHSC sets several technical financial targets for the NHS England Group, including the core operational limit (general RDEL) described in the table below. These limits are ringfenced, which means that underspends on the other revenue limits cannot be used to support core patient services covered by the general RDEL limit.
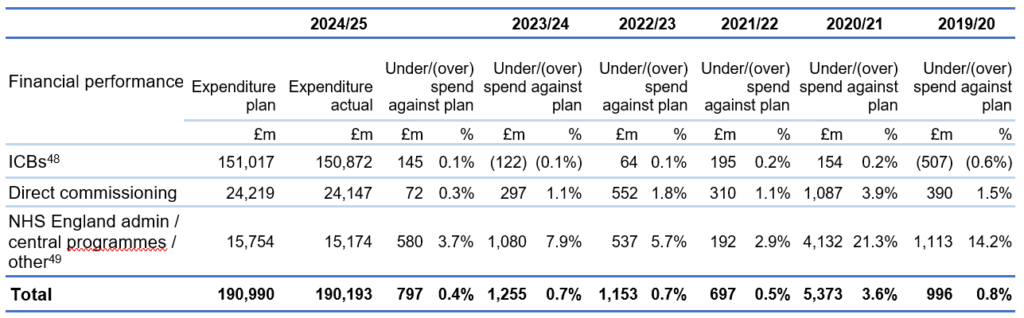
2024/25 performance against key financial performance duties
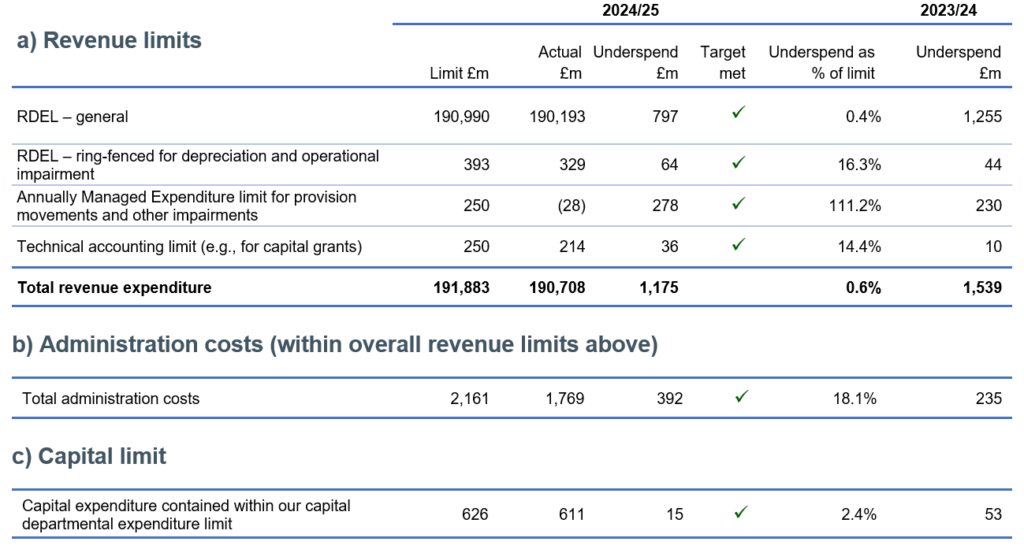
Financial priorities for 2025/26
Our priorities continue to centre on the recovery of core services and productivity across the NHS. Key to delivery is making sure that the frontline of the NHS has the resources and support it needs to deliver on our priorities for patients, with a focus on reducing the time people wait for elective care, improving A&E waiting times and ambulance response times, improving patients’ access to general practice and urgent dental care, and improving patient flow through mental health crisis and acute pathways, including improving access to children and young people’s mental health services.
At the heart of delivery are our staff. We must continue to recognise their ongoing efforts and ensure that all colleagues are well supported, so that they can keep doing their best work for patients.
For 2025/26 we will be working with ICSs to:
- reduce ICB running costs by 50% and reversing corporate cost growth by 50% across NHS providers, as well as in NHS England ahead of the integration with the DHSC (NHS England » Working together in 2025/26 to lay the foundations for reform).
- support the delivery of system financial plans, with targeted support for the more financially challenged systems to help them recover and maintain financial stability over the medium term.
- reduce agency and bank spend as a proportion of the total pay costs for the year, by 30% for agency and 10% for bank (NHS England » Revenue finance and contracting guidance for 2025/26).
- use the specific resources we have been provided with to reduce the number of people waiting for elective procedures, with a continued focus on improving access to planned care and addressing long waits.
- maintain robust spending controls and deliver care as efficiently as possible in the context of ongoing operational constraints. We will also intervene proactively where there is a risk of non-delivery to board approved plans ensuring accountability and timely course correction.

