Executive summary
This primary medical services policy and guidance manual (PGM) provides a suite of policies and guidance that should be followed by all commissioners of NHS primary medical services.
This approach ensures that commissioners, providers and most importantly patients are treated equitably, and that NHS England and its commissioners can meet their statutory and/or delegated duties.
The PGM is updated and refined periodically to reflect changes in legislation, contracts or central policy and guidance.
Note: substantive policy and guidance changes or additions in this update are highlighted in the Summary of changes to the Primary medical services policy and guidance manual document. Some content has also been moved or summarised to improve navigation or readability.
1. Introduction
1.1 NHS England became responsible for direct commissioning of primary medical services on 1 April 2013. Since 1 July 2022 this responsibility has been delegated to integrated care boards (ICBs). The responsibilities delegated to ICBs are set out in the standard delegation agreement entered into between NHS England and each ICB.
1.2 The PGM is mandated guidance under the delegation agreement and provides the policies and guidance ICBs must observe to support a consistent and compliant approach to primary medical services commissioning and contract management across England.
1.3 The PGM identifies sections which describe mandatory functions (that is, those absolutely defined in legislation and law) versus those which are provided as national policy, guidance or best practice.
1.4 The PGM is also supported by a legacy suite of e-learning modules to provide commissioners with a deeper appreciation of some of the more complicated or frequent commissioning/contract management scenarios they may face. These are subject to review to align with this latest PGM update but can be accessed via the links below:
- approving GP practice boundary changes
- special Allocation Schemes
- GP contractor changes: incorporation and novation
- developing a primary medical care service procurement strategy
- handling threats to the continuity of GP services
Users require an account with NHS England’s e-Learning for Healthcare. Each module should only take 30–40 minutes to complete. Commissioners are invited to suggest areas where additional e-learning content would be helpful.
Change control and transitional arrangements
1.5 The PGM is updated and refined periodically and following changes in legislation, contracts or central policy and guidance. Users of this PGM are therefore advised this is a controlled document and the most up to date version should always be used, which is published on NHS England’s website.
1.6 This PGM replaces all previous versions. The processes and procedures set out in this PGM must be followed where a matter arises after the date of publication of this PGM.
1.7 Where a matter arose prior to the publication of this PGM (and the parties are therefore following a previous policy), the parties should continue to follow that previous policy as this would have been the expectation of the parties at the time.
1.8 Parties following a previous policy should consider switching to the relevant policy set out in this PGM if there is a natural transitional point in the matter and provided all parties agree.
2. The legislation, abbreviations and acronyms
2.1 The legislation and law applying to primary medical services may be amended from time to time. It is important that users of the PGM are familiar with the relevant in force published documentation.
2.2 The PGM must be read in conjunction with the relevant law, which may not be repeated in full in this PGM.
2.3 However, to assist users of the PGM, the links below provide access to the relevant documents’ content pages from where the user may find the appropriate section, regulation, etc:
- Equality Act 2010
- Equality Act 2010 (Specific Duties and Public Authorities) Regulations 2017
- National Health Service Act 2006
- Health and Social Care Act 2012
- Health and Care Act 2022
- The National Health Service (General Medical Services Contracts) Regulations 2015
- The National Health Service (Personal Medical Services Agreements) Regulations 2015
- The Health Care Services (Provider Selection Regime) Regulations 2023
Note: while www.legislation.gov.uk updates legislation, at any point in time there may be outstanding amendments. Therefore, users are advised to ensure they are familiar with current amendments pending any updating as appropriate.
2.4 The law published in directions can be found on the gov.uk website and, at the time of publishing this PGM, the links below provide access to relevant documents as originally published as a whole and from where the user may find the appropriate direction and paragraph:
- Alternative Provider Medical Services Directions (2022)
- The Primary Medical Services (Directed Enhanced Services) Directions 2022
Note: any subsequent amending directions are not updated, and users are advised to ensure they are familiar with current amendments until any subsequent publication as appropriate.
2.5 The following abbreviations and acronyms are used in the PGM:
|
APMS |
alternative provider medical services | |
|
APMS Directions |
Alternative Provider Medical Services Directions | |
|
CATS |
commissioning and transformation support | |
|
COSHH |
control of substances hazardous to health | |
|
CQC |
Care Quality Commission | |
|
GMS |
general medical services | |
|
GMS Regulations |
The National Health Service (General Medical Services Contracts) Regulations 2015 | |
|
GMS SFE |
General Medical Services Statement of Financial Entitlements Directions | |
|
GP | general practitioner |
|
|
HWB |
health and wellbeing board | |
|
ICB |
integrated care board | |
|
ICS |
integrated care system | |
|
LMC |
local medical committee | |
|
NBM |
new business models | |
|
NHS Act |
National Health Service Act 2006 | |
|
PSR |
Provider Selection Regime | |
|
NHSR |
NHS Resolution | |
|
PCA |
Primary Care Appeals (Part of NHSR) | |
|
PCSE |
Primary Care Support England (delivered by Capita on behalf of NHS England) | |
|
PCN |
primary care network | |
|
PCRM |
Primary Care Registration Management | |
|
PDS |
Personal Demographics Service | |
|
PHSO |
Parliamentary and Health Service Ombudsman | |
|
PMS |
personal medical services | |
|
PMS Regulations |
The National Health Service (Personal Medical Services Agreements) Regulations 2015 | |
|
TUPE |
Transfer of Undertakings (Protection of Employment) Regulations 2006 | |
2.6 This acronym buster may also be helpful as it provides a list of NHS acronyms broader than those used in this document. For an understanding of the NHS, see An introduction to the NHS.
2.7 Reference to external legislation or guidance may be required to ensure access to current wording, mitigating the need to update the PGM where hyperlinks to such changes may be provided.
3. General
This PGM is divided into 4 parts:
Part A: Excellent commissioning and partnership working
Part B: General contract management
3.1 Each part has headed numbered chapters with headed numbered sub-sections, which can be found in the contents table at the beginning of the PGM.
3.2 Reference to external legislation or guidance may be required to ensure access to current wording, mitigating the need to update the PGM where hyperlinks to such changes may be provided.
3.3 Where templates are provided these are hyperlinked if published elsewhere or embedded as extractable documents for easier onward use.
3.4 For the purposes of the PGM, the commissioner of the service is not always referred to by name but simply as the ‘commissioner’. This reflects the fact the identity of the commissioner in an area is an ICB with delegated responsibility from NHS England.
3.5 For matters which have not been delegated to ICBs (or which are not able to be carried out by an ICB) the commissioner will be NHS England.
3.6 The delegation agreement sets out the matters for which the ICB has decision-making responsibility. Where the delegation agreement sets out obligations on the ICB – for example, liaising with NHS England in relation to managing disputes – the relevant PGM chapter refers to the delegation agreement and highlights relevant points.
Part A: Excellent commissioning and partnership working
1. Commissioning described
1.1 ICB delegated commissioning arrangements
1.1.1 From July 2022, ICBs assumed delegated responsibility for primary medical services excluding section 7A Public Health functions. From April 2023 ICBs assumed delegated responsibility for dental (primary, secondary and community), general ophthalmic and pharmaceutical services.
1.1.2 NHS England retains reserved functions such as performers list management, and wider aspects of professional regulation. Further functions retained nationally include:
- identifying national priorities, setting outcomes and developing national contracts or contractual frameworks
- maintaining national policies and guidance that will support ICBs to be effective in their delegated functions
- delivering support services
1.1.3 NHS England retains overall accountability for the discharge of its responsibilities delegated to ICBs and therefore requires the necessary assurance that its functions are being discharged safely, effectively and in line with legal requirements. Oversight and assurance of ICBs’ delegated commissioning of primary medical services is covered outside this PGM.NHS England remains legally accountable to the Department of Health and Social Care (DHSC), led by the Secretary of State, which is in turn accountable to Parliament.
1.1.4 NHS England remains legally accountable to the Department of Health and Social Care (DHSC), led by the Secretary of State, which is in turn accountable to Parliament.
1.2 Primary care networks
1.2.1 Primary care networks (PCNs) build on the core of existing primary care services to enable greater provision of proactive, personalised, co-ordinated and more integrated health and social care, with greater collaboration between general practice and other local system partners including community pharmacy, local authorities, social care, community providers, mental health providers and voluntary services. Clinicians described this as a change from reactively providing appointments to proactively caring for the people and communities they serve. PCNs also help to provide stability and resilience for practices.
1.2.2 PCNs are based on GP registered lists and are made up of a practice or practices (and possibly other providers) typically serving natural communities of around 30,000 to 50,000 people. These parameters mean that PCNs are small enough to provide the personal care valued by both patients and GPs, but large enough to have impact and economies of scale through better collaboration between practices and others in the local health and social care system.It is important that PCNs and neighbourhood collaborations work together, fostering an environment where best practices are shared and unwarranted variation and health inequalities are reduced, while still allowing for personalised, patient-centred care.
1.2.3 NHS England has published the Network Contract DES: contract specification for 2025/26 – PCN requirements and entitlements, setting out eligibility requirements and the rights and obligations of practices, PCNs and commissioners under the DES. A range of additional information is provided on the NHS England GP contract page to assist commissioners and providers further.
1.2.4 NHS England has published the Network Contract DES: contract specification for 2025/26 – PCN requirements and entitlements, setting out eligibility requirements and the rights and obligations of practices, PCNs and commissioners under the DES. A range of additional information is provided on the NHS England GP contract page to assist commissioners and providers further.
2. General duties of NHS England (including addressing health inequalities)
2.1 Introduction
2.1.1 This chapter outlines the general duties that must be complied with and that are likely to affect the decisions commissioners take regarding the provision of primary care.
2.1.2 In many instances the duties placed on NHS England are mirrored by similar duties placed on ICBs. We have highlighted the equivalent ICB duty. However, this note does not cover any further ICB duties that apply only to ICBs and not to NHS England.
2.1.3 There are many general duties on commissioners. It is important that decision-makers are familiar with all these duties because if a duty has not been complied with when a decision is taken, that decision can be challenged in the courts on the grounds that it is unlawful.
2.1.4 This guidance looks at the general duties that commissioners are required to comply with that are most applicable to primary care, providing examples to illustrate how they might affect decision-making.
2.1.5 As has been noted, under delegation arrangements NHS England retains the legal responsibility for compliance with the duties in respect of primary medical services commissioning. Accordingly, NHS England will require assurance that its statutory functions are being discharged effectively by an ICB. This underlines the importance of compliance with the duties outlined in this chapter.
2.2 Equality and health inequalities duties
2.2.1 This section considers equality and health inequality duties. First, the duties under the Equality Act 2010 are considered followed by the other health inequality-related duties. NHS England’s Equality and Health Inequalities Unit has a resource hub with information. Additionally, the Equality and Human Rights Commission publishes a wealth of information.
Equality Act 2010
2.2.2 Commissioners have both general and specific equality related duties under the Equality Act 2010. The general duty can be found in section 149 of the Equality Act. It is known as the public sector equality duty or the PSED. The specific duties are imposed on commissioners by secondary legislation, namely the Equality Act 2010 (Specific Duties and Public Authorities) Regulations 2017.
2.2.3 Further details on both the PSED and the 2017 Regulations are provided in the sections below.
2.2.4 The duty to have regard to the PSED will arise when commissioners are exercising their functions. A commissioner will be open to legal challenge if it is unable to demonstrate its regard to the PSED when publishing guidance or policies or making decisions. A failure to comply with the prescribed duties outlined in the 2017 Regulations will also be unlawful. Guidance on the PSED can also be found on the Equality and Human Rights Commission website.
The protected characteristics
2.2.5 The Equality Act 2010 prohibits unlawful discrimination in the provision of services (including healthcare services) on the basis of “protected characteristics”.
The protected characteristics are:
- age
- disability
- gender reassignment
- marriage and civil partnership
- pregnancy and maternity
- race
- religion or belief (which can include an absence of belief)
- sex
- sexual orientation
Unlawful discrimination
2.2.6 Unlawful discrimination can also occur if a person is at a disadvantage because of a combination of these factors.
There are broadly 4 types of discrimination in the provision of services that are unlawful under the Equality Act 2010. (Unlawful discrimination is also prohibited in the field of employment and other areas but these are not covered in this guidance.)
Public sector equality duty
2.2.7 The general public sector equality duty can be found in sections 149 to 157 of the Equality Act 2010.
2.2.8 The Equality Act 2010 requires commissioners to have “due regard” to the need to:
- eliminate discrimination that is unlawful under the Act
- advance equality of opportunity between people who share a protected characteristic and people who do not share it; and
- foster good relations between persons who share a protected characteristic and persons who do not share it
2.2.9 These objectives are often referred to as the “three aims” of the PSED. The aims are amended for the protected characteristic of marriage and civil partnership. Commissioners do have to have due regard to eliminate unlawful discrimination based on marriage and civil partnership (the first aim). However, they are not required to have due regard to the need to advance equality of opportunity or foster good relations in relation to marriage and civil partnership (the second and third aims).
2.2.10 Compliance with the 3 aims of the PSED can require a commissioner to take positive steps to reduce inequalities. In this regard the Act permits treating some people more favourably than others but not if this amounts to unlawful discrimination (what is meant by unlawful discrimination is considered above). The PSED has been used successfully on many occasions to challenge changes to services.
2.2.11 This means that a commissioner has a duty to help eliminate any unlawful discrimination practised by the providers of primary care: for example, through requiring premises to be accessible. Failing to use its negotiating power to secure such changes could be seen as a breach by a commissioner of the PSED, as well as a breach of the non-discrimination rules by the service provider.
Example
After a site visit the commissioner becomes aware that consulting rooms in a GP surgery are no longer accessible to those with limited mobility as they have been moved upstairs.
The commissioner decides that as there are no consulting rooms downstairs and there is no lift or stair lift, this is a breach of the practice’s duty to make reasonable adjustments under the Equality Act 2010.
This in turn is a breach of the practice’s duty under its contract with the commissioner to comply with legislation. To comply with the PSED, the commissioner takes steps to ensure that the practice complies with its Equality Act duties by raising the issue informally and issuing a breach notice if the problem is not remedied.
Example
A hearing impaired patient complains to the commissioner about their experience with a local (NHS commissioned) provider. The patient was unable to communicate effectively with the provider because of their hearing impairment.
When the patient suggested that the provider obtain a sign language interpreter to translate for them, this was refused. It is likely that the provider will be in breach of its obligations under the Equality Act 2010 to make reasonable adjustments. To comply with the PSED, NHS England takes steps to investigate and enforcement action if needed.
2.2.12 Carrying out appropriate equality and health inequalities impact assessments (EHIAs) is usually critical to proving discharge of the PSED, although they are not as such a legal requirement. This is because if there is no assessment of the impact of a possible change on groups with protected characteristics, it is very difficult to argue that the commissioner had the impact properly in mind when it made its decision. This is the case even if the impact on protected groups is minimal.
2.2.13 It is not always easy to assess the equality impact. A robust service user involvement exercise will help the commissioner to identify any issues. It is advisable to ask question(s) directly aimed at equalities issues. In many cases, it is advisable to take special steps to reach seldom heard groups affected by the decisions: for example, by working with local voluntary, community and faith sector groups and holding meetings in community venues. The more likely a decision is to disproportionately affect a protected group, the more important it is to get feedback from that group about the decision. Undertaking a literature search can also be helpful to see what evidence is available.
2.2.14 The PSED means that the commissioner must consider equalities issues when making decisions. In some cases, there may be a solution that causes less disadvantage to a protected group but for other reasons is undesirable. In these situations, it is important to acknowledge the disadvantage, work towards reducing the negative impact caused and be clear about why the decision was taken. This may include outlining cost concerns. It also makes sense to monitor the situation – for example, to understand if the demographic of service users changes as a result of the decision – and timetable a formal review in, for example, a year’s time.
2.2.15 There are a few themes arising from the cases we have seen on the application of the PSED (and similar duties in previous legislation):
- a need to explicitly recognise that the PSED applies and equalities issues need to be considered
- the duty is an ongoing one – to be considered at all stages of decision-making not just at the end
- a need to be clear about the factors driving a decision, even if these are unpalatable: for example, budgetary pressures
- a need to analyse in some detail the impact of a proposed policy or decision so that the public authority has a clear idea of who is affected and how. Statements of impact need to be supported by evidence where possible
- if a decision is made that will impact negatively on a protected group, that should be acknowledged and the rationale explained
- there should be a detailed consideration as to how any negative impact of the decision could be mitigated. If the steps identified are not practicable, this should be explained
- the duty must be complied with at the time of the decision. Reasoning is rarely allowed after the event, so a record should be made at the time about how equalities issues were considered
The Equality Act 2010 specific duties
2.2.16 In addition to the PSED, NHS England and ICBs are also required to comply with the specific duties contained in the Equality Act 2010 (Specific Duties and Public Authorities) Regulations 2017.
2.2.17 The 2017 Regulations came into force on 31 March 2017. The 2017 Regulations replace the first set of specific duty regulations made in 2011.
2.2.18 The 2017 Regulations among other things require commissioners to publish:
- equality objectives that should be achieved to comply with the PSED (Regulation 5). This had to be done by 30 March 2018 and the objectives need to be updated once every 4 years. ICBs should ensure that they are familiar with NHS England’s equality objectives, which are published on the resource hub
2.2.19 The Equality and Human Rights Commission can, under sections 31 and 32 of the Equality Act 2006, investigate and enforce a failure to comply with the PSED or the specific duties. Alternatively, a failure to comply with the general and specific duties could be challenged by way of judicial review. Such a claim could be brought by a person or group directly affected by a failure to comply with these duties.
Health inequalities duties and the NHS Act 2006 (as amended by the Health and Social Care Act 2012)
2.2.20 Under the Health and Social Care Act 2012 commissioners are required to have regard to the need to:
- reduce inequalities between patients with respect to their ability to access health services
- reduce health inequalities between patients with respect to the outcomes achieved for them by the provision of health service
2.2.21 When making decisions about primary care – particularly about service changes – decision-makers will need to bear in mind the impact on health inequalities. To do this the commissioner will need some data on existing health inequalities, and to consider whether its decision can be used to diminish these. A vast amount of data is available – for example, in joint strategic needs assessments (JNSAs) and Right Care packs – to help commissioners identify health inequalities in their area.
2.2.22 The key point is that the commissioner can show (through documentation, principally an EHIA) that the impact a decision will have on health inequalities has been considered, and that its decision is based on some relevant data and evidence.
2.2.23 NHS England has published resources to assist organisations to find out about information, resources and action being taken to reduce health inequalities in England. Local JSNAs prepared by local health and wellbeing boards, NHS oversight framework indicators and NHS RightCare can be valuable sources of information about local health inequalities.
2.3 The regard duties
2.3.1 The “have regard”, “act with a view to” or “promote” duties under the National Health Service Act 2006 form a loose hierarchy of legal duties:
- the duty to have regard means that when taking actions, a certain thing must be considered
- the duty to promote means action must be taken that actually achieves an outcome. Additionally, it is possible to promote something by encouraging others to do it
- the duty to act with a view to means that action must be taken with a purpose in mind
2.3.2 In contrast to the promotion duties and the view to duties, the regard duties apply to every action of a commissioner where it is carrying out its primary care functions. (Pausing there, the duty will not normally apply to “private law” decisions that would be taken by any private sector organisation: for example, leasing estate.)
2.3.3 The PSED cases are the best guide that we have to how a court would interpret a commissioner’s regard duties under the NHS Act 2006. We can learn from these that:
- Commissioners that have to take decisions must be made aware of their duty to have regard to the various issues outlined in the duties. Failure to do so will render the decision unlawful.
- The regard duties must be fulfilled before and at the time that a particular decision is being considered. If they are not, any attempts to retrospectively justify a decision as consistent with the regard duties will not be enough to discharge them.
- Commissioners need to engage with the regard duties with rigour and with an open mind.
- It is good practice for the decision-maker to refer to the regard duties.
- It is not possible for the commissioner to delegate the duties to another organisation to comply with. This applies in respect of NHS England delegated arrangements for primary care services (see section 1.1 above). NHS England will always have to comply with its duties under the NHS Act 2006, even if an ICB is carrying out commissioning on its behalf. However, it is a requirement of the delegation agreement that ICBs act in such a way that enables NHS England to comply with its duties. If a commissioner acts through contractors, it must ensure as necessary that they act consistently with the duties.
- The regard duties are continuing ones that apply throughout decision-making. It is not enough to only ‘rubber stamp’ a decision by reference to the regard duties at the end of a decision-making process. The regard duties need to be borne in mind throughout.
- It is crucial to keep an adequate record of how the regard duties are considered. If records are not kept it will be more difficult, evidentially, for the commissioner to persuade a court that the duties imposed have been fulfilled.
2.3.4 One key point to understand is that there is no obligation to achieve the object of the regard duties. For example, it is not unlawful not to eliminate health inequalities (although equally, if health inequalities persist and widen, that fact would need to inform consideration of the regard duty). Nor does the commissioner have the luxury of ‘pausing’ the health service while it investigates a health inequality or any other matter. The duties are to have regard, not to achieve perfection, and this is a practical rather than an academic exercise.
Reduce health inequalities
2.3.5 This duty has been discussed in section 2.2 above. It is listed here for completeness, as it is one of the regard duties under the NHS Act 2006.
Act with autonomy
2.3.6 NHS England has a statutory duty to have regard to the desirability of allowing others in the healthcare system to act with autonomy and avoid imposing unnecessary burdens on them, so far as this is consistent with the interests of the health service.
Example
NHS England is considering commissioning new primary care services in a particular area. When deciding what type of contract it wants to award (GMS, PMS or APMS), it should weigh in the balance the desirability of the extra autonomy a PMS agreement or APMS contract offers.
Promote education and training
2.3.7 Commissioners have a duty to have regard to the need to promote education and training of those working within (or intending to work within) the health service.
Impact in areas of Wales or Scotland
2.3.8 NHS England has a duty to have regard to the likely impact of commissioning decisions on healthcare delivered in areas of Wales or Scotland close to the border with England. This will clearly be relevant for those working in NHS England regional teams that border Wales or Scotland. NHS England will also need to comply with the duty when making national strategic decisions about the delivery of primary care that affect bordering areas as well as others.
Example
The commissioner is considering commissioning new primary care services for a town in England close to the border with Scotland. It is concerned that many of the local residents have difficulty in accessing local primary care services, the nearest practice being based over the border in Scotland.
That provider is difficult to access by public transport and in the winter the short route is often impassable.
To comply with its duty to have regard to the likely impact of commissioning decisions on healthcare delivered in areas of Scotland close to the border with England, the commissioner discusses the impact that commissioning services on the English side of the border would have on the Scottish provider.
It takes this impact into account when it makes its decision about the commissioning of services.
2.4 The promote duties
2.4.1 It is helpful to look next at the promote duties. These are:
- the duty to promote awareness of the NHS Constitution among patients, staff and members of the public (in respect of NHS England, see section 13C(1)(b) of the NHS Act 2006; and in respect of ICBs, see section 14P(1)(b) of the NHS Act 2006)
- the duty to promote the involvement of patients and carers in decisions about their own care (in respect of NHS England, see section 13H of the NHS Act 2006; and in respect of ICBs, see section 14U of the NHS Act 2006)
- the duty to promote innovation in the health service (in respect of NHS England, see section 13K of the NHS Act 2006; and in respect of ICBs, see section 14X of the NHS Act 2006)
- the duty to promote research and the use of research on matters relevant to the health service (in respect of NHS England, see section 13L of the NHS Act 2006; and in respect of ICBs, see section 14Y of the NHS Act 2006)
A decision that is positively contrary to achieving the relevant outcome might breach a promote duty unless there was some compelling reason to adopt it. In this situation, if the decision is being made by NHS England or by ICBs under delegated authority, the NHS England legal team should be contacted for further guidance.
Additionally, some decisions will be obvious opportunities where, for example, patient involvement could easily be promoted. In such cases the safest course of action is to ensure that this is done.
2.4.2 To meet the duty a commissioner does not have to do everything itself – be more innovative, improve its use of research data, etc. It can meet the duty by encouraging other people to do things.
Example
A commissioner decides to run a competition to reward GP practices that are innovative in their use of telehealth devices – smart medical devices that transmit data from a patient to their treating clinician without the need for the patient to attend surgery. The winners will be showcased so that other practices can follow their lead.
This helps to meet the duty to promote innovation in the health service. If a request were received by a commissioner for extra funding to support the implementation of a local telehealth initiative, for example, it would not be obliged to support it because of the duty to promote innovation.
That duty has already been met by the commissioner in a different way.
2.5 The view to duties
2.5.1 The view to duties are:
- the duty to act with a view to delivering services in a way that promotes the NHS Constitution (in respect of NHS England, see section 13C(1)(a) of the NHS Act 2006; and in respect of ICBs, see section 14P of the NHS Act 2006)
- the duty to act with a view to securing continuous improvement in the quality of services in health and public health services (in respect of NHS England, see section 13E of the NHS Act 2006; and in respect of ICBs, see section 14R of the NHS Act 2006)
- the duty to act with a view to enabling patients to make choices about their care (in respect of NHS England, see section 13I of the NHS Act 2006; and in respect of ICBs, see section 14R of the NHS Act 2006)
- the duty to act with a view to securing integration, including between health and other public services that impact on health,
- where this would improve health services (in respect of NHS England, see section 13N of the NHS Act 2006; and in respect of ICBs, see section 14Z1 of the NHS Act 2006)
2.5.2 The duty to exercise its functions with a view to securing that health services are provided in an integrated way where it considers that this would:
- improve the quality of those services (including the outcomes that are achieved from their provision)
- reduce inequalities between persons with respect to their ability to access those services
- reduce inequalities between persons with respect to the outcomes achieved for them by the provision of those services
(In respect of NHS England, see section 13N of the NHS Act 2006; and in respect of ICBs, see section 14Z1 of the NHS Act 2006.)
2.5.3 In many ways the considerations for these duties and the promote duties are the same. One difference is that while a promote duty can be met by encouraging others to achieve it (for example, encouraging GP practices to make better use of telehealth devices), with the view to duties the actions have to be carried out by the commissioner.
2.5.4 The view to duties are less onerous than the promote duties because they do not require the commissioner to achieve a particular outcome (although that would be desirable) – only to do something that aims to achieve it. This contrasts with the promote duties, which require an outcome to be achieved.
2.5.5 The view to duties are most likely to affect strategic decisions taken at directorate level within NHS England. Provided the commissioner can show that within the totality of its activities significant action has been taken with the intention of achieving the outcomes that the commissioner is required to have a view to, the duty is discharged.
2.5.6 As with the promote duties, decision-makers on the ground should be wary of doing something that actively goes against one of the goals set out in the view to duties. In this situation, if the decision is being made by NHS England or by an ICB under delegated authority, the NHS England legal team should be contacted for further guidance. Also, if there is a clear opportunity to help deliver one of the view to objectives, it is best to take it.
2.6 The involvement duty
2.6.1 Under sections 13Q of the NHS Act 2006, NHS England has a statutory duty to “make arrangements” to involve the public in the commissioning of services for NHS patients. (This duty is also placed directly on ICBs under section 14Z2.)
2.6.2 Section 13Q applies to:
- the planning of commissioning arrangements
- the development and consideration of any proposals that would impact on the manner in which services are delivered to individuals or the range of services available to them
- decisions that would impact on the manner in which services are delivered to individuals or the range of services available to them
2.6.3 The section 13Q duty only applies to plans, proposals and decisions about services that are directly commissioned by NHS England. This includes GP, dental, ophthalmic and pharmaceutical services. However, under delegated authority ICBs must act in a way that enables NHS England to comply with the 13Q requirements.
2.6.4 (The section 14Z2 duty applies in relation to any health services which are, or are to be, provided pursuant to arrangements made by an ICB in the exercise of the ICB’s own functions; that is, commissioning of secondary care.)
Commissioners’ arrangements for public involvement
2.6.5 The statutory duty to “make arrangements” under section 13Q of the NHS Act 2006 is essentially a requirement to make plans and preparations for public involvement.
2.6.6 NHS England has set out its plans as to how it intends to involve the public in the following publications:
- policy on working in partnership with people and communities
- Statement of Arrangements and Guidance on Patient and Public Participation in Commissioning
- framework for patient and public participation in primary care commissioning
2.6.7 These publications set out and explain the arrangements NHS England has in place:
- corporate infrastructure – how public involvement is embedded in the way that NHS England is constituted and carries out its business
- involvement initiatives – initiatives designed to involve the public in strategic planning and the development of policy or other aspects of NHS England’s activities
- monitoring arrangements – a step-by-step process to help commissioners identify whether section 13Q applies and decide whether sufficient public involvement activity is already in place or whether additional public involvement is required
- responsive arrangements – guidance to commissioners on how to make arrangements for public involvement where monitoring has indicated that such arrangements are required
2.6.8 As well as setting out the above arrangements, which commissioners should follow, the documentation is regularly reviewed and updated and contains useful resources for commissioners, including:
- details of existing corporate infrastructure and involvement initiatives that could be drawn on by commissioners to involve the public in their commissioning activities
- reference to NHS England’s framework for involving patients and the public in primary care commissioning, which includes resources developed especially for primary care
- resources to help commissioners identify whether section 13Q applies, put in place appropriate arrangements for public involvement and avoid legal challenges
- guidance on a variety of topics that often arise, such as what ‘public involvement’ means, how to involve the public, who to involve, when involvement should take place, urgent decisions and joint involvement exercises
- case studies based on primary care scenarios
- summaries of related legal duties
- details of how to seek further advice if needed
2.6.9 The documentation is intended to be used by both commissioners (that need to understand and comply with the arrangements when commissioning services) and the public (to understand how NHS England involves the public in its commissioning of services). As noted, for ICBs commissioning under delegated authority from NHS England, these arrangements are supplementary to their own requirement to have in place arrangements for public involvement under section 14Z2 of the NHS Act 2006.
2.7 Duty to act fairly and reasonably
2.7.1 Commissioners have a duty to act fairly and reasonably when making decisions. These duties come from case law that applies to all public bodies.
Acting fairly
2.7.2 Normally, to act fairly a commissioner will need to act in accordance with its own policies and relevant policies published by NHS England. For ICBs commissioning under delegated authority from NHS England, this will include NHS England policies concerned with the commissioning of primary care. A commissioner can depart from guidance if there is good reason to do so. In this scenario, the commissioner will need to explain the situation fully to the people and organisations affected and give them a chance to provide their views on the procedure to be followed. This will include why it wants to depart from the usual policy and what it will do instead.
2.7.3 Commissioners also need to be careful about keeping promises made to contractors or the public: for example, that there will be a public consultation before any final decision is made on closing a particular pharmacy. It is sometimes (but not always) possible to depart from such promises. Therefore, care should be taken about giving any clear commitments to a particular course of action until the commissioner is sure that it is what it wants to do. If a commissioner is considering departing from a commitment it has given to do a particular thing or follow a particular type of process, then, if the decision is being made by NHS England or by an ICB under delegated authority, the NHS England legal team should be contacted for further guidance.
2.7.4 It is also important to act proportionately, taking into account any adverse impact on patients and/or contractors.
Acting reasonably
2.7.5 The commissioner must take all relevant factors into account when making its decisions and exclude irrelevant factors. It is up to the commissioner how much weight it gives to competing considerations and it may give a factor no weight at all. The key point is that all the relevant factors are identified and documented.
Example
The commissioner has to decide whether to approve a practice’s application to stop opening on Wednesday evening and open on Saturday morning instead. The practice is based in an area with a high Jewish population.
Relevant factors in this decision include whether services will become more or less accessible as a result of the change, any adverse impact on people with protected characteristics (is the Jewish population disadvantaged as Saturday falls on the Jewish rest day?) and any costs implications for the commissioner.
An example of an irrelevant factor is that the commissioner has been promised some good publicity by the practice if it agrees to the change.
2.7.6 The reasons for the commissioner’s decisions also need to ‘stack up’. It is important for the commissioner to document its reasons for a decision as the commissioner needs not only to act reasonably but be able to show that it has acted reasonably by reference to contemporaneous documents. This means that, particularly where a controversial decision is being made, the thinking behind the decision needs to be carefully documented.
2.8 The duty to obtain advice
2.8.1 A commissioner has a duty to “obtain appropriate advice” from persons with a broad range of professional expertise (in respect of NHS England, see section 13J of the NHS Act 2006; and in respect ICBs, see section 14W of the NHS Act 2006).
2.8.2 This means that decision-makers need to collect appropriate information before making decisions. If the commissioner does not have the information it needs, then it should seek appropriate advice. In many cases, it will not be necessary to do this as all the necessary information is to hand.
2.8.3 The duty is most relevant to strategic decisions, where decision-makers will need to document how they obtain advice from those with professional expertise (some of whom may be employees or secondees).
2.9 The duty to exercise functions effectively
2.9.1 The commissioner has a duty to exercise its functions effectively, efficiently and economically (in respect of NHS England, see section 13D of the NHS Act 2006; and in respect of ICBs, see section 14Q of the NHS Act 2006).
2.9.2 This is a statutory reformulation of a duty that has been contained for many years in HMT’s managing public money and its predecessors. If the commissioner has complied with the other duties in this guidance – in particular, the duty to act reasonably – it is highly unlikely that it will breach this duty.
2.10 The duty not to prefer one type of provider
2.10.1 NHS England must not try and vary the proportion of services delivered by providers according to whether the provider is in the public or private sector, or some other aspect of their status (section 13P). ICBs must also act in accordance with this duty when they are commissioning under delegated authority from NHS England.
2.10.2 This means that the commissioner must focus on the services delivered by an organisation and its sustainability. It should not make choices about contractors based solely on their status: for example, company, partnership, public sector, private sector, charity or not for profit organisation.
3. Working together – commissioning and regulating
3.1 Introduction
3.1.1 This chapter is intended to inform commissioners of work to establish a robust and practical joint working framework.
3.1.2 The Care Quality Commission (CQC), NHS England and NHS clinical commissioners with the support of the General Medical Council(GMC), published a joint working framework in 2018, intended to help provide structure and support for relationships between commissioners and the CQC, with examples of good practice.
3.2 Existing good practice and principles
3.2.1 Steps to streamline processes and share information include:
- NHS England regularly shares General Practice Annual Electronic Self-Declaration (eDec) data and information with the CQC
- NHS England shares eDec data with all commissioners, including analysis and outlier reports to help commissioners target contract review activity and support locally
- CQC shares inspection schedules and rating updates with commissioners wherever possible
- commissioners share local information and intelligence with CQC and NHS England
- in some areas commissioners work closely with GP practices prior to inspections to support them
3.2.2 Collaborative working arrangements:
- Positive working relationships are critical for ensuring successful partnership working. Commissioners and the CQC have established some formal mechanisms for ensuring successful collaborative working, but these should not be seen as the only means by which those relationships can be developed. We also recognise the role of quality surveillance groups and other forums that have been established for information sharing in some areas of the country.
- It is recognised that contacting the right person at the right organisation at the right time is the best means of developing those relationships and avoiding duplication wherever possible. It is important that commissioners engage with and know their local contacts.
3.2.3 Existing good practice:
- All parties will be transparent. We will ensure information governance and data protection principles are adhered to without exception and ensure that GP practices are fully sighted on this.
- Commissioners should actively and effectively communicate with each other and the CQC to ensure GP practices are not overburdened: for example, to avoid the situation whereby a commissioner contract visit overlaps with a CQC inspection.
- Commissioners should keep in regular contact with the CQC throughout the year and have more targeted and regular communication in the run-up to inspection or annual review.
- Commissioners should actively engage with and support GP practices pre- and post-inspection.
4. Commissioning and transformation support (CATS)
4.1 Introduction
4.1.1 NHS England is supporting commissioners to improve general practice through effectively discharging their responsibilities for commissioning and transformation of general practice services.
4.1.2 This includes the development and co-production of resources to help develop the capability of commissioners to improve general practice – reducing unwarranted variation and promoting improvement in quality, safety and patient and staff experience in general practice.
4.1.3 NHS England expects commissioners to recognise the importance of general practice improvement and transformation within their delegated commissioning responsibilities, as a key mechanism for addressing overall system challenges, development and improvement. ICBs should therefore make resources available to enable improvement and transformation of general practice services.
4.2 NHS England aims to support commissioners by:
4.2.1 Supporting commissioners to understand variation between practices and general practice support needs, using relevant national tools such as:
4.2.1.1 The practice and PCN support level frameworks (SLFs) – these frameworks support practices or PCNs to understand their strengths and support needs for improvement. They can be accessed on Support Level Framework Online. The platform can be accessed only by primary care colleagues.
4.2.1.2 A national General Practice Dashboard – a management information tool providing commissioners with a simple at-a-glance oversight of GP practice variation across key national priority metrics. The dashboard helps commissioners, when used alongside local data and intelligence, to benchmark or inform where they may need to target local contract reviews and provide support for improvement. It will also help NHS England to understand GP practice variation. Note the dashboard is only available to approved commissioner users.
4.2.2 Supporting commissioners in identifying and implementing the most appropriate support for general practices depending on their needs:
4.2.2.1 The ‘intervention support approach’ sets out a systematic approach for commissioners to segment practices according to whether they need support to stabilise, improve or sustain services. In line with the overall assurance framework for contract reviews, commissioners will need to take a risk-based approach to identifying and working with practices with unwarranted high variation and/or other issues that may be leading to poor service provision to patients. However, commissioners should also be looking to provide support to other practices to make continuous improvement over time and to sustain and share existing good practice, to support high quality and improvement across the commissioning area. The CATS intervention support approach can be found in annex 1.
4.2.2.2 Enabling commissioners to access the General Practice Improvement Programme’s practice level support (GPIP PLS) for their practices in 2025/26. GPIP PLS provides direct hands-on support to help practices implement modern general practice, supporting change in 3 improvement areas:
- improving patient experience of access (online, face to face and via phone)
- supporting practices to improve care navigation and clinical triage workflow to safely and effectively assess patient needs (supported by online consultation tools)
- better aligning existing capacity with demand including optimising use of a multidisciplinary team across the practice and PCN
4.2.3 Understanding and developing ICB capacity and capability for general practice commissioning and improvement:
4.2.3.1 A ‘CATS tool’ has been co-developed to enable commissioners to assess and understand (ideally through a facilitated conversation) their strengths in respect of leading general practice transformation, commissioning, managing compliance and performance, and to identify areas of development and support/change needed for improvement. The CATS tool and its supporting resources can be accessed on the FutureNHS collaboration platform (login required). More information is available by emailing engagepcti@nhs.net
4.2.3.2 Supporting commissioners to successfully embed locally led sustainable modern general practice transformation expertise, which includes enabling and supporting primary care transformation peer ambassadors (alongside wider local leadership). More information is available on the FutureNHS collaboration platform and by emailing engagepcti@nhs.net
4.2.3.3 Undertaking a baseline survey of ICB current capacity and capability to support general practice improvement and identify what would be needed to accelerate improvement. The results of the survey are being used in 2025/26 to inform national commissioning development offers and ICB approaches.
Part B: General contract management
1. Contracts described
1.1 Comparison of contract types
1.1.1 Throughout this document there are many references to standard contracts for general medical services (GMS), personal medical services (PMS) and alternative provider medical services (APMS). In addition to the statutory provisions regarding eligibility in sections 1.2, 1.3 and 1.4 below, the following table provides a quick comparator between the 3 contract types:
|
|
GMS contract |
PMS agreement |
APMS contract |
Can the commissioner award new contracts? | Yes All contracts are available to commissioners subject to compliance with the Provider Selection Regime and the requirements of the delegation agreement (see 1.5) |
Yes All contracts are available to commissioners subject to compliance with the Provider Selection Regime and the requirements of the delegation agreement (see 1.5) |
Yes All contracts are available to commissioners subject to compliance with the Provider Selection Regime and the requirements of the delegation agreement (see 1.5) |
|
Is the contract time limited? |
No Except in certain circumstances when a temporary GMS contract (see 1.1.2) can be used – see urgent contracts below |
Yes Note that a PMS contractor providing essential services may apply for a GMS contract any time prior to the end of the PMS agreement |
Yes |
|
Can the commissioner terminate at will? |
No |
Yes |
If agreed by the parties and relevant clause contained within the contract |
|
Must the contractor provide essential services? |
Yes |
No |
No |
|
Is there a standard form contract? |
Yes |
Yes |
Yes |
|
Does the standard form contract contain key performance indicators (KPIs)? |
No |
No |
No |
|
Can KPIs be added? |
KPIs can be agreed between the parties in relation to supplementary quality-based services |
Yes |
Yes |
|
Payment arrangements |
GMS SFE |
As agreed by the parties and contained within the agreement – there may be reference to the GMS SFE |
As agreed by the parties and contained within the contract |
1.1.2 Following the termination of a GMS contract, commissioners have the authority, as per Regulation 16(2) of the GMS Regulations, to enter into a temporary GMS contract with a contractor. This contract allows the provision of primary medical services to the former patients of the terminated contractor for a maximum period of 12 months. Commissioners should refer to section 1.6: Urgent contracts.
1.2 Statutory provisions: persons eligible to enter into GMS contracts
1.2.1 By virtue of the delegation agreement, all references in legislation should be assumed to apply also to ‘the commissioner’.
1.2.2 Section 86 of the NHS Act sets out the types of persons (including organisation types) that may enter into a GMS contract.
- In section 86: “health care professional”, “NHS employee”, “section 92 employee”, “section 107 employee”, “section 50 employee”, “section 64 employee”, “section 17C employee” and “Article 15B employee” have the meaning given by section 93.
1.2.3 GMS Regulations, part 2, Regulations 4 to 6 set out the eligibility criteria that must be satisfied before any of the types of persons set out in section 86 of the NHS Act can enter into the GMS contract.
1.3 Statutory provisions: persons eligible to enter into a PMS agreement
1.31 By virtue of the delegation agreement, all references in legislation should be assumed to apply also to ‘the commissioner’.
1.3.2 Section 93 of the NHS Act sets out the types of persons (including organisation types) that may enter into a PMS agreement (referred to in the Act as 3ection 92 agreements).
- In section 93: “health care professional”, “NHS employee”, “section 92 employee”, “section 107 employee”, “section 50 employee”, “section 64 employee”, “section 17C employee” and “Article 15B employee” have the meaning given in this section.
13.3 PMS Regulations, part 2, Regulations 4 and 5 set out the eligibility criteria that must be satisfied before any of the types of persons set out in section 93 of the NHS Act can enter into the PMS agreement.
Note: where 2 or more persons operate their practice as a partnership, the PMS agreement is not treated as being made with that partnership rather the persons agree to contract together as “the contractor”.
1.4 Statutory provisions: persons eligible to enter into an APMS contract
1.4.1 By virtue of the delegation agreement, all references in legislation should be assumed to apply also to “the commissioner”.
1.4.2 The NHS Act does not list persons who may (or may not) enter into an APMS contract.
1.4.3 The APMS Directions 4 and 5 contain provisions relating to circumstances in which certain types of persons or organisation may not enter into an APMS contract. Provided Direction 5 does not apply, any person or organisation may enter into an APMS contract.
1.5 Provider Selection Regime
1.5.1 The NHS Provider Selection Regime (PSR) is set out in the Health Care Services (Provider Selection Regime) Regulations 2023 (the PSR Regulations).
1.5.2 The PSR seeks to ensure that decisions about who provides healthcare services are:
- made in the best interest of patients, taxpayers and the population
- robust and defensible, with conflicts of interests appropriately managed
- made transparently
- compliant with the rules of the regime as set out in NHS England guidance
1.5.3 NHS England has published PSR statutory guidance to support implementation of the PSR Regulations, setting out what relevant authorities as defined by the PSR Regulations (that is, commissioners) must do to comply with them. This includes supplementary guidance for arranging primary care services.
1.5.4 As a general rule:
- new primary medical care services:
- that involve a relevant authority selecting a provider
- where the number of providers available to patients is restricted by the relevant authority
- must be arranged by applying the most suitable provider process or the competitive process
- continuation of existing primary medical services:
- where the contract of the current provider is coming to an end
- the number of providers available to patients is limited by the relevant authority
- the relevant authority wishes to continue with the existing provider and decides that the existing provider is satisfying the existing contract and will likely satisfy the proposed contract to a sufficient standard (taking into account the key criteria and applying the basic selection criteria)
- the proposed contract is not changing considerably
- may be awarded under direct award process C
- urgent contracts and modifications to existing contracts:
- may be made in line with the statutory guidance
1.5.5 Commissioners are reminded the delegation agreement includes a requirement that they seek the relevant NHS England regional director’s sign off of all contracts whose term can exceed 5 years. Commissioners should have systematic processes for confirming plans for such contracts, both before proceeding with any selection process and on confirmation of contract award. These processes will need to align with the relevant NHS England region’s process for sign-off, including the provision of such information as may be requested to support sign-off decisions.
1.5.6 Commissioners are also reminded the delegation agreement includes a requirement that they seek the relevant NHS England regional director’s sign-off for any matter in relation to the delegated functions which is novel, contentious or repercussive. In the context of PSR and primary medical care contracting, this would include any novel, contentious or repercussive use of the contract modification process.
1.5.7 By way of this PGM, NHS England introduces an additional requirement with immediate effect: proposed contract modifications that would lead to a cumulative change in the lifetime value of the contract since it was entered into of £500,000 or 25% or more* now need NHS England regional director sign-off. That is, contract modifications at or above these thresholds made under Regulation 13 of the Provider Selection Regime Regulations that would require a commissioner to publish a transparency notice.
* There is no national guidance on these calculations and reasonable local judgement should be used.
1.5.8 Routine variation for enhanced services that are available to all GP practices e.g. annually, are excluded from this new NHS England regional sign off requirement.
1.5.9 The intention of the sign off requirement is to safety net against potentially novel, contentious or repercussive contract modifications, for example, a proposal to modify an existing contract to take over the services of an expiring time-limited contract. This is an additional safeguard in support of (but not replacing) the requirement for any matter in relation to the delegated functions which is novel, contentious or repercussive (in this case commissioning plans) to be approved by relevant commissioners and NHS England.
1.5.10 The processes referred to at 1.5.5 should be amended by commissioners and NHS England regions to support this additional requirement.
1.5.11 General queries about the PSR can be sent to psr.development@nhs.net.
1.6 Urgent contracts
1.6.1 Circumstances may arise that require the commissioner to put in place an urgent contract. Such circumstances may include:
- the death of a contractor
- the bankruptcy or insolvency of a contractor
- termination of an existing contract due to patient safety grounds
1.6.2 Where continuity of services to patients is required, the short timescales involved may not allow the commissioner to undertake a managed closedown and transfer to a new provider (details of which are set out in the chapter on planned). Additional information can also be found in part C, chapter 2: Unplanned/unscheduled and unavoidable practice closedown. The commissioner may therefore look to award a contract to a specific party that is able to provide the services to patients at short notice.
1.6.3 Prior to awarding a contract in this scenario, the commissioner should consider a number of factors that are set out in the paragraphs below.
Provider Selection Regime
1.6.4 Commissioners should defer to the published PSR statutory guidance. The urgent provisions within the regime may apply to secure immediate needs: for example, to establish caretaker arrangements. However, as this will be a temporary arrangement it must be reconsidered after a set period. The statutory guidance provides further information about proper application.
Premises
1.6.5 The previous contractor may own or lease the premises which, as a result, may not be available for the provision of the services under a new contract. The availability of the premises must be ascertained before entering into a temporary contract.
Primary care networks
1.6.6 The commissioner should facilitate a discussion between the incoming contractor and the PCN to which the outgoing contractor was a member, involving the relevant local medical committee (LMC), with the expectation that PCN membership should be maintained to ensure that patients continue to receive uninterrupted network services.
1.6.7 If the contractor is still not willing to join the PCN, then the commissioner will work with the existing PCN core network practices (GP practices that signed up to and are responsible for delivering the requirements of the network) to ensure continuity of services to its registered patients.
1.6.8 If the PCN is not prepared to accept the contractor as a member, the commissioner may require a PCN to include the practice as a core network practice of that PCN. Where the commissioner is minded to require a PCN to do so, the commissioner must engage with the relevant LMC and, when making its determination, have regards to the views of the LMC. Section 4.6 of the Network Contract DES specification sets out the process for allocating a practice to a PCN.
Public involvement
1.6.9 One of the general duties of commissioners is to ensure there is public involvement where a decision leads to an impact on the provision of primary care services. If under a new contract services are provided from a different location, this will be an impact on the services which may trigger the need to undertake a public involvement exercise.
1.6.10 Where there is no time for undertaking an exercise prior to entering into the contract, the commissioner should ensure that as soon as possible after the contract is entered into, it arranges for such an exercise to be undertaken prior to the commissioner making any decisions about the long-term provision of services.
Commissioner standing orders (SOs) and standing financial instructions (SFIs)
1.6.11 The commissioner may have organisational standing orders and standing financial instructions that require contracts to be procured in certain ways: for example, securing 3 quotes for contracts up to a certain financial value. Where time does not allow the rules to be followed, there may be an emergency process that must be followed.
Other factors
1.6.12 Further factors may be relevant depending on the circumstances of the matter. Please refer chapter 10: Practice closedown (planned/scheduled) and part C, chapter 2: Unplanned/unscheduled and unavoidable practice closedown for a list of all factors that may be relevant.
1.6.13 Commissioners should also consider that if a practice has closed because of concerns in relation to patient safety, the incoming provider may need to be commissioned to undertake a review of systems and processes. This should include, but is not limited to, undertaking audits to provide assurance around patient safety. This recognises the additional work that commissioners may need to reflect in the contract to provide assurance with regard to patient safety and public confidence.
Which contract form?
1.6.14 A GMS contract can be used where the commissioner has terminated a contract of another provider of primary medical services, and as a result of that termination, it wishes to enter into a temporary contract for a period specified in the contract for the provision of services.
1.6.15 A time limited PMS agreement may not be attractive in this scenario as the PMS contractor, if providing essential services, can request a non-time limited GMS contract at any time (if eligible to hold such a contract).
1.6.16 It is common for APMS contracts to be used in such a scenario due to the flexibility of:
- types of organisations that can enter into APMS contracts
- flexibility of types of services and payment mechanism that can be agreed
- flexibility around duration and termination provisions
1.6.17 The commissioner should therefore consider what services and duration are required and whether there are any restrictions on the proposed contractor entering into different contract types to meet local diverse health needs.
Primary Care Support England (PCSE) services notifications
1.6.18 Commissioners should ensure that following any contract award or contract merger, GP performers are informed of their obligation to notify within 28 days Primary Care Support England (PCSE) using the online portal.
1.6.19 Additionally, and more generally, GP performers and indeed performers in all contractor groups are required to notify PCSE of any changes relevant to their entry on the national performers list. Further information is available on the NHS England website.
2. Assurance framework for contract reviews
2.1 Introduction
2.1.1 Commissioners of primary medical services are responsible for the quality, safety and performance of services delivered by providers within their area of responsibility and for addressing inequalities. ICBs must have due regard to their obligations as set out within the delegation agreement which include adherence with policies and guidance issued by NHS England, including this PGM.
2.1.2 This chapter outlines the approach to be taken by commissioners when overseeing primary medical services contracts to ensure compliance with quality, safety and performance standards, providing a framework for assessing general practice services delivered through the normal contractual routes (that is, GMS, PMS and APMS).
2.1.3 This chapter should be read alongside and is supplemented by part A, chapter 4: Commissioning and transformation support (CATS) which describes support and resources available to ICBs to improve general practice through their delegated responsibilities for commissioning and transformation. It is anticipated the CATS approach will be formally integrated into this assurance framework for contract reviews in future updates.
2.1.4 It is important to note that while exercising of the function has passed to ICBs, NHS England remains accountable. Oversight and assurance of ICBs delegated commissioning of primary medical services is covered outside this PGM.
2.1.5 Commissioners are reminded that early engagement with LMCs presents the best opportunity to support practices in making effective and sustainable changes to support service improvement should this be found to be appropriate and necessary.
2.1.6 This chapter does not give the details of the various types of contracts or the contractual actions available as these are covered elsewhere within this PGM. It provides practical advice and guidance to support commissioners and contract managers.
2.2 Background
2.2.1 While it is recognised that most healthcare professionals and providers of primary medical services operate to a very high standard, it is essential that commissioners have robust monitoring arrangements in place for the quality, safety and performance of services.
2.2.2 Monitoring arrangements should create a balance of support, oversight and intervention where necessary. Furthermore, they should create a culture of openness and transparency and a vehicle to promote peer to peer improvement.
2.2.3 While practices as providers are accountable for the quality, performance and safety of services and are required to have their own monitoring processes in place, commissioners have a responsibility for assurance. Through the Duty of Candour and the contractual relationship with commissioners, practices are required to provide information and assurance to commissioners and engage in system-wide approaches to improving quality, safety and performance.
2.3 Contract review
2.3.1 Through the publication of this policy framework, NHS England requires commissioners to undertake a risk-based approach to reviewing contracts, along with a rolling programme of deep-dive contract reviews. Depending on the number of practices within the commissioning area, the types of contracts held and the resources available to effectively manage these, a rolling programme could span 1 to 3 years.
2.3.2 For APMS contracts this would need to be more frequent owing to their length and the variable key performance indicators within them. It is recommended that if new information becomes available to the commissioner which suggests high levels of variation, a visit may be required and the contract reviewed.
2.3.3 Commissioners also have a statutory duty to conduct a routine annual review of every primary medical services contract it holds. This is covered through the General Practice Annual Electronic Self-Declaration (eDec) collection which NHS England has established with providers (and is currently delivered by NHS England). Commissioners should ensure they review practice eDec returns following submission to inform and support contract review and management responsibilities.
2.3.4 Commissioners should maintain accurate records of all contract reviews and will be required to demonstrate this to NHS England when requested, including evidence of compliance, or otherwise support oversight of primary care commissioning arrangements – for example, via NHS England’s assurance arrangements or internal and external audit functions.
2.4 Setting and monitoring key performance indicators
2.4.1 Commissioners should ensure key performance indicators (KPIs) are negotiated into relevant contracts. These should be specific, measurable, achievable, relevant and time-bound (SMART) and include relevant payment thresholds.
2.4.2 Primary medical services providers will then be required to submit evidence to the commissioner in relation to those KPIs, against which payment will be considered. The commissioner should be assured that the evidence submitted by the contractor is robust, relevant and proportionate.
2.5 Using data and information effectively
2.5.1 In a model for improvement, it is recognised that commissioners are using various data sets to oversee the delivery of services but that these provide only part of a large picture. Data used in isolation presents not only a risk of inaccuracy, but anxiety among those providing services or those responsible for oversight of the delivery of those services. Data must be put into the context of the individual provider practice and used alongside other intelligence to gain a full understanding of any potential risk to quality and patient safety.
2.5.2 The use of measures and indicators to assess quality, safety and performance should not remove, diminish or unduly influence sound evidence-based clinical decisions and judgements. Commissioners should take steps to ensure that indicators are not abused as perverse incentives to change clinical practice or ways of working which are inconsistent with the delivery of high-quality patient centred care.
2.5.3 It is essential that commissioners have in place a robust assurance management programme to identify and share best practice, recognise where additional management may be needed and highlight when things are going wrong at an early stage in primary medical services provision.
2.5.4 Through transparent measurement across practices within the commissioning area, the practice–commissioner relationship provides a forum for collaborative and engaging discussions. Such engagement and collaboration recognise the contribution that each practice can make to both the quality of services to their registered patients and the wider impact on service delivery across the practice and the wider local population.
2.5.5 The use of measures and indicators is to act as a starting place for conversations, asking questions along the way as to why variation may be occurring and acknowledging that variation may be warranted or unwarranted depending on the context and wider supporting information available. A practice visit may be needed to support further understanding when high levels of variation are occurring. This may be supported through targeted and structured conversations using appropriate tools to better understand practice support needs and improvement priorities.
2.5.6 If there are greater concerns about a practice, bordering on contractual failure, this will require a more formal conversation with the practice which should be led by the commissioner. The focus will be the same for all practices: to agree support and actions to stabilise, recover, improve and then sustain improvements. In exceptional cases, actions may include possible contractor reconfiguration (for example, managed mergers or partnership changes) to strengthen the provider or, as a last resort, a managed provider exit.
2.5.7 Recognising that practice-specific data alone is not conclusive evidence of poor service provision and needs to be considered in the context of the practice, the commissioner will use a range of information to identify, prioritise, assess and mitigate any potential risks to service provision within a practice including:
2.5.7.1 NHS England data. NHS England provides commissioners with a range of, often pre-analysed, data which supports (and is expected to be used in) commissioners’ assessment of variation in the provision of primary medical services and consistent contract monitoring. 2 sources of data and intelligence are provided specifically to support commissioners’ contract review programmes:
- General Practice Annual Electronic Self-Declaration (eDEC). This includes practice-declared information such as practice details, operating policies, services and assurance of good workforce planning, contractual requirements and CQC regulatory responsibilities. It may also contain responses to ‘reasonable requests for information’: for example, from other governmental departments. The declaration content is updated annually to ensure it aligns with national changes: for example, GP contracts.
- GP practices are required to complete this mandatory declaration each autumn, with subsequent data available to commissioners immediately following eDEC closure (usually around the end of the calendar year). NHS England produces a subsequent national analysis to support commissioners in identifying and prioritising areas of declared non-compliance (for example, NHS England’s eDec outlier report which is usually available 6–8 weeks following eDec closure), supporting their contract review and management responsibilities.
- The eDEC information is also shared with the CQC, reducing the burden of separate information returns across organisations: for example, as part of pre-inspection information requests.
- General Practice Dashboard. As set out in part A, chapter 4: this new dashboard, launched in April 2025, supports commissioner understanding of variation between practices. The dashboard provides a simple at-a-glance oversight of GP practice variation across key national priority metrics (organised across domains of access, workforce, clinical quality and outcomes, medicines management, vaccinations and screening). When used alongside local data and intelligence, the dashboard can help commissioners benchmark or understand where they may need to target contract reviews and provide support for improvement. The dashboard can be accessed via the Federated Data Platform but as a management information tool is only available to authorised commissioner users.
2.5.7.2 Note: this policy framework previously set out a requirement that commissioners must use NHS England’s centrally defined GP indicator data set, available on the Primary Care Indicators website. This data set has been decommissioned but will remain available to view, with data/refresh as of January 2025, to all current users until 30 September 2025.
2.5.7.3 Practice demographic data will also be critical to understand the characteristics of each practice: for example, the demography of the population served. While such information is unlikely to change significantly over time, it may contain specific information which when presented alongside performance and outcomes data, can provide a more complete picture and better understanding of the potential impact on achievement of certain standards: for example, the effect of student practices or those that serve more discreet populations (homeless, high ethnic minority, highly deprived, etc). DHSC publishes national general practice profiles that are designed to support providers and commissioners in ensuring that they are providing and commissioning effective and appropriate healthcare services for their local population.
2.5.7.4 Care Quality Commission (CQC) data. The CQC is the independent regulator of health and adult social care in England. It seeks to ensure services are safe, effective, compassionate and delivered to a high quality, encouraging services to improve.
The inspection of general practice includes 5 key questions of services: whether services are safe, effective, caring, responsive to people’s needs and well-led. Assessment under each key question is against a set of quality statements that describe the characteristics of ‘high-quality, person-centred’ primary medical services.
CQC rates each of the 5 questions to give an overall rating for a practice: outstanding, good, requires improvement and inadequate. These ratings and practice reports are available on the CQC website and will be a key component of commissioner’s assurance management programme, supporting the prioritisation of contract reviews.
2.5.8 Commissioners should use data, along with any new or emerging sources of intelligence, to identify areas of concern and risk. The above sources of data and information will direct commissioners to those potential areas or pockets where risk is highest.
2.5.9 It is acknowledged that these sources of data do not capture the full range of services provided by general practice. However, they are an important starting point in supporting commissioners (and in turn providers and other stakeholders) to build a more holistic view of performance with a focus on objective service improvement and outcomes.
2.5.10 There are very few circumstances where data alone should determine commissioner intervention. To ensure flexibility and to account for warranted practice nuance, commissioners should review these sources of data and any future published sources of data and information to understand whether a practice requires support to improve or intervention: for example, if the commissioner considers there may be a risk to quality and patient safety. If necessary, the commissioner should provide additional appropriate and adequate support as agreed with the practice. If despite that support a practice is unable to demonstrate improvement within a reasonable period, the commissioner must determine whether it considers there is an actual cause for concern. This will require scrutiny of any other relevant sources of intelligence or data such as those listed below:
- wider general practice data dashboards
- medicines optimisation dashboard
- GP workload tool
- Friends and Family Test
- General Practice Patient Survey
- NHS RightCare future indicator sets for general practice
- GPIT Digital Maturity Index
- patient complaints (K041b) indicator set
- performer performance/concerns (if appropriate)
- ICB engagement and relationship
- LMC intelligence
- local intelligence from wider stakeholders: for example, Healthwatch
- data provided by the practice
2.5.11 Where a potential or actual risk to quality, safety or performance is identified, and therefore adherence to the contract, the commissioner will be expected to take the necessary steps to assure itself that adequate and effective support is being provided to reduce the risk, identify any ongoing areas for improvement and be able to demonstrate and measure that improvement.
2.5.12 The commissioner retains contractual accountability. Through the commissioner relationship with the practice/LMC and its use of supporting data, in conjunction with robust, fair and consistent application of guidance for the management of service and performance improvement, will help to ensure risks to quality, safety and performance are addressed in a timely and proportionate manner.
2.5.13 Data alone is not however a panacea. The commissioner must consider the practice in the context of wider determining factors: for example, social deprivation, health needs, population profile, resourcing, to name but a few.
2.5.14 Underlying this approach is the recognition that the best way of ensuring continued excellence lies in the consistent and proportionate application of an assurance framework, which requires commissioners to consider multiple sources of reliable and accurate information and intelligence against relevant and specific criteria.
2.6 Practice visit – best practice
2.6.1 The commissioner remains accountable for contract management, a co-ordinated practice/commissioner/CQC/LMC relationship provides an opportunity for an engaging and collaborative discussion that covers each practice’s quality and achievement across a range of agreed standards, be that in respect of the service provided by a practice or a practices use of for example, secondary care services.
2.6.2 By way of an example and to provide clarity, a commissioner may have a conversation with a member practice which from an initial view appears to have a disproportionate number of emergency admissions for conditions usually managed in primary care. In itself, this may not necessarily indicate a problem but allows the commissioner to understand the implications in the wider commissioning arrangements.
2.6.3 The commissioner will not necessarily focus solely on the contractual requirements and may include quality improvement and health outcomes to ensure it is meeting its duties to improve quality and secure good public health in the population.
Understand the background
2.6.4 To align with the commitment to reduce burden and bureaucracy, commissioners should consider whether the visit can be managed remotely or whether other practice visits may be planned or recently undertaken to avoid unnecessary duplication. Such visits may be planned by the CQC or NHS England in relation to regulation or educational standards.
2.6.5 Visits to practices may originate from many areas and may be formal or informal. The reasons for visiting a practice may be for:
- list closure application
- CQC report
- new contractor visits
- practice support
- investigation of concerns raised (see annex 2: a sample practice visit letter)
- annual review of provider
- contractual concerns: for example, boundary changes
- practice mergers
- performer concerns that may be impacting on contract
Note: in addition, commissioners should still undertake a rolling programme of review as outlined at the start of this chapter, but this should include a random sample of practices not identified through other intelligence-led approaches.
Gathering information
2.6.6 Before visiting the practice, the commissioner should collate all relevant and available data and For example:
- CQC report if available or discussion with CQC data and/or inspection team
- NHS England’s new General Practice Dashboard
- General Practice Annual Electronic Self-Declaration (eDEC) return
- wider general practice data dashboards
- medicines optimisation dashboard
- DHSC GP practice profiles
- K041b complaints
- any local profiling tools or dashboards
- legal advice if required
- ‘soft’ intelligence – ask the practice to complete a template which may save time during your visit
Communications
2.6.7 Early communication is key to a successful visit. Always contact the practice to advise them that you will be visiting the practice and the reason why. The agreed date must be confirmed in writing. Give plenty of notice unless there is a patient concern (see annex 2: a sample practice visit letter). Ensure and confirm adherence to infection control procedures which may be in place.
Informal visits
2.6.8 If an informal visit is planned, the practice has usually instigated it themselves and therefore is aware of the reason; that is, a practice merger. Ensure you have the right information available for the matter to be discussed. For example, if the visit is to discuss a list closure, ensure you know the practice list size, list variations, surrounding practice closures, etc.
Formal visits
2.6.9 Concerns about a practice can be raised to commissioners through various routes. Depending on the issues raised, the commissioners will need to make an informed decision on the extent to which they need to investigate.
2.6.10 Commissioners should:
- establish a task and finish group
- establish terms of reference for task and finish group (see annex 3: a sample terms of reference (ToR) for a task and finish group investigating concerns)
- task and finish group agree the actions required:
- practice visit
- breach/remedial notices issued where appropriate
- contract termination
- referral to quality surveillance group/performance advisory group
- agree clear and specific ToR for any visit, including a commitment to review/amend the ToR in light of any new/emerging evidence. Amendments should be agreed between parties
- investigation team identified – to include, for instance, GP, primary care nurse lead, safeguarding lead, nursing and quality lead, contract manager. Admin support where appropriate
- initiate formal contact with practice
- communication with practice, with recommendation of inclusion of LMC
- practice visit with appropriate team
- report/action plan drafted (see annex 4: a sample overview of concerns – investigation plan
- report/action plan submitted to task and finish group
- report/action plan finalised
- report/action plan sent to practice for comment
- meeting with practice to discuss taking action plan forward
- monitoring meetings to ensure targets/deadlines are met
- final meeting with practice to close process
- final task and finish group to give assurance issue/concern is resolved
2.6.11 If issues are not resolved, then contract breach/termination notices may be served.
Consultation with and support from the local medical committee
2.6.12 If the commissioner is undertaking a targeted visit relating to concerns raised or known contractual underperformance, which may result in actions being imposed or considered, then it shall, whenever it is reasonably practical to do so, consult the local medical committee (LMC).
2.6.13 The LMC has a role in supporting practices facing remedial, breach and termination notices or those undergoing performance investigations. The LMC can advise practices on how to complete actions required by remedial notices, how to address issues to avoid further contract breaches and appeal against termination notices if appropriate. The LMC can signpost practices to experts who can help: for example, the practice’s medical defence organisation or consultants who can advise on practical issues such as practice policies. For those practices undergoing performance investigations, the LMC can support practices in preparatory meetings with the investigating officers and the commissioners, assist with drafting terms of reference, guide practices through the investigation process and sit in on interviews with clinicians and staff to ensure that due process is followed.
2.6.14 Commissioners are encouraged to advise practices in these circumstances to make contact with their LMC as early as possible to ensure they have access to expert help and advice.
3. Managing patient lists
3.1 Introduction
3.1.1 Practices operate either an open or a closed patient list. Patients have the ability to register with any local practice which operates an open list. Practices continue to have discretion over new patient registrations, although fair and reasonable grounds should be presented in the event of a refusal to accept a patient onto an open practice list.
3.1.2 Practices must ensure that they meet all general legal duties and must ensure that they are not directly or indirectly in breach of the public sector equality duty.
3.1.3 The commissioner has an obligation to prepare and keep up to date a list of patients accepted by the contractor or assigned to its list of patients and who have not been removed from that list. Primary Care Support England (PCSE) processes new patient registrations and de-registrations and ensures that the national patient records database [Patient Demographics Service (PDS)] reflects what is shown in each practice’s patient list on behalf of commissioners. The Primary Care Registration Management (PCRM) is the national service which manages the formal process to change the patient’s registered GP practice recorded in PDS.
3.1.4 Primary Care Support England (PCSE) services generally (delivered on behalf of NHS England by Capita). In September 2015, PCSE took on responsibility for the delivery of NHS England’s primary care support services. PCSE provides support services to GP practices, pharmacies, dentists and opticians. For general practices they provide services covering:
- GP payments and pensions – administrating monthly contracts and reimbursements to GP practices
- patient registrations and list maintenance – processing new patient registrations and de-registrations (supported by NHS England’s PCRM system and PDS) and undertaking list reconciliation and maintenance activities to keep patient lists up to date
- medical records – responsible for moving hard copy patient medical records and temporary patient records between practices and into storage; and facilitating urgent medical record access requests
- practice mergers and closures – administering the merger and closure of GP practices
- supplies – providing NHS stationery, pre-printed forms, needles and syringes via an online portal
- the National Performers List (NPL) – administering entry and changes to performers lists on behalf of NHS England
A brief introduction to and further details on PCSE services can be found on the PCSE webpage.
3.1.5 This policy sets out:
- the arrangements for managing patient assignments (part A)
- list maintenance for primary medical services including general list maintenance by PCSE (part B1) and targeted list cleansing by commissioners (Part B2)
- managing closed lists (part C)
3.2 Part A: managing patient assignments
Scope
3.2.1 This part A sets out the processes the commissioner should follow in respect of patient assignment to practice lists. It also provides information regarding the grounds for practice refusal to register a new patient and potential difficulties that may arise following removal from a practice list and the procedures that must be followed in the event patient assignment to a practice list is required.
3.2.2 Where a practice list is open, a patient may apply for registration either in person or on behalf of another, whether or not they are resident in the practice area or are currently registered at another practice.
Refusing patient registration onto an open list
3.2.3 In most circumstances, practices operating an open list do so effectively and in a reasonable manner, accepting applications for new registrations on a daily basis. There are, however, a number of circumstances in which a patient may find it difficult to obtain registration with their local practice and, in these circumstances, it is important that the commissioner is fully aware of the grounds under which a practice may refuse registration and the processes that must be followed to demonstrate that this refusal has not been on prejudicial grounds.
3.2.4 A practice may only refuse to accept a patient onto an open list where it has reasonable grounds for doing so. Reasonable grounds will not relate to the patient’s race, gender, social class, age, religion, sexual orientation, appearance, disability or medical condition. Where a practice refuses to register a patient, the reason for this refusal must be given in writing to the patient within 14 days of the request for inclusion being made. The contractor must keep a written record of applications and reasons for refusal. Reasonable grounds for refusal may include that the patient:
- does not live in the practice area
- is already registered with a Special Allocation Scheme provider
3.2.5 The operation of a waiting list for registrations is not appropriate. Where a practice feels that it cannot accept new registrations at the time of the patient’s application to join the practice, it may need to consider whether the practice list should remain open and enter into discussions in this respect with the commissioner. See chapter 3: Managing patient lists for more information.
3.2.6 In the event the commissioner is approached regarding any refusal of registration, it must contact the practice to confirm the situation and address the matter in line with the GMS Regulations, PMS Regulations or APMS Directions (as appropriate).
Removing a patient from a practice list
3.2.7 Where a practice wishes to remove a patient from its practice list, the practice must normally provide the reason for removal in writing to the patient. The reason:
- must not relate to the patient’s protected characteristics such as: age, disability, gender reassignment, marriage and civil partnership, pregnancy, race, religion or belief, gender or sexual orientation
- must not directly relate to a patient’s medical history of mental illness, learning disability or neurodiversity
- may include a statement to the fact there has been an irrevocable breakdown in the relationship between the patient and the contractor, where that is the case and the circumstances are such that it is not appropriate to give a more specific reason
3.2.8 Removal may normally only be requested if, within the period of 12 months prior to the date of the request, the practice has warned the patient in writing that they are at risk of removal and stated the reasons for this.
3.2.9 It may be justified that a written warning was not possible or appropriate in the circumstances that:
- the reason for removal relates to a change of address outside of the practice area including where a patient has been registered as a temporary resident elsewhere and has exceeded the 3-month temporary residency period
- the practice has reasonable grounds for believing that the issue of a warning would be harmful to the physical or mental health of the patient or put at risk one or more members of the practice team
- it is, in the opinion of the contractor, not otherwise reasonable or practical for a warning to be given. The practice must record in writing either the date of any warning given and the reason for such a warning or the reason why no such warning was given
3.2.10 All patient removals must be recorded by the practice, including the reasons for and circumstances of the removal and this record must be made available to the commissioner should it be requested.
3.2.11 Notifications by the contractor to the commissioner (via PCSE) should be made on removals from the contractor’s patient list. The commissioner must refer to the relevant regulations/directions (set out in Schedule 3, part 3 of the GMS Regulations; Schedule 2, part 3 of the PMS Regulations; the APMS Directions do not require APMS contracts to have provisions relating to patient lists – the commissioner should refer to the wording of the relevant APMS contract).
3.2.12 Practices may remove a patient with immediate effect where the patient has committed an act of violence or behaved in such a way that the contractor, practice staff, other patients or those present at the place the services were provided have feared for their safety. The incident leading to the request for immediate removal must have been reported to the police. It is highly likely that there are different ways in which violent patients are managed nationally as services were commissioned in different ways under a violent patient directed enhanced service scheme. For this reason, the commissioner must refer to the relevant regulations/directions and chapter 7: Managing violent patients – Special Allocation Scheme.
3.2.13 Patients may experience difficulties in registering where they have been removed from a practice list, although (other than on the grounds of violence or threatening behaviour) this should not ordinarily be a factor considered by practices when approached by new patients. It should also be noted that patients have the right to choose to move from one practice to another, even within the same locality, without providing grounds for doing so.
3.2.14 In any type of patient deduction, consideration must be given to any potential safeguarding concerns. Where a patient is at risk of being removed for missed appointments, for example, that may reflect on parenting/caring capacity (for example, mental health) and consideration must be given to safeguarding either for children or vulnerable/at-risk adults. Advice should always be sought from local safeguarding leads and/or the commissioner’s designated professional.
3.2.15 With regard to the deduction of children (aged under 18) GP practices have the clinical expedient prerogative to retain children (under 18 years old) under the paramountcy of the child within the Children and Families Act 2014, until such time that they understand how the children might be cared for by another NHS or private GP, especially if vaccinations or screening are still indicated.
3.2.16 It should also be noted that:
- children and young people (CYP) on a protection order or protection plan should not be de-registered on the grounds of behaviour including non-attendance
- CYP (not protected) and adults with a learning disability and/or who are autistic, individuals with a mental health issue or those with a formal carer should not be de-registered on the grounds of behaviour including non-attendance
3.2.17 These citizens may need to be referred to safeguarding leads since they might be at risk either through behavioural problems or non-attendance of their appointments.
3.2.18 These citizens should be allowed to sustain their GP registration for continuity of care until such time as it can be established how they might be cared for by another NHS or private GP. Therefore:
- children of parents or carers who have been removed from the list for any reason must not be left without access to primary care service
- where parents or carers have been removed from the list due to aggressive or violent behaviour a risk assessment should be completed to identify any risk to their children and the appropriate safeguarding referrals made
Removal from a practice list – at the request of the patient
3.2.19 In circumstances where a patient wishes to be removed from a practice list, the patient must ideally contact the GP practice; however, they may choose to contact PCSE.
Where PCSE receives a patient removal request, they will only process applications from adults. PCSE will first contact the practice to check if any safeguarding considerations apply where patients may need to remain registered with the practice. If there are no safeguarding concerns confirmed by the practice, the patient will be removed 14 days after the request is received. Where safeguarding concerns are present and the practice has made PCSE aware of this, the patient will remain on the contractor’s list. PCSE will contact the practice using GP Links when these occasions occur.
Please see for further reference Course: Safeguarding Hub | RCGP Learning.
Where patient assignment to a practice list is required
Assignment to an open list
3.2.20 The commissioner may assign a new patient to a practice whose list of patients is open and, in making the assignment, the commissioner shall have regard to:
- the wishes and circumstances of the patient to be assigned
- the distance between the patient’s place of residence and the practice premises
- assignment as an out of area patient where the patient lives outside the practice area and this would be appropriate in the individual’s circumstances (and the practice has not otherwise agreed to register as if in area)
- whether, during the 6 months ending on the date on which the application for assignment is received by the commissioner, the patient’s name has been removed from the list of patients of any practice in the area of the commissioner, at the request of the practice
- whether the patient’s name has previously been removed from the list of patients of any practice in the area of the commissioner owing to violent behaviour and, if so, whether the practice to which the patient is to be assigned has appropriate facilities to deal with such a patient
- other matters the commissioner considers relevant
3.2.21 A new patient is defined as a person who:
- has been refused inclusion in a contractor’s list of patients or has not been accepted as a temporary resident by a contractor
- would like to be included in the list of patients of a contractor in whose outer boundary area (as specified in accordance with regulation 20(1)(d)) that person resides
3.2.21 In making an assignment, the commissioner will contact the practice to which the patient is to be assigned, to inform it that an assignment is being made. Following this contact, the commissioner will send an assignment notification (see annex 5: example assignment notification) to both the receiving practice and PCSE (patientremovals@nhs.net) for their information. A letter (see annex 6: example patient letter confirming registration) will also be sent to the patient informing them of their registration and provide details as to how they may access the service. In most cases, this letter will be issued by PCSE; however, the commissioner should ensure that this process is satisfied either through this mechanism or through its own local arrangements.
PCSE is responsible for sending the standard patient letter in the case of allocations to open lists.
Assignment to a closed list
3.2.23 The commissioner may not assign a new patient to a practice that has closed its list of patients except in the following circumstances:
- most or all the providers of essential services (or their equivalent) whose practice premises are within the commissioner’s area have closed their lists of patients
- the assessment panel (as detailed below) has determined that patients may be assigned to the practice in question, and that determination has not been overturned either by a determination of the Secretary of State or (where applicable) by a court
- the commissioner has entered discussions with the practice in question regarding the assignment of a patient, whereby additional support that the commissioner can offer to the practice may be required. The commissioner shall use its best endeavours to provide appropriate support and should discuss support in respect of the first assignment of a patient and any subsequent assignments made to that contractor during their list closure
PCSE is responsible for sending the standard patient letter in the case of allocations to closed lists.
Assignment based on the determination of a commissioner assessment panel
3.2.24 Where the commissioner has the need to assign a patient to a practice that has a closed list and most or all the providers of essential services (or their equivalent) whose practice premises are within the locality of the commissioner have closed their lists of patients, the commissioner must:
- prepare a proposal to be considered by the assessment panel which must include details of those practices to which the commissioner wishes to assign patients
- ensure that the assessment panel is appointed to consider and determine its proposal and the members of the assessment panel include:
- a commissioner director/officer
- a patient representative who is a member of the local health and wellbeing or local Healthwatch
- a member of a LMC but not a member of the LMC formed for the area in which the contractors who may be assigned patients as a consequence of the panel’s determination provide services
- notify the following in writing that it has referred the matter of patient assignment to the assessment panel:
- the relevant LMC for the contractors in the area of the commissioner
- any contractors whose practice premises are within the commissioner’s jurisdiction that have closed their list of patients and may, in the opinion of the commissioner, be affected by the determination of the assessment panel
3.2.25 In reaching its determination, the assessment panel shall have regard to relevant factors including:
- whether the commissioner has attempted to secure the provision of essential services (or their equivalent) for new patients other than by means of their assignment to contractors with closed lists of patients
- the workload of those contractors likely to be affected by any decision to assign such patients to their list of patients
3.2.26 The assessment panel shall reach a determination within the period of 28 days from the date on which the panel was appointed.
3.2.27 The assessment panel shall determine whether the commissioner may assign patients to practices which have closed their lists of patients. If it determines that the commissioner may make such assignments, it shall also determine those practices to which patients may be assigned.
3.2.28 The assessment panel may determine that the commissioner may assign patients to practices other than those practices specified by the commissioner in its proposal, as long as the practices were notified during the preparation stages of the assessment panel being held. The assessment panel’s determination must include the factors considered by the panel and be made in writing to:
- the LMC for the contractor(s) in the area of the commissioner to which the determination relates
- any contractors whose practice premises are within the commissioner’s jurisdiction that have closed their list of patients and may, in the opinion of the commissioner, be affected by the determination of the assessment panel
NHS dispute resolution procedure relating to determinations of a commissioner assessment panel
3.2.29 Where an assessment panel determines that the commissioner may assign new patients to contractors which have closed their lists of patients, any contractor specified in that determination may refer the matter to the Secretary of State to review the determination of the assessment panel. Please refer to part C, chapter 4: Managing disputes.
Removal by a contractor of patients assigned to the practice
3.2.30 Historically, practices have often applied an unwritten agreement to the retention period of assigned patients. However, there are no formal arrangements in respect of timescales for patient retention in these circumstances. While the significant majority of practices continue to manage assigned patients in the same manner as an ordinarily registered patient, others may commence a formal removal process immediately following assignment. The commissioner has a responsibility to ensure that all requests to remove a patient at the request of the contractor must be managed in line with the relevant regulations/directions.
3.3 Part B1: general list maintenance for primary medical services
Scope
3.3.1 This part B1 sets out the processes for the commissioner to ensure list maintenance is appropriately managed. It details the list maintenance and data quality measures to be undertaken and suggests additional measures to be taken. Where references are made to actions to be followed by the commissioner, these actions should, where possible, be done together with the available support services or payment authority.
3.3.2 Primary medical service contracts are predominantly funded on a capitation basis. It follows, therefore, that if a patient list is overstated, the contractor will receive more funding than it is entitled to and this presents a significant financial burden on NHS resources.
3.3.3 While in most cases, contractors endeavour to maintain their registered lists in a current and accurate state, patients often fail to notify their registered practice when leaving the area and/or country, resulting in potential duplicate registrations and ghost and gone away patients remaining registered on the national patient registration systems.
3.3.4 Some degree of list inflation is inevitable, but manageable if kept within reasonable bounds. The commissioner and PCSE are expected to engage in regular proactive list reconciliation and maintenance activities with general practices.
3.3.5 Ongoing and effective maintenance of lists is essential to ensure they are accurate. However, even with the most effective list maintenance procedures in place, a practice list can hold 3% to 8% of inaccuracy due to patient turnover alone.
3.3.6 Practices with robust systems in place to verify and record patient details at the point of registration, as well as regular systematic checking of details when patients contact the practice, have more accurate lists. The introduction of the online GP registration service is expected to help by standardising the way practices receive registrations online and automatically checking these.
3.3.7 The accuracy of a practice’s registration list is important for:
- the efficacy of ill-health prevention/screening programmes and total population capture
- the assessment of performance and clinical outcomes which are often compared on a ‘per patients’ denominator
- the appropriate use of public funds, as allocations are made on a £ per patient basis
Operating principles
3.3.8 List maintenance processes should be designed with the proactive engagement of the commissioner, patients (or their representatives), PCSE and LMCs on behalf of GPs and practice managers. This should be through a continuous rolling programme: for example, working through the practice registers over a 1 to 3-year period or targeting specific patient cohorts to, for example, support a vaccination or screening programme: for example, childhood immunisations, influenza or cervical screening.
3.3.9 A ‘one-hit’ approach in which a single practice is targeted should be avoided except in exceptional circumstances. This might include due diligence when transferring a full list to a new contract, for example. In all cases this should be carried out in discussion with the LMC.
3.3.10 Contractors have a crucial role in ensuring their staff access relevant training, are familiar with the FP69 process and are proactive partners in the list maintenance process, responding to requests from PCSE. (Note: the timeframe for the FP69 process will reduce from 6 to 3 months from 1 October 2025 following agreed changes to the GMS contract.)
3.3.11 When responding to an active FP69 (see annex 7: stage 1 of a list maintenance programme and annex 8: stage 2 of a list maintenance programme) a practice declaration will be sufficient. The practice is responsible for ensuring all declarations made are accurate and should be made aware that these can be challenged where any inconsistencies are highlighted through a cluster-wide audit. Where possible, practices should respond to active FP69 using the available dropdowns to remove ambiguity in free text responses. PCSE may query a practice’s declaration and take the appropriate action when there is no response from the practice.
3.3.12 A list maintenance exercise is not designed to address performance failures. Where there are reasonable grounds for believing that list inflation is particularly high at an individual practice, this concern should be handled separately as part of contractual review and management activity.
3.3.13 The commissioner should ensure that where the PCSE disputes the practice declaration, the practice is told why and is advised of any list actions that have been taken.
Minimising inconvenience
3.3.14 Improving patient selection criteria – for example, using a range of data to improve accuracy and relevance – will ensure the right patients are targeted and will increase the efficacy of list maintenance processes for both patients (that is, fewer patients having to confirm their continued registration) and practices (the FP69 process being applied more accurately to suspected ‘gone away’ patients).
3.3.15 Improving patient communication methods – for example, increasing the use of digital communication channels, such as email, the NHS App and SMS – while maintaining flexibility for patients to choose the most appropriate way to respond, will mean they can respond more easily and quickly.
3.3.16 Advance screening of the proposed cohort by practices can mean that fewer patients will be inconvenienced by having to respond, but this needs to be balanced with the additional workload burden this can place on GP practices. A patient-first approach, targeted at the right patients with a range of communication methods, is likely to be more effective.
3.3.17 The commissioner should maximise awareness in the patient population of list maintenance procedures by ensuring that an effective patient communication strategy is in place. This could include actions, for example, to support patients to proactively de-register from their GP practice when they leave the country. Examples of what has worked well include:
- communications addressed to named patients and not the occupier (see annex 9: sample letter to patients)
- contractor teams alerting patients to registration checks well in advance – as part of the registration conversation, through display notices in a practice
- the commissioner and contractors making the process clear to patients through any letters and posters – for example, what the letter looks like, what to do when you get one, the steps in place to minimise de-registration errors, what to do if there is a de-registration error, what to do if a letter arrives for someone not living at that address
- communications must take into account the Accessible Information Standard which requires organisations to ensure that disabled patients receive information in formats that they can understand
- communications must be tailored for different languages and consideration of other support for patients whose first language is not English
3.3.18 List maintenance is also an opportunity to improve other aspects of patients’ registration including the accuracy of the patient information held. The commissioner should ensure that contractors verify the details held on the practice system systematically as part of routine ongoing maintenance.
Patient registration process
3.3.19 Appropriate and timely management of the patient registration process is essential in minimising the potential for list inflation.
3.3.20 The standard registration process following an online or paper registration request, requires all general practices to notify all registrations to the national Primary Care Registration Management (PCRM) system. The PCRM user should then confirm the registration to the practice and take steps to arrange via PCSE for the transfer of paper medical records from the patient’s previous general practice. Electronic links are in place between PCRM and all general practices that enable this process.
3.3.21 GP practices are required to monitor that all their registrations and patient deductions are acknowledged by PCRM. This ensures that patients are correctly registered and will be included in NHS screening and immunisation programmes.
3.3.22 Practices should also check their list size of registered patients on a quarterly basis against the GP Payments and Pensions System by logging into PCSE online. This ensures that payments to the practice remain accurate and any issues with the registration process are identified.
3.3.23 The process for confirming the new patient registration by PCRM involves checking the patient details against the Personal Demographics Service (PDS) to confirm the patient’s NHS number. Where NHS numbers cannot be traced, the system provides for the user to request the allocation of a new NHS number.
3.3.24 Where it is not possible to trace an NHS number for a patient, rather than request allocation of a new NHS number, the registration should be kept pending and the previous general practice contacted to obtain further details.
3.3.25 If the practice cannot provide further information to enable the NHS number to be traced, it should be asked to contact the patient to obtain this. By taking these steps, the user will ensure that allocation of new NHS numbers is kept to a minimum and therefore minimises the potential for list inflation.
3.3.26 Where a new NHS number has been allocated, then additional checks are undertaken by the PDS National Back Office (NBO) to help ensure a duplicate NHS number has not been created for a patient. Where a duplicate NHS number is identified, this is referred to the NBO for rectification.
3.3.27 It is essential that robust procedures are in place to prevent the creation of duplicate registrations at the time of registration.
3.3.28 NHS England works to ensure that the PCSE is processing routine registrations in a timely manner as this is also key to ensuring accuracy of practice lists.
Elements of a rolling list maintenance programme
3.3.29 Returned mail. Routine business processes that involve sending letters to patients help reduce list inflation, as any returned letters result in general practices being given the statutory notice period to confirm that the person is a patient to whom it is still responsible for providing essential services. The FP69 flag in these circumstances will affect invitation to screening programme. Where confirmation is not provided, then the patient is removed from the practice list. The only exception to this is patients aged under 18 who will remain registered under the paramountcy principle of protection (refer to chapter 4: GP patient registration standard operating principles for primary medical services for further information).
3.3.30 These letters to patients, using data sourced from the PDS system, are inclusive of, but not limited to, the following:
- cervical screening invitation letters sent to all women aged 25–64
- cervical screening test results sent to all women attending for a test as part of the NHS Cervical Screening Programme
- flu vaccination invitation letters sent to patients aged 65 and over together with any patients identified by general practices as being in an ‘at-risk’ group
- chlamydia screening invitation letters sent to patients on behalf of certain local authorities
- bowel screening invitation letters sent to all patients aged 54 and 74
- letters sent to all patients registered with a specific general practice if there are any significant changes to practice arrangements
- new patient registration letters when someone registers with the NHS for the first time
- verification by general practices of the vaccination status of all children aged 2 years and 5 years registered with the practice on the first day of each quarter
3.3.31 The use of NHS Notify to send direct patient care letters has enabled the automation of notifications to PCSE to raise the statutory FP69 process.
3.3.32 In maintaining the PCRM system, specific tasks need to be undertaken to reduce list inflation and help maintain the accuracy of practice lists. The annual programme of checks to be undertaken is shown below together with the standard procedure which should be adopted for each.
3.3.33 NHS England may agree with PCSE to pause these checks in exceptional circumstances. NHS England may equally agree with PCSE to adjust the volume of checks in response to increasing national rates of patient list inflation: for example, increasing at times of high patient list inflation and reducing at times of low patient list inflation.
3.3.34 The flowcharts in annex 7: stage 1 of a list maintenance programme and annex 2: stage 2 of a list maintenance programme indicate the standard process to be followed.
Annual list reconciliation checks
| Scope | Process |
|---|---|
| 3-year rolling cycle for all GP practices, meaning a third of GP practices each year |
PCSE must:
Failure to adhere to the timeframes will result in downloads being out of date and repeat work for practices and PCSE. Where PCSE does not receive the response required in the given timeframe, commissioners will be notified for follow-up action. Any delays in the validation process can create potential patient safety risks for safeguarding and access to wider health and cancer screening services. Delays can also risk the GP practice not receiving correct patient payments. Note: commissioners and GP practices can request a one-off review if they believe there is a discrepancy with patient list size by emailing pcse.dataquality@nhs.net and including the details given on PCSE’s patient lists webpage. |
| Patient group/cohort | Frequency | Process |
|---|---|---|
| Multiple occupancy (MO) | After the initial month, PCSE will check the additional patients who appeared at MO addresses and reset |
PCSE must:
|
| University/college student/residential school | Annually October to December |
PCSE must:
|
| Patients aged 100 and over | 6-monthly March and September checks |
PCSE must:
|
| Transient checks | Monthly |
PCSE must:
|
| Notification of demolished addresses (the FP69 flag in these circumstances will affect a breast screening invitation) | Quarterly |
|
| Patients not seen by general practice in previous 5 years | Annually |
PCSE should:
|
3.3.35 NHS England has agreed (as part of the package of changes on the 2025/26 GP contract) to enable patient communications for list maintenance purposes to be supported digitally, in addition to or instead of by letter, allowing additional routes to support effective patient communication and responses. Letter references in this current policy may include communication and reminders issued by email, SMS or NHS App.
Additional measures (see also part B2 below)
3.3.36 Despite initiating a rolling programme of list maintenance measures, figures comparing ONS mid-year populations with PCRM registered population may still show significant inflation. These inflation rates may also differ significantly for local areas.
3.3.37 If the commissioner has a particularly large variance it may wish to undertake a targeted campaign to reduce this in one large exercise. If so, the commissioner is strongly urged to engage their general practices and the relevant LMCs.
3.3.38 Suggested work that could be undertaken is:
- comparison of ONS mid-year stats with PCRM figures at middle SOA level. This will identify localities within each area where inflation rates are highest and will therefore highlight specific areas to be targeted
- send mailshot to confirm residency to male patients aged 18–44 living in areas where inflation rates are highest. ONS and PDS comparison at area level has previously shown that the highest inflation rates are related to male patients in this age group, possibly because there are no routine mailshots sent to this cohort
- undertake further immigrant checks 3 years after the date of first registration for persons who immediately before their current registration are recorded as having arrived from abroad
- issue guidance and clarification for general practices on the FP69 procedure. Greater awareness of the processes for removing patients within general practices could reduce the scale of list inflation. If guidance has not previously been given to practices on the FP69 process, then this should be provided. Once in place, this could become part of a standard rolling programme
3.3.39 It is essential that work is carried out to reduce list inflation and verify practice lists, but it is also important to recognise the resource implications of undertaking this work. It is equally essential that all work carried out is recorded and the outcomes monitored to evaluate the success of each initiative.
3.3.40 The commissioner should ensure that PCSE submits a quarterly report to the commissioner detailing the practice and patient volumes reviewed and the outcomes.
3.3.41 Given the requirement (from 1 October 2025) to allow a practice 3 months to confirm the address before a patient can be removed from the practice list, it is recognised that any list maintenance exercise could take 3 to 6 months before benefits are realised. This needs to be considered when assessing the effectiveness of interventions.
3.4 Part B2: targeted list maintenance for primary medical services
Background
3.4.1 The Office for National Statistics (ONS) regularly publishes mid-year population estimates, currently down to the level of ICB (ONS ICB mid-year population estimates), middle super output area (ONS MSOA populations) and lower super output area (ONS LSOA populations). Using these population estimates alongside the numbers of patients registered at a GP practice and other sources of local intelligence, such as patient postcode list, can assist in determining at a local level whether the difference could warrant further investigation.
Scope
3.4.2 This part B2 sets out some considerations and investigations that could be undertaken to determine whether a targeted list validation exercise may be beneficial within the commissioning area and what that could involve.
3.4.3 A key line of enquiry in national counter fraud exercises often relates to list maintenance and so GP practices may welcome support in proactively reviewing their registered list.
Available data sources
3.4.4 Of the data sources listed below, not all will be available to all organisations: for example, patient level data cannot be held by NHS England.
Data providers
3.4.5 NHS England:
- number of patients registered at a GP practice
- number of patients registered at a GP practice (PCN/ICB level)
- number of patients registered at a GP practice (NHS England commissioning region)
- number of patients registered at a GP practice mapped to LSOA
From April 2017, NHS England began publishing the above data monthly. Prior to this publication was quarterly, on the first day of April, July, October and January.
The above data is available in both 5 year age groups and single year of age (by male, female and total). Files are available to download for onward analysis, but NHS England also provides an interactive platform, the General Practice Data Hub.
3.4.6 Office for National Statistics:
- ICB mid-year population estimates
- middle super output area mid-year population estimates
- lower super output area mid-year population estimates
ONS publishes this data annually, usually at the end of October each year, for the previous year.
3.4.7 data.gov.uk:
- postcode to output area to lower layer super output area to middle layer super output area to local authority district lookups for England and Wales
What to consider, who and why?
3.4.8 Where a GP practice list contains records of people who should no longer be on the list this is known as list inflation. There can be many reasons for this and commissioners and GP practices should work together to minimise this through list maintenance.
3.4.9 In some GP practices there can often be high turnover (leaving and joining) of patients, which can be challenging to monitor but easier with timely processing.
3.4.10 There are records that link to patients who do not de-register and there are 2 principal reasons why an individual may not de-register.
3.4.11 Some people may be slow to re-register at other GP practices, despite having moved away from the area, as they are relatively healthy and do not see re-registration as a priority.
3.4.12 People who live abroad are required to de-register from their GP practice. They may fail to do so either because they do not see it as a priority when moving abroad or because they wish to have continued access to the NHS (often referred to as ‘ghost patients’). This affects list inflation at both the local and national level.
3.4.13 ONS suggests that the following groups tend to be quicker to register a change of address:
- mothers with young children
- those with ongoing health conditions
- the very elderly
3.4.14 Additionally, the following tend to be slower to register a change of address:
- young healthy adults, especially males – including students
- highly mobile individuals
- healthier persons, especially males
- males – in general
3.4.15 Parental home: mobile young adults may choose or default to remaining registered at their parental address.
3.4.16 Shared custody: there is potential for a range of issues where there is shared custody of children at different addresses. These can potentially include:
- split residence not reflected in the record
- duplicate registrations
- use of different names (particularly surnames)
3.4.17 Care homes (and similar institutions): where a patient moves into a care home this may not be recorded as a change in address, particularly if the intended stay is short. These stays may become longer so that there has in effect been a change in residence, although the GP register has not been updated. By contrast a move may be intended as long-term (and the move recorded on the patient register) but the patient may die soon after the move.
3.4.18 Please note, a change of address should also not be considered where a patient attends a special residential school, boarding school, children’s homes or other residential facility, unless this is a secure or specialist hospital setting or immigration centre.
3.4.19 There are 2 potential consequences for statistical use of data:
- a spell of residence away from the home address can be missed
- a death can be recorded with a place of residence given as different from that recorded on the patient register
3.4.20 Confused or mismatched records: this is where more than one patient is associated with the same NHS number; that is, one NHS number with multiple patients. Potential reasons for patients being confused in this way include:
- mismatching a patient to another with similar details on registration or other interaction and assigning to them someone else’s NHS number
- clerical error on input of NHS number or other detail (demographic or clinical), such as into a clinical system or recording in manual records
- error by the patient in writing their NHS number or other demographic details, or poor legibility, and there is no check of the details or a check fails to identify the error: for example, the same date of birth or similar names
- in rare cases, fraud, where one patient is deliberately misrepresenting and using the NHS number of another patient to obtain drugs or medical services
3.4.21 Duplicate records: this is where one patient is associated with more than one NHS number. Potential reasons for duplicate records being created include:
- on registration with a GP, a patient is incorrectly identified as a new entrant to the NHS, such as a returning emigrant, person discharged from the armed forces or person returning from private practice. This may be because the patient does not provide sufficient information or the questions they are asked about their history are insufficient
- on registration with a GP, no match is traced to previous records. This may be because:
- the patient’s name has changed or a variant, possibly a shortened version, is provided
- clerical error on data input meaning there is a difference between the data already recorded and the data being used to trace
- error by the patient in providing their details, including legibility and where a check is not undertaken or fails to identify the error, for example, date of birth format or a name spelling
- on registration with a GP, a patient gives insufficient details to allow a match
3.4.22 For both confused or duplicate record, errors may occur in primary, secondary or other care settings for the reasons outlined above. It remains important to validate patient data at every interaction so that data quality can be maintained and identified issues can be resolved at the earliest opportunity.
3.4.23 Snapshot: the data that NHS England currently use from the patient register is based on a (typically annual) snapshot. This gives the position at that point in time, as it occurs on the register. This approach means there is no ‘history’ between snapshots of changes. For example, where there are 2 or more changes of address in a year, only the first and last of these addresses are captured (implying a single move). Moves before exiting from the system (including emigration and death) can also be missed, as can moves shortly after entry to the system (including immigration and birth).
3.4.24 Coverage: the patient register is a broad coverage source, but some groups are not included (under-coverage of the total population) and there are also some over-coverage issues. Evidence from ONS shows that over-coverage tends to be the larger issue, with the patient register having 4.3% more people registered than the 2011 Census estimate of population, while we are aware in NHS England the range can be 3% to 8%.
3.4.25 The following groups are not included in GP practice register, and may be the cause of statistical under-coverage:
- patients solely registered with private GPs
- babies who have yet to be registered at a GP practice
- migrants into the UK who have yet to register
- armed forces (though some remain on GP lists)
- some armed forces dependants
- prisoners (other than those with a sentence under 6 months)
- some prisoners with a short sentence who have received medical assistance in prison
- patients who have been removed through ‘no contact’ measures
- patients with a temporary NHS number, where no ‘permanent number exists or where their permanent number is not on a GP register
3.4.26 The following groups, for some statistical purposes, may be thought of as over-coverage:
- patients who are no longer resident in the UK (emigrants)
- patients who are staying in the UK for only a short period
- duplicate records
What local checks could be undertaken
3.4.27 Utilising the data sources and data listed in 3.4.5 and the intelligence from ONS in 3.4.6 above, commissioners can determine where they may wish to focus attention and or support for the practice. Decisions should be made locally and on a case-by-case basis. Commissioners may wish to undertake analysis internally or work with a partner, such as a commissioning support unit (CSU), which can work with its Data Services for Commissioners Regional Offices (DSCRO) should it wish to interrogate record-level data that has been appropriately processed.
Comparing data sources and geographies
3.4.28 The considerations below provide a sample of the checks that could be embarked on when undertaking a targeted list exercise.
3.4.29 Commissioners should review trends in ICB resident population estimates compared to trends in GP registered populations and ask the following:
- are the proportions similar?
- are all the GP practices within the ICB’s area increasing or decreasing by a similar proportion?
- are any practices significantly variant in comparison to other practices and the ICB trend?
- have there been any practice mergers or closures resulting in list dispersal?
- have there been any new and large-scale property developments recently?
3.4.30 Commissioners should also review trends in LSOA population (ONS estimates) compared to trends in GP registered populations (LSOA data from NHS England) and ask:
- are the proportions similar?
- which LSOAs fall within the practice boundary? (answering this may require the support of a third party. Can you map record-level patient data to determine in which LSOAs the practice has the majority of its patients?
- are the LSOA populations (resident and registered) mapped to GP practices increasing or decreasing in broadly the same proportions as those for the GP practices as a whole?
- how do they compare to other neighbouring practices?
- have there been any practice mergers or closures resulting in list dispersal?
- have there been any new and large-scale property developments recently?
- is there any in-depth work that could be undertaken with a partner (CSU) and record-level record data?
3.5 Part C: managing closed patient lists
Scope
3.5.1 This part C sets out the processes to be implemented when managing applications to close patient lists and to extend a closure period.
3.5.2 At all stages of these processes, it is essential that the commissioner works with the contractor and the relevant LMC to ensure clear and transparent decision-making and that all decisions are made in line with internal governance arrangements.
Applications to close a patient list
3.5.3 Sometimes a contractor may wish to close its list to new registrations: for example, where there are internal capacity issues or premises refurbishments. The contractor must seek approval from the commissioner by a written application (the “application”) before this may happen. A template application for the contractor to complete is provided in annex 10: sample template. The contractor should use the template application to ensure it completes all the required information. The contractor may obtain the application itself (for example, by accessing this policy) or it may be requested by the contractor. An example covering letter from the commissioner to the contractor enclosing an application form is provided in annex 11: sample letter.
3.5.4 The commissioner must acknowledge receipt of the application within 7 days of receipt and may request further information from the contractor to enable it to consider the application thoroughly.
3.5.5 With a view to possibly enabling the contractor to keep its list of patients open, the commissioner and the contractor must talk openly to establish:
- what support the commissioner may give the contractor
- changes the commissioner or contractor may make
3.5.6 The contractor or the commissioner may at any time throughout these discussions invite the appropriate LMC to be included in the dialogue about the application.
3.5.7 The commissioner should ensure compliance with the general duties of NHS England. Please refer to part A, chapter 2: General duties of NHS England for further information. The commissioner may consult affected parties – an example letter is provided in annex 12: consultation letter.
3.5.8 The contractor may withdraw the application at any time before the commissioner makes its decision on the proposed list closure.
3.5.9 The commissioner must determine within a period of 21 days, starting on the date of receipt of the application (or within a longer period as the parties may agree), whether:
- to approve the application and determine the date the closure is to take effect and the date the list of patients is to re-open
- to reject the application
3.5.10 The commissioner must notify the contractor of its decision in writing as soon as possible after the 21-day period.
Approval of patient list closure: closure notice
3.5.11 Where the commissioner has granted approval for closure of the patient list, a closure notice must be issued to the contractor as soon as possible after the decision is reached, with a copy sent to the LMC for its area (if any) and to any person consulted in the decision-making process. The commissioner should use the template notice in annex 13: approval of closure – example closure notice to ensure it responds to the contractor with all the required information.
3.5.12 The contractor must close the list on the date in the notice and the list should remain closed for the time specified unless the commissioner and the contractor agree that the list should be re-opened to patients before the expiry of the closure period.
Rejection of application for list closure
3.5.13 When the commissioner decides to reject an application to close a list of patients, it must as soon as possible:
- provide the contractor with a notification including the reasons why the application was rejected. The commissioner should use the template in annex 14: rejection of closure – example letter to ensure it responds to the contractor with all the required information
- at the same time, send a copy of the notification to any affected LMC for its area and to any person it consulted in the decision-making process
3.5.14 When the commissioner decides to reject a contractor’s application to close its list of patients, the contractor must not make a further application until:
- the end of the 3-month period starting on the date of the decision of the commissioner to reject; or
- the end of the 3 months starting on the date of the final determination regarding a dispute arising from the decision to reject the application made pursuant to the NHS dispute resolution procedure (or any court proceedings) (please refer to part C, chapter 4: Managing disputes for further information on the NHS dispute resolution procedure), whichever is the later
3.5.15 A contractor may make a further application to close its list of patients where a change in its circumstances is affecting its ability to deliver services under the contract.
Application to extend a closure period
3.5.16 A contractor wishing to extend an agreed closure period must apply to the commissioner no less than 8 weeks before the closure period is due to end.
3.5.17 A template for completion by the contractor is provided in . An example covering letter from the commissioner to the contractor enclosing an application form is provided in annex 16: sample letter.
3.5.18 The commissioner must acknowledge receipt of the application within 7 days and then, if necessary, discuss potential support that could be offered to the contractor and consult any affected LMC and other affected parties before reaching a decision on the application to extend within 14 days from receipt of the application. The commissioner should use the template consultation letter provided in Annex 1.
3.5.19 If the decision is to accept the application, the commissioner must issue an extended closure notice as soon as possible after the decision is reached to the contractor, with a copy sent to the LMC for its area (if any) and to any person it consulted in the decision-making process. The commissioner should use the template provided in annex 18: approval of extended closure – example closure notice to ensure that the contractor receives all the relevant information.
3.5.20 If the decision is to reject the application, the commissioner must provide the contractor with a notification, including the reasons for the rejection of the application, with a copy sent to the LMC for its area (if any) and to any person it consulted in the decision-making process. The commissioner should use the template provided in annex 19: rejection of extended closure – example letter.
3.5.21 The contractor may re-open its list of patients before the closure period expires if the commissioner agrees to this.
3.5.22 Where an application for the extension of the closure period has been made in accordance with this policy, and that application has been rejected, the list of patients will remain closed until such time as any dispute arising from the application has been resolved through the NHS dispute resolution procedure (or any court proceedings) or until such time as the original closure notice expires. Please refer to part C, chapter 4: Managing disputes for further information on the NHS dispute resolution procedure.
4. GP patient registration standard operating principles for primary medical services
4.1 Policy statement
4.1.1 There have been no change in national policy in respect of patient registration for primary medical services. This guidance clarifies the rights of patients and the responsibilities of providers in registering with a GP practice in particular issues in relation to:
- who can access free healthcare
- the provision of documentary evidence of identity or residence on registration – this can in particular affect migrants, refugees and asylum seekers (including ‘failed’ asylum seeks) as they may not have ID or documents such as household bills
- the rights of patients who are temporarily resident in a specialist hospital away from their home address and access to their ‘usual’ GP practice
4.2 Aims
4.2.1 In issuing these patient registration operating principles NHS England aims to:
- clarify the contractual rules in respect of patient registration for patients, practices and commissioners
- reduce the risk of worsening health inequalities for specific populations: for example, asylum seekers or people who are experiencing homelessness
- simplify and standardise the patient registration process for patients and practices
- embed best practice approaches for patient registration
- ensure fairness, equity and transparency in the way general practice services are delivered across England
4.3 Context
4.3.1 The Health and Social Care Act 2012 places an obligation on NHS England to secure the provision of primary medical services for patients throughout England. In addition, the Health and Social Care Act 2012 introduced statutory duties on the NHS to “have regard to the need to reduce inequalities” in access to and outcomes achieved by services.
4.3.2 There are further duties around equality and health inequalities imposed on NHS England under the Equality Act 2010 and NHS Act 2006.
4.3.3 NHS England wishes to establish operating principles for GP practices for patient registration that promote equality, human rights and public health and reduce health inequalities.
4.3.4 In addition, the Care Quality Commission (CQC) provides guidance: GP myth buster 29: looking after homeless patients in general practice and GP myth buster 36: registration and treatment of asylum seekers, refugees and other migrants.
4.3.5 In 2014 homeless and health research provided by Homeless Link reported that, of the people who are homeless they surveyed, 90% were registered with a GP. However, many responded that they were not receiving the help they needed for their health problems and 7% had been refused access to a GP or dentist in the previous 12 months. In some cases, these refusals were due to having missed a previous appointment or because of behaviour. Others reported that they were refused access if they did not have identification or proof of address.
4.3.6 The General Practitioners Committee (GPC) of the British Medical Association (BMA) has related guidance on the BMA website.
4.4 Who can register for free primary care services?
4.4.1 A patient does not need to be ‘ordinarily resident’ in the country to be eligible for NHS primary medical services – this only applies to secondary (hospital) care. In effect, therefore, anybody in England may register and consult with a GP without charge.
4.4.2 Where a GP refers a patient for secondary services (hospital or other community services) they should do so on clinical grounds alone; eligibility for free care will be assessed by the receiving organisation.
4.4.3 As there are no reciprocal arrangements between the nation states, a patient’s nationality is irrelevant in giving people entitlement to register as NHS patients for primary medical services.
4.4.4 In October 2017, contractual requirements were introduced to help identify patients with a non-UK issued EHIC or S1 form or who may be subject to the National Health Service (Charges to Overseas Visitors) Regulations 2015.
4.4.5 For those patients who self-declare at the point of registration that they hold either a non-UK issued EHIC or a S1 form, the practice will be required to manually record that the patient holds either a non-UK issued EHIC or a S1 form in the patient’s medical record and then send the details of the non-UK issued EHIC to NHS England (costrecovery@nhs.net) or send the S1 form to the Overseas Healthcare team via email (nhsbsa.faregistrationsohs@nhs.net) or post. If a registration form has been submitted online via the register with a GP surgery service, then such forms do not need to be sent manually as they will automatically be sent to NHS England as part of the service.
4.4.6 DHSC has agreed to provide practices with hard copy patient leaflets explaining the rules and entitlements of overseas patients accessing the NHS in England.
4.4.7 It is important to note that there is no set length of time that a patient must reside in the country to become eligible to receive NHS primary medical services.
4.4.8 Therefore, all asylum seekers and refugees, students, people on work visas and those who are homeless, overseas visitors, whether lawfully in the UK or not, are eligible to register with a GP practice even if those visitors are not eligible for secondary care (hospital care) services.
4.4.9 The length of time that a patient is intending to reside in an area dictates whether they are registered as a temporary or permanent patient. Patients should be offered the option of registering as a temporary resident if they are resident in the practice area for more than 24 hours but less than 3 months. In some cases, a prospective patient may not know how long they will reside in an area: for example, destitute asylum seekers housed in temporary Home Office commissioned ‘initial’ accommodation. Generally, in such cases where there is uncertainty over the length of time that a patient may be residing in an area, this time will likely be months rather than weeks and NHS England advises that the patient should be registered as a permanent patient.
4.4.10 An immigration health charge (or ‘surcharge’) is now payable by non-UK nationals who apply for a visa to enter or remain in the UK for more than 6 months. People with indefinite leave to remain in the UK and those not subject to immigration control (for example, diplomats posted to the UK) are not liable to pay the surcharge and may be ordinarily resident here and entitled to free NHS healthcare on that basis.
4.4.11 Payment of the health surcharge entitles the payer to NHS-funded healthcare on the same basis as someone who is ordinarily resident, from the date their visa is granted and for as long as it remains valid. They are entitled to free NHS services, including NHS hospital care, except for services for which a UK ordinary resident must also pay, such as dentistry and prescriptions in England.
4.4.12 Payment of the health surcharge is mandatory when making an immigration application, subject to exemptions for certain categories of people and the discretion of the Home Secretary to reduce, waive or refund all or part of a surcharge payment. Most of these groups also receive NHS-funded healthcare on the same basis as an ordinarily resident person.
4.4.13 Patients who have paid this surcharge as part of their visa application process should be registered in the same way as any other patients.
4.5 Immediately necessary treatment
4.5.1 General practices are also under a duty to provide emergency or immediately necessary treatment, where clinically necessary, irrespective of nationality or immigration status.
4.5.2 The practice is required to provide 14 days of further cover following provision of immediate and necessary treatment.
4.6 Determining if the patient lives in the practice area or is registered on a Special Allocation Scheme
4.6.1 All practices are required to have agreed an ‘inner’ boundary with their commissioner. Anyone who resides within the practice’s inner boundary is entitled to apply to register for primary medical services and the practice boundary should be clearly advertised to patients on the GP practice’s leaflet or website if it has one.
4.6.2 In addition, most practices have also agreed an ‘outer’ practice boundary.
4.6.3 Patients who move out of a practice’s inner boundary area but still reside in the outer boundary area may be able to remain registered with the practice if they wish and the practice agrees.
4.6.4 GP practices are able to register new patients who live outside the practice area without any obligation to provide home visits or services out of hours when the patient is unable to attend their registered practice. It is for a practice to decide, at the point of registration, whether it is clinically appropriate and practical to register the individual patient in that way.
4.6.5 Practices are reminded when considering new patients on the register to check GP links and email from PCSE which notifies the practice the registration should be declined for reasons patient is already registered on the Special Allocation Scheme.
4.7 Access to registration
4.7.1 Practices should ensure there is equitable access for all patients who wish to register with them. Registration should be available to all patients every day rather than on particular days and throughout the practice’s advertised opening hours.
4.7.2 Where possible, it is good practice for practices to provide pre-registration documentation in advance: for example, to help patients understand the practice and the services it delivers.
4.7.3 It is It is possible for patients to register via paper form or digital/online and practices should make clear to patients the different ways in which they can register with their practice.
4.7.4 Updates to the GP contract in 2022/2023 removed the need for a patient to provide a wet signature for registration.
4.7.5 An online registration service and corresponding paper form developed by NHS England is available to all practices in England to use. Further information on this service can be found on the Register with a GP surgery service resource hub.
4.7.6 Patients have the right to change practices if they wish. The grounds on which a practice can refuse a registration are limited – see section 4.10: Refusing registration for further detail.
4.8 New patient health checks
4.8.1 It is a contractual requirement that once registered all patients must be invited to participate in a new patient check. However, neither registration nor clinical appointments should be delayed because of the unavailability of a new patient check appointment.
4.9 Requesting documentary information from patients
4.9.1 Under the terms of their primary medical services contracts, GP practices cannot refuse an application to join its list of NHS patients on the grounds of race, gender, social class, age, religion, sexual orientation, appearance, disability or medical condition.
4.9.2 Practices can refuse an application to join a practice list if:
- the commissioner has agreed that they can close their list to new patients
- the patient lives outside the practice boundary
- they have other reasonable grounds
4.9.3 In practice, this means that the GP practice’s discretion to refuse a patient is limited.
4.94 In addition, when patients seek to register there is no regulatory requirement for them to prove identity, address or immigration status or provide an NHS number to register. However, there are practical reasons why a practice might need to be assured that people are who they say they are or to check where they live. Seeing some form of documentation regarding the patient’s identity can help to ensure the correct matching of a patient to the NHS central patient registry, thereby ensuring any previous medical notes are passed on to a new practice. It is legitimate therefore for the practice to apply a consistent but non-discriminatory policy to ask for patient ID as part of their registration process.
4.9.5 Any practice that requests documentation regarding a patient’s identity or immigration status must apply the same process for all patients requesting registration equally. Acceptable exceptions to this are outlined in 4.9.6 and 4.9.7. A practice policy should not routinely expect a patient to present a photograph as this could be discriminatory.
4.9.6 The majority of patients will not find it difficult to produce ID/residence documentation. However, there will be some patients who do live in the practice area but are legitimately unable to produce any of the listed documentation. Examples of this may be:
- people fleeing domestic abuse staying with friends, family or in a shelter
- people living on a boat, in unstable accommodation or street homeless
- people staying long term with friends but who are not receiving bills
- people working in exploitative situations whose employer has taken their documents
- people who have submitted their documents to the Home Office as part of an application
- people trafficked into the country who had their documents taken on arrival
- children born in the UK to parents without documentation
4.9.7 Reasonable exceptions therefore need to be considered and the individual registered with sensitivity to their situation.
4.9.8 As there is no requirement under the regulations for people to produce identity or residence information, the patient must be registered on application unless the practice has reasonable grounds to decline. The inability to produce identity or residence information would not be considered reasonable grounds to refuse to register a patient and neither should access to appointments be withheld in these circumstances. If a patient cannot produce any supportive documentation but states that they reside within the practice boundary, then practices should accept the registration.
4.9.9 Where necessary (for example, for patients experiencing homelessness), the practice may use the practice address to register them if they wish. Further, they could use an address which the local authority has provided to the patient to use. If possible, practices should try to ensure they have a way of contacting the patient if they need to (for example, to give test results).
4.9.10 If a practice suspects a patient of fraud (such as using fake ID), then they should register and treat the patient but hand the matter over to the NHS Counter Fraud Authority (NHSCFA):
- NHS Counter Fraud Authority Reporting Line: 0800 028 4060
- report to the NHSCFA using the online NHS fraud reporting tool
4.10 Refusing registration
4.10.1 Acceptable reasons for a practice declining a new patient registration request are described in 2.4.
4.10.2 Practices should not decline new patient registration requests because the patient has previously been removed from a practice under the 8-day removal process or where, following such an instance, the practice initiating the 8-day removal subsequently reported an incident to the police. The provisions for the removal of violent patients which do support the refusal of registration is on the grounds such patients would be managed in the Special Allocation Scheme. This position has been clarified in changes to the 2025/26 GP contract.
4.10.3 If a practice refuses any patient registration where acceptable reasons apply, they must record the name of patient and the date and reason for the refusal and write to the patient explaining why they have been refused, within a period of 14 days of the decision to refuse their registration.
4.10.4 This information should be made available to commissioners on request. Commissioners may ask practices to submit the numbers of registration refusals, age and ethnicity of the patients refused and the reasons as part of their quality assurance process.
4.11 Patients who are temporarily resident in a specialist hospital away from home
There has been some confusion in respect of GMS Regulations, part 5, Regulation 17(4).
4.11.1 This regulation does not provide ‘reasonable grounds’ to refuse registration with a practice according to legal advice. 17(4)(b) relates to patients who are already registered with the GP practice and cannot be used as a reason/justification for not registering certain patients. It only becomes relevant after a patient is registered.
4.11.2 There are no legal grounds for refusing to register a patient because they are an inpatient in a hospital. Indeed, the ‘gatekeeper’ role of the NHS GP for accessing secondary care services depends on patient registration.
4.11.3 Practices are not however expected to provide anything other than essential and minor surgery in these circumstances. If the resident requires any other services these must be arranged by the hospital or the commissioner. The commissioner that is responsible for securing specialist hospital services should ensure that all services over and above those normally associated with general practice are both agreed as part of the contract specification and actively monitored to ensure delivery against that specification.
4.11.4 A is provided to support GPs, commissioners and providers in clarifying the contractual requirements of primary care providers and those of the hospital, and the regulatory and professional obligations of the clinicians to ensure safe care. This includes examples that describe ‘shared care’ arrangements/responsibilities so that patients receive holistic care.
4.11.5 There are however instances where patients’ temporary residence is in a specialist hospital away from home. Where spells are for long periods of time, commissioners should consider establishing an integrated primary and specialist care offer for those patients to ensure their essential and additional primary medical service needs can be met more effectively. In those instances, the commissioner when securing specialist hospital services will want to ensure those services normally associated with general practice are agreed as part of the contract specification and actively monitored to ensure delivery against that specification. This will require use of the APMS contract ‘bolt-on’ available to the NHS standard contract.
4.12 Registering children
4.12.1 As a minimum requirement, the arrangements above in respect of the registration of any patient with a GP surgery should be followed when the person registering is a child. However, practices should be aware of the circumstances in which safeguarding guidance should be followed.
4.12.2 The legal definition of a child is 0 to 18 years of age; however, young people may be able to make independent decisions from as young as 13 years old, depending on their Gillick competency.
4.12.3 Section 11 of the Children Act 2004 places a statutory duty on the NHS to safeguard and promote the welfare of all children up to the age of 18 years. The Victoria Climbie Enquiry Report 2003 (9.104) stresses the importance of GP registration for every child. It sets out the importance of knowing the identity and name of those registering the child and their relationship to that child.
4.12.4 If a child under 16 attempts to register alone or with an adult who does not have parental responsibility, the practice child safeguarding lead should be alerted.
4.12.5 For purposes of safeguarding children, the following should be considered while recognising that patients must still be registered in the absence of documentation and policies must be applied in a non-discriminatory manner.
4.12.6 The practice should seek assurance through:
- proof of identity and address for every child, supported by official documentation such as a birth certificate (for example, this helps to identify children who may have been trafficked (see Modern slavery: statutory guidance for England and Wales (under section 49 of the Modern Slavery Act 2015) and non-statutory guidance for Scotland and Northern Ireland) or who are privately fostered (see Department for Education guidance on private fostering)
- an adult with parental responsibility should normally be registered at the practice with the child. There may be legitimate exceptions to this, such as where both parents are serving in the armed forces and are registered with an ‘armed forces’ GP, or practical explanations: for example, parents wishing for their child to be registered with a practice closer to school. The ID of the adult is essential as it can be matched to the birth certificate details. However, the practice should not refuse to register a child if there is no-one with parental responsibility who can register, as it is generally safer to register first and then seek advice from the practice child safeguarding lead, health visitor or practice manager (this situation may alert you to a private fostering arrangement which will require notification to the local authority)
- offering each child a new patient registration health check as soon as possible after registration
- proof of parental responsibility or relevant guardianship agreements
- seeking collaborative information (supported by official documentation) relating to:
- current carers and relationship to the child
- previous GP registration history
- whether the child is registered with a school and previous education history
- previous contact with other professionals such as health visitors and social workers
- regularly reviewing children who have been temporarily registered with the practice and proceeding to permanent registration as soon as possible and ideally within 3 months of temporary registration. Likely length of stay should be determined at initial registration and the patient registered as temporary/permanent as appropriate
- as children of parents or carers who have been removed from the list for any reason must not be left without access to primary care services:
- where parents or carers have been removed from the list due to aggressive and or violent behaviour, completing a risk assessment to identify any risk to their children and the appropriate referrals safeguarding made. Please ensure you consult relevant safeguarding procedures and record any referral decision
- taking a ‘think family’ approach when seeing either the adult(s) or child/children within the surgery. If you are aware that an adult has significant risk-taking behaviour, chronic mental health concerns or repeated episodes of stress and anxiety, safeguarding and support consideration should be given to the welfare and safety of the child/children being cared for by that adult
4.12.7 Practices should be alert to potential risks such as those described above when young people aged between 16 and18 years of age register alone. They should deal with these in line with practice safeguarding procedures and escalate outside the practice through local procedures if appropriate.16–18-year-olds are still children by law of child protection but can also be parents and carers. It is imperative that the risks and vulnerabilities within this age group are considered.
4.12.8 There is nothing to stop a parent de-registering their family and not registering again. It is not compulsory to be registered with a GP whether an adult or a child. To amend this there would need to be legislative change. Such legislation would encroach on areas of personal freedoms and patient and parental rights so would likely attract resistance. In addition, it is difficult to see how this could be enforced or police as there is no jurisdiction or levers to ensure that all children are registered.
4.12.9 If a practice is concerned about a family who is de-registering their children with no plan to register with another general practice, it needs to consider whether this should be raised with the local authority as part of normal safeguarding processes.
4.13 Registration of those previously registered with defence medical services and priority NHS care for veterans
4.13.1 Defence medical services (DMS) have their own GP services that look after serving personnel, mobilised reservists and some families. These specific primary care services are commissioned separately by the DMS of the Ministry of Defence. When servicemen and women leave the armed forces, their primary healthcare reverts to the responsibility of the local NHS. As a minimum requirement, the arrangements set out above in respect of the registration of any patient with a GP surgery should be followed when the person registering is a veteran. Prior service should be recorded on registration and allocated the correct read/SNOMED code. This should enable access to specialist or bespoke care or charity support as necessary for such patients and for the delivery of the armed forces covenant.
4.13.2 A veteran is an ex-service person or reservist who has served in the armed forces for at least 1 day. There are around 2 million of these veterans in England at the time of drafting.
4.13.3 All veterans are entitled to suffer no disadvantage from their service and to receive priority access to NHS hospital care for any condition that relates to their service (subject to clinical need), regardless of whether or not they receive a war pension.
4.13.4 All people leaving the armed forces are given a summary of their medical records, which they are advised to give to their new GP when they register. The practice will also normally be advised automatically of prior registration with DMS (with a summary of their in-service care).
4.14 Persons released from prisons, immigration centres or children’s secure facilities
4.14.1 NHS England introduced a contractual change in October 2017 to allow patients who will not be registered with a general practice on release or are being released to a different area to register with a practice before they leave the detained estate. This agreement includes the timely transfer of clinical information, with an emphasis on medication history and substance misuse management plans, to the practice from the detained estate healthcare service to enable better care when a new patient first presents at the practice.
4.14.2 Those in contact with the Criminal Justice System may get a letter from the Youth Offending Service, the Committee for the Right of the Child (CRC) or the National Probation Service.
4.15 Registering civil servants and their dependants and the dependants of members of the armed forces returning from overseas postings
4.15.1 Contractual changes in October 2021 enable civil servants who are posted overseas and their relevant family members (see 4.15.9 for the definition of ‘relevant family member’) who have accompanied them on their posting, and relevant family members who have accompanied a member of the armed forces (a ‘service person’) posted overseas, to register with a GP practice more easily. This includes as a permanent patient or temporary resident and in advance of (or on) their return to the UK. This is because these individuals have faced challenges registering and accessing primary medical services in a timely way when returning to the UK from overseas postings.
Registration with a patient’s previous practice or its successor
4.15.2 Where an application is made to a contractor by one of the following individuals, the contractor must accept them, even if their patient list is closed. (The only exception to this is where the contractor has reasonable grounds to refuse the application; see 4.15.8):
- civil servants returning to the UK from an overseas posting (or former civil servants who were posted overseas and are returning to the UK for the first time since leaving the civil service) – provided they were registered with that contractor or a predecessor contractor immediately before that posting or the first of consecutive postings. A ‘predecessor contractor’ is a contractor (‘A’) whose obligations to provide services have been partly or fully assumed by the contractor to which the application for registration is made. This will cover practice mergers, as well as where, in relation to a general medical services contract, there has been a change of status from individual medical practitioner to partnership (or vice versa)
- relevant family members of a civil servant (or former civil servant) who are returning to the UK and immediately before their return are or were accompanying the civil servant (or former civil servant) on their overseas posting – provided the civil servant (or former civil servant) was registered with the contractor or a predecessor contractor immediately before that overseas posting or the first of consecutive postings
- relevant family members of a current or former service person who are returning to the UK and who, immediately before their return to the UK, are or were accompanying the current or former service person on an overseas posting – provided the family member was registered with the contractor or a predecessor contractor immediately before accompanying the service person on that overseas posting or the first of consecutive postings
4.15.3 The application in 4.15.2 may be made from overseas up to 1 month before that individual’s planned date of return to the UK, and if the application is for permanent registration, it must be made no later than 3 months after the patient’s arrival in the UK. Applications for permanent registration made after the end of the 3-month period are to be dealt with in the same way as any other patient registration request.
Registration with a new practice
4.15.4 Where an application is made by one of the following individuals, the contractor must register them if their patient list is open. (The only exception to this is where the contractor has reasonable grounds to refuse the application; see 4.15.8):
- civil servants (or former civil servants) returning to the UK from an overseas posting who were not previously registered with the contractor or a predecessor contractor
- relevant family members who are returning to the UK and who:
- are or were accompanying a civil servant (or former civil servant) or a service person (or former service person) on their overseas posting from which they are returning; and
- are not required to be treated as previously registered with the contractor (see 4.15.2)
If the contractor’s list of patients is closed, it may register the individual if they are an immediate family member of a registered patient.
4.15.5 The application in 4.15.4 may be made from overseas up to 1 month before that individual’s planned date of return to the UK. If the application is for permanent registration, it must be made at least 24 hours before the planned return date. Applications for permanent registration which are made less than 24 hours before the planned return date or after the individual returns to the UK are to be dealt with in the same way as any other patient registration request.
4.15.6 Applications in 4.15.2 and 4.15.4 may be made in-person or remotely to the contactor: for example, via posting or emailing a signed printed or scanned PRF1 (formerly GMS1) form or the practices local temporary registration form (commonly referred to as a GMS3 form) as relevant. The form should be sent to the contractor with the following additional information:
- confirmation the patient is seeking registration under the contract provisions for crown servants returning from overseas postings
- the patient’s planned date of arrival in the UK
- anticipated length of stay in the UK (if not permanent and if known)
- a list of all relevant family members (where applicable)
- proof of being or having been overseas in the circumstances defined in 4.15.2 and 4.15.4. This would normally be some documentary evidence or cover letter from the employer of the current or former civil servant/service person
4.15.7 Should the practice need to validate that a patient was previously registered with them (or their predecessor contractor) immediately before they went overseas, the practice may confirm this through the PDS/PCRM.
4.15.8 If the practice cannot confirm prior registration with it, it may request proof from the patient: for example, letter, email, text message. If neither the practice nor the patient is able to evidence prior registration, the practice may still choose to accept the individual’s application if it is nevertheless satisfied that it or the patient to which they are a relevant family member (as the case may be) was previously registered with the practice (or its predecessor contractor) – for example, a practice may see proof of an individual being previously resident in that practice’s area as sufficient to accept their application.
Date of registration and duty to provide care
4.15.9 Where a contractor accepts an application in 4.15.2 or 4.15.4 for:
- temporary registration, it must confirm this with the individual or the appropriate person. The contractor’s responsibility for that individual begins on the later of: (a) the date on which the contractor accepts the application, and (b) the date on which the individual returns to the UK. The contractor must notify its commissioner that it accepted the individual as a temporary resident at the end of the contractor’s period of responsibility for that individual
- permanent registration, the contractor must give notice in writing to its commissioner of that acceptance as soon as possible. If the application is accepted before the individual’s planned return date, the contractor must notify the commissioner of that return date. The commissioner must add the individual to the contractor’s list of patients from the later of: (a) the date on which the commissioner receives the relevant notice from the contractor, and (b) the date on which the individual returns to the UK. The contractor is not required to provide primary medical services to that individual before their actual return to the UK
Once a contractor has accepted an application, regardless of whether the individual is still overseas, the contractor may book on request appointment(s) for that individual which are only to take place once the individual has arrived in the UK. Individuals must not attend appointments (that is, remote appointments) with the contractor while they are still overseas.
4.15.10 A contractor may only refuse to register individuals in 4.15.2 under the Crown servant registration provisions where it has reasonable grounds for doing so. Such grounds must not relate to the patient’s race, gender or gender reassignment, marriage or civil partnership, pregnancy or maternity, social class, age, religion or belief, sexual orientation, appearance, disability or medical condition. Reasonable grounds may include, in the case of an application for permanent registration, that the patient does not live or intend to live in the contractor’s practice area or the outer boundary area. Where a contractor refuses to register a patient, this decision and the reasons for it must be communicated to the patient (or the person who made the application on their behalf) in writing within 14 days of that decision being made. The contractor must keep a written record of applications and reasons for refusal.
4.15.11 Under the contract regulations [see Note 1 below], the following are relevant family members of a current or former civil servant/service person:
- their children (adopted and stepchildren as well as natural children), if:
- they are or were at the time of leaving the UK to accompany the civil servant or service person on their overseas posting, under 21 (or under 25 in the case of the child of a service person) and wholly or mainly financially dependent on the civil servant or service person while accompanying them; or
- they are or were wholly or mainly financially dependent on the civil servant or service person while accompanying them on their posting because of a disability [see Note 2 below]
- their spouse, civil partner or individual whose relationship with the current or former civil servant or service person has the characteristics of a relationship between spouses or civil partners
- their former spouse, civil partner or individual whose relationship with the current or former civil servant or service person has ended (for any reason) but had the characteristics of a relationship between spouses or civil partners
- their widow/widower or surviving civil partner if the civil servant or service person passed away while on their posting
Individuals who become relevant family members of a current or former civil servant/service person during an overseas posting and are returning to the UK are to be treated in the same way as those who were family members before the start of such a posting. This includes, for example, a child born or adopted during an overseas posting who remains with their civil service parent throughout that posting, or a person who marries a civil servant during their overseas posting and accompanies that person on their posting from that time.
Note 1: See the definition of “relevant family member” in paragraph 32A(7) of Schedule 3 to the National Health Service (General Medical Services Contracts) Regulations 2015 and in paragraph 31A of Schedule 2 to the National Health Service (Personal Medical Services Agreements) Regulations 2015. These provisions were inserted by the National Health Service (General Medical Services Contracts and Personal Medical Services Agreements) (Amendment) (No. 2) Regulations 2021.
Note 2: As defined in part 2, chapter 1, section 6 of the Equality Act 2010.
4.16 Armed forces: dual registration and the GP contract
4.16.1 Under the terms of their primary medical services, general practices have the ability to register members of the armed forces of the Crown for a period of up to 2 years. To be eligible for registration, the patient must obtain written authorisation from the defence medical services and must reside or work within the practice area during the specified time period mentioned in the authorisation.
4.16.2 The arrangements for including armed forces personnel on a contractor’s patient list are outlined in clause 13.5A of the GMS contract. You can find the latest version of the contract, which includes this clause (page 71), on the NHS England website. The same clause is included in the 2015/16 GMS contract (page 67). The corresponding regulations can be found in the Schedule 3, paragraph 19 of the GMS Regulations 2015.
4.17 Temporary residents
4.17.1 A contractor may, if the contractor’s list of patients is open, accept a person as a temporary resident. This is provided the contractor is satisfied that the person is temporarily resident away from their normal place of residence and is not being provided with essential services (or their equivalent) under any other arrangement in the locality where that person is temporarily residing; or moving from place to place and not resident in any place for the time being.
4.17.2 It is of note that a notification to the commissioner of the acceptance of a temporary resident on to the contractor’s list only occurs at the end of the period of 3 months from the date on which the contractor accepted that person as a temporary resident; or, if the contractor’s responsibility for that person as a temporary resident came to an end earlier, at that point. Any clinical records relating to the temporary registration period of care can/should be submitted via PCSE for repatriation to the registered GP practice or storage in archive.
4.17.3 As this type of registration is not submitted to PCSE via GP Links at the commencement of the temporary registration, there is potential for a contractor to accept as a temporary resident a patient who is actively registered with a Special Allocation Scheme (SAS). Should a contractor become aware that a patient is registered with an SAS, it should contact its local commissioner. The commissioner may seek to secure temporary primary medical services for the patient with a local SAS.
4.18 Sensitive patient registrations
4.18.1 GP practices are required to work with PCSE and take actions on their clinical systems to ensure that the registration information for patients who change their identity is accurate and up to date. This is also the case for adoptions, gender transition and patients in witness protection schemes. This ensures that data, as well as being kept up to date, is held in line with information governance requirements on national demographics systems.
4.18.2 Commissioners must also work with PCSE in relation to managing escalations where there are potential blockages or delays in practices responding to PCSE requests.
5. Temporary suspension to patient registration
5.1 Formal list closure
5.1.1 The GMS contract and PMS agreements allow for a practice to request permission from its commissioner to close its list to new patients (Schedule 3, Part 2, paragraph 33 of the NHS [GMS contracts] Regulations 2015). This option exists to give practices a degree of workload control over the management of their services, particularly when there is unusual and sustained demand from patients or in situations of workforce or recruitment difficulties that affect a practices ability to provide services to an acceptable and safe standard.
5.1.2 As the commissioner also has a duty to ensure the availability of primary care services for the resident population, it has certain powers with regard to these requests including agreeing to the length of the closure and the conditions that would need to exist to trigger a re-opening of the list. The commissioner will also need to consider the availability of alternative provision for new patients and any impact on neighbouring practices. Following changes to the formal list closure process in 2012, the commissioner does not have the power to halt a practice’s delivery of additional and/or enhanced services as a means to reduce practice workload and thereby keep the patient list open.
5.1.3 When a practice does formally close its list, the requirement is to close for between 3 and 12 months; not less than 3 months. An approved closure notice must specify the time period.
5.2 “Informal” or “temporary” list closure
5.2.1 While GMS contracts and PMS agreements do not allow for a ‘temporary’ or ‘informal’ list closure, they do allow for a practice to refuse individual patient applications for inclusion in a contractor’s list of patients providing there are reasonable non-discriminatory grounds to do so (GMS Regulations: Schedule 3, Part 2, paragraph 21). In this guidance we distinguish a patient refusal on a case-by-case basis, based on the patient circumstances, from a refusal to allow a patient to join the list because of the circumstances surrounding the provider and so do not consider paragraph 21 to be appropriate in these circumstances.
5.2.2 Practices can, however, suffer unforeseen pressures that can reasonably be predicted to be short term. In these circumstances there may be a real or perceived risk to ‘safe patient care’ from accepting more new patients on to the list and action to address this by the practice should be received by the commissioner as a trigger for support.
5.2.3 NHS England has seen a significant rise in the number of practices suspending registration on a temporary basis, causing a significant problem for patients, neighbouring practices and commissioners in some areas.
5.2.4 Practices do not exist in isolation. When a practice restricts new patient registration, this has an impact not only on patients but also on neighbouring practices. The formal list closure procedure exists for this type of circumstance; to allow for a considered and managed approach to list management across all practices.
5.2.5 Because of the potential impact of ‘temporary suspension’, NHS England encourages practices to open a dialogue with their commissioner as early as possible when considering temporary suspension.
5.2.6 These guidelines for commissioners describe the circumstances where a temporary suspension by the contractor of patient registration may be appropriate and the conditions that should govern that decision such that the roles and responsibilities of both parties are not compromised.
5.3 Overview of current activity
5.3.1 The increase in a temporary suspension of patient registration is a symptom of rising pressure in primary care, which creates a risk to patients, neighbouring practices and the commissioner; however, the risk to patients being registered with an oversubscribed practice should also be considered.
5.4 Facts/principles
5.4.1 Addressing practices seeking to ‘informally’ or ‘temporarily’ suspend patient registration on to their list should be in the context of NHS England and commissioners commitments to supporting practices in difficulty.
5.4.2 However, NHS England has a duty to ensure that patients have access to primary care where:
- a core service by the fact of regulation is operating an open list and this is how NHS England ensures access to services; the NHS Act confers a duty on the commissioner to ensure the provision of services
- any actions considered by the commissioner should ensure, system-wide, safe, quality and accessible core services to patients and be proportionate and sensitive to the providers concerned
- NHS England and commissioners have a responsibility to address health inequalities
- commissioners and providers must work together to ensure compliance with the Equality Act, ensuring the rights of those with protected characteristics are not directly or indirectly compromised
- good medical practice states that if a GP is aware that patient safety is being compromised, then they have a professional duty to act
- the unintended impact of any action needs to be considered in relation to both registered patients and unregistered patients in the locality as well as the impact on other local providers of both primary (GP and pharmacy) and secondary care
5.4.3 The commissioner has the right to assign patients throughout the period that the list is not formally closed having due regard to the quality and safety of services and the reasons behind the list closure in the first place.
5.5 Issues to be taken into consideration
5.5.1 NHS England acknowledges that things can rapidly change within practices. These may include:
- an immediate and unpredicted shortfall in the availability of staff: for example, through sickness or a delay to a staff appointment
- an unpredicted surge in demand
- an unexpected event affecting a practice’s ability in the short term to provide the full range of services normally available: for example, a flood or a fire (see force majeure provisions of the standard GMS contract, PMS agreement and APMS contract)
- impact on a practice of an unfavourable CQC inspection where remedial action temporarily affects normal service provision
5.5.2 In some circumstances the action required to remedy a problem may take several months and in others just a few weeks: for example, a planned short-term suspension of registration as part of a recovery plan. Alternatively, practice capacity may be temporarily compromised by premises development or IT upgrades. Under these circumstances, it would be usual to expect planning and communication with patients in advance, with a specific start and end date and disruption measured in weeks not months.
5.5.3 In all but exceptional circumstances, practices should approach the commissioner in advance so that an action plan that minimises the impact on patients can be considered jointly at the earliest opportunity and the commissioner can provide immediate support. A request to temporarily suspend patient registration should be considered by the commissioner as a trigger for support as should a formal application to close the list.
5.5.4 This guidance does not prescribe the length of time that it is appropriate to approve a temporary list suspension for as this will vary depending on the circumstances. The key words are unpredictable and/or short term. In circumstances where there is a known history of difficulty in recruitment, including the availability of locums, or the circumstances affecting the practice can be predicted to last longer – for example, a planned refurbishment or a rebuilding programme scheduled to last months, say following a flood or a fire – the formal list closure procedure should be encouraged.
5.5.6 In both cases (request to temporarily suspend or formally close the list) the practice’s eligibility and need for resilience support should be considered by the commissioner.
Circumstances in which an ‘informal’ or ‘temporary’ list closure is not appropriate are (list is not exhaustive):
- the practice considers its list is full (a formal application should be made)
- long-term sickness absence (a formal application should be made)
- issues expected to be longer term: for example, over 3 months
- a formal closure application has been declined
5.6 Process to be adopted
5.6.1 All practices should be encouraged to contact their commissioner at the earliest possible opportunity; that is, at the point that suspension to registration is being considered so that the provider and commissioner can work together to agree what support is required.
5.6.2 At this point commissioners should:
- seek to understand the reasons behind the action
- engage the LMC at the time of a decision as the LMC also carries a responsibility for representing all its affected parties
- facilitate action to be taken by the practice and/or commissioner for the list to be re-opened. If actions can reasonably be expected to take longer than 3 months, the practice should be asked to make a formal application to close its list
5.6.3 Actions should trigger consideration of the general practice resilience programme or use of section 96: for example, a diagnostic/review of the difficulties faced and recommended action.
5.6.4 At the end of the agreed period of temporary suspension of patient registration, the list would normally re-open. There are only 2 alternative outcomes:
- if the situation is almost resolved – for example, an appointment has been made but the post will not be filled for another week or two – an extension to the temporary arrangement can be negotiated
- despite support to deliver an action plan the practice continues to feel compromised. The commissioner should then consider an application for formal list closure, which will require wider consultation. The parties will need to agree the status of the practice list during the formal process – that is, whether, having regard to all local circumstances, the practice should continue to operate a temporary suspension to patient registration
5.6.5 These guidelines have been drafted in recognition of the immediate pressures facing some practices; they do not however sanction the term ‘open but full’. Where a practice is failing to engage with the commissioner and unilaterally seeking to determine its own restrictions on patient access, without consideration of the impact on patient access generally or the implications for neighbouring practices, then contractual action may need to be considered.
6. Managing [non-violent] patient behaviours which lead to removals from the list at the request of the contractor including protecting against discrimination, harassment or victimisation
6.1 Introduction
This chapter supplements and should be read alongside the guidance in chapter 3: Managing patient lists and chapter 7: Managing violent patients – Special Allocation Scheme, to support the management of behaviours which challenge healthcare staff, including inappropriate and unacceptable patient behaviours and behaviours evolving from distress or sensory challenges, and to protect practice teams and other patients from discrimination, harassment or victimisation.
Providers should use the violence prevention and reduction (VPR) standard (2024) as a framework. This includes a high-level assessment and improvement action plan to support this.
All NHS organisations have a legal duty to prevent violence in their workspaces. They can do so by identifying and preventing the escalation of distressed behaviour and promptly responding to abusive behaviour. Organisations should have a designated member of staff of an appropriate leadership level and with relevant training to take on the responsibilities of violence prevention and reduction.
6.2 Key areas
Given the importance of the interests this guidance seeks to balance, ensuring that circumstances which lead to removals from the list at the request of the contractor are appropriately managed, while ensuring all patients are able to access primary medical services they need and are entitled to, this guidance covers the following key areas:
- the scope of inappropriate and unacceptable patient behaviours
- contract regulations relating to the removal from the list at the request of the contractor
- considerations for ensuring ongoing access for patients
6.3 The scope of inappropriate and unacceptable patient behaviours
6.3.1 Many practices operate local policies to support positive behaviours between staff and patients, fostering a culture of mutual respect and psychological safety, such as respect policies and violence prevention and reduction policies, through patient and staff charters.
Non-violent behaviours which may lead to removal from the list at the request of the contractor may include but are not limited to:
- using offensive language or swearing at practice staff or other service users
- racial abuse
- sexual harassment
- unnecessarily persistent or unrealistic service demands that cause disruption
- causing damage to practice premises or to the property of staff or other service users
- stealing from practice premises, staff or other service users
- obtaining drugs and/or medical services fraudulently
Under usual circumstances, patients must not be immediately removed from a practice list for minor offences not reported to the police or behaviour that was not appropriate to report to the police: for example, a patient who has never been aggressive before and/or who is suffering mental or physical distress. In such circumstances, it will be appropriate to use the standard procedure for a breakdown in practice/patient relationship and explaining that the continuation of these behaviours may result in the patient being removed from the practice list, for the health and safety of other patients and staff.
Usually this is undertaken by writing to the patient requesting an explanation or apology and warning that a continuation of such behaviour could result in them being removed from the practice’s list. Practices may also choose to use or agree on a good behaviour contract with the patient to support their continued registration. Providers may also choose to use or agree on a mutual behaviour contract between the provider and the patient to support their continued registration.
6.3.2 Violence and threatening abuse are dealt with separately in chapter 7: but it is acknowledged the behaviours above can escalate to include or happen alongside violence and abuse.
6.3.3 Common to all such policies should be the underlying principles and values set out in the NHS Constitution which bind together the communities and patients the NHS serves and the people who work in it. Everyone has a right to be treated fairly and equally, with dignity and respect and free from discrimination, harassment, violence and abuse. There are extensive legal rights, embodied in general employment and discrimination law.
6.3.4 The protection and safety of the provider’s teams (and other service users) mental wellbeing is as important as the protection and safety of their physical safety. NHS England supports and requests that providers should review existing policies using the NHS violence prevention and reduction (VPR) standard as a framework, to ensure incidents of discrimination, harassment or victimisation are recorded accurately. Where a crime has been committed, this should be reported to the police. This data should inform development of interventions to protect staff from harm and appropriate health and wellbeing support offers to staff who have been affected. The following definitions may be useful:
- discrimination: the act of being treated unfairly because of who they are or because they possess certain characteristics. Within the Equality Act 2010 the following are protected characteristics:
- age
- gender reassignment
- being married or in a civil partnership
- being pregnant or on maternity leave
- disability
- race including colour, nationality, ethnic or national origin
- religion or belief
- sex
- sexual orientation
- harassment: the act of being subject to unwanted behaviour, which is offensive, intimidating or humiliating. Harassment can happen on its own or alongside other forms of discrimination
- victimisation: the action of being singled out for cruel or unjust treatment
- microaggressions: verbal, non-verbal and environmental slights, snubs and insults which communicate hostile, derogatory or negative messages and behaviours that target a person based on their protected characteristic or belonging to a marginalised group. These can be intentional and unintentional and are based on biases (either conscious or unconscious)
6.4 Contract regulations relating to removal at the request of the contractor
6.4.1 Where a provider wishes to remove a patient from its practice patient list, removal may normally only be requested if, within the period of 12 months prior to the date of the request, the provider has warned the patient in writing that they are at risk of removal and reasons for this have been stated. However, the contract regulations also acknowledge that it may be justified that a written warning was not possible/appropriate in the circumstances that such a warning:
- would be harmful to the person’s physical or mental health
- would put at risk the safety of one or more relevant person(s)
- the contractor considers that it is not otherwise reasonable or practical for a warning to be given
Practices should be aware of the guidance in the VPR standard which encourages identifying root cause of behaviour and seeking to mitigate where possible.
6.4.2 The General Medical Council states in Ending your professional relationship with a patient – professional standards that: “In rare circumstances, the trust between you and a patient means you can’t continue to provide them with good clinical care. This might occur when a patient has, for example:
- been violent, abusive, or made threats to you or a colleague
- displayed other criminal behaviour, such as stealing from you or the premises
- acted in a sexual way towards you
- persistently acted unreasonably
6.4.3 Removing a patient from the practice patient list, including without prior written notice under reasonable grounds or grounds of irrevocable breakdown in the relationship, is expected to be an exceptional event.
6.4.4 Providers will also recognise that in incidents of patient behaviour which challenge healthcare staff, including inappropriate and unacceptable behaviours, the patient’s mental health, clinical presentation, neurodiversity and any other health conditions which may influence their behaviour will need to be taken into account. They will also need to ensure that the patient’s own protected characteristics have no bearing on the consideration process.
6.5 Process for managing behaviour which challenges healthcare staff, including inappropriate and unacceptable behaviours
6.5.1 Where a patient has behaved inappropriately or unacceptably, the provider will need to carefully consider (taking account of the nature and severity of the incident/behaviour, the impact on practice services, staff or other service users and the patient’s own circumstances) if the incident:
- meets the relevant criteria for removal of the patient from the practice patient list and, if so, if it is nevertheless willing to continue to manage its relationship with the patient or proceed with the removal
- does not meet the relevant criteria for removal from the practice patient list and how it will manage its continuing relationship with the patient
6.5.2 The stated consequences of stepping outside the provider’s practice polices of expected patient behaviours need to be things that the practice can and will carry out. The process for removing patients from the practice list on reasonable grounds is described in chapter 3: Managing patient lists and the process for removing violent patients is described in chapter 7: : Managing violent patients – Special Allocation Scheme.
6.5.3 The British Medical Association General Practitioner Committee acknowledges “many patients who are misusing services can change their behaviour if it is brought to their attention”.
6.5.4 Following the NHS VPR standard, providers are encouraged to explore route causes and attempt to mediate the relationship between the provider and patient. A warning letter can provide such an opportunity and where used should indicate continued registration will cease if the inappropriate or unacceptable behaviour continues or reoccurs and therefore formally documents and evidence reasonable grounds for future removal should it do so. Annex 20 provides a template warning letter.
6.5.5 A mutual behaviour contract (otherwise known as practice-patient or doctor-patient contracts) can also be a useful tool to bring about a mutual respect between the patient and practice and should be considered as either an intervention before, a follow up, or used alongside a warning letter. The agreed terms set out in the agreement need to be reasonable in line with the providers practice policies and any specific interventions linked to the individual case (use of ‘cooling off’ periods, quiet rooms to wait for an appointment, meeting communication needs, being supported by a social/support worker) should be fair and not excessively burdensome or disproportionate to the risk. Annex 21 provides a template mutual behaviour guidance agreement.
6.6 Considerations for ensuring ongoing access for patients removed from a practice patient list due to inappropriate and unacceptable behaviours
6.6.1 Other than on the grounds of violence or threatening behaviour, the grounds a patient has been removed from a practice patient list should not ordinarily be a factor to be considered by practices when approached by new patients.
6.6.2 Additionally, where a patient has been removed from a practice list and subsequently not been able to register with a new practice, commissioners may need to assign the patient to a practice with an open patient list. Where patient assignment to a practice list is required’, section 3.2: Part A: managing patient assignments is clear about the considerations that commissioners should take into account.
6.6.3 It is recognised that some patients can fall into routine cycles of being removed and re-registered. Commissioners should consider how the needs of such patients may be best met and the support providers may need locally to ensure such cycles are broken, in the interests of both providers and such patients.
7. Managing violent patients – Special Allocation Scheme
For information only: other terminology previously used in relation to special allocations of this type includes but is not limited to Violent Patient Scheme (VPS) or Zero Tolerance Scheme.
7.1 Executive summary and key messages
This chapter provides guidance to commissioners and providers of essential primary medical services in relation to the removal of patients who are violent from their practice list. The Special Allocation Scheme (SAS) intends to ensure such patients can continue to receive primary medical services. Provision for SAS is set out in the National Health Service (General Medical Services Contracts) Regulations 2015 and the National Health Service (Personal Medical Services Agreements) Regulations 2015 (together the regulations).
This guidance focuses on several key themes which are intended to support the implementation, commissioning and monitoring of a SAS:
- provider and service requirements and monitoring
- scope of/eligibility criteria for an SAS
- process for requesting immediate removal of a patient
- what happens after removal, including returning choice to patient
Given the importance of the interests that SAS seeks to balance, 2 messages are emphasised at the outset.
The first relates to the scope of the SAS. The regulations regarding the removal of patients who are violent is specific in terminology and they require that GMS contracts and PMS agreements provide for “removal from the list of patients who are violent”.
However, the regulations further specify that the grounds on which a contractor may request that a person be removed from its list of patients with immediate effect are that “the person has committed an act of violence against any of the persons specified in sub-paragraph (2) or has behaved in such a way that any of those persons has feared for their safety“.
The commissioner should therefore be clear that violence does not have to be physical or actual. It can be perceived, threatened or indeed a perceived threat of violence. A person’s fear for their safety can also be actual or perceived. In these circumstances, the regulations specify that a practice can request the immediate removal of that patient from its list. Commissioners should also consider the need to place patients on the SAS.
In the case of requests for the immediate removal of patients whose behaviour is disruptive but falls short of the above grounds, commissioners should discuss with the practice if the patient should instead be removed from the practice on the alternative ground of irrevocable breakdown in the relationship between the person and the contractor (see Schedule 3, Part 2, paragraph 24 of the GMS Regulations and Schedule 2, Part 2, paragraph 23 of the PMS Regulations.
Refer to section 3.2: Part A: managing patient assignments (sub-section: removing a patient from a practice list) and chapter 6: Managing [non-violent] patient behaviours which lead to removals from the list at the request of the contractor.
The second key message is that we want all providers to understand the process for immediate removal of a patient, where a patient’s behaviour is deemed within the scope of this SAS chapter.
The regulations require that, for a patient to be immediately removed from a practice list, the practice must report the incident to the police.
The following 14-point process is designed to work in all but very exceptional circumstances. Those infrequent and exceptional cases relate solely to commissioner instigated allocations (for example, a patient who could fall within the remit of a SAS allocation but has not recently been removed from a GP practice list) and must be discussed and agreed with the commissioner and the patient in advance.
1. The practice calls the police to report the incident (as required under the regulations), obtain a response (if required) and police incident number. Where possible the police incident number should be provided at the time of reporting the incident. It must be included in the written report provided by the practice within 7 days (a contractual requirement under ‘reasonable requests for information’). If a practice is not able to include the police incident number at the time of the initial referral to PCSE, this can be followed up by the practice emailing this as an addendum to PCSE.
Note: practices should be reminded of the statutory requirement to notify the CQC about any incident related to their service that is reported to or investigated by the police.
Furthermore, where appropriate, the practice should consider if the incident and subsequent patient removal from its list warrants notification to any other agency (for example, local authority) where there may be concern for welfare or safeguarding because of the incident (that is, the deducted patient has children or is a carer for another vulnerable person including elderly relatives).
2. Having assured itself that the removal is not as a result of the patient’s protected characteristics and key past medical history, including mental health, a learning disability and neurodiversity, the practice requests an immediate removal from NHS England’s Primary Care Support England (PCSE) service provided by Capita. Ideally this request should be made by completing the Patient Removals | PCSE online form. If there are any difficulties in using the online form, practices can email patientremovals@nhs.net attaching the form or by phone 0333 014 2884.
PCSE will request the police incident number. [Note: this is different from a crime reference number, which can only be allocated by the police once it has been established that a crime has been committed. The police will however record an incident number on police systems for all incidents according to If the practice does not have a police incident number at this point (which should be in exceptional circumstances only), the practice will be asked to provide details of the date, time and mechanism (for example, 999, 111, local number) via which the incident was reported to the police. The absence of an incident number will not delay the immediate removal of a patient. However, practices should inform PCSE by email when the incident number is known. In the circumstances where a patient is homeless or of no fixed abode, the copy of the letter is sent by PCSE to the removing practice and SAS provider so it can be provided by them. ** Practice and PCSE actions **
3. PCSE removes the patient from the practice list and informs the appropriate commissioner. ** PCSE action **
4. The regulations require that the practice notifies the patient in writing that a request for removal has been made, unless to do so would harm the patient’s physical or mental health or put others on the practice premises at risk. ** Practice action **
5. PCSE allocates the patient to an appropriate SAS provider. Commissioners are responsible for commissioning SAS either from GPs or another provider. ** PCSE action **
6. PCSE notifies the patient in writing by first class that they have been removed from the practice list (as per the regulations (Schedule 3, Part 2 patients: general, regulation 25(7) of the GMS Regulations or Schedule 2 other required terms, Part 2 patients: general, regulation 24(7) removal from the list of patients who are violent of the PMS Regulations) and allocated to the SAS provider. Annex 22 provides a standardised patient communication from PCSE. ** PCSE action **
7. The practice provides a follow-up report in writing to the commissioner (refer to number 2 above; annex 23: PCSE request for removal of patient from practice list form) within 24 hours where possible but before the end of a period of 7 days from the date on which notice was given. Where the practice was unable to provide a police incident number initially; the practice will be asked to include this in the report (under the contractual requirement for reasonable requests for information). ** Practice action **
8. Following 7 days from the incident, the commissioner and PCSE will liaise to ensure an incident number has been received (either by PCSE or via the written practice report to the commissioner). In the event an incident number has not been provided, the commissioner will contact the practice to ensure one has been obtained and provided. ** Commissioner action **
9. The SAS provider will provide all new allocated patients with a welcome letter. ** SAS provider action **
10. As part of the new patient assessment, the SAS provider must be commissioned to undertake and embed initial appropriate assessment, referring to the commissioner any case where the SAS provider believes the referral may be inappropriate. The commissioner should discuss the referral with the referring provider and support patients who have not been accepted onto the SAS to find an alternative primary medical service provider. Note: initial appropriateness assessments should be part of all newly commissioned SAS services and where possible commissioners should seek to make arrangements – for example, as part of contract review processes – to add these to existing service contracts.
11. The SAS provider will ensure risk assessment and regular monitoring including rehabilitation of the patient’s behaviour which triggered the removal and allocation to the SAS, together with any other behaviours or areas of concern identified through risk assessments and regular monitoring. This is to enable the patient to be repatriated back into mainstream GP practice (primary care) as soon as is reasonable to do so. ** SAS provider action **
Note: commissioners should ensure the SAS provider’s initial risk assessment of a new patient includes:
- a level of security and safety measures required
- patient care plan
- assessment of the patient’s rehabilitation needs to enable discharge from the SAS
- travel needs of the patient
- safeguarding considerations
Annex 24 provides a sample risk assessment form.
Depending on the needs of the patient, rehabilitation options could include counselling, anger management, drug and alcohol interventions and other local initiatives or pilot programmes on rehabilitation.
The following e-learning modules can help staff to handle difficult conversations with compassion:
- handling difficult situations with compassion
- handling difficult situations – caring for yourself and others with compassion
The patient’s risk assessment should be continually reviewed and updated after each patient encounter with the SAS provider with the aim of returning choice to the patient where safe to do so.
12. The SAS provider will notify PCSE via email when choice has been returned to the patient and they have been removed from the SAS. This will ensure the patient’s records are amended accordingly by PCSE (that is, flag removed from patient record), allowing the patient to re-register at their chosen practice. ** SAS provider and PCSE action **
13. Where a commissioner considers that its existing SAS provider(s) is unable to meet the exceptional needs of a patient allocated to it, it may be necessary to commission a bespoke service for the patient.
14. Where a patient on the SAS moves address and between commissioning areas and a change in SAS provider is required, the previous SAS provider must notify PCSE and ensure a safe transfer (for example, by secure email) of an electronic summary of the patient record to the new SAS provider as soon as possible but not later than 5 days following deduction, to ensure continuity of care while the new provider awaits the transfer of the patient’s full medical records.
7.2 Introduction
Purpose of this document
7.2.1 In response to concerns of increasing abuse towards primary care staff following the second wave of the Covid-19 pandemic, the NHS England primary medical services policy and guidance manual (PGM) was previously updated to support further consistency of service delivery.
7.2.2 There will undoubtedly be instances when practices manage behaviours from patients which challenge healthcare staff, including aggression, abuse and in some cases violence. To support the health and wellbeing of GPs and practice staff and to allow them to carry out their roles, commissioners, in collaboration with the wider stakeholders, have developed this guidance.
7.2.3 Under the SAS, designated GP practices or another provider will provide services to patients by prior appointment and at specific locations and times as detailed in individually agreed contracts. Patients are allocated to SAS following a process of immediate removal because of an incident that was reported to the police.
7.2.4 The purpose of this document is to provide commissioners with consistent national guidance to support good commissioning of SAS. It provides a steer on the implementation of SAS in practice and how to work with PCSE, which is delivered on behalf of NHS England by Capita. Refer to section 7.3: Commissioning a robust SAS.
Background to this work
7.2.5 The SAS [originally known as the Violent Patient Scheme (VPS) and still referred to in the Directions as the VPS) was introduced as a Directed Enhanced Service in 2004. Its aim is to provide a secure environment to patients who have been removed from their GP practice and allocated to the SAS so they can continue to receive primary medical services. The SAS cannot be used in any other circumstances without the express and prior agreement of the commissioner.
7.2.6 The SAS allows commissioners to balance the rights of patients to receive primary medical services from the SAS provider to ensure that specified persons, including GPs, their staff, patients, and others on the premises, deliver and receive those services without actual or threatened violence or other reasonable fear for their safety.
7.2.7 Removing a patient under the regulations should be a rare event and used as set out in this section. Refer also to chapter 3: Managing patient lists and chapter 6: Managing [non-violent] patient behaviours which challenges healthcare staff, including protecting against discrimination, harassment or victimisation.
Existing arrangements
7.2.8 The administrative arrangements of the existing SAS across England have been disparate and varied. This has created challenges when trying to apply the regulations consistently and for the practical application of SAS through a single delivery partner (PCSE).
Particular issues
7.2.9 First, the regulations provide for immediate removal of a patient from a practice list following a phone call from the practice, yet some SAS services require commissioner intervention of some sort before a removal is actioned. This is outside the provisions as set out in the regulations.
7.2.10 Second, the regulations require a practice to report an incident to the police but do not mandate the acquisition of a police incident number or crime number before a removal is actioned. NHS England’s stakeholders [including the BMA’s General Practitioners Committee (GPC)] acknowledge that the provision of an incident number (but not a crime number) is a ‘reasonable request for information’ in accordance with the contract. However, an incident number should not be a prerequisite to the immediate removal of a patient whose behaviour is such that they meet the criteria for removal.
7.3 Commissioning a robust SAS
7.3.1 Commissioners should ensure all commissioned SAS services (new and existing) have:
7.3.2 An equality and health inequality impact assessment (EHIA) , which includes consideration of increased travel distances and potential mitigations such as contribution to travel cost, patient transport and/or mobile outreach services (safety risk assessment supporting). The key point is that the commissioner can show (through documentation, principally an EHIA) that the impact a decision will have on health inequalities has been considered and that its decision is based on relevant data and evidence. Refer to part A, chapter 2: General duties of NHS England (including addressing health inequalities) for more information.
7.3.3 Access to services including by telephone, online and face to face.
7.3.4 Pathways to support equitable access needs when patients are managed by a SAS provider out of area: for example, access to PCN services, referral to diagnostic services, maternity and district nursing.
7.3.5 A comprehensive discharge summary in place and completed after a final risk assessment with the patient. This should be saved in the patient’s medical record, ensuring that it is made available to the receiving practice. The discharge summary should include information on any outstanding referrals in progress and consideration of the provision of prescription medication in the interval before the patient registers with a mainstream GP practice (normally 3–4 weeks’ supply).
7.3.6 Arrangements requiring SAS provider to have access to or arrange enhanced security if risk assessment identifies the need.
7.3.7 Arrangements requiring SAS provider to have local information sharing in place where a risk assessment identifies a risk to other staff – that is, out of hours, community pharmacy.
7.3.8 We encourage SAS providers to establish a community of practice support network, linking with other SAS providers and prison medical services in local areas.
7.4 When to request a removal of this type under the regulations (information on eligibility for commissioners and providers)
7.4.1 It is important that these regulations are not misused or used lightly. Their use should be reserved for those patients who meet the criteria for removal and for whom an incident has been reported to the police and for patients who are deemed a future safety risk to themselves or others within the primary care setting.
7.4.2 It is not the intention to encourage a situation where patients are immediately removed for comparatively minor offences (for example, those that have not been reported to the police) or for behaviour that could be ascribed to a health condition and which can be alleviated through careful management, care and treatment. Refer to chapter 6: Managing [non-violent] patient behaviours which lead to removals from the list at the request of the contractor.
7.4.3 We therefore provide the following comprehensive guidance that outlines circumstances deemed appropriate to remove a patient from the patient list (only intended to be used as a guide and therefore not exhaustive) and emphasises the importance of applying this procedure when strictly necessary. The overarching objective behind a SAS is to ensure any patient removed under the regulations has access to essential services and commissioned enhanced services. Mutual behavioural expectations should also be communicated to patients exploring the root causes of their behaviour, to support their rehabilitation back into local services, while at the same time minimising the risks to the safety of health professionals and others. Refer to annex 2: sample SAS good conduct guide.
7.4.4 Commissioners should consider how additional support and resources to SAS providers (current and prospective) could be enhanced or put in place.
Increased local support could include a range of options: establishing a community of practice, professional support networks and collaborative working, developing specialist training, learning and development opportunities on key items such as: continuous risk assessment, personal safety and clinical training on trauma informed practice, substance misuse and mental health. Where an appropriate need for staff training is identified, the following may be useful:
- introduction to violence prevention and reduction
- handling difficult situations with compassion – e-learning programme
- handling difficult situations – caring for yourself and others with compassion – e-learning
Types of behaviour covered by this guidance
7.4.5 The Health Circular 2000/01 defined violence in the primary care context as:
“Any incident where a GP, or his or her staff, are abused, threatened or assaulted in circumstances related to their work, involving an explicit, or implicit, challenge to their safety, wellbeing, or health”.
7.4.6 The main kinds of behaviour which are considered to bring a patient within the regulations covered by this guidance are (these are only intended to be used as a guide and therefore the list is not exhaustive):
Assault
7.4.7 For an assault to fall within the scope of removal from the list, it should involve a person intentionally or recklessly causing another to apprehend the immediate infliction of unlawful force on an individual in a manner which either results in injury or causes that individual to fear injury or some other immediate threat to their safety.
Threatening behaviour
7.4.8 Any verbally threatened harm towards others, with or without accompanying gestures, will fall within the scope of a removal. Threats of non-violent acts are unlikely to do so: for example, use of offensive language without threats.
Behaviour resulting in damage to property
7.4.9 Any behaviour resulting in damage to property, whether accompanied by verbal threats or not and whether that damage is intentional or not, is likely to be within the scope of the scheme if the behaviour was intended to terrorise or intimidate individuals or is seen as a precursor to a personal assault.
Further considerations in relation to 7.4.7–7.4.9
7.4.10 Examples of the cases referred to above would include any incident in which the patient has:
- struck, grabbed or punched a GP, member of staff or other individuals either within the practice premises or elsewhere in a targeted attack
- thrown an inanimate object at a GP or member of staff either within the practice premises or elsewhere in a targeted attack
- struck, grabbed, punched or thrown an inanimate object at other patient(s) within the practice premises
- wielded a weapon, or used an object as one, in an actual or intended assault or in a manner intended to intimidate or terrorise staff, patients or other persons on the practice premises
- threatened to assault or physically harm a primary care worker
- threatened to damage property or to ‘seek revenge’ in a menacing way
- caused damage to property with an intention to intimidate or cause harm
This list is not exhaustive.
Types of behaviour this scheme does not ordinarily cover
7.4.11 Examples of the types of behaviours that would not ordinarily fall within the scope of the regulations covered by this guidance are:
- invasion of another person’s personal space, which can be considered threatening
- shouting or banging the reception desk
These are only intended to be used as a guide and therefore the list is not exhaustive. Any person who felt threatened or fearful of their own safety should still report the incident. These removal regulations cover all persons on the practice premises.
7.4.12 In such circumstances, the practice should explore the root cause which is causing this behaviour – this may include unmet needs, a communication breakdown, fear/anxiety/stress and sensory overwhelm – and, where possible, take action to rectify the cause. Following an attempt to identify and understand the root cause, it might be appropriate to use the standard procedure for a breakdown in practice–patient relationship, usually writing to the patient after the event to warn them that a continuation of such behaviour could result in them being removed from the practice list. Practices may also choose to use or agree a mutual behaviour agreement with the patient to support their continued registration.
7.4.13 Patients must not be immediately removed for minor incidents not reported to the police.
7.4.14 Consideration should be given as to the history and circumstances of a patient including:
- wherever the behaviour can be ascribed to a condition capable of being rapidly alleviated by treatment: for example, mental health illness or medical/acute conditions with known behavioural changes such as head injury
- whether it relates to a patient who has never been aggressive before and/or who is clearly suffering mental or physical distress
- whether there have been extenuating circumstances affecting the care provided to the patient
Careful consideration of any mitigating circumstances must be given as to whether a referral to the scheme is in the best interests of the patient.
7.4.15 Incidents that occur outside the primary care setting and have no connection with the practice, such as community or hospital-based incidents would ordinarily default to and be dealt with by that specific setting’s policy.
It is important to recognise that the SAS does not usually provide for the ongoing treatment of the families of those patients allocated to it for incidences which have been reported to the police and an incident number provided. A practice must not unilaterally remove all family members unless they have also behaved in a way as to require allocation to an SAS and each patient must be referred separately. On a case-by-case basis, as part of their safeguarding considerations, SAS providers should consider the support any vulnerable dependent family member of the patient may need and their need to be registered with the SAS provider: for instance, assessment of child dependants and whether the patient being diverted to the SAS is the sole parental carer to take any child to their GP where:
- the child is aged 16–18 years old; this might then not be an issue since children of this age can often consent to treatment
- the child is aged 14–16 years old; they may require another responsible and trusted adult to attend, including an older sibling or kinship carer
- the child is under 14 years old; they should always have a parent, kinship carer or guardian present
Safeguarding: registering children
7.4.16 Section 11 of the Children Act 2004 places a statutory duty on the NHS to safeguard and promote the welfare of all children up to the age of 18 years. The Victoria Climbie Enquiry Report 2003 (9.104) stresses the importance of GP registration for every child. It sets out the importance of knowing the identity and name of those registering the child and their relationship to that child.
The legal definition of a child is 0 to 18 years of age. However, while 16–18-year-olds are still children by law of child protection, they can also be parents and carers. Therefore, it is important that risks and vulnerabilities within this age group are considered.
Where parents or carers have been removed from the list due to aggressive or violent behaviour, a risk assessment should be completed to identify any risk to their children and the appropriate referrals safeguarding made. Please ensure you consult relevant safeguarding procedures and record any referral decision.
In any type of patient deduction, consideration must be given to any potential safeguarding concerns. Where a patient is at risk of being removed that may impact on parenting/caring capacity (for example, mental health), consideration must be given to safeguarding for children or vulnerable/at-risk adults. Advice should always be sought from local safeguarding leads and/or the commissioner’s designated professional.
With regards to the deduction of children (aged under 18), GP practices have the clinical expedient prerogative to retain children (under 18 years old) under the paramountcy of the child within The Children Act 2014, until such time that they understand how the children might be cared for by another NHS or private GP, especially if vaccinations or screening are still indicated.
It should also be noted that:
- children and young people (CYP) on a protection order or protection plan should not be de-registered on the grounds of behaviour including non-attendance
- CYP (not protected) and adults with learning disabilities and/or who are autistic, individuals with a mental health issue and with those with a formal carer should not be de-registered on the grounds of behaviour including non-attendance
These individuals may need to be referred to safeguarding leads since they might be at risk either through behavioural problems or non-attendance of their appointments.
These individuals should be allowed to sustain their GP registration for continuity of care until such times as it can be established how they might be cared for by another NHS or private GP.
Therefore:
- children of parents or carers who have been removed from the list for any reason must not be left without access to primary care service
- where parents or carers have been removed from the list due to aggressive or violent behaviour, a risk assessment should be completed to identify any risk to their children and the appropriate safeguarding referrals made. Please ensure you consult relevant safeguarding procedures and record any referral decision
A ‘think family’ approach should be taken when seeing either the adult(s) or child(ren) within the surgery. If healthcare professionals are aware that an adult has significant risk-taking behaviour, chronic mental health concerns or repeated episodes of stress and anxiety, safeguarding and support consideration should be given to the welfare and safety of the child/children being cared for by that adult.
Refer to chapter 3: Managing patient lists and chapter 4: GP patient registration standard operating principles for primary medical care for further information on safeguarding.
7.4.17 Where a breakdown in relationship has occurred with non-dependant family members as a result of one family member being placed on the SAS, then they should be removed using a more relevant process: for example, 8-day removal. Refer to section 3.2: Part A: managing patient assignments (sub-section: removing a patient from a practice list).
Note: where a practice is unsure how to proceed, they can contact their commissioner for support, advice and guidance. The practice may also choose to seek guidance from their local medical committee (LMC).
7.4.18 Please refer to section 3.2: Part A: managing patient assignments (sub-section: removing a patient from a practice list). This describes what can be a more appropriate route in the event of an irrevocable breakdown in GP–patient relationship. However, a patient must usually be sent a warning letter within the proceeding rolling 12-month period and given the opportunity to moderate their behaviour. Removal can only normally be effected if the behaviour is repeated and then the patient can be given 8 days’ notice to find a new GP. This method of removal by the contractor is suitable for less serious circumstances. Patients must not be removed using the ’immediate removal’ process unless the matter has resulted in the incident being reported to the police.
In circumstances where a patient displays inappropriate or unacceptable behaviour towards staff or other service users short of violence and threatening abuse (for example, discrimination, harassment or victimisation), refer to chapter 6: Managing [non-violent] patient behaviours which lead to removals from the list at the request of the contractor.
Removing a patient immediately
7.4.19 Under the regulations, once satisfied that a patient’s behaviour warrants removal from the practice list, to remove a patient immediately the practice is required to:
Notify the police
7.4.20 To remove a patient immediately for cases of assault, threat or damage, the incident has to be serious enough to justify reporting the incident to the police in an appropriate timeframe, due to the incident having left the person(s) feeling sufficiently threatened for their own safety or that of another.
7.4.21 The practice, where appropriate, should dial 999 on the day of the incident and, if necessary, summon police assistance/attendance. When contacting the police, it is important that the practice makes it clear that an incident has occurred and that the practice wants to make a formal statement as soon as possible, to support the immediate removal of the patient from the practice list.
7.4.22 Due to the nature of incidents requiring an immediate removal under the regulations, it would not be expected that the practice notifies the police days after the incident. A further contact to the police within 7 days may be required if the incident number for the call was not recorded, retained or provided at the time of the call. The SAS policy is in place for urgent incidents and, as such, this information and evidence may be used for local audit purposes.
Notify the commissioner (via PCSE)
7.4.23 The practice is required to notify the commissioner via PCSE by using the online forms on the PCSE website, as set out in section 7.1: Executive summary and key messages, number 2. The practice will need to confirm that prior to removing the patient from its patient list, it has carefully considered the patient’s protected characteristics and key past medical history, learning disability and neurodiversity and completed any safeguarding considerations where applicable. At this point there will be a reasonable expectation that practices will be able to evidence contact with the police by passing on an incident number or detail why this has not been possible. The practice will be required to follow up the call by emailing a written report of the incident (including police incident number) to the commissioner, preferably within 24 hours but no more than 7 days after the incident occurring. Annex 23 provides a PCSE request for removal of patient from practice list form.
7.4.24 The practice must notify the patient that it has requested their removal from the patient list, as set out in the regulations unless an exception applies.
7.4.25 PCSE will ensure the patient removal process commences. Following the removal and in conjunction with the commissioners as necessary, PCSE will decide on the best arrangement to ensure continuity in primary medical services for the patient. This may include allocation to the SAS. A flag is placed on the patient record which prevents the patient from registering at other GP practices.
7.4.26 PCSE will write to the patient to notify them of the removal and ongoing management arrangements. Refer to annex 22. It is expected that this process will be completed within a 24-hour working period from the initial notification.
NHS England is committed to working with its partners, patients and patient representative groups to refine and improve this standardised letter further. We are also committed to making this communication available in alternative languages.
7.4.27 Following removal, all patients must be allocated to and accepted by the SAS provider commissioned by the ICB. Subsequently:
- all patients allocated to SAS should have an assessment of appropriateness to be accepted in the scheme by the SAS provider (subject to services being commissioned to do so where not already in place or where commissioners have made alternative processes for enabling appropriateness assessments)
- once a patient has been accepted, all patients should receive a welcome letter from the SAS provider (subject to services being recommissioned where appropriate)
- the patient’s risk assessment should be continually reviewed and updated after each patient encounter with the SAS provider
- the SAS panel will monitor ongoing appropriateness of the patient’s continued registration with the SAS and their rehabilitation. This is with a view to safely returning choice to the patient in a timely way and their re-integration into mainstream GP practice
- the patient should be discharged where there is clear evidence of change in behaviour and supporting safety risk assessment. This will usually involve patients being reviewed on a minimum of 3 occasions unless in circumstances of a successful SAS appeal
- the SAS provider will also carry out an initial risk assessment of all new patients, which much include:
- a level of security and safety measures required
- patient care plan
- assessment of patient’s rehabilitation needs to enable discharge from SAS
- travel needs of the patient
- safeguarding considerations (noting subject to contract variation procedures as appropriate)
- depending on the needs of the patient, rehabilitation options could include counselling, anger management, drug and alcohol interventions and other local initiatives and pilot programmes
SAS providers should complete a comprehensive discharge summary after the final risk assessment with the patient. The discharge summary should include any outstanding referrals in process and consideration should be given to the provision of prescription medication to cover the interval before the patient registers with a mainstream GP practice (normally 3–4 weeks supply). A copy of the discharge could be saved in the medical records to make it available to the receiving practice.
A patient who has not engaged with the SAS provider following their immediate removal and allocation will remain registered with the SAS until they do engage and have been assessed by the SAS provider. Registration with an SAS provider prevents the patient from being able to register with a mainstream GP practice, thus protecting the safety of NHS staff and service users.
On discharge from the scheme, SAS providers should be encouraged to support patients in finding an alternative GP practice. Find a GP includes information on registration.
This may help break a cycle of registration and removal, as patients are supported with the transition. In addition, SAS providers can help to allay any concerns a newly registered practice may have about registering the patient.
7.4.28 Registered providers and managers of NHS GP and other primary medical services must also comply with their regulatory obligations: for example, to notify the CQC about certain incidents that took place “while an activity is actually being provided” or as “a consequence of its being provided” (CQC, 2013) and when an incident is reported to or investigated by the police. Further information is available on the CQC website.
7.4.29 For further information relating to the process, please refer to annex 25: what happens to the patient following allocation?
7.4.30 The practice must notify the patient that it has requested their removal from the patient list, as set out in the regulations unless an exception applies.
7.5 Patient appeals process
7.5.1 The appeals process must recognise that a practice has already fulfilled its obligation under the regulations by reporting the incident to the police and notifying the commissioner.
7.5.2 Patients referred to the SAS have a right of appeal and, should they wish to do so, can appeal against the decision by putting this in writing within 28 days of the notification of the referral, addressing it to the commissioner’s SAS liaison team. The commissioner will contact the practice to notify it of the appeal and invite the practice to provide any supplementary information in relation to the removal.
The appeals process does not delay the immediate removal of a patient following an incident that has been reported to the police and the commissioner (via PCSE).
7.5.3 The appeal should be reviewed by a panel convened by the commissioner (a ‘SAS panel’) within 28 days of receipt of the patient’s appeal. The panel should include appropriate representations (including from the LMC and, if appropriate, a patient representative or patient representative group when requested by or agreed with the patient). Refer to annex 26: sample terms of reference for an appeal panel.
7.5.4 It is the responsibility of the SAS panel to review the evidence provided by the patient in support of their appeal. The SAS panel will uphold or reject the appeal where it has reasonably considered if a removal under the regulations was made in error or inappropriately.
7.5.5 Pending the outcome of any appeals process, should the patient need to access primary medical services, this will have to be provided by the SAS to which the patient had been allocated.
7.5.6 The commissioner will notify the patient of the panel’s decision in writing within 14 days of the SAS panel decision, having first discussed the outcome with the practice from which the patient was removed.
Patient appeals – additional information
7.5.7 To support appeal panels in reaching a determination, the following annexes may be useful and some sample considerations are provided below (list not exhaustive):
- annex 25: sample SAS good conduct guide
- annex 27: sample data sharing agreement
- annex 28: risk assessment approach
7.5.8 The panel should be assured that:
- the identity of the removed patient and that of the patient who was involved in the incident should be confirmed as the same and be without any doubt
- where the reported incident occurred during a clinical consultation, the removed patient had an appointment at the practice on the same day
- a police incident number has been provided, either at the time of the removal or within 7 days as part of the written report
- a written report has been submitted to the commissioner (usually via PCSE). See annex 23: PCSE request for removal of patient from practice list form
- the information provided in the report is consistent with the requirements for immediate removal, as set out in the GMS/PMS Regulations
- the content and strength of any evidence provided by the removed patient does not wholly support their claim that they should not have been removed: for example, clear and incontrovertible evidence that they were out of the country at the time of the incident or at another location, such as in hospital
7.5.9 The panel should also:
- invite the patient to submit any further relevant information or a statement in relation to the alleged incident. This will ensure all parties are considered to have been treated fairly and equally should the matter be escalated to the Parliamentary and Health Service Ombudsman (PHSO) or through a legal route
- seek confirmation from the GP practice of which member of staff who was involved in the incident
- seek confirmation from the practice of which member of staff requested the deduction
- discuss the incident with the practice
- re-confirm with the practice the details of the patient involved in the incident and cross-check this with the details of the patient making the appeal
7.5.10 In reaching a determination, the panel may conclude that the patient’s appeal should be upheld. In this case, the SAS flag on the patient records should be removed (by the commissioner notifying PCSE) and choice returned to the patient. This presents several options to the panel and the commissioner and will depend entirely on the reason for upholding the appeal.
7.5.11 If, for example, a case of mistaken identity is confirmed, the panel in consultation with the commissioner may (if agreed in advance with the removing GP practice) seek to return the patient to the GP practice they were removed from.
7.5.12 Return of choice to the patient enables them to choose another GP practice in the area where they live. This could be an option where the GP practice that removed the patient under the immediate removal process considers there has also been an irrevocable breakdown in relationship. Refer to chapter 3: Managing patient lists.
7.5.13 In reaching a determination that the patient appeal should be rejected, the patient should remain on the SAS and be reviewed in accordance with policy.
7.5.14 In all cases the patient must be notified within 14 days of the appeal hearing. Sample patient letters can be found at:
7.5.15 Each commissioner’s SAS panel should consider any patient appeal. The panel’s decision with regard to the removal and SAS allocation does not affect the patient’s right to escalate the matter to the Commissioner or the Parliamentary and Health Service Ombudsman (PHSO).
Note: If a patient’s appeal is upheld, the commissioner must notify PCSE via pcse.patientremovals@nhs.net.
8. Contract variations (templates available)
8.1 Introduction
8.1.2 This policy describes the process to determine any contract variation, whether by mutual agreement or required by regulatory amendments, to ensure that any changes reflect and comply with legislation and to maintain robust contracts.
8.2 Types of contract variation
8.2.1 Variations to contracts fall broadly within 4 categories:
- changes due to legislation or regulatory change
- changes to the contracting party
- changes to services
- changes to the payment arrangements
8.2.2 Where a GMS contract or PMS agreement is varied, the commissioner is required by the regulations to notify relevant patients where such variation:
- changes the range of services provided to the contractor’s registered patients; or
- where patients who are on the contractor’s list of patients are to be removed from that list
8.2.3 The commissioner must inform those patients of the steps they can take to obtain the services in question elsewhere or register elsewhere for the provision of essential services (or their equivalent).
8.2.4 The commissioner should consider whether any such provision is contained within any APMS contracts it holds.
8.3 Legislation/regulatory changes
8.3.1 Usually both parties to a primary medical contract must agree on a variation for it to take effect. The commissioner may, however, vary the contract without the contractor’s consent where it is reasonably satisfied that it is necessary to do so to comply with the NHS Act, any regulatory changes pursuant to the NHS Act or any direction given by the Secretary of State pursuant to the NHS Act. This right is contained within all GMS contracts, PMS agreements and APMS contracts.
8.3.2 The commissioner must notify the contractor in writing of the wording of the variation and the date it will take effect. Where it is reasonably practicable to do so, the date the variation will take effect must not be less than 14 days after the notice is served.
8.3.3 There is no need for the commissioner to seek agreement or require a signature of acceptance for this type of variation, as there is no right of refusal or negotiation.
8.3.4 The process for issuing a variation notice due to legislation/regulatory changes is:
- a regulatory amendment to existing regulations or new directions are issued under statutory instrument. Commissioners should ensure arrangements are in place to take the appropriate action as quickly as possible after the issue of an amendment
- where the GMS Regulations, PMS Regulations and/or APMS Directions are amended, there will be centrally issued variation notices. These should be used (and in the centrally issued template provided) to update the relevant contracts and ensure contractors are informed of the changes
- the commissioner must notify contractors of the variation and its effective date. Template variation notices are provided in annex 31 for GMS contract variations and annex 32 for PMS/APMS contract variations
- for GMS contractors, the notification should include the GMS variation and the relevant pages of the amended contract document for completeness. For PMS and APMS contractors, the commissioner will be required to ensure the regulatory amendments become a contractual amendment, citing the correct clause numbers affected within the individually held contracts and including the relevant pages of the document for completeness
- all electronically held contracts should be updated with the variations at this stage to ensure that the centrally held documents remain up to date with current legislation. Commissioners should retain a copy of the notice on file for completeness. Each contract file should contain a variation log and commissioners should ensure that this is updated accordingly
- commissioners should notify PCSE of all contract changes to ensure accurate GSUM calculations are made and contract values are updated
8.4 Changes to the contracting party
8.4.1 Changes to the contracting party may be due to:
- partnership changes
- company changes
- retirement (including 24-hour retirement)
- novation, mergers and splits
- death of a contractor
8.4.2 There are specific processes to follow on the death of a contractor. Please refer to the part C, chapter 3: Death of a contractor for further information.
8.4.3 The GMS Regulations, PMS Regulations and the APMS Directions contain provisions relating to the remaining scenarios listed above which are considered in more detail below.
8.5 Partnership changes
8.5.1 Changes to the composition of a partnership will require variation to the contract and may require a variation to the standard registration conditions with the CQC.
8.5.2 Generally, this type of contract modification is permitted under the PSR, although in some circumstances the admittance of a new contracting party may constitute and require a new ‘selection’ decision following the most suitable provider process or the competitive process. Commissioners will find it helpful to review the PSR supplementary guidance for primary care alongside this section when considering each case. The PSR statutory guidance should be referred to and appropriate advice taken at an early stage where necessary for complex cases.
8.5.3 The GMS Regulations, PMS Regulations and APMS Directions place restrictions on the organisational structures that are eligible to enter into different types of primary medical contracts. Please refer to chapter 1: Contracts described for details on the eligibility criteria.
8.5.4 Contracts may be varied in a number of ways with relation to partnership matters, including the following which are looked at in more detail below:
- individual contractors changing to more than one individual (which may be a partnership which requires a different process depending on whether it is a GMS contract or not)
- changes to the parties of contracts with more than one individual (which may be from a partnership to an individual contractor or changes to the composition of partnerships)
8.5.5 There may be many reasons for partnership changes including disputes between parties which are considered further below.
Individual to partnership – GMS contracts
8.5.6 If a GMS contractor is currently an individual medical practitioner who wishes to enter into partnership with one or more individuals under that contract, the contractor is required to notify the commissioner in writing and provide the following information:
- the name of the individual or individuals with whom the contractor proposes to practice in partnership
- confirmation that the individual or individuals are either a medical practitioner or a person who satisfies the conditions specified in section 86(2)(b) of the NHS Act
- confirmation that the individual or individuals satisfy the conditions imposed by Regulations 4 and 5 of the GMS Regulations (please refer to chapter 1: Contracts described for further information)
- whether or not the partnership is to be a limited partnership and, if so, who is a limited and who is a general partner
- the date on which the contractor wishes to change its status (which shall not be less than 28 days from the date on which the notice was served on the commissioner)
8.5.7 The notice must be signed by the individual contractor and by the individual or individuals with whom the individual contractor is proposing to practise in partnersh Where the contractor contacts the commissioner about such a change, the commissioner should send annex 33: request for information relating to change from individual to partnership – GMS contracts.
8.5.8 The commissioner must ensure the accuracy of the information prov This may be achieved, for example, by checking the registration status of the proposed partner(s) and that the proposed partner(s) meet the eligibility criteria for holding a GMS contract.
8.5.9 Where the change is agreed, the commissioner will confirm in writing that the contract will continue with the partnership and issue a variation notice accordingly to amend the relevant sections of the contrac The commissioner must specify in the notice the date on which the contract will continue as a partnership. Where reasonably practicable this should be the date requested by the contractor or the nearest date to it (see annex 34: acknowledgement of information relating to change from individual to partnership – GMS contracts).
8.5.10 A variation notice must include the wording of the proposed variation and the date on which the variation will take effect. The contractor would then be required to return a signed copy of the variation notice. The commissioner should ensure that the electronically held contract documentation is amended accordingly.
8.5.11 If the new partner is not accepted as eligible, the commissioner should advise the contractor in writing of the reasons it believes the proposed partner(s) to be ineligible and confirm that the contract status will remain with an individual medical practitioner until the matter can be resolved or a further notice is provided by the contractor proposing an alternative eligible partne
Individual to more than one individual
PMS agreement
8.5.12 The PMS Regulations do not allow PMS agreements to be treated as made with a partnership. Where individuals are practising in partnership, the PMS agreement will be entered into with each person (which may or may not be in partnership). The persons comprising the signatories to the PMS agreement collectively form the contractor.
8.5.13 The PMS Regulations do not require a PMS agreement to define a specific process for any variation to the signatories. The commissioner must, therefore, review the relevant PMS agreement to determine whether any provisions have been added relating to this and prior to following any process for variation.
8.5.14 If the contractor is currently an individual medical practitioner and they wish to have one or more persons join them under that agreement, then they must seek the commissioner’s consent in writing for any such variation to the contract. Where the contractor contacts the commissioner about such a change, the commissioner should send annex 35: request for information relating to change from individual to more than one individual – PMS contracts.
8.5.15 The commissioner must ensure the proposed person(s) meet the eligibility criteria for holding a PMS agreement (please refer to chapter 1: Contracts described for further information).
8.5.16 The commissioner should confirm its decision on the variation in writing to the contractor detailing the reasons for the decision and details of any information that they have relied on in the process (see annex 36: acknowledgement of information relating to change from individual to more than one individual – PMS agreements).
8.5.17 If the decision is to consent to the variation, then the commissioner shall issue a variation notice accordingly to amend the relevant sections of the contract. A variation notice should include the wording of the proposed variation and the date on which the variation will take effect. The contractor would then be required to return a signed copy of the variation notice. The commissioner should ensure that the electronically held contract documentation is amended accordingly.
8.5.18 If the contractor does not return a signed copy of the variation notice, then no amendment to the agreement can take place.
8.5.19 If the new person is not accepted as eligible, the commissioner should advise the contractor in writing of the reasons they believe the proposed person(s) to be ineligible and confirm that the contract status will remain as it was until the matter can be resolved or a further notice is provided by the contractor proposing an alternative eligible person.
Individual to more than one individual – APMS contract
8.5.20 APMS contracts can be entered into with a partnership and the commissioner should consider the wording of the relevant contract to determine whether there are any specific provisions covering a request from the contractor to have one or more persons join them under the contract. Where there are no such provisions, a similar process to PMS agreements could be followed.
Changes to contracts with more than one individual – GMS contracts
8.5.21 Changes to the contracting parties may occur where a partnership dissolves or terminates or where the composition of the partnership changes. Both scenarios are explained below.
8.5.22 Where a partnership is dissolved or terminated and the contractor consists of 2 or more individuals practising in partnership, the contract may continue with one of the former partners if the following conditions apply:
- the former partner must be nominated by the contractor; and
- the former partner must be a medical practitioner who meets the condition in regulation 4(2)(a) of the GMS regulations
8.5.23 The nomination of the former partner by the contractor must:
- be in writing and signed by all the individuals who are practising in partnership. Where the contractor contacts the commissioner about such a change, the commissioner should send annex 37: request for information relating to change from partnership to individual – GMS contracts
- specify the date on which the contractor proposes to change its status from that of a partnership to that of an individual medical practitioner
- be provided to the commissioner at least 28 days in advance of the date on which the contractor proposes to change its status from that of a partnership to that of an individual medical practitioner
- specify the name of the medical practitioner with whom the contract will continue, which must be one of the partners
8.5.24 Where the commissioner receives such a nomination, it must acknowledge receipt in writing before the date specified in the nomination as the date on which the contractor proposes to change its status from that of a partnership to that of an individual medical practitioner (see (see annex 38: acknowledgement of information relating to change from partnership to individual – GMS contracts).
8.5.25 Where the commissioner agrees the nomination, the commissioner may vary the contract but only to the extent that it is satisfied it is necessary to reflect the change in status of the contractor from a partnership to an individual medical practitioner. The commissioner must notify the contractor in writing of the wording of the proposed variation and the date on which that variation is to take effect.
8.5.26 A variation notice will need to be included with this letter.
8.5.27 The commissioner should be satisfied that the arrangements in place for continuity of service provision to the contract’s registered patients are robust.
8.5.28 In circumstances where the commissioner is not satisfied that the nominated partner is eligible to hold the contract as an individual, they should enter into dialogue with all the partners to explore potential solutions.
8.5.29 These might include the partners nominating an alternative partner to continue with the contract, in which circumstances a new notice should be issued to the commissioner to include these details and propose a new date on which the changes will occur.
8.5.30 Where the contractor consists of 2 or more individuals practising in partnership and the composition of the partnership changes, either by a partner leaving (but without the partnership terminating) or a new partner joining, the contract will need to be amended to recognise the new partnership composition. For the variation to have effect, it must be in writing and signed by all parties to the contract.
Changes to contracts with more than one individual – PMS agreements
8.5.31 As stated in 8.5.13, the PMS regulations do not require a PMS agreement to define a specific process for any variation to the signatories. The commissioner must, therefore, review the relevant PMS agreement to determine whether any provisions have been added relating to this and prior to following any process for variation.
8.5.32 If the contractor is currently 2 or more persons and wishes to change to an individual contractor, then it must seek the commissioner’s consent in writing for any such variation to the contract. Where the contractor contacts the commissioner about such a change, the commissioner should send annex 39: request for information relating to change from more than one individual to an individual – PMS agreements.
8.5.33 The commissioner must ensure that the proposed person(s) meets the eligibility criteria for holding a PMS agreement (please refer to the chapter 1: Contracts described for further information).
8.5.34 The commissioner should confirm its decision on the variation in writing to the contractor detailing the reasons for the decision and details of any information that it has relied on in the process (see annex 40: acknowledgement of information relating to change from more than one individual to an individual – PMS agreements).
8.5.35 If the decision is to consent to the variation, the commissioner shall issue a variation notice accordingly to amend the relevant sections of the contract. A variation notice should include the wording of the proposed variation and the date on which the variation will take effect. The contractor would then be required to return a signed copy of the variation notice. The commissioner should ensure that the electronically held contract documentation is amended accordingly.
8.5.36 If the contractor does not return a signed copy of the variation notice, then no amendment to the agreement can take place.
8.5.37 If the new person is not accepted as eligible, the commissioner should advise the contractor in writing of the reasons it believes the person is ineligible and confirm that the contract status will remain as it was until the matter can be resolved or a further notice is provided by the contractor proposing an alternative eligible person.
8.5.38 The principles outlined in 5.31 to 8.5.37 will also apply where the contractor consists of 2 or more persons and the composition of the contractor changes, either by a person wishing to leave the agreement or a new person joining the agreement. The contract will need to be varied to recognise the new contractor composition.
8.5.39 The commissioner should ensure that it is satisfied that the contractor will remain eligible to hold the agreement after the variation. For the variation to have effect, it must be in writing and signed by all existing (and new) persons to the contract.
8.5.40 The commissioner should also be satisfied that the arrangements for continuity of service provision to the registered population covered within the contract are robust and may wish to seek written assurances of the post-variation contractor’s ability and capacity to fulfil the obligations of the contract and its proposals for the future of the service.
8.5.41 APMS contracts or PMS agreements are not required to contain a right of termination where one or more persons have left the practice during the existence of the contract. The commissioner should review the relevant contract to determine whether any such provisions have been included.
Changes to contracts with more than one individual – APMS contracts
8.5.42 The commissioner should consider the wording of the relevant APMS contract to determine whether there are any specific provisions relating to changes to the composition of the contractor. Where there are no such provisions, a similar process to PMS agreements could be followed.
Partnership splits/members dispute – GMS contracts and PMS agreements
8.5.43 Where the contractor to a GMS contract is a partnership and the partnership dissolves due to an internal partnership dispute, the parties may agree for the contract to continue with one or more existing partners (see 8.5.22). If the partnership dissolves and there is no agreement between all partners who will continue the contract, commissioners should:
8.5.43.1 Where the 2025/26 GMS contract variations have not yet been applied to the contract (for example, until October 2025) refer to annex 41: managing circumstances where partnership dissolves with no clear successor – GMS contracts for further advice.
8.5.43.2 Where the 2025/26 GMS contract variations have been applied (for example, from October 2025), the contract may be terminated by the commissioner if it is otherwise unable to determine which parties of the dissolved partnership (if any) the contract should continue with in the absence of any agreement between all partners. This would mean commissioners may have little time to make arrangements to ensure service continuity from an alternative provider (or multiple providers in case of decision to split the contract – noting the effect of this proposal on statutory duties, particularly the involvement duty under section 13Q duties and PSR considerations in the award of new contracts).
8.5.44 It is desirable that the partners of a GMS contract can resolve disputes internally where possible, with the support of the LMC and/or mediation services.
8.5.45 If the partnership holding a GMS contract does not dissolve or terminate but the partnership no longer wishes to be a party to the contract, then the contractor will need to terminate on notice, which must not be less than 6 months unless agreed by the commissioner. Failure to give 6 months’ notice of termination is a breach of contract and the appropriate action will be taken in line with the part C, chapter 1: Contract breaches, sanctions and terminations.
8.5.46 Under PMS agreements, subject to the terms of the individual agreements, partnership matters (including dissolution or termination of the partnership) do not affect the continuation of the agreement. This is because where the agreement is with 2 or more persons that are practising in partnership, the agreement is not entered into with the partnership but instead with those persons (who collectively make up the contractor).
8.5.47 If a PMS contractor is practising in partnership and, following termination of a partnership, the contractor no longer wishes to be a party to the contract, the contractor will need to give notice to terminate the contract, such notice being a minimum of 6 months unless agreed with the contractor.
8.5.48 Where partnerships or membership are formalised through a partnership agreement, it is very helpful if the parties are able to rely on the detail of these agreements to support the early resolution of internal disputes and to ensure that such agreements are reviewed and maintained to be current with associated legislation.
8.5.49 Unfortunately, many partnership organisations do not have agreements in place or have insufficient or outdated documents which can often lead to very protracted and acrimonious disputes between the partners.
8.5.50 The commissioner should not get involved in endeavouring to resolve the dispute between the partners, instead insisting that the parties notify the commissioner of their final decision when it is reached.
8.5.51 It is likely that the commissioner will have numerous contacts from different partners and their staff about the dispute, but the commissioner should try to maintain a detached position in this respect. Any accusations of inappropriate behaviour or concerns should be considered; however, this should not be used as a means to endeavour to resolve the dispute.
8.5.52 Throughout the dispute the commissioner should maintain open dialogue with the LMC and implement contract performance management protocols if and when necessary.
8.6 Retirement of a contractor – single handed
8.6.1 There is no specific reference to retirement in the GMS Regulations, the PMS Regulations or the APMS Directions. The commissioner should deal with a request to retire as a request to terminate the contract by the contractor on notice.
8.6.2 The contractor must provide the commissioner with a written notification of the intended retirement date which will be the termination date of the contract. This notice period must not be less than 3 months for GMS contracts held by an individual medical practitioner or less than 6 months for GMS contracts that are not held by an individual and for PMS agreements/APMS contracts.
8.6.3 For GMS contracts, if the termination date is not the last calendar day of a month, the contract shall instead terminate on the last calendar day of the month in which the termination date fa
8.6.4 For PMS agreements/APMS contracts there is no such requirement. The commissioner must calculate the date of termination, based on the terms in the individual contract and from the date of the notice.
8.6.5 In exceptional circumstances, such as ill health, the commissioner may wish to waive its right to the full notice period, but it remains its right alone to do so. Consideration should be given, among other matters, to the effect that holding a contractor who is unwell to the full notice term may have on the contractor, the practice’s patients and colleague
8.6.6 In either case the commissioner should confirm receipt and acceptance of the retirement/termination notice in writing, the date on which the contract will terminate and any consequences and actions that the contractor must take as a result of the notice
8.6.7 Although not required by the GMS Regulations, the standard GMS contract clearly sets out the arrangements that must be made on termination of a contract, which include (but are not limited to) the contractor having to:
- cease performing any work or carrying out any obligations under the contract
- co-operate with the commissioner to enable any outstanding matters under the contract to be dealt with or concluded satisfactorily
- co-operate with the commissioner to enable the contractor’s patients to be transferred to one or more other contractors or providers of essential services (or their equivalent)
- deliver up to the commissioner all property belonging to the NHS including all documents, forms, computer hardware and software, drugs, appliances or medical equipment which may be in the contractor’s possession or control
8.6.8 The commissioner shall have in place arrangements for collecting any property owned by the NHS on or immediately after the termination date, which should be included on a log of collection, and against any commissioner held asset list, and where possible the contractor should be asked to sign to confirm the property that has been removed, accepting that it is owned by the NHS.
8.6.9 On termination of the contract, the commissioner shall perform a reconciliation of the payments made by the commissioner to the contractor and the value of the work undertaken by the contractor under the contract. The commissioner must then serve the contractor with written details of the reconciliation as soon as reasonably practicable, and in any event no later than 28 days after the termination of the contract.
8.6.10 Each party shall pay the other any monies due within 3 months of the date on which the commissioner served the contractor with written details of the reconciliation, or the conclusion of any NHS dispute resolution procedure, or court action as appropriate as the case may be.
8.6.11 PMS agreements/APMS contracts must make suitable provision for arrangements on termination, including the consequences (whether financial or otherwise) of the contract ending, subject to any specific requirements in the regulation While these terms are likely to mirror those set out in GMS contracts, the individual contracts must be checked by the commissioner to ensure that no additional or alternative terms were included. This is especially important when considering termination of an APMS contract, which may include very specific additional terms in this respect.
8.6.12 The key elements for consideration leading up to a termination remain the same in respect of patients, property and transfer of records and confidential information.
8.6.13 For a list of considerations relating to termination, please refer to part C, chapter 1: Contract breaches, sanctions and terminations.
8.7 Retirement of a contractor – 2 or more partners/individuals
8.7.1 Where a partner wishes to retire from a GMS partnership, as constituted from time to time, the contractor will need to notify the commissioner that it wishes to vary the contract. The commissioner should follow the process in 5.21 to 8.5.30 of this policy.
8.7.2 Where an individual wishes to retire from a PMS agreement, where that agreement is also held by one of more persons, the contractor will need to notify the commissioner that it wishes to vary the agreement. The commissioner should follow the process in 5.31 to 8.5.40.
8.7.3 Where a partner of a partnership holding an APMS contract wishes to retire, the commissioner should follow any process defined within the contract, or in the absence of any defined process, the consent of the commissioner must be sought through a contract varartion.
8.7.4 Any changes to the partners within a contract may require a new registration with the CQC.
8.8 Taking 24-hour retirement and returning to the partnership
8.8.1 24-hour retirement is a process by which members of the NHS Pension Scheme seek to qualify for their retirement benefits while continuing to work (albeit with a break).
8.8.2 24-hour retirement usually involves resigning from all involvement in an NHS contract, not returning to the NHS in any capacity for at least 24 hours and not working for more than 16 hours a week in the first month of retirement. The commissioner should ensure that it is aware of the current conditions around 24-hour retirement.
8.8.4 If the commissioner is approached by a contractor wishing to take 24-hour retirement, it must not offer advice relating to pension arrangements.
8.8.5 Where a contractor confirms that 24-hour retirement requires ‘resignation’ from the contract, steps will need to be taken to ensure that the contractor is removed from the contract, either by:
- termination on notice in the case of a single-handed contractor
- variation of the contracting party in the case of a partnership
8.8.6 The commissioner may wish to suggest single-handed practitioners take independent advice, as 24-hour retirement using the method described above would necessitate the termination of the contract as set out in 6.1 to 8.6.13.
8.8.7 Commissioners should consider the application of the Provider Selection Regime (PSR) in the event of a 24-hour retirement that would necessitate the termination of the contract: for example, does it trigger the necessity for a new PSR process? Commissioners should defer to the published PSR statutory guidance and seek legal advice locally as appropriate.
8.9 Variation provisions specific to a contract with a company limited by shares (GMS) or a qualifying body (PMS)
8.9.1 A GMS contract may be held by a company limited by shares (subject to certain conditions). PMS agreements may be held by a qualifying body (a company limited by shares, all which are legally and beneficially owned by persons who may enter into a PMS agreement).
8.9.2 APMS contracts, in principle, have fewer restrictions on the types of organisations that may enter into the contracts and therefore the commissioner can enter into APMS contracts with any individual or organisation that meets the provider conditions detailed in the APMS Directions.
8.9.3 For further information on what types of organisations can enter into the different types of contracts, please refer to part B, chapter 1: Contracts described for further information).
8.10 Contracts and incorporation/dis-incorporation
8.10.1 It is possible for individual GPs or partnerships holding a GMS contract, PMS agreement or APMS contract to seek commissioner approval to operate and deliver services through a company limited by shares (called a ‘qualifying body’ in PMS) – this process is known as ‘incorporation’. A change from a single-handed or partnership contract to a limited company is a complete change of the identity of the contracting party, regardless of whether the company is owned and/or run by the original contractors.
8.10.2 Dis-incorporation is the same process in reverse.
8.10.3 There is no right for a contractor to incorporate or dis-incorporate. It needs agreement from the commissioner, which does not have to be given. In reaching its approval or rejection decision, a commissioner should consider carefully the proposal including assessing the application for its benefits – for example, to patients – but also the opportunities including strategic alignment with local priorities to transform services and improve care quality. A commissioner should also consider the risks.
8.10.4 There are a range of incorporation scenarios that commissioners may be asked to consider. The most straightforward scenario is a request for the existing individual contractor(s) to form a company and continue to run the business themselves as the shareholders and directors of that company (or vice versa on dis-incorporation). There are a range of complex scenarios in which change to the nature of the contractor may need to be sought: for example, arising from corporate mergers, takeovers or group structures. Again, commissioners should defer to the published PSR statutory guidance and seek tailored legal advice locally to fully assess the risks and issues. In scenarios that include a plan to merge practices, there are a further set of considerations as set out in section 8.11: practice mergers and/or contractual mergers.
8.10.5 A commissioner may conclude that a proposal, and the associated benefits, is worth supporting provided that there is alignment with local strategic priorities and identified risk can be mitigated and/or minimised. If so, the contract will need to transfer from the old to the new contractor. A legal document called a novation agreement is used. Its primary function is to change the parties to the contract. In practice, it ends the contractual relationship between the commissioner and old contractor and creates a contractual relationship between the commissioner and new contractor. The agreement must be signed by each of the 3 parties. Before signing a novation agreement commissioners should defer to the published PSR statutory guidance and should seek legal advice locally. A contract variation cannot be used in place of a novation agreement.
8.10.6 The novation agreement can also capture what has been agreed at the point of novation including the nature of any controls, including pre-conditions to be satisfied, that have been placed on the contractor. Any such provisions can be added to the template novation agreement but this is likely to require legal advice (see 8.10.33).
8.10.7 Some incorporation scenarios may involve a contractor selling its business and as part of the sale transferring its contracts, including its list of registered patients, to the buyer. In the event this request is approved and the contract is novated, the buyer is agreeing to take over the seller’s responsibilities for performing the contract, along with any associated debts and obligations.
8.10.8 It is anticipated that GP practices operating on a PCN footprint may seek to incorporate. The drivers for this may include strengthening their collaboration with their PCN partners to deliver primary medical services, the ‘network’ contract and potentially other locally commissioned services.
8.10.9 Scenarios involving ‘at scale’ providers of primary medical services would create systemically important companies if those requests are approved.
Incorporation toolkit
8.10.10 To support effective decision-making in these scenarios, NHS England has co-developed with regional and local commissioning colleagues a toolkit that includes a standardised approach for assessing the requirements and considerations set out in this chapter. The toolkit includes:
- a standardised assessment framework to support commissioner decision-making processes
- a supporting guidance document to help commissioners apply the framework and consider essential checks and risk mitigations including for the ‘at scale’ provider of primary medical services scenarios at scale in this context can be defined in a number of ways:
- by the size of the population served: for example, on PCN footprint
- by the number of contracts held
- by the extent to which they operate across multiple commissioner areas only one of these needs to be present but, in some cases, more may be present
- an application template for providers aligned to this framework
- an example due diligence procedure that commissioners can adapt and tailor according to local arrangements
8.10.11 The objective of the toolkit is to support commissioners to:
- undertake their due diligence in a structured and consistent way including a standardised approach for assessing the requirements and considerations set out in this chapter
- reach an approval or rejection decision based on assessed levels of risk
- apply approval conditions as necessary to mitigate identified risks and issues
8.10.12 The assessment framework has been designed to be comprehensive in scope and to support commissioners to assess all incorporation scenarios. The framework should be applied in full when assessing ‘complex’ or novel incorporation proposals: for example, those involving ‘at scale’ providers of primary medical services. For more straightforward incorporation applications, commissioners should use their discretion as to whether the assessment framework should be applied in full. For all applications, commissioners should be able to audit and justify their approval or rejection decision.
The toolkit is intended to supplement, not replace, the considerations and guidance set out further in the remainder of this chapter.
Toolkit annexes:
- annex 42: supporting guidance for the commissioner framework for incorporation requests
- annex 43: acknowledgement of requests to incorporate and incorporation application – template and guide
- annex 44: assessment framework
Procurement considerations
Managing a request for incorporation and dis-incorporation
8.10.13 On receipt of a request from a contractor to incorporate or dis-incorporate, the process below should be followed:
- the commissioner should acknowledge the request and send the contractor an assessment template. . Annex 47 provides an acknowledgement letter and assessment template for dis-incorporation
- the commissioner should make the contractor aware of the potential implications of the incorporation or dis-incorporation. Contractors should be made aware that the commissioner will have to consider the request in light of the PSR. If a new PSR process is necessary, the existing or proposed new contractor may not be successful in winning the new contract. Where the change in the identity in the provider does not render the contract materially different and is solely a change in the succession of the provider as a result of corporate changes, this may be a permitted modification
- on receipt of the information, the commissioner should review the application using the toolkit and decide whether or not to agree the request
8.10.14 The commissioner should first consider whether the proposed new contractor is eligible to enter into the contract. If it is not eligible, the commissioner must refuse the request (see annex 48: letter of refusal of request to incorporate).
8.10.15 Where the proposed contractor is eligible, the commissioner should undertake further essential checks (including that they are satisfying their own statutory duties) and undertake a risk-based assessment when assessing any request.
8.10.16 These matters are outlined further in this section and detailed in the incorporation toolkit. In considering these matters, the commissioner is required to act reasonably and in accordance with public law principles. Matters to consider include:
- to determine whether the change proposed in the application aligns with the PSR or there is a risk of challenge under the PSR (see also Provider Selection Regime in part A, chapter 1: Commissioning described)
- the effect of the proposal on the statutory duties of NHS England, particularly the involvement duty under section 13Q (note: in the coming months, supplementary information and guidance will be will be made available to commissioners in the form of frequently asked questions) of the NHS Act 2006 (although this is not usually triggered by a change solely to the identity of the contractor), duty under section 13K (duty to promote innovation) and section 13P (duty as respects variation in provision of health services) (see chapter 2: General duties of NHS England)
- the value of the contract – both in terms of whether it represents value for money and whether it would be a contract of interest to others
- the likely level of market interest in the contract
- the potential for innovation
- the need to protect services in the core contract – commissioners should ensure that if novation goes ahead, it will not result in any reduction in services to patients
- whether the commissioner is satisfied that there will be continuity of patient care
- the extent to which the original contractor(s) will be controlling and giving instructions to the proposed contractor to comply with contractual obligations
- the extent of change to the terms of the existing contract (for example, when making additional changes to the contract such as contract value or services) and whether this makes it materially different – this is important in assessing both the provisions of the PSR and whether there is a service change requiring patient and public involvement
- payments under the existing contract and value for money
- benefits to patients of the proposal – these should be outlined by the contractor and, as a minimum, there should be no detrimental impact on patients or reduction in services
- opening hours (including evening and weekend) required – note that any reduction may trigger the patient and public involvement duty (see part A, chapter 2, General duties of NHS England, section 13Q) and in any case, is unlikely to be acceptable unless there are exceptional reasons justifying such a change
- sustainability – the commissioner should be assured that the proposed novation will ensure ongoing sustainability of the practice and patient services in the area going forward
- any impact on patient choice
- whether the commissioner requires that the existing contractor guarantees the performance of the proposed contractor (for example, this may be appropriate where on incorporation the new company will not have any assets) – any such requirement must be proportionate to the risks associated with the novation and reasonable with a clear rationale for placing such a responsibility on the existing contractor. Legal advice should be sought
- whether the commissioner has any concerns about the proposed contractor’s financial standing and financial stability – serious concerns are likely to suggest the proposed contractor is unsuitable as a contractor, whereas minor concerns could, for example, be a factor in deciding to seek a guarantee
- whether the commissioner is satisfied with the proposed contractor’s plans for managing and operating the practice, including any proposed changes from current arrangements
8.10.17 Where the proposed contractor is a company:
- but is not registered with Companies House (the contractor may take the view that this cannot be finalised until agreement in principle has been given by the commissioner)
- and any director of the company has been disqualified from another registered company (check Insolvency Website and Companies House Disqualified Directors)
8.10.18 An unsatisfactory Disclosure and Barring Scheme.
8.10.19 Whether the existing contractor has outstanding debts and whether novation is made conditional on repayment being made.
8.10.20 Whether the existing contractor has received any breach or remedial notices or contract sanctions and whether novation is made conditional on the proposed contractor taking on the consequences of the notices: for example, action the remedial activity; and/or
8.10.21 Whether the existing contractor has outstanding issues regarding CQC inspection or practice inspection by the commissioner and whether the novation should be made conditional on those issues being resolved – or in some circumstances it may not be appropriate to agree to a novation until those issues are resolved.
Making a decision
8.10.22 Each of the above factors, along with any other relevant information about the particular request, should be carefully considered in deciding whether or not the commissioner will consent to the incorporation or dis-incorporation request. If there are concerns about the level of risk of challenge, legal advice should be sought.
8.10.23 Requests for incorporation or dis-incorporation should be agreed with or without conditions unless there are concerns that the request will not benefit patients or will create a significant risk of successful legal challenge.
8.10.24 In practice, if the commissioner does not agree to novate the contract, the existing contractor may decide not to incorporate/dis-incorporate but to keep the existing contract in place. Where this happens, there will be no new contract to arrange.
8.10.25 Where the commissioner agrees the request, the original contract will be novated. Annex 49 provides a template agreement letter and annex 50 a template novation agreement.
8.10.26 As a contract novation is technically termination of the original contract and replacing it with a new contract, the commissioner must make appropriate arrangements for termination of the contractual relationship with the outgoing contractor including:
- carrying out a financial reconciliation
- any other requirements in the contract relating to termination
8.10.27 The novation process and the discretion commissioners have in approving the request provide an opportunity for commissioners to negotiate and agree a range of controls with the contractor. Those controls can take the following forms (these are not mutually exclusive):
- contractual requirements: there is some, although limited, scope to agree local contract variations that would bind contractors into a course of action and be enforceable using the core contractual levers
- non-contractual requirements: these are declarative statements of intent that describe expected behaviours and/or actions but are not enforceable through the core contract
8.10.28 There are opportunities and limitations in implementing both type of controls. The supporting guidance that forms part of the incorporation toolkit sets out further advice on how the contract novation process can be used by the commissioner to address identified risks and issues should it wish to approve the request.
8.10.29 Contractual requirements are the most binding form of control that can be placed on a contractor. They must be agreed between, and signed by, both parties in line with local contractual variation processes.
8.10.30 As the contractor has to agree to them, negotiating local contract variations at the same time as considering novation puts the commissioner in a good negotiating position. The value of documenting them in the novation agreement is to confirm and emphasise what has been agreed contractually at the point of novation.
8.10.31 However, there are rigid national rules and processes governing the core GP (GMS/PMS) contractual framework that limit the scale and nature of what local contractual variations are implementable outside the national requirements (which cannot be changed).
8.10.32 The nature of what is permissible when seeking to vary the contract needs to be considered on a case-by-case basis. In summary, the following broad principles act as parameters as to what might be suitable:
- variations are targeted, proportionate and can be justified on reasonable grounds – these can be linked to either contractor performance, their capabilities and contractual management arrangements
8.10.33 Variations must not seek to alter or extend the agreed core GMS service provision requirements – these are negotiated nationally with the BMA and are reflected in the relevant GMS/PMS Regulations and Statement of Financial Entitlements (SFE).
8.10.34 There are a practical set of local contract variations that are precautionary, support provider sustainability and can help mitigate for the occurrence and consequences of provider failure in line with good practice. For example, as the new contractor will be a body corporate, it will be appropriate to require that the new contract contains a change of control clause. Such a clause requires the contractor to notify the commissioner where there is a change in ownership or control of the contractor and can include a requirement to obtain the commissioner’s consent. If the commissioner does not consent to the change but the contractor proceeds anyway, the commissioner may issue a remedial notice.
8.10.35 The supporting guidance that forms part of the incorporation toolkit describes the different types of controls in more detail including the circumstances in which they might apply.
8.10.36 Commencement of the new contract must be made conditional on the new contractor being CQC registered. The CQC cannot provide the notification of decision until the date of commencement is agreed. The contractor should, however, provide the commissioner with written confirmation from the CQC that the CQC does not intend to impose any restrictions on registration of the new contractor.
8.10.37 Where the contractor does not agree with the commissioner’s decision, the contractor may appeal the decision. Please refer to part C, chapter 4: Managing disputes for further information.
8.10.38 Following the commissioner’s decision, any changes to the contracts must be made on the relevant payment and contract management systems.
8.11 Practice mergers and/or contractual mergers
8.11.1 A GP or partnership may hold more than one form of primary care contract with a commissioner. For example, a GMS contractor can also be a party under a PMS agreement and vice versa and/or a company may, for example, hold several GMS contracts.
8.11.2 This flexibility has enabled GP practices to come together in varying ways to provide support for each other, expand on the services available and/or resolve premises issues and achieve economies of scale, though each will have its own reasons for coming together.
8.11.3 The overarching issues for the commissioner to consider when any such proposal is made are the benefits to patients and the financial implications of the practice merger.
Note: Where a proposed merger involves one or more dispensing practices, contract managers should also refer to the Pharmacy manual.
Note: When considering a proposed merger that involves practices spanning multiple ICB boundaries, commissioners should continue to follow this guidance. A GP practice merger across ICB boundaries will not automatically trigger an ICB boundary change. However, if patient flows are likely to be significantly affected and commissioners wish to explore the possibility of requesting a change, they should refer to ICS boundary changes and mergers procedure.
Practice merger models
8.11.4 There are many ways in which practices may seek to come together. The most common are listed below but commissioners should recognise that a proposed practice merger may fall into one or more of the models below or may propose a different approach:
- Model 1: GP providers agree loose arrangements such as sharing back-office functions or management staff or may even create a new legal entity to manage and oversee the delivery of services under the GP contracts. This is not a formal merger and the contracts with the commissioner will not change (this model is often referred to as a contractual joint venture).
- Model 2: The GP partners from practice A may join the partnership of practice B and vice versa. The new partnership may continue to hold the 2 separate contracts but will have merged at an operational level.
- Model 3: GP partners from practice A join the partnership of practice B and practice A ceases trading. The commissioner terminates practice A’s contract and varies practice B’s contract to include the services originally provided by practice A. This may happen with more than 2 practices so that the larger partnership holds one larger contract for services originally provided by several practices under separate contracts. The parties are likely to enter into a business transfer agreement for the transfer of assets and staff.
- Model 4: GP providers come together to create a new legal entity: for example, the GP partners become shareholders of a new company limited by shares. This may involve:
- novating the existing GP contracts to the new entity (see also section 8.10: Contracts and incorporation/dis-incorporation)
- terminating the majority of the existing GP contracts and varying one to include all existing services; or
- terminating the existing GP contracts and directly awarding a new contract to the new entity
8.11.5 Practice mergers can be complex matters which should not be approached lightly by either the contractors or the commissioner. Where a practice merger requires amendments to the practice contracts, the final commissioning decision on whether contracts should be amended to effect the proposed merger lies with the commissioner. The commissioner does not have to agree to change the existing contracts and there are a number of important issues that would need to be considered prior to giving consent. An overview of the potential issues is set out below. This is by no means an exhaustive list and the commissioner should refer to and seek appropriate guidance in each case to ensure that all relevant matters are considered. Some of the factors set out in section 8.10: Contracts and incorporation/dis-incorporation in deciding on whether to agree to a novation are likely to be relevant here too, so please refer to that section for more information.
Benefits to patients
8.11.6 The commissioner should consider the following matters in relation to the effect of the proposed practice merger on patients:
- how patients would access a single service
- what would the practice boundary be (inner and outer)
- assurances that all patients will access a single service with consistency across provision – that is, home visits, booking appointments, essential and minor surgery, opening hours, extended hours, and so on, single IT and phone system
- premises arrangements and accessibility of those premises to patients
- proposed arrangements for involving the patients about the proposed changes, communicating the change to patients and ensuring patient choice throughout
- the impact on patient choice
- how the proposed merger is intended to benefit patients
Costs/value for money
8.11.7 A contract merger is likely to merge 2 contracts with differing values. This would have an ‘averaging’ effect, possibly resulting in a higher cost per head of population under a single contract than the commissioner would have expected. For example:
- practice A attracts £120 per patient with a list size of 1,400
- practice B attracts only £90 per patient but has a list size of 5,000
- practice A’s contract value by registered population = £168,000
- practice B’s contract value by registered population = £450,000
- total cost to the commissioner = £618,000
- a merger would result in a list size of 6,400 patients and as result the per patient cost would require renegotiation. From a procurement perspective, the commissioner should not usually enter into a new contract at a higher value than that covering the existing contracts
8.11.8 There may be other financial arrangements that need to be considered including but not limited to:
- the impact of directions under the Statement of Financial Entitlements or any specific terms included in the individual contracts
- quality and outcomes framework (QOF) – merging contracts midway through a financial year in respect of QOF achievements and payments is enormously complex and requires significant safeguards to be built in to ensure there is no duplication of payments at year-end. There will also be an averaging of the arrangements and achievements in this respect too. For example:
- practice A has always achieved highly against each indicator of QOF
- practice B has struggled to meet the criteria under several of the indicators
- the results of a merger might be a single practice with mediocre achievement against aspirations and this would affect the aspirational payment that the single contract would attract. Premises reimbursements would also be affected
General duties of NHS England
8.11.9 The general duties of NHS England/the commissioner are likely to be relevant to a decision by the commissioner to approve a practice merger that results in changes to the way services are delivered.
8.11.10 As set out in part A, chapter 2: General duties of NHS England, section 13Q of the NHS Act 2006 requires NHS England to make arrangements to involve the public in the commissioning of services. The requirements are triggered if there are proposals that mean patients would experience a change to the range of services available or the manner in which they are delivered: for example, if a practice is closed following a practice merger.
8.11.11 As set out in part A, chapter 2: General duties of NHS England, NHS England has published guidance on section 13Q in the form of ‘The statement of arrangements and guidance on patient and public participation in commissioning’ (the ‘statement’).
8.11.12 The statement sets out that a change in the GP delivering the service is not usually enough to trigger the duty, but that care must be taken if a change in personnel makes services less accessible to patient groups: for example, because patients wish to be treated by someone of the same religion and/or gender as them. Where a practice merger may result in a change of the personnel delivering the service, the commissioner should be alert to this.
8.11.13 In practice, what will be sufficient in terms of patient involvement is very context specific. The extent of the patient engagement activities required will depend on a number of factors including the extent of the impact any changes will have. As a general rule, the greater the extent of changes and number of people affected, the greater the level of activity that is likely to be necessary to achieve an appropriate level of public involvement.
8.11.14 Generally speaking, to meet the section 13Q duty, involvement needs to apply to and inform the whole decision-making process, but this does not mean that patients need to be actively involved at every moment. Provided involvement is suitably built into the overall process, its timing can be arranged at stages to suit the commissioner’s decision-making processes. In particular, it is not necessary to involve patients immediately at the outset of any planning/consideration/decision-making process in relation to any proposals of the commissioning of new services, provided patient involvement is planned for some early stage in the process. The plans for patient involvement should be clearly documented from the outset and the commissioner should consider liaising with patient representative groups, such as local Healthwatch or the practices’ patient participation groups.
8.11.15 The timing of public involvement is again a matter of broad discretion for the commissioner. However, any involvement should be meaningful. As such, the commissioner should involve patients at the time proposals are developed and considered. Overall, it is helpful to bear in mind the ‘gunning’ principles (these are used to judge whether or not a consultation exercise has been ‘fair’ but are useful when making arrangements for patient and public involvement), as follows:
8.11.16 Involvement should take place when the proposal is still at a formative stage.
8.11.17 Sufficient information regarding the proposals should be provided, to allow meaningful involvement.
8.11.18 Adequate time should be given for consideration of the information provided and for response.
8.11.19 The product of the involvement should be conscientiously taken into account by the decision-maker.
8.11.20 Separately, bearing in mind the commissioner’s equalities responsibilities, the commissioner should consider carrying out an equality and health inequality impact assessment (EHIA), to check whether any specific groups of people require specific or enhanced forms of involvement.
Procurement
8.11.21 Practice mergers often require the commissioner to either:
- mutually agree the termination of existing contracts and directly award a new contract to a new legal entity; or
- terminate existing contracts and then significantly vary one contract to add all the terminated services
8.11.22 The commissioner’s consent is required to vary any terms (for example, the services, performance standards or pricing) of any GP contract.
8.11.23 Statutory guidance on the provisions of the PSR are clear that mergers may involve major modifications to contracts or constitute a new contract. Mergers that result in the same services continuing, albeit with different groups or individuals, under one of the previously existing contracts, may be a permitted contract modification under the regime. However, mergers that result in material modifications to the contract, such as a material change to the services, may require a new contract and therefore a PSR process. Commissioners should refer to the PSR regulation and the PSR statutory guidance.
Other matters
8.11.24 These may include but not limited to the effect of the practice merger on:
- the provision and/or contracting out of minor surgery, enhanced and locally commissioned services
- out of hours opt-outs
Mergers generally
8.11.25 Generally, contractual mergers should only be considered in cases of like-for-like contracts – that is, GMS with GMS, PMS with PMS and APMS with APMS – because of the differences in terms (including duration) and financial arrangements. However, this does not remove the ability of a PMS provider to request to merge its business with a GMS provider and eventually work under one form of contractual terms.
8.11.26 Commissioners should advise contractors to seek guidance from their representative bodies in this instance to ensure they follow due process and are fully aware of the implications.
8.11.27 It is essential that patients from the terminating contract are included under the remaining contract through bulk transfer where possible to avoid additional cost pressure.
8.11.28 The commissioner must bear in mind that despite avoiding this additional cost, once patients are under the new contract, the Carr-Hill formula will be applied and may then increase the cost of the transferring patients based on one of the other factors, such as rurality, when it may not have applied to the terminating contract.
8.11.29 The Carr-Hill allocation formula is used to adjust the global sum payment for a number of local demographic and other factors, which may affect a practice workload. For example, a practice with a large number of elderly patients may have a higher workload than one that primarily cares for commuters.
8.11.30 The factors included in the Carr-Hill formula are:
- patient age and gender (used to reflect frequency of home and surgery visits)
- additional needs: standardised mortality ratio and standardised long-standing illness for patients under the age of 65 years
- number of newly registered patients (generate 40% of work in first year)
- rurality
- costs of living in some geographical areas
- patient age/gender for nursing/residential consultations
8.11.31 The commissioner may request that practices proposing to merge collectively submit a business case which the commissioner can use to base its decisions on whether to approve the merger and the consequential contract variations. Annex 51 provides a template business case for practice merger. Annex 52 provides a template mobilisation plan for practice merger which practices can tailor and submit with their business case.
8.11.32 The commissioner will need to amend the template business case to ensure it requests all the relevant information in respect of the merger. The commissioner should therefore seek to engage with the practices early in the development process to shape the business case and to liaise with the practices on any amendments or updates to the business case, to ensure the business case is as comprehensive as possible prior to the commissioner making its decision.
‘Super-practices’
8.11.33 Some mergers involve the creation of so-called ‘super-practices’. Where such a merger is approved by the commissioner in accordance with this section 8.11, it may be that the merger is bringing together the partners of multiple practices by adding them as partners to each other’s existing contracts. This will result in a large group of partners holding a number of primary medical contracts. For this specific scenario, and provided that partners are only being added (with none leaving any of the contracts), commissioners may use the super-practice template variation agreement at annex 53. This allows the various partners to sign a single document so as to affect the addition of all the partners to all the contracts. It can also be used to designate a small number of the partners as authorised signatories in relation to contractual matters going forward. The variation agreement is not for use in any other scenario.
8.11.34 In addition, this variation agreement includes agreement for future changes to the partnership to take effect via a single notification to the commissioner for all the contracts. This applies only where the simplified variation agreement for super-practices is used and in all other cases a change of partners must be dealt with in accordance with section 8.5: Partnership changes.
8.11.35 The super-practice template variation agreement at annex 53 is only for use where multiple contracts will be held by a partnership. While there is no definition of or criteria for a super-practice/partnership, to avoid inappropriate use, NHS England requires that this variation agreement should only be used where a super-partnership is being formed, usually to cover a large geographical area and registered patient population (minimum 30,000), a minimum of 3 contracts (at least one must be a GMS contract) and at least 10 partners. For the avoidance of doubt, this variation agreement should not be used, for example, when merging 2 PMS agreements, regardless of the number of partners.
Delegated commissioning arrangements
8.11.36 The delegation agreement includes a section on approving GP practice mergers and closures. When carrying out such actions, the commissioner is required to act in accordance with the delegation agreement which includes but is not limited to:
- undertaking all necessary consultation when taking any decision in relation to GP practice mergers or GP practice closures, including those set out under section 14Z2 of the NHS Act 2006 (duty for public involvement and consultation). The consultation undertaken must be appropriate and proportionate in the circumstances and should include consulting the LMC
- prior to making any decision, clearly demonstrating the grounds for such a decision and fully considering any impact on the GP practices’ registered populations and those of surrounding practices. The ICB must be able to clearly demonstrate that it has considered other options and has entered into dialogue with the GP contractor as to how any closure or merger will be managed; and
- in making any decisions, taking account of the ICB’s obligations as set out in the delegation agreement in relation to procurement, where applicable
8.12 Changes to services
8.12.1 Commissioners will need to consider changes to local service provision as a consequence of a health needs assessment of the local community with particular regard to the diverse nature of the community and reducing health inequalities in access and outcomes.
8.12.2 The commissioner and the contractor shall only agree to any change to the delivery of services after all legal obligations in respect of consultation, engagement or involvement of the public, patients and other organisations have been fulf
8.12.3 Sections 8.13 to 8.19 below outline the principles and steps required to process the most commonly occurring service changes.
8.13 Open and closed lists
8.13.1 There are circumstances where a contractor may wish to close its list to new registrations: for example, internal capacity issues or premises refurbishment A contractor may also seek to extend a closed list period or open its list again before the end of an agreed period. Further details on how to manage patient lists are set out in chapter 3: Managing patient lists.
8.14 Boundary changes
8.14.1 There may be circumstances when a contractor wishes to change its main practice boundary to either expand or contract the practice area for new registrations due to new re-development, local authority compulsory purchase schemes and/or road developme
8.14.2 Most practices will also have within their contracts a defined outer boundary to allow patients who move home a relatively short distance outside the main boundary and would prefer to stay with their existing practice with which they may have a well-established relationship, to remain register
8.14.3 For the purposes of service provision, the full range of contractual services must be made available to those patients registered with the practice within the outer boundary and the outer boundary area must be treated as part of the practice’s contracted ar
8.14.4 Any changes to the practice area (main and outer boundary) must be considered a variation to the contract and the definitions of these areas amended under a variation notice. The contractor must notify the commissioner of its intent to vary its area in writing, setting out the reasons for the change and full details of the proposed practice area, with any additional supporting evidence that may assist the commissioner in reaching its Annex 54 provides a template application to change the practice area.
8.14.5 The contractor and the commissioner must engage in open dialogue concerning the circumstances that have led to the request to change boundary and discuss the possible implications of the action – that is, a reduced patient register, an expanded patient register and the financial implications of both – and any possible alternative actions that may be taken by either party to enable the practice to maintain its existing practice are
8.14.6 Commissioners must consider the application having regard to other practices’ boundaries, patient access to other local services and other health service coverage within a location and may seek to involve the public to seek their view
8.14.7 Once a decision is reached on whether to accept or reject the application, the commissioner should notify the contractor of its decision in writing Annex 55 provides a template letter to acknowledge an application to change practice area.
8.14.8 If the commissioner accepts the proposed changes to the practice area, the contractor should be notified, as soon as possible, in writing of:
- the acceptance
- the date on which the changes will take effect
- a requirement of the contractor to publish the details of the new practice area within its patient information leaflet and on its website (if it has one)
8.14.9 If the commissioner declines the proposed changes to the practice area, the contractor should be notified, as soon as possible, in writing of that decision and to include:
- the reasons for the decision
- the right of the contractor to appeal and the process for doing so
- specify any period within which the commissioner would not consider a further application from this contractor to vary its practice area
8.14.10 Practices that are intending to reduce their practice area must be advised that registered patients who subsequently fall outside the new agreed area, but who are within the original practice area (main and outer boundary), can only be removed from the list if one or more of the provisions of the relevant regulations/directions that relate to removal of patients from the practice’s patient list apply.
8.15 Premises
8.15.1 A contractor may wish to make changes to its contracted practice premises (including branch surgeries – for further information, see section 8.16: Branch surgeries) from which services are provided.
8.15.2 This would likely be a significant change to services for the registered population and, as such, the commissioner and the contractor must engage in open dialogue in the first instance to consider the consequences and implications of the proposed change and discuss any possible alternatives that may be agreed between them.
8.15.3 The commissioner and contractor, through their dialogue, may establish that there is a need to retain medical service provision in the locality and must seek to find a solution, which could include tendering for a new provider within that locality, though not necessarily within the same premises.
8.15.4 Once, and if, the final date for closure is confirmed, the commissioner will issue a variation agreement notice to remove the registered address from the contract and, as in other variations under this policy, include the wording of the variation and the date on which it will take effect. The commissioner must also inform PCSE about changes to the main site location.
8.15.5 The contractor will be fully responsible for the cessation or assignment of the lease for any rented premises and any disposal of owner-occupied premises.
8.15.6 While it is likely that a PMS agreement/APMS contract would reflect the terms as laid out in the GMS contract, it is essential that the commissioner reviews the individual contract for relevant provisions that relate to removing the closing premises and any rights associated with that prem
8.15.7 Where the premises relocation is in relation to a dispensing doctor’s practice, contract managers should also refer to the Pharmacy manual, as moving the site may have significant implications for which patients are eligible to be dispensed to by the practice.
8.15.8 The practice should also apply separately for permission to relocate the dispensing rights of the practice elsewhere, and the timeframes involved in getting approval for that relocation may influence the broader relocation plans and timetable.
8.16 Branch surgeries
8.16.1 It is important to note that unless there are specific reasons for variation, the addition of branch surgeries to the contract should be held to the same standard of service level as a ‘main surgery’, unless there is specific reason for a lesser service provision. An example may be in rural areas, where the principle is ensuring local access and this would be for local commissioning determination.
8.16.2 A commissioner or contractor request to open a new branch site should be considered based on each individual case. Many of the considerations on whether to close a branch (see section 8.17: Branch closure) will apply equally to establishing if a new branch site is needed and the decisions to agree this and the subsequent contract variation.
8.16.3 Within the context of PCNs, where a practice has one or more branch surgeries in different PCNs, the practice can only be a Core Network Practice of only one PCN, and a non-core member of the other PCN(s) within which the relevant branch surgeries are situated. There is increasing interest in opportunities for realigning branch sites to be a party to a Core Network Practice within the PCN within which it is situated i.e. where currently it is a non-core member. Beyond coordinating reciprocal contract variation actions to affect a branch closure with the current Core Network Practice and opening up a new branch surgery with the intended Core Network Practice there is currently no mechanism to enable a transfer of branch surgeries between practices. Such proposals would draw on the considerations outlined below (Branch Closures).
8.17 Branch closure
8.17.1 The closure of a branch surgery may be due to an application made by the contractor to the commissioner or due to the commissioner instigating the closure following full consideration of the impact of such a closure.
8.17.2 In the circumstances that the commissioner is instigating a branch closure, the commissioner must be able to clearly demonstrate the grounds for such a closure and have fully considered any impact on the contractor’s registered population and any financial impact on the contractor. The commissioner will be expected to demonstrate that it has considered any other options available prior to instigating a branch closure and entering into a dialogue with the contractor as to how the closure is to be managed. The commissioner will need to have complied with the duty (under section 13Q of the NHS Act 2006) to involve patients in decision-making before any final decision to close a branch is made.
8.17.3 Where a contractor wishes to close a branch surgery, the contractor should have preliminary discussions with the commissioner to determine appropriate and proportionate patient involvement requirements prior to the consideration of such a service provision change. Even though the closure is being instigated by the contractor, the commissioner will still need to comply with the section 13Q duty to involve patients in decision-making before any final decision is made.
8.17.4 The closure of a branch surgery would be a significant change to services for the registered population and, as such, the commissioner and the contractor should engage in open dialogue in the first instance to consider the consequences and implications of the proposed change and discuss any possible alternatives that may be agreed between them. At this stage, the duty to involve the public in proposals for change is triggered and the commissioner and contractor should work together on fair and proportionate ways to achieve this. The commissioner should ensure clarity on what involvement activities are required by the contractor.
Contractor and commissioner discussions resulting ultimately in a decision about a branch closure will often include consideration of (but not be limited to):
- financial viability
- registered list size and patient demographics
- condition, accessibility and compliance to required standards of the premises
- accessibility of the main surgery premises including transport implications
- the commissioner’s strategic plans for the area
- other primary healthcare provision within the locality (including other providers and their current list provision, accessibility, dispensaries and rural issues)
- dispensing implications (if a dispensing practice)
- whether the contractor is currently in receipt of premises costs for the relevant premises
- other payment amendments
- possible co-location of services
- rurality issues
- patient feedback
- any impact on groups protected by the Equality Act 2010 (for further detail see part A, chapter 2: General duties of NHS England)
- the impact on health and health inequalities
- any other relevant duties under part 2 of the NHS Act (for further detail see part A, chapter 2: General duties of NHS England)
8.17.5 The commissioner and contractor, through their dialogue, may establish that there is a need to retain medical service provision in the locality and must find a solution, which could include tendering for a new provider within that locality though not necessarily within the same premises. Note that most changes in premises will trigger the commissioner’s duties to involve patients in decision-making.
8.17.6 The commissioner should confirm any such arrangements and agreements in writing to the contractor as soon as is practicably possible after the agreement is reached and must notify PCSE of any branch closures, so that PCSE can update the record of the GP practice. Please note PCSE does not provide services connected to a branch site closure. If the practice or commissioner wishes to use PCSE to inform patients or to move paper medical records, this will need to be commissioned separately with PCSE.
8.17.7 If the commissioner and the contractor are unable to reach an agreement to keep the branch surgery open, then the contractor, based on its previous discussions with the commissioner regarding appropriate and proportionate involvement, will continue to involve patients in the proposed changes.
8.17.8 The contractor is required to follow:
- statement of arrangements and guidance on patient and public participation in commissioning
- framework for patient and public participation in primary care commissioning
8.17.9 The process for patient and public participation should be as appropriate to the arrangements agreed with the commissioner, with support and advice as appropriate from the commissioner. Adherence to the patient and public participation involvement process will help ensure that an appropriate involvement exercise is carried out, one that meets the legal obligations on the commissioner.
8.17.10 Once this involvement exercise has been undertaken and the results provided to the commissioner, the contractor would then submit a formal application to close the branch surgery to the commissioner for consideration. Annex 56 provides a template application notice to close branch premises.
8.17.11 The commissioner will then assess the application regarding the closure and the outcome of the patient involvement exercise with a view to either accepting or refusing the proposal. These assessments will need to again consider all the relevant factors, including those listed in 8.17.4. The commissioner should document how it has taken the various factors into account.
8.17.12 Either the contractor or the commissioner may invite the LMC to be a party to these discussions at any time.
8.17.13 Where the commissioner refuses the branch closure through its internal assessment procedure, the contractor shall be notified in writing within 28 days following the internal assessment and the contractor may then follow the relevant resolution process as referenced in the contract. Please refer to annex 57: acknowledgment of application to close branch premises.
8.17.14 Where the commissioner approves the branch closure, the commissioner will need to ensure that it retrieves all NHS owned assets from the premises.
8.17.15 The contractor remains responsible for ensuring the transfer of patient records (electronic and paper Lloyd George notes) and confidential information to the main surgery, having full regard to confidentiality and data protection requirements, records management: NHS code of practice guidance and any relevant guidance from NHS England or the Information Commissioner’s Office. Where a third-party contractor is being used to handle records, it must be vetted and appropriate contractual arrangements put in place.
8.17.16 The contractor remains responsible for carrying out public involvement in accordance with the instructions given by the commissioner and informing the registered patients of the proposed changes. However, ultimately it is the commissioner’s responsibility to ensure that involvement activities have met legal requirements, even if carried out by the contractor. Further guidance can be found in the NHS England documents listed in 8.17.8.
8.17.17 Once the final date for closure is confirmed, the commissioner will issue a standard variation notice to remove the registered address of the branch surgery from the contract, including the amended sections of the contract for completeness.
8.17.18 Where the contractor has previously been granted premises consent to dispense and these rights are only associated with the closing premises in question (that is, listed on the relevant dispensing contractor list), the contractor’s consent to dispense will cease.
8.17.19 The commissioner shall update its records and ensure that the relevant dispensing contractor list is updated appropriately to reflect the removal of the premises.
8.17.20 It is possible that a PMS agreement or APMS contract will reflect the terms as set out above. It is however essential that the commissioner reviews the individual contract for these or any other relevant provisions to allow a variation to effectively remove the closing premises and any rights associated with that premises alone.
8.18 Service opt-outs
8.18.1 Services under primary medical contracts are categorised as:
8.18.2 Essential services – these are the services described in Regulation 15 of the GMS Regulations which a GMS contractor must provide. Essential services are not mandatory for PMS or APMS
8.18.3 Minor surgery and out-of-hours services – these are specific services that are additional to essential services. It is not mandatory for contractors to provide these services but where GMS and PMS contractors provide such services, the contracts must contain terms relating to the procedure for opting out of those services. It is not a requirement that APMS contracts contain such opt-out provisions but the commissioner should review the relevant APMS contract to determine whether any such provisions have been included; or
8.18.4 Enhanced services – these are any services that go beyond essential, minor surgery or out-of-hours services that the contractor may have agreed to be included.
8.18.5 Where a contractor has opted out of delivering minor surgery or out-of-hours services, the commissioner must commission these services from an alternative source for the registered patients under that contract.
8.18.6 Prior to any opt-out taking effect, the commissioner and the contractor shall discuss how to inform the contractor’s patients of the proposed opt-out. The commissioner can request that the contractor informs its registered patients of an opt-out and the arrangements made for them to receive minor surgery or out-of-hours services by either placing a notice in the practice’s waiting rooms or including the information in the practice leaflet.
8.18.7 The regulations do not refer to opt-ins – that is, where a contractor wishes to provide services which it previously opted out of providing. If the commissioner receives a request to opt-in, it should refer to its legal team for consideration of the procurement implications.
Opt-out of minor surgery
8.18.8 Where a contractor wants to opt out of providing minor surgery services, the contractor must notify the commissioner in writing stating the reasons for wishing to opt ou This notice is referred to as a preliminary opt-out notice.
8.18.9 As a next step, the commissioner must discuss with the contractor what support the commissioner may give the contractor to enable the contractor to continue to provide minor surgery. The parties must also discuss other changes which could enable the contractor to continue providing the service. These discussions must be started as soon as is reasonably practicable and in any event within 7 days from the date the preliminary opt-out notice is received. The commissioner and the contractor must use reasonable endeavours to enable the contractor to continue to provide minor surgery.
8.18.10 The discussions must be completed within 10 days from the date the preliminary opt-out notice is received or as soon as reasonably practicable after the 10 days.
8.18.11 If, after the discussions, the contractor still wishes to opt out of minor surgery, the contractor must send an opt-out notice to the commissioner which must include:
- whether the contractor wishes to temporarily or permanently opt out
- the reasons for wishing to opt out
- the date from which the contractor would like the opt-out to commence, which must:
- in the case of a temporary opt-out, be at least 14 days after the date of service of the opt-out notice
- in the case of a permanent opt-out, must be the day either 3 or 6 months after the date of service of the opt-out notice
- in the case of a temporary opt-out, the desired duration of the opt-out
8.18.12 The contract regulations do not allow contractors to temporarily opt out of providing minor surgery more than twice. Where a contractor has given 2 previous temporary opt-out notices within the period of 3 years ending with the date of the service of the latest opt-out notice, the commissioner must treat the latest opt-out notice as a permanent opt-out (even if the notice says that the contractor wishes to temporarily opt-out).
Temporary opt-out of minor surgery
8.18.13 Where the contractor has provided a temporary opt-out notice, the commissioner must follow the process below:
- the commissioner must, as soon as is reasonably practicable and in any event within the period of 7 days from the date the temporary opt-out notice is received, either:
- approve the opt-out notice and specify both the date on which the temporary opt-out is to commence (which wherever reasonably practicable must be the date requested by the contractor in its opt-out notice) and the date that it is to come to an end (“the end date”); or
- reject the opt-out notice on the ground that the contractor:
- is providing minor surgery to patients other than its own registered patients or enhanced services
- has no reasonable need temporarily to opt out having regard to its ability to deliver minor surgery
- notify the contractor whether it has approved or rejected the opt-out notice as soon as possible, including reasons for its decision
8.18.14 The commissioner or the contractor may have concerns about the ability of the contractor to provide the services at the end of the temporary opt-out. If the commissioner considers that the contractor will not be able to satisfactorily provide minor surgery at the end of the temporary opt-out, it can agree with the contractor to extend the end date. If such extension is not possible, the commissioner may notify the contractor in writing at least 28 days before the end date that a permanent opt-out shall immediately follow the temporary opt-out. Similarly, a contractor that has temporarily opted out may, at least 3 months prior to the end date, notify the commissioner in writing that it wishes to permanently opt out of minor surgery.
Permanent opt-out of minor surgery
8.18.15 Where the contractor has provided a permanent opt-out notice, the commissioner must approve or reject it. The commissioner must do so as soon as is reasonably practicable and in any event within the period of 28 days from the date on which the permanent opt-out notice is received. The only ground on which the commissioner may reject the notice is that the contractor is providing minor surgery to patients other than its registered patients or enhanced services. The commissioner must notify the contractor of its decision as soon as possible, including reasons for its decision where its decision is to reject the opt-out notice.
8.18.16 If the contractor wishes to withdraw the notice after the commissioner has approved a permanent opt-out, it can only do so if the commissioner agrees. This is because after approving the opt-out, the commissioner may have made arrangements for the contractor’s registered patients to receive minor surgery from an alternative provider.
8.18.17 It may be difficult for the commissioner to find an alternative provider to deliver minor surgery from the date on which the contractor proposes to opt out. Where this is the case, the commissioner must notify the contractor 1 month before the proposed opt-out date that it requires the contractor to continue to provide minor surgery for a certain period as set out below.
8.18.18 Where the proposed opt-out date is 3 months after service of the opt-out notice (if 6 months, see 18.20), the contractor shall continue to provide minor surgery until the day 6 months after the service of the opt-out notice. If during this period, the commissioner, despite using its reasonable endeavours, is still unable to find an alternative provider, it can provide a further notice to the contractor requiring the contractor to provide minor surgery until the day 9 months after the date of service of the permanent opt-out notice.
8.18.19 The contractor may find it difficult to continue providing minor surgery for a further 9 months. Therefore, as soon as is reasonably practicable and in any event within 7 days of the commissioner serving a further notice to the contractor to continue providing minor surgery until 9 months after the date of service of the permanent opt-out notice, the commissioner must enter discussions with the contractor. These discussions must consider what support the commissioner may give to the contractor or other changes which either party may make in relation to the provision of minor surgery until the actual opt-out date. The requirement to enter discussions only arises where the commissioner requires the contractor to provide minor surgery until the date 9 months after service of the opt-out notice. It does not apply where the commissioner requires the contractor to provide minor surgery until the day 6 months after service of the opt-out notice.
8.18.20 Where the proposed opt-out date is 6 months after service of the opt-out notice, the contractor shall continue to provide minor surgery until the day 9 months after the service of the opt-out notice.
8.19 Opt-out of out of hours
8.19.1 If a contractor wishes to terminate its obligation to provide out-of-hours services, it must provide the commissioner with an out-of-hours opt-out notice specifying the date from which the contractor would like the opt-out to take effect, which must be either 3 or 6 months after the date of service of the out-of-hours opt-out notice.
8.19.2 As soon as is reasonably practicable and in any event within 28 days of receiving the out-of-hours opt-out notice, the commissioner shall approve the notice and confirm the date on which the out-of-hours opt-out is to commence. The commissioner cannot reject an out-of-hours opt-out notice.
8.19.3 If the contractor wishes to withdraw the out-of-hours opt-out notice after the commissioner has approved it, it can only do so if the commissioner agrees. This is because after approving the opt-out, the commissioner may have made arrangements for the contractor’s registered patients to receive the out-of-hours service from an alternative provider.
8.19.4 If the commissioner cannot find an alternative provider, above will apply as if the reference to minor surgery was a reference to the out-of-hours service.
8.19.5 Once the terms of any permanent or temporary opt-out are agreed, a variation notice must be issued in accordance with the principles laid out in this policy to amend the relevant section of the contract.
8.19.6 The commissioner should follow the same process for PMS contractors. For APMS arrangements, the commissioner should review the contract to determine whether it contains any relevant provisions.
8.20 Financial changes – Statement of Financial Entitlements (SFE)
8.20.1 The contract will contain the terms of any payments d Any change to those terms will require a notice of variation which should be provided no less than 28 days before the proposed variation takes effect.
8.20.2 For GMS contracts, the financial terms must reflect those set out in the GMS SFE. There is no such requirement under PMS agreements or APMS contracts which have been locally agr NHS England does however have a policy of equitable funding for the core services expected of all GP practices. Any changes under the GMS SFE should be reviewed against the terms of each of the individual contracts to ascertain what, if any, affect those changes have on local financial terms.
8.21 Primary care support services notifications
8.21.1 Commissioners should ensure that following any contractual merger, GP performers are informed of their obligation to notify Primary Care Support England (PCSE) using the relevant online portal or forms issued by NHS England within 28 days.
8.21.2 Additionally, and more generally, GP performers and indeed performers in all contractor groups are required to notify PCSE of any changes relevant to their entry on the national performers list. Further information is available on the PCSE website.
9. Managing a PMS contractor’s right to a GMS contract
9.1 Introduction
9.1.1 The aim of this policy is to ensure that all parties to the contract understand the process and procedures that must be followed when a contractor requests a transfer from a PMS agreement to a GMS contract.
9.1.2 Subject to the contractor’s eligibility to hold a GMS contract and the requirement to provide essential services, then there should be no variation in the application of this policy.
9.2 Roles and responsibilities
9.2.1 Commissioners will need to ensure that the finance department and relevant persons are made aware of the change to the contracting arrangements as there will be long-term financial implications. A GMS contract is not time limited and exists in perpetuity. Anyone with delegated authority can sign off the transfer.
9.2.2 The payment and contract management system must be updated by the officer managing the transfer.
9.3 Background
9.3.1 A contractor holding a PMS agreement which is providing essential services has the right to a GMS contract in accordance with Regulation 32 of the PMS Regulations which states:
“A contractor which is providing essential services and which wishes a general medical services contract to be entered into pursuant to this regulation shall notify [the commissioner] in writing at least 3 months before the date on which it wishes the general medical services contract to be entered into”.
9.3.2 This policy sets out the decision-making process that the commissioner will follow, together with refusal (where eligibility is not satisfied), appeal processes and discussions regarding any actions that are required.
9.4 Notification from a contractor
9.4.1 The commissioner should receive at least 3 months’ notice in writing from the contractor requesting a GMS contract.
9.4.2 The contractor’s notice must:
- state that the contractor wishes to terminate the PMS agreement
- state the date on which the contractor wishes the PMS agreement to terminate which must be at least 3 months after the date of service of the notice
- give the name of the person(s) with whom the contractor wishes the commissioner to enter into a GMS contract (a person’s name may only be given in a notice if that person is a party to the PMS agreement)
- confirm that the person(s) named meet the conditions set out in section 86 of the NHS Act 2006 (persons eligible to enter into GMS contracts) and Regulations 4 and 5 (where applicable) of the GMS Regulations or, where the contractor is not able to confirm, the reason why it is not able to do so and confirmation that the person(s) immediately prior to entering into the GMS contract will meet those conditions
9.5 Process for PMS agreements
9.5.1 The commissioner must acknowledge receipt of the notice within 7 days from the day the notice is received.
9.5.2 While it is not a requirement of the PMS Regulations, when the commissioner receives such a notice it should discuss the full implications of this action with the contractor to ensure the contractor has fully understood the necessary changes to the contractual income streams (see 9.5.4) and should advise the contractor to seek its own independent advice.
9.5.3 The commissioner will check that all necessary information has been provided in the contractor’s notice and undertake a review of the PMS agreement to establish if the contractor provides essential services; and if it is eligible to hold a GMS contract (as set out in section 86 of the NHS Act 2006 (persons eligible to enter into GMS contracts) and Regulations 4 and 5 of the GMS Regulations. This information is referenced in chapter 1: Contracts described.
9.5.4 The commissioner must apply the GMS SFE on first setting up a GMS contract and calculating the global sum monthly payment. While a PMS contractor has the right to a GMS contract, there is no entitlement for the contractor to carry the same funding arrangements it had under the PMS agreement into that GMS contract. GMS contracts are funded according to terms set out in the GMS SFE while PMS agreements are funded through local agreement. There is the discretion to agree additional payments under GMS arrangements outwith the GMS SFE and which are not necessarily payable under the GMS SFE. It is essential that the commissioner has ascertained the financial impact of the contractor’s decision to move to a GMS contract.
9.5.5 If the contractor does not provide essential services, the commissioner must notify the contractor that they are not entitled to transfer to a GMS contract. Annex 58 provides a template letter.
9.5.6 If the contractor is not eligible to hold a GMS contract the commissioner must refuse to enter into a GMS contract. Annex 59 provides a template letter.
9.5.7 If the commissioner confirms that the contractor provides essential services and is eligible to hold a GMS contract under section 86 of the NHS Act 2006 and Regulations 4 and 5 of the GMS Regulations, the commissioner will acknowledge receipt of the notice and outline the next steps within 7 days of receipt of the notice. Annex 60 provides a template letter.
9.5.8 The GMS contract will start immediately after the termination of the PMS agreement. The GMS contract start date should be the date set out in the notice to the commissioner unless a different date is agreed by the parties. The GMS contract will include all the terms required by the GMS Regulations.
9.5.9 The new GMS contract must require the provision of the same services that were commissioned under the PMS agreement and were provided by the contractor immediately prior to the PMS agreement terminating unless the parties otherwise agree.
9.5.10 The names of the patients included in the contractor’s list of patients immediately before the PMS agreement termination must be included in the first list of patients prepared and maintained by the commissioner.
9.5.11 The out-of-hours services must be the same as were provided under the PMS agreement before it terminated.
9.5.12 The commissioner must use the current standard GMS contract ensuring that it is amended to the specific contractor.
9.5.13 Once a GMS contract is agreed and entered into and the PMS agreement has terminated, the commissioner must ensure all nationally held records of the contractor’s status are adjusted appropriately. This must include, but not be limited to, changing the contractor’s status on the Calculating Quality Reporting Service (CQRS), from PMS to GMS, to ensure that the correct quality and outcomes framework calculations are completed at year-end and any contractual payment systems are used (that is, Exeter).
9.5.14 The calculation of the contractor’s first initial global sum monthly payment must be made in accordance with part 1 of the GMS SFE.
9.6 Disputes
9.6.1 Where there is a dispute about whether or not a person satisfies the conditions set out in section 86 of the NHS Act 2006 or Regulations 4, 5 and 6 of the GMS Regulations, the contractor may appeal to the First-Tier Tribunal.
9.6.2 Any other dispute about the GMS contract shall be determined by the Secretary of State [NHS Resolution (NHSR) – Primary Care Appeals (PCA)] in accordance with Regulation 9(2) and (3) of the GMS Regulations (pre-contract disputes).
9.6.3 The commissioner can identify whether the contract is an NHS contract or not by reviewing the agreement. This will enable the commissioner to identify whether it can apply for NHS dispute resolution (with or without the need for the written consent of the contractor) if appropriate.
10. Practice closedown (planned/scheduled)
10.1 Introduction
10.1.1 This policy outlines the approach to be taken when a time-limited primary medical services contract is coming to an end. Where an urgent contract needs to be put in place, please refer to part B, chapter 1: Contracts described for further information).
10.2 Scope
10.2.1 Time-limited contracts can be in place regarding GMS contracts, PMS agreements and APMS contracts. GMS contracts, however, do not usually have an end date but a temporary GMS contract can be put in place for a period not exceeding 12 months, for the provision of services to the former patients of a contractor following the termination of that contractor’s contract.
10.2.2 PMS agreements may be in perpetuity or for a time-limited period. Commissioners should review the relevant PMS agreement to establish if there is a defined end date.
10.2.3 APMS contracts must be for a fixed-term period, the duration of which may be governed by the commissioner’s standing financial instructions and is subject to NHS England regional sign-off. Commissioners should retain a schedule of all their APMS contract end dates to support planning.
10.2.4 In each of the cases above there are generic principles that will apply and individual circumstances that will need to be considered. This policy covers the steps to be taken in advance of the end of any contract and will support the commissioner in planning procurement cycles and future service provision.
10.2.5 The commissioner must consider whether the expiring contract contains provisions relating to the end of the contract that impact on any practice closedown actions. The NHS England standard primary medical service contracts contain provisions relating to the consequences of termination, including a requirement that the contractor co-operates with the commissioner, and arrangements for a financial reconciliation exercise.
10.26 Contracts may come to an end by reasons other than by expiry including by:
- being terminated by either the commissioner or the contractor (in which case refer to part C, chapter 1: Contract breaches, sanctions and terminations)
- an adverse event (in which case refer to part C, chapter 5: Adverse events)
- the death of the contractor (in which case refer to part C, chapter 3: Death of a contractor)
- retirement of the contractor (in which case refer to section 8.6: retirement of a contractor – single handed and section 8.7: retirement of a contractor – 2 or more partners/individuals)
10.3 Timetable for managing contracts coming to an end
10.3.1 The commissioner needs to be aware of the end dates of all contracts held so that advance planning can be undertaken to ensure both capacity and timescales can be aligned with the key stages outlined below.
10.3.2 It is essential that the commissioner ensures continued communication with contractors throughout the stages to enable them to have a clear understanding of the processes, expectations and obligations. Annex 61 provides a guide to communications with practices and Annex 62 provides a proposed checklist for documentation recording when contract ends.
10.3.3 Commissioner should also refer to PCSE’s practice mergers and closures process. In the case of a planned closure, the commissioner should involve PCSE in the process as soon as possible but not later than 14 days of when a closure/merger is to take effect.
10.3.4 In each of the stages below there is a range of actions that may need to be undertaken, depending on the commissioner’s preferred route, and the commissioner may usually discuss actions with the appropriate LMC throughout.
10.4 Summary of key stages
10.4.1 Stage 1 – minimum 9–15 months before contract end (all essential):
- needs assessment
- impact
- engagement proposal
10.4.2 Stage 2 – 12 months before contract end:
- notice period – exit plan
- commence procurement and either:
- begin negotiations for continuation with contractor; or
- begin exit arrangements of incumbent provider and mobilisation of any new provider
10.4.3 Stage 3 – at contract end:
- contract end – possible dispersal of patient list
- variation to contract/extension
- commencement of new provider
10.5 Stage 1 – 9–15 months before contract end
10.5.1 The considerations that should be given when completing each action are provided below. This list is not exhaustive but does provide a platform for commissioners to fully assess the existing and future service needs of its population. Commissioners should ensure that all appropriate stakeholders are given the opportunity to input into the needs assessment for their population, including but not limited to public health.
a. Needs assessment
10.5.2 Is there still a demand for this service in this locality and a requirement for it to continue? – for example, to reduce inequalities in access or health
10.5.3 Does the contract specification still address current local priorities?
10.5.4 Has the contract delivered on the expected outcomes?
10.5.5 Has it provided added value to the local population and service provision?
10.5.6 Have you assessed the potential service needs for any forthcoming new developments?
10.5.7 What is the capacity of other local providers and the market for other providers to deliver services?
10.5.8 Have you given consideration to any specialist services needs in the locality?
10.5.9 Are there any needs that are not met by the contract, which could be delivered?
b. Impact
10.5.10 Have you considered available outcome and delivery data held nationally and locally, regarding the current service and impact on other providers?
10.5.11 Have you compared the cost of the current service against other providers – that is, cost per head of population while taking into account any differences in the scope of the services provided?
10.5.12 Is the current service still affordable within projected future budgets?
10.5.13 Has the contract delivered on the expected financial outcomes?
10.5.14 What other objectives might be set within the existing budget?
10.5.15 Have you considered the potential impact on service users/patients?
10.5.16 Have you considered the potential impact on other service providers: for example, GPs, pharmacy, local trust, out of hours, community services?
10.5.17 Have you considered the potential impact on the current provider – that is, continued viability within the locality?
10.5.18 Have you considered patient choice and equality?
10.5.19 Have you considered the potential risks – that is, reputational (adverse publicity, commissioner/provider relationship), market testing, timescales and financial?
10.5.20 Have you considered how the expiry of the contract affects compliance with the general duties? For further information, please refer to part A, chapter 2: General duties of NHS England.
c. Engagement proposal
10.5.21 Each situation will need to be managed regarding each individual circumstance and the nature of the procurement process to be followed, if at all. However, where it has been deemed appropriate to complete a form of engagement before taking action, the commissioner should consider:
10.5.22 Have arrangements been made for the involvement of patients and the public (please refer to part A, chapter 2: General duties of NHS England) for more information on this requirement)?
10.5.23 Have other local providers and other interested parties – that is, LMC, local members of parliament, review and scrutiny committee, etc – been engaged?
10.5.24 Have the local ICBs been engaged?
10.5.25 If the answer is ‘no’ regarding any of the above, the commissioner should be able to identify the grounds under which it felt engagement was unnecessary and these should be included in the report defined below.
10.5.26 Completion of stage 1 will provide all the information required to enable the commissioner to make an informed commissioning decision on whether to recommission, procure or allow the service to end. At this stage, the commissioner should develop a detailed report about the investigations undertaken, engagement and outcomes. This report shall demonstrate that the commissioner has considered all possible options and the rationale behind the decision taken. Annex 63 provides a template detailed report.
10.6 Stage 2 – 12 months before contract end
10.6.1 Below are the potential next actions following stage 1 based on the commissioner’s decision regarding the proposed way forward. It is important to note that where a contract has a duration or an end date specified, and the intention is to allow the contract to naturally expire, there is no requirement to issue a formal termination notice. It would be best practice to issue a formal letter of notice detailing the commissioner’s intentions and the obligations on the contractor throughout the remainder of the contract period.
a. Notice period – exit plan
10.6.2 Issue a letter of notice of intentions.
10.6.3 Develop an exit plan with the contractor with clearly defined commissioner/contractor responsibilities. This should be developed whether the contract is to cease or transfer to a new provider. The commissioner should review the contract and ensure any exit arrangements detailed in the contract are followed. Annex 64 provides a template exit plan.
b. Procurement
10.6.4 Ensure any new contract is procured in accordance with the Provider Selection Regime (PSR). Commissioners must also act in accordance with any procurement protocol issued by NHS England.
10.6.5 Once a preferred provider is established, agree an operational management plan. Annex 65 provides a template operational management plan – this template should only be used where the contract does not contain exit arrangements as any such arrangements take precedence over the template.
c. Begin negotiations for continuation of the contract with the existing contractor, if appropriate
10.6.6 Extending any contract beyond a previously agreed end date could be considered a material change to the terms of that contract. Commissioners must ensure that they comply with the provisions for contract modifications in the PSR, as well as the terms of the specific contract.
10.6.7 If there is no extension period already included in the contract, the commissioner will need to consider carefully whether such an extension should instead be subject to a provider selection process. Where the current provider’s contract is coming to an end, the number of providers available to patients is limited by the relevant authority, the relevant authority wishes to continue with the existing provider and decides that the current provider is satisfying the existing contract and will likely satisfy the proposed contract to a sufficient standard (taking into account the key criteria and applying the basic selection criteria) and the proposed contract is not changing considerably, the contract for continuation of existing services may be awarded to the existing provider under direct award process C.
10.6.8 If the commissioner’s decision is that no procurement process is necessary, then it must ensure it is aware of the necessary steps which must be taken to satisfy the PSR and any procurement protocol issued by NHS England.
10.6.9 Once the decision to extend has been reached and all correct processes have been followed the commissioner will need to consider:
- the length of the extension
- any alterations to the existing contract (including the financial arrangements)
- any agreement of new key performance indicators
d. Begin exit arrangements (completion of stage 2)
10.6.10 Completion of stage 2 will provide the commissioner with the firm foundations and detailed preparations ready to manage the end of the contract.
10.7 Stage 3 – at contract end
Below are the possible outcomes culminating from stages 1 and 2.
a. Contract end
10.7.2 Dispersal of list if applicable (please refer to part C, chapter 1: Contract breaches, sanctions and terminations and part C, chapter 2: Unplanned/unscheduled and unavoidable practice closedown, section 2.5 regarding orphan data.
10.7.3 Communication to be sent to all parties involved: for example, management of patient communication working with the provider, management of the press, notification of contract end to relevant stakeholders.
b. Variation to contract – extension
10.7.4 Contract variation issued and signed off by both parties.
c. Commencement of the new provider
10.7.5 Issue of a new contract.
10.7.6 Operational management plan implemented.
10.7.7 Relevant communications undertaken, internally and externally.
10.7.8 On completion of stage 3, the commissioner will have reached an agreed, structured outcome about the management of contract end.
10.7.9 As part of any practice closedown, PCSE makes a site visit to remove, store and forward patient records to a new provider(s). Patient records should contain reprints of electronic records for patients who have not re-registered at the point of practice closure and will need to be individually placed in transit polytopes. Records will only be collected from the closing practice’s main site. The GP practice should send PCSE a list of records that are being collected. Records are held in archive until the patient re-registers or the retention period expires, and then they are securely destroyed.
10.7.10 Commissioner should ensure completion of the dispersal of all registered patients from the closed practice immediately following the contract end date and within 6 months at the very latest, as after this date the practice is classified as closed on national IT systems. This includes reconciling any patients who may have chosen not to re-register, ghost patients, etc.
10.8 Primary care networks
10.8.1 When new services are procured, the commissioner should facilitate a discussion between the incoming contractor and the relevant primary care network (PCN) and involving the relevant LMC, to ensure uninterrupted network services for the incoming contractor’s registered patients.
10.8.2 If the provider is not willing to join the PCN, then the commissioner will work with the existing PCN core network practices to ensure continuity of services to the registered patients of the practice not signed up to the Network Contract DES.
10.8.3 If the PCN is not prepared to accept the provider as a member, the commissioner may require a PCN to include the practice as a core network practice of that PCN. Where the commissioner is minded to require a PCN to do so, the commissioner must engage with the relevant LMC and, when making its determination, have regard to the views of the LMC. Section 4.6 of the sets out the process for allocating a practice to a PCN.
10.9 Links to relevant PCSE information and documentation
11. Discretionary payments (made under section 96 of the NHS Act 2006)
11.1 Introduction
11.1.1 Section 96 of the NHS Act 2006 (as amended) makes provisions for NHS England (delegated to local commissioners) to provide assistance and support to primary medical services contractors, including financial support.
Section 96 Assistance and support: primary medical services states:
(1) NHS England may provide assistance or support to any person providing or proposing to provide –
(za) primary medical services pursuant to section 83(2),
(a) primary medical services under a general medical services contract, or
(b) primary medical services in accordance with section 92 arrangements.
(2) Assistance or support provided by NHS England under subsection (1) is provided on such terms, including terms as to payment, as NHS England considers appropriate.
(3) “Assistance” includes financial assistance.
11.1.2 For clarity of purpose, assistance and support relates to the provision of:
- education or training
- financial assistance
- any other resources available to NHS England or the commissioner
11.1.3 However, NHS England is increasingly being expected to demonstrate publicly what it is spending its money on and what it is getting for its money, and to demonstrate that it allocates funding to support initiatives fairly and in the best interests of the organisation and public funds. As such, when providing any financial assistance, the commissioner must be able to demonstrate that you have acted with propriety, that you have understood and complied with any wider financial requirements as set out in the NHS England standing financial instructions, that you have followed all steps to provide best value for money and that you have followed requirements in relation to public sector bodies as stipulated in HMT managing public money (May 2023).
11.2 Key principles
11.2.1 All financial assistance must be provided within the principles of openness, fairness, probity and accountability.
11.2.2 The provision of financial assistance should not conflict with UK policies and actions including the rules on fraud, bribery and corruption, competition, state aid and other equality duties.
11.2.3 It must be demonstrated how the financial assistance supports NHS England and local commissioner functions and strategic objectives.
11.2.4 Financial assistance must demonstrate value for money and be in the best interests of NHS England, local commissioners and the patients.
11.2.5 Financial assistance must be proportionate to the identified need and represent better value for the taxpayer than alternative solutions.
11.2.6 Financial assistance will only be made available in exceptional circumstances and NHS England (delegated to the local commissioner) has the statutory duty to determine the payment terms.
11.3 Programme and non-programme financial assistance
11.3.1 Section 96 exceptional discretionary funding is generally used to safeguard patients’ interests by providing additional funding to support persons or public authority bodies, as listed in section 11.1: introduction, facing a crisis situation.
11.3.2 Formal national programmes of support do not cover or replace all circumstances where there is a need for support and agreement on eligibility for funding support from local primary care budgets. Their proposed use – and the amount provided – will still generally need to be managed by individual local commissioners. When setting up a new section 96 financial assistance scheme, commissioners should seek legal advice as some section 96 payments may constitute a subsidy and be subject to the relevant control regime.
11.3.3 The pressures on general practice mean that requests for support are being received more frequently with a consequent need to have a more structured approach to considering and approving such expenditure outside formal programmes.
11.3.4 It is also important to ensure that ad-hoc requests are minimised through proactive work with practices via appropriate programmes of support that may be in place.
11.4 Process for financial assistance for individual provider
Section 96 financial assistance application process for GP practices (updated for delegated ICB commissioning)
| Step | Process description |
|---|---|
| 1 | The practice raises its sustainability issue with its ICB contract officer to discuss issues. Verify contract payments are correct. |
| 2 | Practice submits a section 96 application functional excel template accompanied by the level of support requested, for what period, and for the type of expenditure with evidence provided to support application and ICB support. |
| 3 | Primary care team review submission and, if necessary, request further information/supporting documentation to produce a business case. |
| 4 |
Following review and validation of the practice information, a business case for the proposed financial assistance must be completed. This must confirm:
|
| 5 |
Review of financial evidence including certified accounts for the previous year and management accounts for the current year, cash flow, declared earnings, etc. Consideration of whether the financial assistance will be sufficient to achieve the objectives. Consideration of value for money versus alternatives. Total likely overall financial risk to NHS England. |
| 6 | Before the application and any required business case is passed for authorisation, the application must be considered and recommended by ICB local arrangements as required. Where, in exceptional circumstances, the financial assistance is above £200,000, the business case must be endorsed by:
|
| 7 | All financial assistance provided must be in compliance with the NHS England standing financial instructions (SFIs). As such, any application for financial assistance must be authorised as set out in the SFIs. The authority levels should be confirmed at the time the financial assistance is provided. |
| 8 | An application from the contractor, along with the commissioner’s business case containing the operational and financial reviews set out above, should be submitted and approved in line with the ICB’s local governance. The NHS England regional team should be informed where financial assistance is above £1 million. The ICB should ensure that financial assistance is approved either in line with its SFIs or as set out in the table below, unless the NHS regional team has specified additional or alternative approval requirements. |
| 9 | All decisions reported as set out below and logged for central reporting and consistency checking. |
| 10 | The practice is advised of outcome. |
| 11 |
MOU populated and signed by the practice and the ICB. The MOU must set out:
|
| 12 | Payment set-up on a non-recurrent basis. |
| 13 | Review of MOU objectives mid-way through period of support. |
| 14 | Routine reporting via the Primary Care Activity Report (PCAR) (see section 11.6: maintaining records and reporting below). |
| 15 | Advise practice of continuation or further review of support depending on MOU progress. |
| 16 | Final review and reporting to local arrangement (as required). |
| Below £50,000 | £50,000 to £200,000 | >£200,000 to below £1 million | Above £1 million |
|---|---|---|---|
| ICB deputy appointed* by director of primary care and public health or director of commissioning, or equivalent senior person | ICB director of primary care and public health or director of commissioning, or equivalent senior person | ICB chief financial officer | ICB chief financial officer and local NHS England regional director or director of finance where this is specified locally by the NHS England regional team or in any delegation agreement |
* For audit purposes and compliance with the governance manual, this must be documented formally.
11.5 Process for commissioner proposed financial assistance programmes
11.5.1 Commissioners may only enter into contracts within the statutory powers delegated to it by the Secretary of State for Health and Social Care and must comply with the following:
- NHS England Scheme of Delegation and standing financial instructions
- other statutory provisions
11.6 Maintaining records and reporting
11.6.1 A clear audit trail of all financial assistance authorised, along with any expenditure incurred under this arrangement, must be maintained and reported. Summary information may be collected by NHS England: for example, through the annual Primary Care Activity Report collection, but commissioners should also maintain adequate records such that you are able to respond to any other routine financial reporting arrangements. Please refer to for authorising and recording individual applications.
11.6.2 All applications for financial assistance should be recorded using the and as set out above.
12. Premises running costs and service charges
Policy for consideration of applications from GP contractors for financial assistance towards premises running costs and service charges.
12.1 Purpose of the policy
To provide a consistent methodology that is fair, transparent and equitable for primary care commissioners to consider formal applications for financial assistance towards premises running costs and service charges in line with the NHS (GMS – premises costs) Directions 2024, part 5, Directions 47 and 48.
12.2 Introduction
The NHS (GMS – premises costs) Directions 2024, part 5, Directions 47 and 48 enable GP contractors to request financial assistance from the commissioner towards premises running costs and service charges that are not reimbursable elsewhere under the directions. The commissioner is required to consider such applications and, subject to budgetary targets, to approve them.
Applications for financial assistance, under Direction 47, in respect of premises running costs, may include costs relating to business rates, Building Improvement District levies, water and sewerage charges, the collection and disposal of clinical waste and certain utilities and other service charges (Directions 47 and 48).
Direction 48(3) offers methods for calculating the amount of financial assistance towards service charges that the commissioner may consider:
- where the amount of the relevant charges can be accurately determined, the amount paid in respect of those charges
- where a lease has been in existence for less than 12 months and the amount of relevant charges cannot be accurately determined, the estimated amount of those charges for the first year of the lease
- where the commissioner has no information as to the amount of those charges, 40% of the amount which the commissioner estimates as being the total yearly service charge
Directions 47 and 48 are provided in full on the gov.uk website.
What the above provisions take no account of is the period in which financial assistance should be provided; what the trigger(s) for a review might be; applications that the commissioner might prioritise over others in light of other budgetary targets; or whether the financial assistance being requested can be mitigated.
This policy seeks to address these issues.
12.3 Principles
For an application for financial assistance to be considered by a primary medical care commissioning organisation, the following principles need to be accepted and adopted by specified stakeholders:
Commissioners will:
12.3.1 Prioritise formal applications from GP contractors that have already been made or those from practices proposing to occupy Local Improvement Finance Trust, NHS PS (property services) or NHS trust buildings on a head or sub/under lease basis, in recognition of the commissioner’s budgetary targets. This does not preclude GP contractors in other tenancy arrangements or those considering entering new tenancy arrangements making an application to primary care commissioners for financial assistance towards their premises running costs or service charges, but it recognises that higher service charge costs are more typically evidenced by practices occupying or proposing to occupy NHS owned or head leased premises. This prioritisation is further evidenced within the local estates’ strategies, developed by ICBs with a wide range of local stakeholders, which seek to maximise use of existing public estate.
12.3.2 Only consider applications that pass through the eligibility criteria check gateway (section 2.1 refers). This enables primary care commissioners to prioritise applications that demonstrate they have the greatest need, which in turn ensures that a GP contractor does not waste its time on completing and providing information when, ultimately, primary care commissioners are unable to support their application.
12.3.3 Only reimburse amounts in accordance with Directions 47 and 48, unless there are exceptional circumstances which justify reimbursement on another basis. Commissioners should be aware that fuel and electricity charges, buildings insurance costs, the cost of internal and external repairs and the costs of plant, building and grounds maintenance are excluded for reimbursement under Directions 47 and 48.
12.3.4 Make recommendations on applications that have passed through all gateways [please refer to section 12.4: The model (eligibility criteria)] to the relevant commissioner part 2 Primary Care Commissioning Committee. Applications can take a considerable time to process. Should they be subsequently approved, back claims will be with effect from the date that the original application was made.
12.3.5 Offer short-term financial support towards premises running costs and/or service charges to GP contractors where there is evidence that their practice expenses are significantly higher than the latest published averages, as a result of high service charge costs and other practice expenses. In this eventuality, a GP contractor must be prepared to put in place a clear action plan, demonstrating that over the next 12 months it will optimise its income and reduce its expenditure. A further assessment as to whether a GP contractor should remain entitled to further financial support will be undertaken 1 year on by re-running the financial assistance model, subject to a GP contractor’s wish to continue to request such support.
12.3.6 Discontinue financial support to GP contractors towards premises running costs and/or service charges after a 12-month period, where the true cost pressure does not relate to service charge expenses. GP contractors can apply for further support under section 96 of the NHS Act 2006.
12.3.7 Have no direct involvement in managing service charge costs but will require evidence that GP contractors and landlords/head leaseholders have taken appropriate steps to mitigate costs. Steps taken by the incumbents may include, but are not limited to, a formal meeting or correspondence with the landlord or head leaseholder during which the service charge costs were explained and justified. GP contractors should also seek assurance from the landlord/head leaseholder that the service charge costs demonstrate value for money and deliver soft and hard maintenance, in the interests of good estate management and following the principles within the Royal Institution of Chartered Surveyors (RICS) code of practice – service charges in commercial property. The current GP contractor should also show that it has analysed its own service expenditure to identify areas where costs can be reduced.
12.3.8 Have interest both in maintaining the viability of its practices and safeguarding taxpayer monies to ensure value for money is delivered.
12.3.9 Use the latest available GP earnings and expenses report currently published by NHS England to benchmark average PMS/GMS GP contractor’s earnings to expenses ratios, which are used as a yardstick to ensure fair and reasonable application.
12.3.10 Take into account changes in income and expenditure, advising GP contractors about any outlying (based on the above NHS England report) costs in the process.
12.3.11 Always use the average previous year’s annual service charge costs (where applicable) as the practice’s starting contribution to new service charge costs, should a case be made for service charge support. While there is a provision to assume 40% of service charge cost is paid by a GP contractor in the event where no historical information is available, the model assesses financial assistance required by the GP contractor based on actual cost projections and expenses and income ratios.
12.3.12 Test a range of alternative inputs to its model to establish which variables provide the best match to enable the GP contractor to attain average PMS/GMS contract earnings.
In light of the number of variables that can impact on a GP contractor’s ongoing need for financial support towards premises running costs and service charges, these would normally be reviewed on an annual basis, when the relevant information is available, reconciling costs back to the last review period.
GP contractors will:
12.3.13 Agree to full disclosure of income and expenditure on an open book and annual basis. Should GP contractors not wish to be party to an annual review, they will need to propose a one-off fixed term support package, which demonstrates a phasing out of financial assistance, taking into account the known variables.
12.3.14 Not seek to occupy an unreasonable amount of space, taking into account their potential list size; and undertake to share space to mitigate costs, wherever this is practicable.
12.3.15 Take responsibility for assessing the potential for growing their practice list and develop the associated trajectory over the relevant period.
12.3.16 Agree to negotiate and sign a lease at the earliest opportunity, while seeking assurance from the landlord/head leaseholder that the service charge costs being levied are fair and reasonable, in compliance with 12.5.1.
12.3.17 Take responsibility for maximising their NHS income by providing GP services commissioned by local and national NHS and local authority commissioners within their sphere of competence, resources, and affordability, so that the burden of use of public monies for service charge assistance is reduced.
12.3.18 Take responsibility for minimising their practice expenditure by ensuring cost effectiveness and value for money spend.
12.3.19 Demonstrate through a clear action plan agreed with support from the LMC (as necessary), how they intend, over a reasonable period (deemed to be 12 months), to optimise their income and reduce expenditure, where there is evidence that their practice expenses are significantly higher than the latest published averages.
Landlords/head leaseholders will be expected to:
12.3.20 Ensure the proposed service charge costs being levied are fair and reasonable, and they have a clear strategy to drive down service costs; and provide associated evidence to their prospective tenant/occupier in accordance with the RICS code of practice – service charges in commercial property.
12.3.21 Enable space to be used flexibly to enable GP contractors to mitigate costs, where possible.
12.3.22 Allow GP contractors to procure their own services (such as cleaning) where it is practicable to do so, subject to the former providing assurance that their specification will comply with life cycle requirements.
Expectation management
12.3.23 Should there be evidence that a landlord is not prepared to fulfil the expectations detailed in 12.3.20 to 12.3.22, this will not, in principle, prejudice a GP contractor’s application for financial support towards premises running costs and service charges. However, it is likely to delay the processing of an application until the information required to complete it is available.
Evidence required to demonstrate application of principles
12.3.24 An expression of interest or application shall normally be considered when the steps identified in 12.3.24.1 to 12.3.24.4 have been evidenced:
12.3.24.1 Meetings and/or correspondence between the landlord/head leaseholder and the GP contractor which include full disclosure of soft facilities management costs backed up with supporting evidence.
12.3.24.2 Agreement that the footprint that the GP contractor occupies or wishes to occupy is sufficient to meet its current service provision and future potential provision.
12.3.24.3 Confirmation that key support service-related matters such as cleaning services have been discussed and agreed.
12.3.24.4 Evidence that the impact of procured soft facilities management services has been discussed in the context of value for money.
12.4 The model
Eligibility criteria
12.4.1 Questions to help establish eligibility should be answered on tab 2 in the financial model template (FMT) provided in annex 66.
12.4.2 Total practice expenses to total practice income (expressed as a percentage) for the most recent financial year must be greater than the published average 2015/16 expenses to earnings ratio for GP contractors in the UK for a similar contract type (see FMT tab 5). The expenses to earnings ratio is a measure of the proportion of an individual’s gross earnings that is consumed by business expenses. For ease of understanding it is expressed as a percentage throughout this report (refer to the latest GP earnings and expenses report).
Note:
“Full time and part time GPs are included. Figures are irrespective of working hours” (refer to the latest GP earnings and expenses report).
“Earnings and expenses results relate to both NHS and private work. It is not possible to provide an NHS/private split using HMRC as a data source as most GPs submit a self-assessment tax return which contains information on all their self-employment earnings while practising as a GP, but which cannot differentiate between NHS and private earnings. GPs can perform both NHS and private work both inside and outside the practice, including the NHS Out-of-Hours Service” (refer to the latest GP earnings and expenses report).
Private income is identified as a very small percentage of average GP income – based on the England data collection “as a guide to NHS/private earning proportions, the average NHS superannuable income for GPMS contractor GPs was 94.8 per cent of income before tax in 2013/14 (refer to the latest GP earnings and expenses report) which is the latest year for which pensions data are available” (GP earnings and expenses 2015/16 by NHS England, published 13 September 2017, page12).
If the value of work being undertaken by a GP partner outside their contractual commitment affects the total practice expenses to total practice income ratio, such that it is significantly greater than the relevant GMS, PMS or APMS benchmark ratio (as appropriate), NHS England reserves the right to exclude additional practice expenses relating to this (for example, locum costs to cover GP partner’s practice sessions). The value of outside clinical work/advice should be included in the expenditure incurred by the practice.
Primary care commissioners recognise that there may be circumstances that impact on the expenses to income ratio that could exclude a practice’s application for consideration for financial assistance towards service charges; these issues will always be evaluated on a case-by-case basis.
12.4.3 The practice should have had no serious contract breaches for any reason since 1 April 2013. The practice can make a statement for mitigation if it has had any serious contract breaches since 1 April 2013.
12.4.4 Should the above criteria not be met or the practice has not yet provided acceptable explanations for mitigation, an application will not be considered any further.
Financial model template
12.4.5 Notes for completion of the template file can be found in tab 1 in the financial model template provided in annex 66.
12.4.6 For the purpose of this exercise, a contract is considered as a whole. In other words, where a practice operates from more than one site, the combined income and expenses should be entered on the template. Similarly, where 2 or more practices are merging, the estimated combined income and expenses of the new practice should be entered on the template.
12.4.7 The practice is required to populate the attached I&E template (income and expenditure – tab 3 in the FMT) declaring its income and expenditure for the most recent financial year, including full disclosure of service charge cost paid during the most recent financial year. Evidence of payment of service charges must be provided. If no service charges were paid, a statement is required stating the reasons why none were paid during the most recent financial year. Applications where this applies will be evaluated on a case-by-case basis.
12.4.8 The practice must provide a breakdown of service charges which allows business rates, water and sewerage charges, and the collection and disposal of clinical waste to be identified. If the practice’s application includes an application for reimbursement of other amounts, the practice must distinguish them from fuel and electricity charges, building insurance costs, the costs of internal or external repairs, and plant building and grounds maintenance.
12.4.9 The practice must show baseline income separate from other income such as income received from QOF, enhanced services, non-NHS organisations and reimbursements.
12.4.10 The practice income and expenditure will be compared with the published 2015/16 UK averages (tab 5 in the FMT) for GMS and PMS practices to determine if the practice is performing broadly in line with these averages. An adjustment may be made for service charges based on the information provided by the practice since the UK average for service charge cost is not available.
12.4.11 On the I&E template (tab 3 in the FMT), the practice should demonstrate through a clear action plan how it intends, over a reasonable period of time, as agreed with the commissioner, to optimise its income and reduce its expenditure, where applicable, to align broadly with the published UK averages for 2015/16 (tab 5 in the FMT) (or more recent when available).
12.4.12 On the service charge template (tab 4 in the FMT), the practice should further demonstrate how it plans to increase its share of the service charge cost and reduce the liability of the primary care commissioner to provide financial assistance. This can be done in fixed percentage/value increments each year or based on list growth or another plan tailored for the practice. The practice is advised to note the impact of its projections on its expenses to earnings ratios. Where a practice cannot increase its share of the service charge cost, it must give reasons why this is not possible. Note that the primary care commissioner’s liability for financial assistance for service charge support can never be higher than the total service charge cost to the practice.
12.4.13 The figures mentioned above will be reviewed on an annual basis in the interest of the practice, primary care commissioner as well as the taxpayer. This includes the income and expenditure, service charge cost as well as the comparison with UK averages where applicable. The projected reduction in primary care commissioner’s liability for financial assistance for service charge cost will also be assessed annually to evaluate whether it is viable or not for the practice to be responsible for a larger share, and ultimately 100% of the total service charge cost. The practice should notify the primary care commissioner of any significant changes and provide an updated FMT to enable the re-evaluation of financial assistance for service charge cost. If there are no significant changes, the practice must provide the primary care commissioner with proof of payment of the most recent year’s service charge costs to compare these with the FMT submitted previously. Primary care commissioners will reconsider financial assistance for service charge cost support to a practice if there are significant changes to the FMT as well as actual service charge costs.
12.4.14 Where a practice chooses not to disclose its income and expenditure information on an annual basis, it will need to propose a fixed term financial assistance package for service charge costs. The practice will still be required – in the first instance – to demonstrate that it meets the eligibility criteria to access financial assistance and must also provide proof of payment of the most recent year’s service charge costs (where applicable). The practice will need to demonstrate a reduction in required service charge support taking into account known variables such as changes in weighted list size, baseline price, other income, actual service charge costs, other expenditure, national averages and other variables that may impact on the financial viability of the proposal. At the start of each financial year and while financial assistance is required, the practice must provide proof of payment of the most recent year’s service charge costs to the commissioner to compare these with the proposed financial assistance package, regardless of its agreement to a fixed term package. The commissioner will reconsider its financial assistance for service charge costs to the practice if there are significant changes to the proposed package and actual service charge costs. Financial assistance towards service charge costs will only be reimbursed based on actual service charge cost paid by the practice and not while there is a dispute between the practice and the landlord and/or there is no lease in place and/or the service charge costs have not been agreed with the landlord following an increase in this cost.
Process flowchart
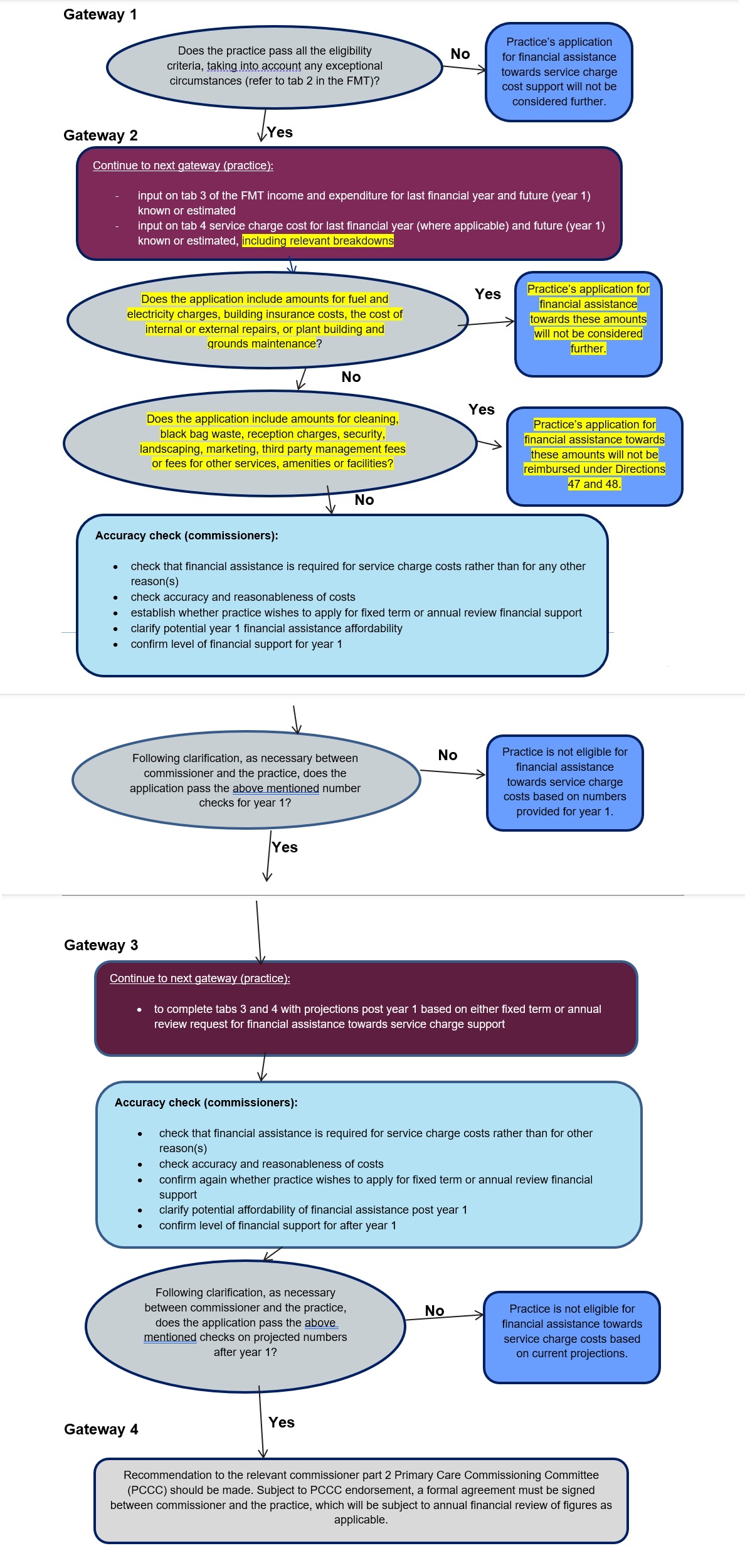
Gateway 1
Overview
This flowchart outlines the process for healthcare practices to apply for financial assistance towards service charge costs. The process involves 4 main gateways with specific eligibility criteria and accuracy checks at each stage.
Gateway 1: Initial Eligibility Assessment
If No:
If Yes:
Gateway 2: Financial Information and Service Charges
Required actions: input tab 3 of the Financial Management Tool (income and expenditure for last financial year and future year 1, known or estimated) and input tab 4 (service charge cost for last financial year where applicable and future year 1, known or estimated, including relevant breakdowns).
If Yes:
If No:
If Yes:
If No:
Gateway 2: Commissioner Accuracy Check
Commissioner responsibilities: check that financial assistance is required for service charge costs rather than for any other reasons, check accuracy and reasonableness of costs, establish whether practice wishes to apply for fixed term or annual review financial support, clarify potential year 1 financial assistance affordability, and confirm level of financial support for year 1.
If No:
If Yes:
Gateway 3: Post Year 1 Projections
Required actions: complete tabs 3 and 4 with projections post year 1 based on either fixed term or annual review request for financial assistance towards service charge support.
Gateway 3: Commissioner Accuracy Check
Commissioner responsibilities: check that financial assistance is required for service charge costs rather than for other reasons, check accuracy and reasonableness of costs, confirm again whether practice wishes to apply for fixed term or annual review financial support, clarify potential affordability of financial assistance post year 1, and confirm level of financial support for after year 1.
If No:
If Yes:
Gateway 4: Final Recommendation
Key Terms and References
Financial Management Tool (FMT): Referenced document with tabs for financial data entry
Directions 47 and 48: Regulatory framework governing reimbursements
Primary Care Commissioning Committee: Decision-making body for final approval
Fixed term vs annual review: Two options for ongoing financial support structure
Process Summary
Process Summary: this is a 4-stage gateway process where initial eligibility is assessed, current financial information is reviewed with specific exclusions, future projections are evaluated, and final recommendation is made to the commissioning committee. Each gateway includes commissioner accuracy checks and clear yes/no decision points that determine whether the application progresses or is declined.
13. Sub-contracting of clinical services: assurance framework
13.1 Introduction
13.1.1 This framework was primarily developed to support commissioners’ assurance of proposals by a GMS contractor to expand into new areas across the country by sub-contracting clinical services to a separate company to deliver services to ‘out of area’ patients, both through the provision of ‘digital-first’ services and face-to-face consultations in sub-contractor’s premises located outside the practice’s area.
13.1.2 The main guidance supporting out of area registration is available from the link below. Supplementary commissioner guidance is also being published by NHS England to support implementation of recent GP contract changes which introduce to requirements for GP practices to work collaboratively with commissioners to implement out of area registration.
NHS England » Safe and effective provision of high quality primary medical services to out of area registered patients: implementing the 2025/26 GP contract change
13.1.3 The framework is provided as a resource to support commissioners and consists of:
- guidance on assuring sub-contracting of clinical services under GMS contracts (section 13.2)
- assurance checklist (section 13.3)
- mandatory contract terms regarding sub-contracting (section 13.4)
The following are outside the scope of this framework:
- sub-contracting of non-clinical matters
- sub-contracting of out-of-hours services
- entering into a contract for services with a health care professional for the provision by that professional personally of clinical services
13.2 Guidance on assuring sub-contracting proposals
13.2.1 This guidance can assist commissioners in assuring proposals for sub-contracting and providers in developing their proposals and addressing potential issues, to enter into preliminary discussions and co-operate with one another prior to formally serving a notice of sub-contracting.
13.2.2 Doing so avoids the considerable time pressures associated with the 28-day period for commissioners to formally object to a notice of sub-contracting under a GMS contract.
13.2.3 However, under the GMS contract, the contractor has the right to serve a notice of sub-contracting at any time. Where a contractor does so, commissioners must act rapidly to undertake assurance of the proposals and (where appropriate) serve any notice of objection within a 28-day period.
Step 1 – identify the relevant contract and terms
13.2.4 In all cases the commissioner should identify the relevant primary medical services contract in place with the contractor and review its terms regarding sub-contracting. These terms set out the respective rights and obligations of the parties in relation to sub-contracting and must be adhered to by both parties.
13.2.5 This guidance and the checklist focus on GMS contracts only and reflect the mandatory terms regarding sub-contracts that must be included in all GMS contracts.
13.2.6 PMS agreements and APMS contracts have fewer mandatory terms regarding sub-contracting and may also have bespoke sub-contracting arrangements agreed within the contract. Therefore, not all aspects of this guidance and checklist will apply to such contracts. See annex 67: summary of the mandatory terms for each type of contract and seek legal advice where required.
Step 2 – notice of sub-contracting
13.2.7 The contractor must give notice in writing of its intention to sub-contract as soon as reasonably practicable before the date on which the proposed sub-contract is intended to come into effect (‘notice of sub-contracting’).
13.2.8 On receipt of such a notice, the commissioner should check if it is valid. A valid notice must include:
- the name and address of the proposed sub-contractor
- the duration of the proposed sub-contract
- the services to be covered by the proposed sub-contract
- the address of any premises to be used for the provision of services under the proposed sub-contract
13.2.9 If the notice is valid, the commissioner should then calculate a period of 28 days beginning with the date on which the notice of sub-contracting was received. The last day of that 28-day period is the last date on which the commissioner may serve a notice of objection (see step 5). The commissioner should take into account the notice provisions of the contract to ensure that the date is correctly calculated and any such notice is served in time.
13.2.10 If the notice is invalid, the commissioner should advise the contractor of this and that the proposed sub-contract will be unlawful unless and until a valid notice of sub-contracting has been served. On receipt of a valid notice, the commissioner has a further 28 days to object, starting on the date it was received.
Step 3 – notification of novel, contentious or repercussive proposals
13.2.11 The commissioner should take an initial view on whether any of the following criteria are met:
- the sub-contracted services will be delivered wholly or partly via a ‘digital-first’ service (that is, care delivery models through which a patient can receive the advice and treatment they need via online symptom checking and remote consultation)
- the sub-contracted services will be provided to ‘out of area’ patients (that is, patients who reside outside the practice area)
- the premises to be used for the provision of services under the proposed sub-contract are outside the contractor’s practice area; or
- the proposed sub-contract is otherwise considered to be novel, contentious or repercussive
13.2.12 Where any of the above criteria are met, the commissioner should immediately notify its regional NHS England primary care team. The purpose of this notification is to enable:
- monitoring of the rollout of such sub-contracting arrangements
- notification of commissioners affected by the proposed sub-contract
- provision of additional guidance and support to the commissioner, where appropriate
- in the case of an ICB commissioning primary medical services under delegated arrangements with NHS England, determining whether the decision requires additional approval by NHS England
13.2.13 In such cases, the NHS England regional team, having consulted with the NHS England national primary care team, will advise the commissioner of any additional procedures to be followed.
Step 4 – assurance of the proposed sub-contract
13.2.14 The commissioner must then assure the proposed sub-contract and decide:
- whether the proposed sub-contract is unlawful (that is, not permitted under the GMS contract)
- whether there are any safety or financial grounds to object to the proposed sub-contract
13.2.15 Where the contractor has served a valid notice of sub-contracting, it is essential that this process is completed (and any notice of objection given) before the 28-day period ends (see step 2).
Unlawful sub-contracting
13.2.16 The contractor is not permitted to sub-contract clinical services unless:
- it has given notice in writing to the commissioner of its intention to sub-contract as soon as reasonably practicable before the date on which the proposed sub-contract is intended to come into effect (see step 2)
- it is satisfied that the sub-contractor has in force in relation to it an indemnity arrangement which provides appropriate cover
- it has taken reasonable steps to satisfy itself that:
- it is reasonable in all the circumstances to sub-contract clinical matters; and
- the person to whom clinical matters are sub-contracted is qualified and competent to provide the service
- the sub-contractor would be able to meet the contractor’s obligations under the contract
- the sub-contract prohibits the sub-contractor from sub-contracting any of the clinical services that it has agreed with the contractor to provide under the sub-contract
13.2.17 The proposed sub-contract will also be unlawful if it involves the sub-contracting of essential services to a company or firm which is or was formed wholly or partly for the purpose of avoiding the restrictions on the sale of goodwill of a medical practice. Seek legal advice if this is a concern.
Objections on safety or financial grounds
13.2.18 The grounds of objection are that the sub-contract would:
- put the safety of the contractor’s patients at serious risk; or
- put NHS England at risk of material financial loss
13.2.19 These are the only grounds of objection available.
Assurance process
13.2.20 The assurance of the proposed sub-contract is at the discretion of the commissioner.
13.2.21 The assurance process should be proportionate and undertaken within the 28-day period to enable objections to be served if necessary.
13.2.22 What is proportionate in any particular case will depend on the circumstances and the commissioner’s assessment of the potential safety, financial and compliance risks associated with the proposal. Proposals that have been identified as novel, contentious or repercussive under step 3 are likely to require the most detailed level of assurance.
13.2.23 Without prejudice to the discretion of commissioners, NHS England has prepared an assurance checklist which sets out a series of matters which could be interrogated as part of such an assurance process – see section 13.3.
Additional information
13.2.24 The commissioner may request further information relating to the proposed sub-contract as appears to it to be reasonable and the contractor must supply such information to the commissioner promptly.
13.2.25 This is particularly likely to apply where the contractor has not engaged with the commissioner in advance of giving notice of sub-contracting, as the commissioner is unlikely to have all the information required to undertake an appropriate assurance exercise.
13.2.26 The 28-day period is not ‘paused’ when requests for information are made. Therefore, any requests for information should be made promptly to allow sufficient time to receive and scrutinise such information.
Decision
13.2.27 A decision on the above matters must be taken within the 28-day period based on the information available at that time.
13.2.28 The decision should be taken in accordance with relevant decision-making processes and (in the case of an ICB commissioning primary medical services under delegated arrangements with NHS England) in accordance with the relevant delegation agreement.
Step 5 – implementation
No objections
13.2.29 If the commissioner considers that that the proposed sub-contract is permitted under the terms of the contract and that there are no safety or financial grounds to object, no further formal steps are necessary. The contractor will be:
13.2.30 In these circumstances, the commissioner may indicate to the contractor that it does not presently have any objections. However, it is recommended that the commissioner states that this is without prejudice to its rights under the contract, including to object to the sub-contract in future, where appropriate.
Unlawful sub-contracting
13.2.31 If the commissioner considers that the proposed sub-contract is unlawful (that is, not permitted under the terms of the contract), it should notify the contractor of this in writing.
13.2.32 If the contractor nonetheless proceeds with the sub-contract, this should be treated as a breach of contract and appropriate contractual action should be taken. What action is appropriate will depend on the circumstances and legal advice should be obtained if necessary.
Objection on safety or financial grounds
13.2.33 Where NHS England is satisfied that there are safety or financial grounds on which to object, the commissioner must give notice in writing of its objection to the sub-contract within the 28-day period (‘notice of objection’).
13.2.34 The notice must specify the specific grounds relied on (see step 4) and include a statement of reasons for NHS England’s objections.
13.2.35 Where a valid notice of objection has been served on the contractor within the 28-day period, the contractor must not proceed with the sub-contract. If the contractor disagrees with the notice of objection, it must follow usual dispute resolution procedures.
13.2.36 If the contractor nonetheless proceeds with the sub-contract, this should be treated as a breach of contract and appropriate contractual action should be taken. What action is appropriate will depend on the circumstances and legal advice should be obtained if necessary.
Step 6 – review
13.2.37 Where sub-contacting proceeds, commissioners should continue to monitor the arrangements. Where issues arise, appropriate contractual action should be taken. What action is appropriate will depend on the circumstances and legal advice should be obtained if necessary.
13.2.37 In some cases, a proposed sub-contract may be unlawful or objected to on safety or financial grounds within the 28-day period but is capable of being permitted following a further period of development and assurance of the proposal. If so, the commissioner may wish to schedule a future review of the decision to assess if any objections can be lifted.
13.3 GP and NHS provider (NHS trusts or foundation trusts) sub-contracting checklist
13.3.1 There are also various emerging arrangements in which NHS trusts or foundation trusts (or their subsidiary companies) are becoming involved in primary medical services contracts (including GMS contracts) through either:
- sub-contracting of services
- contract award (PMS agreements and APMS contracts)
13.3.2 This section provides an overview of some key and emerging issues that commissioners may wish to assure themselves where such arrangements are proposed. It is structured into 4 parts:
- part A – issues that the NHS England regional teams will need to consider, to ensure that its own statutory responsibilities are upheld
- part B – issues that an ICB would need to consider to ensure it is meeting its responsibilities
- part C – issues that the NHS England regional team or the ICB would need to consider, depending on whether primary care commissioning responsibilities are delegated
- part D – issues on which the commissioner may need to seek assurance that the provider has considered
Part A: Issues for consideration by the NHS England regional teams
Issue: responsible officers
The Medical Profession (Responsible Officers) Regulations 2010 establish the role of the ‘responsible officer’ (RO). Organisations with a responsibility to appoint a RO include NHS England (for example, for an individual on the performers list) and organisations ‘designated’ under the regulations.
Those who wish to perform primary medical services on behalf of the NHS must generally be included in the national performers list (except in certain specified circumstances) and NHS England has a responsibility to provide a RO for those on the performer’s list – this includes in instances where that person(s) on the performers list is employed by another organisation (such as an NHS trust or foundation trust). This is likely to encapsulate the types of arrangements described given that they are performed under a GMS (sub)contract.
There may be circumstances in which it is appropriate for the NHS trust/foundation trust to provide a RO for someone providing primary medical services – for example, if they have employed an overseas GP who is not required to be on the performers list.
Considerations
There may be a risk of either:
- potential duplication between NHS England and providers – that is, both may provide a RO inappropriately; or
- that both the provider and NHS England may assume that the other party is providing the role
Action required
NHS England should ensure its responsible officer (RO) responsibilities are upheld. In practice, NHS England regional/local teams should confirm which organisation is taking responsibility for appointing a responsible RO and check that each GP employed/operating the sub-contract has a RO appointed.
Part B: Issues for consideration by the ICB
Issue: potential conflicts of interest
Commissioners are expected to manage any conflicts that may arise in relation to membership and decision-making.
Considerations
There is potential that a direct relationship between GPs and trusts/foundation trusts may raise additional conflicts of interest for decision-making. In particular, it is possible that GP practices affiliated with one NHS trust/foundation trust could become dominant within an ICB’s membership, and then potentially (dependant on its constitution) have an ability to influence other aspects of ICB policy which may benefit that trust. ICBs may also need to consider and manage potential conflicts of interest in their governance and decision-making arrangements.
Action required
Commissioners should consider this issue and refer to NHS England’s managing conflicts of interest guidance.
Part C: issues on which the commissioner may need to seek assurance that the provider has considered
Issue: following due process
There are set rules that govern the nature and circumstances in which primary medical services can be sub-contracted. It is worth noting that those rules differ slightly between GMS, PMS and APMS contractual frameworks. Further guidance on assuring sub-contracting arrangements is covered earlier in this chapter.
Those rules specify that where a GMS contractor wishes to sub-contract clinical matters, it must give notice in writing to NHS England of its intention to sub-contract as soon as is reasonably practicable before the date on which the proposed sub-contract is intended to come into effect (note that there is an exception in relation to sub-contracting out-of-hours services).
The contractor must not proceed with a sub-contract or, if the sub-contract has already taken effect, the contractor must take steps to terminate it where:
- NHS England gives notice in writing of its objection to the sub-contract on the grounds that the sub-contract would:
- put the safety of contractor’s patients at serious risk
- put NHS England at risk of material financial loss
and notice is given by the NHS England before the end of the period of 28 days beginning with the date on which NHS England received a notice from the contractor:
- the sub-contractor would be unable to meet the contractor’s obligations under the contract
A statement of reasons for an objection must be provided and should set out a clear rationale for the decision.
Considerations
Commissioners must ensure that commissioned services continue to be delivered in accordance with the GMS contract.
Action required
In considering any such proposals to sub-contract, commissioners should consider whether the GMS contract, under sub-contract, will continue to be delivered to the nationally agreed terms and requirements. This may include seeking assurance of, for example, matters such as how services will be delivered in accordance with the GMS contract and quality of care will be ensured.
Commissioners should also identify whether, because of the particular delivery model, the GMS contract holder – and therefore the person to whom the ICB should be escalating performance management concerns – could have a conflict of interest with their responsibilities to the NHS trust/foundation trust. If any conflict is identified, the commissioner should ensure that measures are in place to manage it.
As part of the assurance process, commissioners may wish to seek confirmation from the contractor that it has updated its CQC registration, and to understand the detail of this registration.
Throughout the duration of any sub-contracting arrangements, commissioners should continue to seek assurance about the delivery of the GMS contract through the lead contractor.
Part D: issues on which the commissioner may need to seek assurance that the provider has considered
There is a range of issues that contractors will need to properly consider and seek appropriate advice. These include but are not limited to:
- indemnity – for example, whether there is appropriate indemnity coverage for flexible use of workforce in the delivery of more integrated services
- implications for regulation – for example, to ensure that the provider’s registration with the CQC has been appropriately updated where applicable
- pensions – in particular, staff employed by sub-contractors are not able to access the NHS Pension Scheme (unless otherwise eligible in their own right: for example, employees of trusts/foundation trusts). This is particularly an issue where primary care contracts are sub-contracted to subsidiary companies with individuals becoming employed by the subsidiary rather than the trust/foundation trust directly
A sub-contractor does not automatically have access to the same digital services and support available to the practice. The practice will need to make a request to the ICB that will follow the guidelines in the GP IT operating model.
Part C: When things go wrong
1. Contract breaches, sanctions and terminations
1.1 Introduction
1.1.1 This chapter outlines the approach to be taken by the commissioner when a contract is considered to have been breached. Where processes differ with regards to GMS contracts, PMS agreements and APMS contracts, these are highlighted.
While network services are delivered by the member practices, they are commissioned from the individual member practices.
Circumstances of non-delivery of network services may result in the issue of a breach notice, a remedial notice, contract sanction or, exceptionally, lead the commissioner to consider termination. These will be applied to individual member practices as those circumstances dictate or are clear: for example, breach at network or practice population level.
1.1.2 Given that any decision to issue a breach or remedial notice, apply sanctions or terminate a contract or agreement can be challenged by the contractor under appeal, it is essential that the commissioner follows, and can demonstrate that it has followed, due process in investigating, communicating and implementing actions in this respect and that the commissioner has acted fairly and reasonably throughout.
1.1.3 It is essential that the commissioner maintains thorough and accurate records of all communications and discussions in respect of all notices under this policy.
1.1.4 Commissioners should maintain accurate records of all breaches, sanctions and terminations and will be required to demonstrate, if requested, evidence of compliance, or otherwise support oversight of primary medical services commissioning arrangements. This may be, for example, via NHS England’s assurance arrangements or internal and external audit functions.
1.2 Contract breaches
1.2.1. Where the commissioner considers that a breach has occurred, there are a number of options on how to proceed. The commissioner can:
- take no action
- agree on an action with the contractor
- issue a remedial notice
- issue a breach notice
- apply a contract sanction
- terminate the contract
1.2.2 In many cases, it will be appropriate, as a minimum, to serve a breach or remedial notice to formally document a breach as part of routine contract management. Where issues with a contractor then escalate, it is helpful if the pattern of breaches to date is already evidenced by appropriate breach and/or remedial notices. However, doing nothing or informally agreeing on an action with the contractor are options that the commissioner may consider appropriate for a very minor or technical breach. The commissioner should be aware of the implications of this decision in that there will be no formal record of the breach to rely on as part of future contract management.
1.2.3 The following paragraphs set out the circumstances in which a remedial notice or a breach notice may be issued, a contract sanction may be applied or the contract may be terminated with an explanation of the relevant process that the commissioner must follow.
1.2.4 The commissioner must ensure that, when issuing a remedial or breach notice, applying a contract sanction or terminating a contract, it follows the proper internal processes around the approval of the action, compliance with any standing orders and due consideration of all relevant factors in the decision-making process.
Delegated commissioning arrangements
The Delegation Agreement reserves primary medical services functions that relate to performers lists to NHS England. Circumstances that may result in the issue of a breach notice, a remedial notice or a contract sanction or may lead the commissioner to consider termination may relate to or include reference to performers lists matters. Where this is the case, the Delegation Agreement requires the ICB to work collaboratively with NHS England and support and assist NHS England to carry out its performers lists functions.
1.3 Remedial notices and breach notices
1.3.1 The GMS Regulations, PMS Regulations and APMS Directions make a clear distinction between the process to be followed where a breach is capable of remedy and the process where a breach is not capable of remedy.
1.3.2 GMS/PMS. Where a breach is capable of remedy, a remedial notice must be issued before the commissioner takes any other action under the contract (such as termination). Where a breach is not capable of remedy, a breach notice must be issued before the commissioner takes any other action under the contract (such as termination).
1.3.3 Contracts are not required to contain provisions relating to remedial or breach notices. The standard APMS contract does, however, contain these provisions. Where there is a potential breach of an APMS contract, the commissioner should always review the actual wording of the contract to ensure the right process is followed.
Remedial notice
1.3.4 Where a contractor has breached the contract and the breach is determined to be capable of remedy, the commissioner may issue a remedial notice to the contractor setting out the actions that must be taken to remedy the breach.
1.3.5 Annex 68: remedial notice flowchart highlights the main steps that the commissioner should take when issuing a remedial notice.
1.3.6 The commissioner must issue a remedial notice before it takes any other action it is entitled to take under the contract, except where the breach relates to the rights of termination set out below. This is because the commissioner has a right to terminate the contract immediately for a breach of any of the circumstances set out below. These rights of termination are explained in more detail in section below:
- provision of untrue information
- fitness to practise matters
- a serious risk to patient safety or risk of financial loss to NHS England
- unlawful sub-contracting
- in the case of a GMS contract, issues relating to the contractor’s eligibility to hold the contract
1.3.7 A breach capable of remedy is where the breach continues but the contractor could take action to stop the breach. Examples of breaches that may be capable of remedy include:
1.3.8 Where the breach creates a serious risk to patient safety, the commissioner can take more immediate action, regardless of whether the breach is capable of remedy or not. For further information on this, please refer to 1.7.32 below.
1.3.9 Where the commissioner has determined that a breach is capable of remedy, the commissioner may, depending on the nature and circumstances of a breach, take the following steps:
- the commissioner should contact the contractor to discuss the breach and the action that it may be entitled to take; that is, the issue of a remedial notice
- this discussion should provide the contractor with an opportunity to provide an explanation as to the circumstances that led to the breach. An accurate minute of any discussions should be retained
- the commissioner should review the evidence related to the breach including any information received during the discussion or in representations
- if the commissioner is satisfied that the matter is a breach which is capable of remedy, then the commissioner may issue a remedial notice to the contractor, requiring the contractor to remedy the breach
These steps do not prejudice or delay a commissioner’s right to issue a remedial notice at any point before or during any of these steps being taken where the commissioner reasonably considers it is appropriate to do so.
It is important that when the steps above are undertaken, this is completed as quickly as is reasonably possible as long delays between the breach occurring, or the commissioner becoming aware of the breach, and the remedial notice being issued could lead to an argument that the commissioner has accepted the breach and waived its right to take action. The commissioner will need to decide what action it considers would be reasonable to take before issuing a remedial notice in the circumstances of an individual breach.
A remedial notice must specify:
- details of the breach which led to the remedial notice being issued and any evidence gathered in respect of the breach
- the steps the contractor must take to remedy the breach to the commissioner’s satisfaction
- the period in which the steps must be taken
- any arrangements for reviewing the matter to ensure that the requirements of the remedial notice have been met; and
- the actions that the commissioner shall take if the contractor fails to satisfactorily remedy the breach
1.3.10 The commissioner may wish to include in the remedial notice how the contractor may appeal against the decision to issue a remedial notice.
1.3.11 Annex 69 provides a template remedial notice. [This notice is provided as a template only and appropriate advice and support should be sought prior to issuing such a notice.]
Where NHS England is the commissioner, the finalised remedial notice should be signed off by the head of commissioning or their nominated deputy. Where the commissioner is an ICB operating under delegated commissioning arrangements, the ICB should ensure the finalised remedial notice is signed off by the chief operating officer (COO) or an individual authorised by the COO.
1.3.12 The period during which the steps to remedy the breach must be taken must not be less than 28 days from the date that notice is given, unless the commissioner is satisfied that a shorter period is necessary to protect the safety of the contractor’s patients or to protect from material financial loss. In setting an appropriate remedial period, the commissioner should ensure that it would be possible for the breach to remedied within that timescale. For example, if a premises breach requires major building works to remedy the issue, 28 days will not be reasonable if it seems likely that it would be impossible to meet this deadline.
1.3.13 The remedial notice must be delivered to the contractor in accordance with the notice provisions of the contract. This usually requires hand delivery or postal delivery (first class or registered post). Delivery of a notice by email may be permissible. The commissioner should review the relevant provisions to the contract to ensure proper delivery. Where the notice is hand delivered, annex 70 provides a template notice receipt.
1.3.14 The commissioner should ensure that arrangements are in place to follow up a remedial notice appropriately and in a timely fashion.
1.3.15 Where the commissioner is satisfied that the contractor has taken the required steps to remedy the breach within the required period, a letter should be issued to the contractor informing it that the terms of the remedial notice have been satisfied and that no further action will be taken at this stage. Annex 71 provides a template remedial notice satisfaction letter.
[This letter is provided as a template only and the commissioner should ensure that appropriate advice and support has been sought prior to issuing such a letter.]
1.3.16 Where the commissioner is satisfied that the contractor has not taken the required steps to remedy the breach by the end of the required notice period, the commissioner may inform the contractor that it has failed to meet the terms of the remedial notice and that the commissioner may terminate the contract with effect from such date as the commissioner may specify in a further notice to the contractor.
1.3.17 Where the commissioner intends to terminate the contract, please refer to sections 1.5 to 1.7 below.
1.3.18 If following the issue of a remedial notice, a contractor either repeats a breach that was the subject of a remedial notice or otherwise breaches the contract that results in a further remedial notice or a breach notice, then the commissioner has the right to terminate the contract by serving notice on the contractor.
1.3.19 For GMS and PMS, the right to terminate in 1.3.18 above must only be used where the commissioner is satisfied that the cumulative effect of the breaches is such that the commissioner considers that to allow the contract to continue would be prejudicial to the efficiency of the services to be provided under the contract. The commissioner does not usually have to establish this when terminating an APMS contract, although the contract wording should be checked. Where the commissioner intends to terminate the contract under this right, please refer to 1.7.46 below.
1.3.20 If the contractor is in breach of any obligation and a remedial notice in respect of that default has been given to the contractor, the commissioner may withhold or deduct monies that would otherwise be payable under the contract in respect of that obligation which is the subject of the default.
Breach notice
1.3.21 Where the contractor has breached the contract and that breach is not capable of remedy, the commissioner may serve a breach notice on the contractor requiring the contractor not to repeat the breach.
1.3.22 Annex 72: breach notice flowchart highlights the main steps that the commissioner should take when issuing a breach notice.
1.3.23 Breach notices cannot be issued where the breach relates to the following rights of termination:
- provision of untrue information
- fitness to practise matters
- a serious risk to patient safety or risk of financial loss to NHS England
- unlawful sub-contracting; and
- in the case of a GMS contract, issues relating to the contractor’s eligibility to hold the contract
For further information, please refer to section 1.7: rights of termination.
1.3.24 A breach that is not capable of remedy is where a breach occurs but either does not continue prior to a notice being issued or there is no action that can be taken to remedy the breach.
1.3.25 Examples of breaches that are not capable of remedy include:
- a practice closing during its contracted opening times in the previous week with no access for the contractor’s registered patients to essential services
- failure to store vaccines correctly and such vaccines have already been provided to patients
1.3.26 Where the breach creates a serious risk to patient safety, the commissioner can take more immediate action, regardless of whether the breach is capable of remedy or not. For further information on this, please refer to 1.7.32 below.
1.3.27 Where the commissioner has determined that a breach is not capable of remedy, the commissioner may, depending on the nature and circumstances of a breach, take the following steps:
- initially the commissioner should contact the contractor to discuss the breach and the action that it may be entitled to take; that is the issue of a breach notice. This does not prejudice or delay a commissioner’s right to issue a breach notice
- the discussion will afford the contractor the opportunity to provide an explanation as to the circumstances that led to the breach and this discussion should be recorded accurately in writing
- the commissioner should review the evidence related to the breach including any information received during the discussion or in representations
- if the commissioner is satisfied that the matter is a breach which is not capable of remedy, then the commissioner may issue a breach notice to the contractor, requiring the contractor not to repeat the breach.
These steps do not prejudice or delay a commissioner’s right to issue a breach notice at any point before or during any of these steps being taken where the commissioner reasonably considers it is appropriate to do so.
The breach notice must specify:
- details of the breach
- the requirement that the contractor must not repeat the breach; and
- the consequences of the contractor further breaching the contract
1.3.28 Annex 73 provides a template breach notice. Where NHS England is the commissioner, the finalised breach notice should be signed off by the head of commissioning or their nominated deputy. Where the commissioner is an ICB operating under delegated commissioning arrangements, the ICB should ensure the finalised remedial notice is signed off by the chief operating officer (COO) or an individual authorised by the COO.
1.3.29 The breach notice must be delivered to the contractor in accordance with the notice provisions of the contract. This usually requires hand delivery or postal delivery (first class or registered post). Delivery of a notice by email may be permissible. The commissioner should review the relevant provisions to the contract to ensure proper delivery. Where the notice is hand delivered, annex 70 provides a template notice receipt.
1.3.30 If, following the issue of a breach notice, a contractor either repeats a breach that was the subject of a breach notice or otherwise breaches the contract that results in a further remedial notice or a breach notice, then the commissioner has the right to terminate the contract by serving notice on the contractor.
1.3.31 For GMS and PMS, this right to terminate can only be used where the commissioner is satisfied that the cumulative effect of the breaches is such that the commissioner considers that to allow the contract to continue would be prejudicial to the efficiency of the services to be provided under the contract. The commissioner does not usually have to establish this when terminating an APMS contract, although the contract wording should be checked. Where the commissioner intends to terminate the contract under this right, please refer to 1.7.46 below.
1.3.32 If the contractor is in breach of any obligation and a breach notice has been issued, the commissioner may withhold or deduct monies that would otherwise be payable under the contract in respect of that obligation.
1.3.33 The commissioner should retain and be able to report on all contractual notices issued in any financial year to support local and national assurance arrangements. The template notice return in annex 74 can be used.
1.4 Contract sanctions
1.4.1 GMS/PMS. The commissioner must follow the process set out in this section. PMS agreements refer to “agreement sanctions” rather than contract sanctions. Reference to contract sanctions in this policy should be read as including reference to agreement sanctions.
1.4.2 APMS contracts are not required to contain provisions relating to contract sanctions. The NHS England standard APMS contract does not contain references to contract sanctions. The commissioner must check the relevant contract to determine whether contract sanctions can be applied.
1.4.3 Contract sanctions must not be applied to a contract unless the commissioner has the right to terminate. Where contract sanctions are applied, this is instead of terminating the contract. The commissioner cannot apply contract sanctions and later decide to terminate the contract based on the breach that triggered the contract sanction.
1.4.4 The circumstances in which the commissioner may apply contract sanctions are those circumstances set out below where a right of termination arises:
- provision of untrue information
- fitness to practise matters
- where there is a serious risk to patient safety or NHS England is at risk of material financial loss
- where the commissioner is satisfied that the contractor has not taken the steps required by a remedial notice to remedy a breach within the required period
- where after a remedial notice or breach notice has been issued the contractor:
- repeats a breach that was the subject of a remedial notice or a breach notice
- otherwise breaches the contract resulting in a further remedial notice or breach notice
- where the contractor carries on business detrimental to the contract; and/or
- for GMS contracts only, where changes in the membership of the partnership are likely to have a serious adverse impact on the ability of the contractor or the commissioner to perform obligations under the contract
Please refer to the relevant right of termination in section 1.7 for further information on how these rights of termination arise.
Contract sanctions must not be applied if they terminate or suspend any obligation that relates to essential services.
1.4.5 Contract sanctions may involve:
- termination of specified reciprocal obligations
- suspension of specified reciprocal obligations for a period of up to 6 months; or
- withholding or deducting monies otherwise payable under the contract
1.4.6 The choice of which contract sanction to use would ordinarily depend on the nature or cumulative effect of the breach, and what is felt to be the most appropriate and proportionate action in those circumstances. For example, if the breaches have occurred in relation to a specific service element under the contract, it might be most appropriate to move to terminate that specific service, such as minor surgery.
1.4.7 Where the commissioner is considering imposing a contract sanction and the contractor has a GMS contract, it is a statutory requirement that the commissioner consults the relevant LMC before it imposes the contract sanction, where it is reasonably practicable to do so. There is no such statutory requirement in respect of PMS agreements or APMS contracts and the commissioner should ensure it considers any relevant wording in the contract.
1.4.8 Where the commissioner decides that the most appropriate sanction would be to withhold or deduct monies, this must be calculated to establish a consistent, fair and measured approach. For further information refer to Annex 75: calculating a financial contract sanction.
1.4.9 Where the commissioner decides to impose a contract sanction, the commissioner must issue a notice of its intent to apply a sanction to the contractor which must include:
- the nature of the sanction to be applied
- if withholding or deducting monies, how this has been calculated and the duration of any such sanction
- if services are to be terminated, which services and from what date
- if a suspension of specified reciprocal obligations under the contract or agreement, the period of that suspension and its end date
- an explanation of the effect of the imposition of the contract sanction
- the contractor’s right to appeal the decision to apply a contract sanction
1.4.10 Annex 76 provides a template contract sanction notice. [This is provided as a template only and appropriate advice and support should be sought prior to issuing such a notice.]
Where NHS England is the commissioner, the finalised contract sanction notice should be signed off by the head of commissioning or their nominated deputy. Where the commissioner is an ICB operating under delegated commissioning arrangements, the ICB should ensure the finalised remedial notice is signed off by the chief operating officer (COO) or an individual authorised by the COO.
The date that the contract sanction takes effect must not be until at least 28 days after the notice was served unless the commissioner is satisfied that it is necessary to impose the contract sanction earlier to protect the safety of patients or to protect from material financial loss.
1.4.11 Where a contract sanction is imposed, the commissioner can charge the contractor reasonable administration costs of imposing the contract sanction.
1.4.12 After imposing the contract sanction on a contractor with a GMS contract, it is a statutory requirement for the commissioner to, as soon as reasonably practicable, notify the relevant LMC in writing of the contract sanction imposed. There is no such statutory requirement in respect of PMS agreements or APMS contracts and the commissioner should ensure it considers any relevant wording in the contract.
1.4.13 If the contractor disputes the imposition of a contract sanction, the commissioner must not impose the contract sanction until the dispute has been determined unless the contract sanction is necessary to protect the safety of patients or to protect from material financial loss.
1.4.14 Where a dispute arises in relation to the imposition of contract sanctions, please refer to chapter 4: Managing disputes.
1.4.15 The commissioner should ensure that arrangements are in place to monitor the contractor’s compliance with a contract sanction notice.
1.4.16 The commissioner should retain and be able to report on all contractual sanctions issued in any financial year to support any local and national assurance arrangements. Annex 74 provides a template notice return.
1.5 Termination
1.5.1 Termination is a very significant action to take both on the part of the commissioner and the contractor and is an area of high risk for both parties in respect of financial impact and continuity of services. Where the commissioner considers that a termination notice may be issued, the commissioner should seek legal advice early in the process to confirm the appropriateness and lawfulness of taking such a step. It is essential that the commissioner maintains thorough and accurate records of all communications and discussions in respect of all notices.
1.5.2 Contractors have the right to appeal so it is essential that the commissioner follows and can demonstrate that it has followed due process in investigating, communicating and implementing actions leading to termination.
1.5.3 It is essential that prior to moving to terminate a contract, the commissioner is satisfied that it is fully within its rights to do so.
1.5.4 Legislation sets out certain rights of termination that are required to be in each type of primary medical contract. These mandatory termination rights are set out below and explained more fully in section . Where the termination relates to a matter that is contained within an alternative policy, this is highlighted.
1.5.5 GMS/PMS may only be terminated using mandatory termination rights. An APMS contract may contain additional termination rights. The commissioner should consider the relevant contract to ensure it is fully aware of all termination rights.
1.5.6 GMS/PMS. The following circumstances relating to rights of termination are required to be in GMS contracts and PMS agreements:
- death of a contractor
- contractor serving notice
- late payment
- provision of untrue information
- fitness to practise issues
- patient safety
- material financial loss
- unlawful sub-contracting
- remedial notices and breach notices
- carrying on business detrimental to the contract
1.5.7 GMS contracts are required to contain additional rights of termination relating to:
- breach of Regulation 4 (conditions relating solely to medical practitioners) of the GMS Regulations
- certain partnership matters
1.5.8 PMS agreements are required to contain additional rights of termination relating to:
- commissioner serving notice
- contractor’s exercise of the right to a GMS contract
- agreement of the parties
1.5.9 The following circumstances relating to rights of termination are required to be in APMS contracts:
- death of a contractor
- provision of untrue information
- fitness to practise issues
- patient safety
- material financial loss
- unlawful sub-contracting
1.5.10 APMS contracts are likely to have further rights of termination. Where the commissioner wishes to terminate for a reason other than those set out in 1.5.9 above, the commissioner must review the contract to determine if any further rights of termination apply.
1.5.11 Contracts may also terminate by:
- reaching their natural end dates, without the need for termination notice (in which case, please refer to part B, chapter 10: Practice closedown (planned/scheduled) for more information)
- retirement of the contractor (in which case, please refer to the part B, chapter 8: Contract variations)
1.5.12 Where the commissioner has considered all the relevant factors and has decided to proceed with termination, it must send a termination notice to the contractor. Annex 77 provides a template termination notice.
1.5.13 Where NHS England is the commissioner, the finalised termination notice should be signed off by the director of commissioning operations or their nominated deputy. Where the commissioner is an ICB operating under delegated commissioning arrangements, the ICB should ensure the finalised remedial notice is signed off by the chief operating officer (COO) or an individual authorised by the COO.
1.5.14 For GMS contracts and PMS arrangements, where the termination relates to:
- provision of untrue information
- fitness to practise issues
- patient safety
- material financial loss
- remedial notices and breach notices
- for GMS agreements: certain partnership matters
- for PMS agreements: carrying on business detrimental to the agreement
The notice usually specifies a date on which the contract terminates that is not less than 28 days after the date on which the commissioner has served the notice on the contractor. The commissioner may state a date less than 28 days where this is necessary to protect the safety of the contractor’s patients or protect from material financial loss. APMS contracts are not required to contain any such provisions and the commissioner should consider the wording of the particular APMS contract.
1.5.15 Where the contractor disputes the commissioner’s decision to terminate the contract, the contractor may invoke the NHS dispute resolution procedure. In such circumstances, the commissioner should refer to chapter 4: Managing disputes.
1.5.16 The commissioner should retain and be able to report on all termination notices issued in any financial year to support local and national assurance arrangements. Annex 74 provides a template notice return.
1.6 Key considerations on termination
1.6.1 The commissioner must establish that grounds exist under the terms of the contract to terminate. The commissioner must follow due process and investigation of the facts and provide the contractor with the opportunity to provide a response to allegations, wherever possible.
1.6.2 Annex 78: termination flowchart highlights the main steps that the commissioner should take when issuing a termination notice.
1.6.3 The commissioner must consider all relevant information available and decide on the appropriate course of action and whether the contract should be terminated.
1.6.4 Apart from considerations regarding whether the right to terminate arises, there are a number of common factors that the commissioner should consider when termination is a proposed course of action. These factors are set out below.
1.6.5 This list is not exhaustive and there are likely to be other issues that need due consideration under these provisions. These considerations will also apply following the sudden death of a contractor (see the chapter 3: Death of a contractor) and in some part on the closure of a branch surgery (see part B, chapter 8: Contract variations).
Continuity of service provision
1.6.6 NHS England has a statutory duty to ensure the continuity of provision of primary care services. Termination of existing service provision may result in some persons not being able to access primary care services. The commissioner must therefore consider how this duty will be discharged if it decides to terminate the contract. This should be considered as soon as the commissioner starts to think about terminating.
1.6.7 If the commissioner envisages that a new contract will be entered into with a provider, the commissioner must consider how to procure that contract and to ensure it is in accordance with procurement law and any procurement protocol issued by NHS England.
PMS to GMS
1.6.8 PMS agreements provide a right for certain contractors to request to enter into a GMS contract. Such a request can only be refused where the contractor fails to meet the conditions set out in the PMS Regulations.
1.6.9 For further information on this, please refer to part B, chapter 9: Managing a PMS contractor’s right to a GMS contract.
General duties
1.6.10 NHS England has a number of statutory duties relating to the exercise of its functions including reducing health inequalities and public involvement. The commissioner must ensure that its actions in terminating a contract and any consequential actions ensure compliance with these duties. In an urgent situation, it may be necessary to balance the duty to involve the public alongside the public interest in maintaining continuity of care and protecting the health, safety and welfare of patients or staff. Please refer to part A, chapter 2: General duties of NHS England for further information.
LMC consultation (GMS contracts)
1.6.11 For GMS contracts, the commissioner must consult the LMC for the area in which the contractor provides services where the commissioner is considering:
- terminating the contract
- which alternative notice to issue where there is a right to terminate for unlawful sub-contracting; or
- imposing a contract sanction
1.6.12 Whether or not the LMC has been consulted, whenever the commissioner imposes a contract sanction or terminates a GMS contract, the commissioner must as soon as reasonably practicable, notify the relevant LMC in writing of the sanction or termination. PMS agreements and APMS contracts are not required to contain such provisions. The commissioner should review the relevant contract to determine whether any requirement has been included.
Premises
1.6.13 The commissioner should ascertain who owns the premises and what arrangements apply to the premises. Where the outgoing contractor owns the premises, a future service provider may not be able to use those premises for the delivery of services. The commissioner should consider what arrangements need to be put in place to ensure continued service provision. The commissioner should also ensure it considers any Premises Cost Directions or guidance published by NHS England in relation to premises.
TUPE
1.6.14 The commissioner should consider the impact of termination on the staff currently employed under the terminating contract. Where a new contract is entered into with a new provider, TUPE may apply to transfer the staff to the new provider.
1.6.15 TUPE can be complex, risky and time consuming for any incoming provider and is likely to have a financial impact on the cost of any service. The commissioner should consider whether the potential for TUPE to apply may be considered a significant risk to any incoming provider.
Equipment
1.6.16 All equipment, including associated software, issued through GP IT is owned by NHS England and is being managed on its behalf by ICBs as responsible commissioners of GP IT services. Arrangements should be put in place to retrieve this equipment, together with other kits issued by the ICB, to ensure it is available to a future service provider.
Patient lists
See also PCSE practice mergers and closures resources
1.6.17 Patients have a right of choice, meaning the commissioner must not routinely transfer all the registered patients to an alternative provider. Patients should be provided with a detailed list of other local practices that are currently accepting new patients and offered the opportunity to register with one of them.
1.6.18 The commissioner should consider what steps will be taken in regard to patients who have not registered elsewhere at the end of the contract. It is often the case that the majority will voluntarily seek alternative registration; however, there are usually a number of patients who do not. Some may no longer be resident in the UK, some may have moved within the UK and not changed their address details at the practice and others may have yet to choose an alternative provider. Some may have died. In these circumstances, the commissioner must be clear on the process of dispersal or allocation that it will follow to avoid the risk of challenge from other local providers. Please refer to part B, chapter 10: Practice closedown (planned/scheduled) and part C, chapter 2: Unplanned/unscheduled and unavoidable practice closedown.
Patient records
See also PCSE practice mergers and closures resources
1.6.19 The commissioner should consider management of NHS patient paper records (Lloyd George notes) and any subsequent clinical mail. It is very likely that the contractor has retained a significant number of patient paper records in the reception area and also often stored elsewhere in the practice premises, including loft spaces and store cupboards. The commissioner must be able to securely retrieve these records and communications, having full regard of data protection and confidentiality, so that these can be distributed accordingly to any providers or returned to central storage. The contractor (or its representative) is responsible for any non-NHS patient or client record, though agreement may be reached with the commissioner to manage (dispose of) any confidential information on its behalf. Please refer to part B, chapter 10: Practice closedown (planned/scheduled) and part C, chapter 2: Unplanned/unscheduled and unavoidable practice closedown.
Prescriptions
See also PCSE practice mergers and closures resources
1.6.20 The commissioner should consider prescription pads, electronic prescriptions and any uncollected completed prescriptions as these will need to be retrieved and dealt with accordingly. The commissioner may wish to decide on a specified age of a current prescription (such as 1 month) and make appropriate arrangements for the handling of these and disposal of any that are older.
Drugs and medicines
1.6.21 The commissioner should consider practice held drugs. These will need to be disposed of but are technically likely to be owned by the contractor whose contract is terminating. The commissioner should seek assurances about the safe and effective disposal of such drugs.
1.7 Rights of termination
Death of a contractor
1.7.1 Please refer to chapter 3: Death of a contractor for further information.
Termination where both parties agree
1.7.2 PMS agreements are required to contain a provision stating that both parties may agree to terminate a contract. Although GMS or APMS contracts are not required to contain such a provision, all types of contracts may be terminated where both parties agree.
1.7.3 Where the parties agree to terminate, the parties must agree on the date from which termination will take place and any further terms relating to the termination. Before agreeing on the termination date, the commissioner should ensure any proposed timescale allows the commissioner to consider any other factors or actions that may be required prior to termination.
1.7.4 The contractor party may be composed of more than one person. The commissioner must agree to the same termination arrangements with all persons that constitute the contractor.
1.7.5 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to part A, chapter 2: General duties of NHS England.
Termination where the contractor serves notice
1.7.6 GMS contracts and PMS agreements can be terminated by the contractor by serving notice in writing at any time. APMS contracts may also contain this right of termination.
1.7.7 Where a contractor serves notice to terminate a GMS contract, it shall terminate 6 months after the date on which the notice is served, except where the contractor is an individual medical practitioner in which case the contract shall terminate 3 months after the date on which the notice is served.
1.7.8 If the date on which the GMS contract will terminate is not the last calendar day of a month, the contract shall instead terminate on the last calendar day of the month in which the termination date falls.
1.7.9 Where a contractor serves notice to terminate a PMS agreement, the period of notice shall not be less than 6 months (unless both parties agree in which case, please refer to 1.7.2 to 1.7.5 above).
1.7.10 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to 1.6.10 above.
Termination where the commissioner serves notice
1.7.11 PMS agreements can be terminated by the commissioner by serving notice in writing at any time, without needing to establish any breach by the contractor. APMS contracts may also contain this right of termination.
1.7.12 Where the commissioner serves this type of notice to terminate a PMS agreement, the period of notice shall not be less than 6 months (unless both parties agree in which case, please refer to 1.7.2 above). Commissioners should bear in mind the right of some PMS contractors to request a GMS contract. For further information on this, please refer to part B, chapter 9: Managing a PMS contractor’s right to a GMS contract.
1.7.13 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to 1.6.10 above.
1.7.14 GMS contracts are usually contracts in perpetuity without any right for the commissioner to terminate on notice.
Termination where the contractor exercises the right to a GMS contract
1.7.15 Please refer to part B, chapter 9: Managing a PMS contractor’s right to a GMS contract for further information.
Termination due to late payment
1.7.16 The contractor may give notice in writing to the commissioner if the commissioner has failed to make any payment due to the contractor under the contract. If the commissioner has failed to make any such payment within 28 days of the notice, the contractor may terminate the contract by a further written notice.
1.7.17 Where the NHS dispute resolution procedure has been invoked by the commissioner within 28 days of the initial notice, the contractor may not terminate the contract until either the NHS dispute resolution determination allows termination or the commissioner ceases to pursue the NHS dispute resolution process.
1.7.18 For further information on the NHS dispute resolution process, please refer to chapter 4: Managing disputes.
1.7.19 NHS England’s general duties may be triggered by termination in these circumstances. For further information, refer to 6.10 above and part A, chapter 2: General duties of NHS England.
Termination for provision of untrue information
1.7.20 The commissioner may serve notice to terminate the contract immediately (or from any date set out in the notice) if, after the contract has been entered into, it comes to the attention of the commissioner that written information provided to the commissioner:
- before the contract was entered into
- for GMS contracts, pursuant to paragraph 50(1)(a) or (b) or 51(1) of Schedule 3 of the GMS Regulations
- for PMS agreements, pursuant to paragraph 46(1)(a) or (b) of Schedule 2 of the PMS Regulations
- in relation to:
was, when given, untrue or inaccurate in a material respect.
1.7.21 NHS England’s general duties may be triggered by termination in these circumstances. For further information, refer to 6.10 above and part A, chapter 2: General duties of NHS England.
Termination due to fitness to practise issues
1.7.22 The commissioner may serve notice in writing on the contractor terminating the contract immediately (or from any date set out in the notice) where a person connected with the contract (such as a medical practitioner, a partnership, a company or a director) falls within any circumstances set out in the relevant regulations/directions. Those circumstances include where the person:
- is disqualified from practising by a licensing body
- has been convicted of certain offences
- has been adjudged bankrupt; or
- has been subject to a disqualification under the Company Director Disqualification Act 1986
The full list of circumstances is set out in the relevant law for GMS contracts, PMS agreements and APMS contracts at:
- GMS Regulations 2015, Schedule 3, paragraph 67
- PMS Regulations 2015, Schedule 2, paragraph 58
- Direction 7(2)(q) of the APMS Directions (2022)
1.7.23 NHS England’s general duties may be triggered by termination in these circumstances. For further information, refer to 6.10 above and part A, chapter 2: General duties of NHS England.
Termination where there is a serious risk to patient safety
1.7.24 The commissioner may serve notice in writing on the contractor terminating the contract immediately (or from such date set out in the notice) where the contractor has breached the contract and, as a result of that breach, the safety of the contractor’s patients is at serious risk if the contract is not terminated.
1.7.25 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to 6.10 above and part A, chapter 2: General duties of NHS England.
Termination where there is a material financial loss
1.7.26 The commissioner may serve notice in writing on the contractor terminating the contract immediately (or from such date set out in the notice) where the contractor’s financial situation is such that the commissioner considers that NHS England is at risk of material financial loss.
1.7.27 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to 6.10 above and part A, chapter 2: General duties of NHS England.
Termination due to unlawful sub-contracting
1.7.28 The commissioner will have a right of termination where it comes to the commissioner’s attention that the contractor has sub-contracted any of its rights or duties under the agreement in relation to the provision of essential services to a company or firm:
- owned wholly or partly by the contractor, or by any former or current employee of, or partner or shareholder in the contractor
- formed by or on behalf of the contractor, or from which it derives or may derive a pecuniary benefit; or
- formed by or on behalf of a former or current employee of, or partner or shareholder in, the contractor, or from which such a person derives or may derive a pecuniary benefit
where that company or firm is or was formed wholly or partly for the purpose of avoiding the restrictions on the sale of the goodwill of a medical practice in section 54 of the NHS Act 2006 or any regulations made wholly or partly under that section.
1.7.29 Where this occurs, the commissioner may serve notice in writing on the contractor terminating the contract immediately or instructing the contractor to terminate the relevant sub-contract.
1.7.30 It is a requirement under GMS contracts that, whenever reasonably practicable to do so, the commissioner must consult with the relevant LMC when considering which alternative notice to issue (for further information on LMC consultation requirements, refer to above). PMS agreements and APMS contracts are not required to contain such provisions. The commissioner should review the relevant contract to determine whether any requirement has been included.
1.7.31 If the contractor fails to terminate the sub-contract, the commissioner may serve a notice in writing on the contractor terminating the contract immediately.
1.7.32 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to 6.10 above and part A, chapter 2: General duties of NHS England.
Termination relating to remedial notices and breach notices
1.7.33 The commissioner has a right to terminate the contract where the commissioner is satisfied that the contractor has not taken the required steps to remedy the breach by the end of the required period as stated in the remedial notice.
1.7.34 The commissioner has a further right of termination where, following the issue of a remedial notice or breach notice, a contractor:
- repeats a breach that was the subject of a remedial notice or breach notice; or
- otherwise breaches the contract that results in a further remedial notice or breach notice
1.7.35 The further breach must have occurred after the breach which was the subject of the remedial notice or breach notice. The commissioner may intend to issue a further remedial notice or breach notice for a breach that occurred prior to the original breach with the need to investigate or gather information delaying the issue of the notice. In these circumstances, the commissioner cannot then rely on this right of termination as the further breach did not occur following the issue of the original remedial notice or breach notice.
1.7.36 For GMS and PMS, this further right to terminate can only be used where the commissioner is satisfied that the cumulative effect of the breaches is such that the commissioner considers that to allow the contract to continue would be prejudicial to the efficiency of the services to be provided under the contract. The commissioner does not usually have to establish this when terminating an APMS contract, although it should check the contract wording.
1.7.37 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to 6.10 above and part A, chapter 2: General duties of NHS England.
Termination due to the contractor carrying on business detrimental to the contract
1.7.38 For GMS and PMS, where the contractor is a company that is carrying on business which the commissioner considers is detrimental to the contractor performance of the contract, the commissioner may give notice to the contractor requiring that it ceases carrying on the relevant business within a specified period (which must not be less than 28 days from the date the notice was given). This termination right does not have to be included in an APMS contract but the commissioner should check the specific contract to see whether it is included.
1.7.39 Where the contractor has not satisfied the commissioner that it has ceased carrying on the business by the end of the notice period, the commissioner may by further written notice terminate the contract immediately (or from such date set out in the notice).
1.7.40 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to 6.10 above and part A, chapter 2: General duties of NHS England.
Termination due to partnership matters
1.7.41 A commissioner has a right to terminate a GMS contract where:
- the contractor is 2 or more persons practising in partnership
- where one or more partners have left the practice during the contract; and
- if the commissioner reasonably considers that the changes in the membership of the partnership are likely to have a serious adverse impact on the ability of the contractor or the commissioner to perform its obligations under the contract
1.7.42 Where this occurs, the commissioner may terminate the contract by notice in writing on such date as is set out in the notice. The notice must contain the commissioner’s reasons for considering that the change in the membership of the partnership is likely to have a serious adverse impact on the ability of the contractor or the commissioner to perform its obligations under the contract.
1.7.43 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to 6.10 above and part A, chapter 2: General duties of NHS England.
Termination due to breach of Regulation 5
1.7.44 Regulation 5 sets out conditions that the contractor must satisfy to enter into a GMS contract. There are a number of rights of termination relating to these conditions, which can be found at GMS Regulations 2015, Schedule 3, paragraph 65.
1.7.45 NHS England’s general duties may be triggered by termination in these circumstances. For further information, please refer to 6.10 of this chapter and part A, chapter 2: General duties of NHS England.
1.8 Consequences of termination
1.8.1 Contracts usually contain certain obligations on both parties on termination of the contract. The GMS Regulations, PMS Regulations and APMS Directions do not set out any requirements for primary care contracts to contain such provision, but the standard GMS Contract contains a number of obligations including provisions relating to:
- co-operation in dealing with any outstanding matters
- delivering up property owned by the other party; and
- carrying out a financial reconciliation
1.8.2 It is likely that PMS agreements and APMS contracts will contain similar provisions. The commissioner should consider the relevant contract to determine what obligations are set out on termination.
1.9 Dealing with Care Quality Commission issues
1.9.1 Commissioners may become aware of potential contract breaches when the CQC takes action following an inspection. CQC action may include suspending registration or cancelling registration completely. Whenever the commissioner becomes aware of issues identified and/or action taken by the CQC, it needs to consider those issues to see if any contractual action should be taken too.
1.9.2 Where evidence from the CQC’s findings and/or any further investigation by the commissioner identifies any breach(es) of contract, the commissioner should work through this chapter in the usual way to determine what steps to take. Often, CQC action will highlight a number of breaches and this may result in several breach or remedial notices being served.
1.9.3 In some cases, the issues identified may be so significant that it is appropriate to consider termination of the contract. In very serious cases, it may be possible to move straight to termination, if an appropriate termination right arises. The position can be complex, particularly where, for example, a suspension has removed any immediate risk to patient safety and the contractor has been given a period of time by the CQC to address the issues. In those cases, it may be appropriate to wait and see whether the contractor complies with the CQC’s requirements, rather than moving straight to termination. Commissioners should seek legal advice if they are unsure how to proceed.
1.9.4 Issues identified by the CQC will sometimes form part of a wider pattern of problems under the contract, in which case the commissioner should consider the full range of problems in deciding appropriate next steps.
1.9.5 During any period of suspension by the CQC, the commissioner will need to ensure that the patients of that practice are able to access primary medical services elsewhere. It may be that the cost of any caretaking arrangement can be partly off-set by appropriate deductions under any breach or remedial notice being served in relation to the issues leading to suspension (see 1.3.20 and 1.3.33 of section 1.3: Remedial notices and breach notices).
1.9.6 If a contractor’s CQC registration is cancelled, it will not be able to provide any services and the commissioner will need to terminate the contract. The commissioner should, however, be aware that the cancellation process can take time and that there is an appeal period following cancellation. Cancellation should not be relied on as final until that appeal period has expired or any appeal has been determined. See chapter 2: Unplanned/unscheduled and unavoidable practice closedown for further information.
2. Unplanned/unscheduled and unavoidable practice closedown
2.1 Introduction
2.1.1 When a GP practice closes at short notice, it is important that commissioners respond and act in a timely way. Such closures may be a result of actions by the CQC – for example, voluntary closure in response to an adverse inspection or cancellation of the practice’s registration – or due to the sudden inability of a provider to continue providing a service for some other reason such as bankruptcy.
2.1.2 Furthermore, it is critical that the management and transfer of patient records (both paper and digital) are undertaken in a secure and robust manner. It is important that adherence to all applicable information governance, records management and data protection regulations and data protection principles are maintained throughout this process.
2.2 Scope
2.2.1 This guidance clarifies the role of the commissioner and the engagement required with patients and any partner organisations: for example, NHS England or CQC. This chapter is intended as guidance with which commissioners can work, with 4 fundamental principles at the core:
- the needs of the registered patients must be at the heart of all decisions and actions
- in many cases taking preventive action in conjunction with support could be a preferable option to closing a practice
- in circumstances where this chapter applies (for example, a closure is unavoidable or in the best interests of patients), all partners and stakeholders should know what to do, when and how, and work effectively together to minimise any disruption to patients and services
- effective communication must be maintained throughout with patients and their families and carers and with other partners (for example, patient participation groups, LMCs and Healthwatch)
2.3 Roles and responsibilities
Commissioners
2..3.1 The commissioner will take the lead in the following actions:
- ensure appropriate interim measures are put in place (for example, a caretaker GP) to keep people safe after the identification of concerns or issues or, at the very latest, the point it is informed of the closure
- establish a team with specialist skills to oversee the closure, including contracting and communications staff, and lead on arranging meetings/consultations with any partners
- establish a task and finish group to oversee the process
- co-ordinate assessments of the practice’s registered list to ascertain patient needs and preferences. This should be completed by individuals with the relevant skills and governance to access patient records (where this is required) or by those brought in for their specialist skills (risk-stratified, for example, vulnerable patients, children in care and end of life patients)
- communicate to patients the details of alternative GP practices which could provide essential and minor surgery, including any details on the current quality of the service (that is, links to nhs.uk website, etc)
- maintain ongoing consultative relations with patients, their families, other local GP practices, the PCN and any other system partners to ensure they are kept informed at each step of the process
- commission new services and arrange people to move practices, including a review of the placement after a reasonable timeframe
- identify a lead to co-ordinate communications
- engage with the local medical committee (LMC)
2.3.2 In the event the practice physically closes, the commissioner/lead commissioner will:
- put in place arrangements for practice post to be redirected to the commissioner and where appropriate make a personal visit to the premises
- forward clinical correspondence to PCSE for 28 days and PCSE will manage onward forwarding to any new provider(s). GP clinical records are delivered by City Sprint on behalf of PCSE so as part of the closedown process, the closed practice is removed from the delivery locations. The PCSE address for returning correspondence can be found on the PCSE website
- after 28 days, mail is redirected to the commissioner, but it is not forwarded to the new provider(s). The commissioner will return clinical correspondence to the sender (hospitals, etc) and should inform the sender of the new provider(s). The sender should update its records accordingly to prevent reoccurrence
- ensure call forwarding arrangements are in place or appropriate answerphone messages are established for the closing practice to alert patients, and inform 111, out-of-hours services
- as part of the practice closedown, the commissioner will ensure that legacy IT hardware is removed from the practice, Health and Social Care Network (HSCN) connections are terminated and clinical system call-off agreements are ended as part of the GP IT system de-commissioning activities
- provide guidance to review, remove or copy files/folders that may be required by the outgoing owners
GP practice (during any period where the practice is still open)
2.3.3 The commissioner will ask the GP practice to:
- assist with ensuring appropriate interim measures are put in place to keep people safe after the identification of concerns
- assist the commissioner with the assessment of and communication with residents and their families to ascertain their needs and preferences
- assist the commissioner in any patient engagement, in particular with those people accessing services provided at or by the GP practice and their families
- as part of the practice closedown, work with the commissioner to ensure legacy IT hardware is removed from the practice as part of the GP IT system de-commissioning activities
- review and act on any guidance provided by the commissioner in relation to the closure
- record, collate and remove prescription pads. This includes both handwritten and computer scripts
- ensure all drugs/medicines in the practice are noted and handed in to the local pharmacy and signed for
Primary Care Support England
2.3.4 As part of any practice closedown, PCSE makes a site visit to remove, store and forward patient records to a new provider(s). Patient records should contain reprints of electronic records for patients who have not re-registered at the point of practice closure and will need to be individually placed in transit polytopes. Records will only be collected from the closing practice’s main site. The GP practice should send PCSE a list of records that are being collected. Records are held in archive until the patient re-registers or the retention period expires, and then they are securely destroyed. Further information can be found at: practice mergers and closures resources
Care Quality Commission
2.3.5 The CQC will lead in the following actions:
- share with the commissioner any information held about the quality of the current service
- share with the commissioner any information held about the quality of alternative services being considered, including the model of care used
- share with the commissioner any information on other providers likely to be involved in the provision of care to people at the new service
- consider bringing forward inspection or other evaluative activities for alternative providers where only limited quality information is available (lead role)
[Note: ‘share with the commissioner’ does not have to be in writing and could be verbal or as part of any scheduled or regular meetings.]
Local medical committee
2.3.6 The LMC for the area will be engaged in the following processes:
- made aware of the engagement occurring with patients
- made aware of any interim proposals and immediate next steps
- made aware of any long-term plans
This recognises that LMCs will champion the welfare of its members and wider practice staff.
2.4 The process
2.4.1 The process for a planned practice closedown commences between 9 and 15 months prior to the scheduled end date of the contract. For unplanned closure(s), it will be necessary to undertake a rapid assessment and determine the most appropriate course of action.
2.4.2 In the large majority of cases where closure is rapid (that is, immediate removal of CQC registration), the most appropriate course of action will likely involve an initial ‘caretaker’ arrangement (another GP or GP practice team) temporarily overseeing the practice at the closing practice’s existing premises and the care of its registered list. Please refer to part B, chapter 1, section 1.6: urgent contacts.
2.4.3 In the very unusual circumstance that this is not possible, it may be necessary to rapidly disperse the list. While the NHS Constitution is clear that patients have a right to choose their GP practice, to mitigate against the risk of patients being without care, the commissioner may temporarily assign a patient to an alternative provider. However, the patient must be advised of their rights under the NHS Constitution to change GP practice at any time.
2.4.4 Patient assignment is also possible during any list dispersal (that is, at the end of a ‘caretaker period’) for the same reason. This should be as a last resort, such as when the commissioner has been unable to contact the patient.
2.5 Key steps (in the case of a list dispersal)
- Patients are contacted in the first instance advising them of the list dispersal and available options (that is, neighbouring practices accepting patients).
- In the event of no response or no registration at another practice, patients are re-contacted advising them again of the list dispersal and available options (that is, neighbouring practices accepting patients). Patients should also be advised at this point that, to prevent risk to ongoing patient care, particularly in vulnerable patient groups, patients who do not re-register or contact the commissioner to advise that they do not wish to be registered with a GP, will be allocated to another practice.
- In the event of no response or no registration at another practice following the second reminder, patients must be allocated to a GP practice (except where they have not been seen or received treatment for 5 years or more – as confirmed by the GP practice). Commissioners should adopt the same approach as that set out in paragraphs 39 and 40 of Schedule 3, Part 4 ‘Assignment of patients to lists’, paragraphs 39 and 40 of the GMS Regulations 2015 or Schedule 2, Part 4, paragraphs 38 and 39 of the PMS Regulations 2015.
- The patient must then be notified in writing of the allocation, the reason for the allocation and of their rights under the NHS Constitution to de-register or re-register at an alternative GP practice should they wish.
- It is imperative that at the end of the process, all patient records and any associated data pertaining to patients (including digital records) and any clinical correspondence are transferred to the provider with which the patient has registered. This process will generally be routine and, in any case, is triggered for digital records when the patient registers at an alternative practice.
- For the avoidance of doubt, at the point of closure, all patients who have not self-registered at an alternative GP practice should be allocated to another GP practice (except where they have not been seen or received treatment for 5 years or more). It is recognised that this may temporarily result in the allocation of ghost patients or patients who have moved away; however, this will be corrected through the rolling list maintenance programme.
- The GP clinical system should be monitored by the commissioner or nominated IT delivery partner for a diminishing patient list. The GP clinical system should not be decommissioned until all patients have dispersed/re-registered either with their practice of choice or through allocation or, in the case of orphaned records (where neither allocation nor re-registration occurs), the records have transferred to NHS England as the data controller.
- Allocations should however have regard to paragraphs 23 to 31 of Schedule 3, Part 2 of the GMS Regulations 2015, and paragraphs 22 to 30 of Schedule 2, Part 2 of the 2015 PMS Regulations 2015 in relation to the removal of patients (see below):
- removal from the list at the request of the patient
- removal from the list at the request of the contractor
- removal from the list of patients who are violent
- removal from the list of patients registered elsewhere
- removal from the list of patients who have moved
- removal from the list of patients whose address is unknown
- removal from the list of patients absent from the UK, etc
- removal from the list of patients accepted elsewhere as temporary residents
- removal from a list of pupils of a school
- termination of responsibility for patients not registered with the contractor
2.5.1 They should also have regard to paragraph 40 (GMS) and 39 (PMS) ‘factors relevant to assignments’; namely:
When assigning a person as a new patient to a contractor’s list of patients, the Commissioner must have regard to:
a. the preferences and circumstances of the person;
b. the distance between the person’s place of residence and the contractor’s practice premises;
c. any request made by a contractor to remove the person from its list of patients within the preceding period of six months beginning with the date on which the application for assignment is received by the Commissioner.
d. whether, during the preceding period of six months beginning with the date on which the application for assignment is received by the Commissioner, the person has been removed from a list of patients on the grounds referred to in:
i. paragraph 23 (relating to circumstances in which a patient may be removed from a contractor’s list of patients at the request of the contractor),
ii. paragraph 24 (relating to circumstances in which a patient who is violent may be removed from a contractor’s list of patients), or
iii. the equivalent provisions to those paragraphs in relation to arrangements made under section 83(2) of the NHS Act 2006 (which relates to the provision of primary medical services) or under a contract made in accordance with the General Medical Services Contracts Regulations;
e. in a case to which sub-paragraph (d)(ii) applies (or to which the equivalent provisions as mentioned in sub-paragraph (d)(iii) apply), whether the contractor has appropriate facilities to deal with such patients; and
f. such other matters as the Commissioner considers relevant.
2.5.2 It is imperative that at the end of the process, all patient records, and any associated data pertaining to patients (including digital records) and any clinical correspondence are transferred to the provider with whom the patient has registered. This process will generally be routine and in any case, is triggered for digital records when the patient registers at an alternative practice.
2.5.3 For the avoidance of doubt, at the point of closure, all patients that have not self- registered at an alternative GP practice should be allocated to another GP practice (except where they have not been seen or received treatment for 5 years or more). It is recognised that this may temporarily result in the allocation of ghost patients or patients that have gone away, however, this will be corrected through the rolling list maintenance programme.
2.5.4 The GP Clinical system should be monitored by the Commissioner or nominated IT Delivery Partner for a diminishing patient list. The GP Clinical system should not be decommissioned until all patients dispersed/re-registered either with their practice of choice, allocation or in the case of Orphaned Records (where neither allocation nor re-registration occurs) the records transfer to NHSE as the data controller.
2.6 Engagement and re-procurement
2.6.1 Where arrangements have been made for a caretaker to temporarily manage the GP practice (refer to part B, chapter 1, section 1.6: urgent contacts) or a practice has terminated a contract with little notice (for example, 6 months), the commissioner should refer to the 3 stages and annexed templates in part B, chapter 10: Practice closedown (planned/scheduled).
2.6.2 It is recognised that in these circumstances it may not be possible to undertake each of these stages as vigorously or to the same timescales as if there were a 12–15 month period available, as is often the case with a planned closure.
2.6.3 NHS England has a number of statutory duties relating to the exercise of its functions including reducing health inequalities and public involvement. The commissioner must ensure that its actions in re-procuring a contract or dispersing a list and any consequential actions ensure compliance with these duties. Please refer to part A, chapter 2: General duties of NHS England for further guidance.
2.6.4 However, in an urgent situation, it may be necessary to balance the duty to involve the public alongside the public interest in maintaining continuity of care and protecting the health, safety and welfare of patients or staff. If a commissioner considers acting in a way that may not comply with its statutory duties, it should seek further advice.
2.7 Relevant PCSE information and documentation
3. Death of a contractor
3.1 Introduction
3.1.1 The aim of this policy is to provide consistency when dealing with the death of a contractor, whether they are a single-handed contractor or in a partnership, including with consideration of GMS contracts, PMS agreements and APMS contracts.
3.1.2 This policy outlines the procedure to follow when a contractor dies. This is a rare occurrence, but there are certain steps to follow within fixed timescales that are laid down in legislation.
3.2 Individual – GMS contract
3.2.1 Where a GMS contract is with an individual medical practitioner and that practitioner dies, the contract must terminate at the end of the period of 7 days after the date of the contractor’s death unless before the end of that period:
- the commissioner and the contractor’s personal representatives agree in writing that the contract will continue for a further period of up to 28 days after the initial 7-day period (that is, the longest possible extension is 35 days from the date of death)
- the contractor’s personal representatives have confirmed in writing to the commissioner that they wish to employ or engage one or more general medical practitioners to assist in continuing to provide clinical services under the contract during that period
- the commissioner agrees to provide reasonable support which would enable the provision of clinical services under the contract to continue during that period
- the commissioner and the personal representatives agree the terms on which clinical services under the contract can continue to be provided during that period
3.2.2 The commissioner should issue a confirmation letter setting out the timescales of the continuation. Annex 79 provides a template letter.
3.2.3 Note that it is not possible to extend the existing GMS contract for a longer period. Termination is mandatory and automatically takes place. In relation to planning for caretaking, re-procurement or list dispersal on termination, commissioners should refer to chapter 2: Unplanned unscheduled and unavoidable practice closedown.
3.3 Individual – PMS or APMS contract
3.3.1 Where the PMS agreement or APMS contract is with a single individual and that individual dies, the contract shall terminate at the end of the period of 7 days after the date of the contractor’s death unless before the end of that period, the commissioner has agreed in writing with the contractor’s personal representatives that the contract should continue for a further period not exceeding 28 days after the end of the period of 7 days (that is, the longest possible extension is 35 days from the date of death).
3.3.2 The commissioner should issue a confirmation letter setting out the timescales of the continuation. The template letter in annex 79 can be used.
3.3.4 Note that it is not possible to extend the existing PMS agreement or APMS contract for any longer period. Termination is mandatory and automatically takes place. In relation to planning for caretaking, re-procurement, or list dispersal on termination, commissioners should refer to chapter 2: Unplanned/unscheduled and unavoidable practice closedown
3.4 Partnership – GMS contract
3.4.1 The GMS Regulations state that where the contract is with 2 or more individuals practising in partnership, the contract shall be treated as made with the partnership as it is from time to time constituted.
3.4.2 The default position in partnership law is that every partnership is dissolved as regards all the partners by the death of any partner. The partners can, however, change this position and agree between themselves that the partnership will not dissolve on the death of any partner. It is likely that most partnerships will have dealt with this issue in their partnership deed to avoid termination of their contract.
3.4.3 The GMS Regulations require GMS contracts to contain specific provisions relating to the dissolution of partnerships.
3.4.4 Where a partner dies, the GMS Regulations distinguish between GMS contracts that are entered into with a contractor that consists of only 2 individuals practising in partnership and those GMS contracts where the contractor consists of more than 2 individuals.
2 individuals practising in partnership – GMS contract
3.4.5 Where the contractor consists of 2 individuals practising in partnership and the partnership is dissolved or terminated due to the death of one of the partners, the surviving partner must notify the commissioner in writing as soon as is reasonably practicable of the death of their partner.
3.4.6 Where the commissioner receives such a notice, it must acknowledge receipt of the notice in writing.
3.4.7 If the surviving partner is a general medical practitioner, the contract will continue with that individual. The commissioner may vary the contract but only to the extent that it is satisfied it is necessary to reflect the change in status of the contractor from a partnership to an individual medical practitioner. The commissioner must notify the contractor in writing of the wording of the proposed variation and the date on which that variation is to take effect.
3.4.8 Annex 80 provides a template notification letter. A variation notice will need to be included with this letter.
3.4.9 To provide assurance that the individual is able to meet the contractual obligations, the commissioner should discuss continued service delivery options with the individual, bearing in mind the size of the practice, the range of services provided and any potential capacity issues.
3.4.10 If the surviving partner is not a general medical practitioner, the commissioner must enter into discussions with the surviving partner and use reasonable endeavours to reach an agreement to enable the provision of clinical services to continue under the contract. The commissioner may, if it considers it appropriate to enable clinical services under the contract to continue, offer the surviving partner reasonable support.
3.4.11 The commissioner may choose to consult the relevant LMC if it considers it appropriate or any other person that the commissioner considers necessary.
3.4.12 Where the commissioner reaches an agreement with a surviving partner who is not a general medical practitioner, the commissioner must notify that individual confirming:
- the terms on which the commissioner agrees to the contract continuing with that individual
- the interim period during which the contract is to continue which must not exceed 6 months
- that the individual will employ or engage a general medical practitioner for the interim period to assist in the provision of clinical services under the contract
- the support, if any, which the commissioner is to provide to enable clinical services under the contract to continue during the interim period
3.4.13 Annex 80 provides a template notification letter. A variation notice will need to be included with this letter.
3.4.14 Where the commissioner cannot reach an agreement with the surviving partner or if the surviving partner does not wish to employ or engage a medical practitioner, the commissioner must terminate the contract immediately by serving notice in writing on the surviving partner.
3.4.15 The commissioner must also terminate the contract in writing to the surviving partner if:
- the surviving partner wishes to withdraw from the agreed arrangements at any stage during the interim period
- at the end of the interim period, the contractor has not entered into partnership with a general medical practitioner who is not a limited partner
3.4.16 Where the commissioner intends to terminate the contract, please refer to part C, chapter 1: Contract breaches, sanctions and terminations for further information on considerations relating to terminating a contract.
3.4.17 Annex 81 provides a template termination letter.
More than 2 individuals practising in partnership – GMS contract
3.4.18 Where there are more than 2 individuals practising in partnership, the death of one of the partners may result in the partnership being dissolved. This may not always be the case as the partnership arrangements between the partners may state that the partnership will continue or make other provision on the death of a partner that does not result in the dissolution of the partnership.
3.4.19 Where the partnership is not dissolved or terminated, the contract will continue and the provisions below will not apply provided that the partnership remains eligible to hold the GMS contract. Please refer to part B, chapter 1: Contracts described for further information on eligibility requirements.
3.4.20 It is possible for the contract to continue where the partnership is dissolved or terminated for whatever reason (which may be due to the death of a partner) and the contractor consists of more than 2 individuals practising in partnership. The contract may continue with one of the former partners if the following conditions apply:
- the former partner must be nominated by the contractor
- the former partner must be a medical practitioner who meets the condition in Regulation 4(2)(a) of the GMS Regulations
3.4.21 The nomination of the former partner by the contractor must be:
- in writing and signed by all the persons who are practising in partnership
- specify the date on which the contractor proposes to change its status from that of a partnership to that of an individual medical practitioner
- provided to the commissioner at least 28 days in advance of the date on which the contractor proposes to change its status from that of a partnership to that of an individual medical practitioner
- specify the name of the medical practitioner with whom the contract will continue, which must be one of the partners
3.4.22 Where the commissioner receives such a nomination, it must acknowledge receipt of the notice in writing before the date specified in the nomination as the date on which the contractor proposes to change its status from that of a partnership to that of an individual medical practitioner.
3.4.23 The commissioner may vary the contract but only to the extent that it is satisfied it is necessary to reflect the change in status of the contractor from a partnership to an individual medical practitioner. The commissioner must notify the contractor in writing of the wording of the proposed variation and the date on which that variation is to take effect.
3.4.24 Annex 81 provides a template notification letter. A variation notice will need to be included with this letter.
3.5 2 or more signatories – PMS agreement
3.5.1 The PMS regulations do not allow PMS agreements to be treated as made with a partnership. Where individuals are practising in partnership, the PMS agreement will be entered into with each individual (who may or may not be in partnership). The individual signatories to a PMS agreement collectively form the contractor. The PMS Regulations do not require a PMS agreement to define a specific process for any variation to the signatories. The commissioner must, therefore, review the relevant PMS agreement to determine whether any provisions have been added relating to this and prior to following any process for variation.
3.5.2 Ideally, a surviving signatory to a PMS agreement will notify the commissioner in writing as soon as reasonably practicable of the death of their co-signatory.
3.5.3 On receipt of the notification from the surviving co-signatory(ies), the commissioner will need to consider the implications that the death of the co-signatory will have on the ongoing provision of services under the agreement
3.5.4 Where the commissioner is satisfied that the remaining signatory(ies) is eligible to hold the agreement and agrees that the agreement is to continue, the agreement will need to be varied to remove the deceased as a signatory.
3.5.5 The process above does not affect any right that the commissioner may have to terminate the agreement under any terms of the agreement.
3.6 2 or more signatories – APMS contract
3.6.1 The commissioner must review the relevant APMS contract to determine whether any provisions relate to the death of a contractor prior to following any process for variation.
3.6.2 Where no provisions cover this scenario, 3.5.2 to 3.5.5 above are likely to be relevant.
3.7 Practical issues arising from the death of a contractor
Request to form a partnership
3.7.1 Where a GMS contract is held by an individual as a result of the death of a partner, that individual (like any individual GMS contractor) may propose to practise in partnership with one or more persons during the existence of the contract. Please refer to part B, chapter 8: Contract variations for more information on the relevant process and obligations of the commissioner.
Procuring a new contract
3.7.2 Where death of a contractor results in termination of the contract in any of the ways described above, the commissioner will need to decide whether to procure primary care medical services to replace the contract.
3.8 Relevant PCSE information and documentation
4. Managing disputes
4.1 Introduction
4.1.1 This policy describes the process to determine the action required where a contractor has requested to follow the NHS dispute resolution process or where the commissioner elects to follow the NHS dispute resolution procedure.
4.1.2 The policy focuses on primary medical services contracts in their various forms.
4.2 Background
4.2.1 The commissioner must identify whether the contract is an NHS contract or a non-NHS contract. In GMS contracts, the commissioner can do this by reviewing clause 3.1 of the standard GMS contract. A similar clause will also be set out within PMS agreements and APMS contracts.
4.2.2 An NHS contract (as set out at section 9 of the NHS Act 2006) is an arrangement under which one health service body arranges for the provision of goods or services to another health service body. It must not be regarded as giving rise to contractual rights or liabilities.
4.2.3 A non-NHS contract is where the contract is legally binding.
4.2.4 Contractors have the right to be regarded as a health service body under Regulation 10 of the GMS Regulations or Regulation 9 of the PMS Regulations or where the APMS contractor is a health service body by virtue of section 9 of the NHS Act.
4.2.5 Where a contractor is regarded as being a health service body, its contract will be an NHS contract. Where a contractor is not regarded as a health service body, its contract will not be an NHS contract. Health service body status affects the eligibility and application process for NHS dispute resolution.
4.2.6 GMS contracts and PMS agreements require the parties to make every reasonable effort to communicate and co-operate with each other to resolve the dispute before referring the dispute for determination in accordance with the NHS dispute resolution procedure or, where applicable, before commencing court proceedings.
4.2.7 There are 2 different routes that can be taken for resolving contractual disputes, depending on the contractor’s health service body status:
4.2.7.1 where the contractor is a health service body and the contract is an NHS contract, the steps laid out in this policy will be used to resolve all matters of dispute. The parties should not make a claim at court in relation to the contracts; or
4.2.7.2 where the contractor is not a health service body and the contract is a non-NHS contract, the dispute can either be resolved using the process described in this policy or using the court system
4.2.8 The dispute resolution process for APMS contracts is specific to the parties’ agreement as set out in the APMS contract. The APMS contract must be reviewed in the event of a dispute and that process followed. The APMS Directions do not require the NHS dispute resolution to be included in the APMS contract and more commercial terms are usually set out.
4.2.9 The use of the court system can be an expensive and public route. In normal circumstances, non-health service bodies will elect to follow the NHS dispute resolution.
4.2.10 Where the parties have followed this policy and the NHS dispute resolution to the end determination, the result is binding. A second referral to the court system for a further ruling on the same issue cannot be made other than to enforce the decision as having the status of a county court judgement or to seek judicial review of the process.
4.3 Managing disputes – informal process
4.3.1 The parties must make every reasonable effort to communicate their issues in relation to decision-making and rationale and must co-operate with each other to resolve any disputes that emerge informally before considering referring the matter for determination through formal dispute resolution procedures.
4.3.2 The formal process should not be initiated until the informal process has been exhausted and it should be noted that both parties may wish to involve the relevant professional representative: for example, the LMC.
4.3.3 The use of an informal resolution process helps develop and sustain a partnership approach between contractor and commissioner.
4.3.4 The informal process may include (but is limited to):
- regular telephone communications
- face-to-face meetings at a mutually convenient location
- written communications
4.3.5 It is essential that the commissioner maintains accurate and complete written records of all discussions and correspondence on the contract file in relation to the dispute at all levels of dispute resolution. The commissioner should ensure that it responds to contractor concerns and communications in a timely and reasonable manner.
4.4 Managing disputes – stage 1 (local dispute resolution)
4.4.1 The timescales set out in this stage 1 are indicative only. The commissioner should ensure any timescales used are appropriate to the circumstances. Regardless of timescales, the parties must ensure that every reasonable effort to communicate and co-operate with each other is made prior to invoking stage 2 of the NHS dispute resolution procedure.
4.4.2 Where a dispute arises, the commissioner should refer to the relevant policy that covers the issue that caused the dispute to determine whether due process has been followed.
4.4.3 The contractor should notify the commissioner of its intention to dispute one or more decisions made in relation to its contract. This notification should usually be received no later than 28 days after the commissioner advises the contractor of its decision except in exceptional circumstances.
4.4.4 The commissioner will immediately cease all actions in relation to the disputed notice or decision until:
- there has been a determination of the dispute and that determination permits the commissioner to impose the planned action
- the contractor ceases to pursue the NHS dispute resolution procedure or court proceedings
4.4.5 Where the commissioner is satisfied that it is necessary to terminate the contract or impose a contract sanction before the NHS dispute resolution procedure is concluded to:
- protect the safety of the contractor’s patients; or
- protect NHS England from material financial loss
then the commissioner shall be entitled to terminate the contract or impose the contract sanction at the end of the period of notice it served. This should only be followed with close reference to the GMS Regulations and PMS Regulations, pending the outcome of that procedure.
4.4.6 The paragraphs below set out a process that may be adopted for stage 1 (local dispute resolution).
4.4.7 The commissioner may acknowledge the notification of dispute within 7 days of receipt and request the submission of supporting evidence from the contractor within a further 28 days from the date they receive the letter. Annex 82 provides an example acknowledgement letter.
4.4.8 On receipt of the evidence the commissioner should review the evidence within 28 days and invite the contractor to attend a meeting, which should be as soon as possible, but at the very latest within a further 28 days. The contractor(s) has the opportunity to invite representative bodies to support it at the meeting: for example, the LMC. Annex 83 provides an example invitation letter.
4.4.9 Once the meeting has been held, the commissioner should notify the contractor in writing of the outcome of the meeting, whether the dispute will now need to move to stage 2 of the NHS dispute resolution procedure (refer annex 84: example stage 1 outcome letter (NHSR PCA referral)) or that the dispute has been successfully resolved (refer to annex 85: example stage 1 outcome letter (matter(s) resolved).
4.4.10 Where the matter is resolved, the issue can be deemed closed, and the commissioner should document the outcome accordingly on the contract file.
4.4.11 Where the matter remains unresolved, the process may be escalated to the next stage of the dispute resolution procedure.
4.4.12 At this point the commissioner should commence preparation of the contract file to ensure that if and when NHSR or the court requests submission of evidence in respect of the dispute, the documentation is in order.
4.5 Managing disputes – stage 2 (NHS dispute resolution procedure)
4.5.1 The informal process and stage 1 (local dispute resolution) should be exhausted before proceeding to this stage of the process. The commissioner or a contractor wishing to follow this route must submit a written request for dispute resolution to:
- Postal address: NHS Resolution, Primary Care Appeals, 8th Floor, 10 South Colonnade, Canary Wharf, London E14 4PU
- Email: nhsr.appeals@nhs.net
Primary Care Appeals (PCA) at NHSR carries out the NHS dispute resolution functions of the Secretary of State in the GMS Regulations and the PMS Regulations and any written request for dispute resolution should include:
- the names and addresses of the parties to the dispute
- a copy of the contract
- a brief statement describing the nature and circumstances of the dispute
4.5.2 The written request for dispute resolution must be sent within 3 years from the date on which the matter giving rise to the dispute occurred or should have reasonably come to the attention of the party wishing to refer the dispute. Please see NHSR PCA determination reference 17156 for further details on the date that the dispute should have reasonably come to the attention of the relevant party.
4.5.3 The commissioner will be required to prepare documentation evidence and potentially an oral presentation in response to evidence presented in support of the dispute. Each party will be asked to prepare representations on the dispute, which will be circulated to the other party, and given an opportunity to provide observations on the other party’s representations. Again, the observations of each party will be circulated to the other party.
4.5.4 The commissioner should not underestimate the preparation that will be required in the event that evidence is required by NHSR PCA, as all records pertaining to the contractor in question may be required, including (but not limited to) all contract documentation and contract variations, all written correspondence (both to and from the commissioner and the contractor) and any electronic correspondence that may have passed between the parties in relation to the dispute. This process will benefit from a clearly recorded contract file.
4.5.5 The commissioner must ensure that records of communications and contract files are maintained to a high standard and all documentary evidence is collated correctly prior to submission to NHSR PCA.
4.5.6 Once NHSR PCA has reached a conclusion (the determination) the commissioner will receive a copy and will be required to act on it. Parties involved in dispute resolution should follow the NHSR PCA guidance note.
Delegated commissioning arrangements
The Delegation Agreement includes a section on claims and litigation which is likely to include a dispute with a GMS, PMS or APMS contractor that has been referred to stage 2 of the NHS dispute resolution procedure. In such cases, the commissioner is required to act in accordance with the delegation agreement which includes but is not limited to:
- notifying NHS England of any documents concerning the dispute and providing copies of these documents
- co-operating fully with NHS England in relation to such dispute and the conduct of such dispute
- providing, at its own cost, to NHS England all documentation and other correspondence that NHS England requires for the purposes of considering and/or resisting such dispute
- at the request of NHS England, taking such action or step or providing such assistance as may in NHS England’s discretion be necessary or desirable having regard to the nature of the dispute and the existence of any time limit in relation to avoiding, disputing, defending, resisting, appealing, seeking a review or compromising such dispute or to comply with the requirements of NHSR PCA in relation to such dispute
4.6 Other dispute resolution procedures
4.6.1 The GMS and PMS Regulations allow the NHS dispute resolution procedure to be used by the contractor as a means of resolving every dispute except where an assessment panel determines that the commissioner may assign new patients to contractors that have closed their practice list of patients.
4.6.2 Disputes may also arise prior to a contract being entered into. Such disputes will relate to the eligibility of the person seeking to enter the contract or contract terms.
4.6.3 Where the commissioner is of the view that a person seeking to enter a contract does not meet the eligibility conditions (please refer to the part B, chapter 1: Contracts described for further information), the commissioner must notify the person in writing.
4.6.4 This notice must state the commissioner’s view of the person’s eligibility, reasons for that view and guidance on the person’s right of appeal.
4.6.5 Where the commissioner has issued such a notice, the recipient of the notice has a right of appeal to the First-Tier Tribunal.
4.6.6 Where the dispute relates to the parties being unable to agree on a particular proposed term of a GMS contract or PMS agreement, either party may refer the dispute to the Secretary of State to consider and determine the matter in accordance with:
- for GMS contracts, Part 12 and Regulation 9 of the GMS Regulations
- for PMS agreements, Part 13 and Regulation 8 of the PMS Regulations
- except where both parties to the prospective agreement are health service bodies (in which case section 9 of the NHS Act applies)
4.7 Assignment of patients to lists: procedure relating to determinations of the assessment panel
4.7.1 Where an assessment panel determines that the commissioner may assign new patients to contractors which have closed their practice list of patients, any contractor specified in that determination may refer the matter to the Secretary of State to review the determination of the assessment panel.
4.7.2 If a referral is made to the Secretary of State, it shall be reviewed in accordance with the following procedure:
- where more than one contractor specified in the determination of the assessment panel wishes to refer the matter for dispute resolution, those contractors may, if they all agree, refer the matter jointly, and in that case the Secretary of State shall review the matter in relation to those contractors together
- within the period of 7 days from the date of the determination by the assessment panel, the contractor(s) shall send to the Secretary of State a written request for a dispute resolution which shall include or be accompanied by:
- the names and addresses of the parties to the dispute
- a copy of the contract (or contracts)
- a brief statement describing the nature and circumstances of the dispute
4.7.3 Each party will be asked to make representations and observations on the representations of the other party both of which will be allocated between the parties.
4.7.4 Within the period of 21 days from the date on which the matter was referred to them, the Secretary of State shall determine whether the commissioner may assign patients to contractors that have closed their lists of patients. If the Secretary of State determines that the commissioner may make such assignments, the Secretary of State shall also determine those contractors to which patients may be assigned.
4.7.5 The Secretary of State may not determine that patients may be assigned to a contractor which was not specified in the determination of the assessment panel.
4.7.6 In the case of a matter referred jointly by contractors, the Secretary of State may determine that patients may be assigned to one, some or all the contractors that referred the matter.
4.7.7 The period of 21 days for determination may be extended (even after it has expired) by a further specified number of days if an agreement to that effect is reached by:
- the Secretary of State
- the commissioner
- the contractor(s) that referred the matter to dispute resolution
4.7.8 The Secretary of State shall record the determination and the reasons for it in writing and shall give notice of the determination (including the record of the reasons) to the parties.
5. Adverse events (for example, flood and fire)
5.1 Background
5.1.1 Adverse incidents are dealt with in the force majeure provisions of the standard GMS contracts, PMS agreements and APMS contracts. Although these provisions are not required by the GMS Regulations, PMS Regulations or APMS directions, the majority of contracts will include them.
5.1.2 The commissioner is advised to check that the force majeure provisions are included in each contract and, if they are, to follow the guidance in this policy. This policy is only applicable where the contract in question has retained the recommended force majeure provisions.
5.1.3 The contractor is responsible for informing the commissioner of any force majeure event.
5.2 Contract wording
5.2.1 Clause 27.5 of the standard GMS contract states that:
“27.5.1 Neither party shall be responsible to the other for any failure or delay in performance of its obligations and duties under this contract which is caused by circumstances or events beyond the reasonable control of a party. However, the affected party must promptly on the occurrence of such circumstances or events:
(a) inform the other party in writing of such circumstances or events and of what obligation or duty they have delayed or prevented being performed; and
(b) take all action within its power to comply with the terms of this Contract as fully and promptly as possible.
27.5.2 Unless the affected party takes such steps, clause 27.5.1 shall not have the effect of absolving it from its obligations under this contract. For the avoidance of doubt, any actions or omissions of either party’s personnel or any failures of either party’s systems, procedures, premises, or equipment shall not be deemed to be circumstances or events beyond the reasonable control of the relevant party for the purposes of this clause, unless the cause of failure was beyond reasonable control.
27.5.3. If the affected party is delayed or prevented from performing its obligations and duties under the contract for a continuous period of 3 months, then either party may terminate this contract by notice in writing within such period as is reasonable in the circumstances (which shall be no shorter than 28 days).
27.5.4. The termination shall not take effect at the end of the notice period if the affected party is able to resume performance of its obligations and duties under the contract within the period of notice specified in accordance with clause 27.5.3 above, or if the other party otherwise consents”.
5.2.2 The provision of individual PMS agreements and APMS contracts should be reviewed and advice sought.
5.2.3 A force majeure event is one which is caused by circumstances beyond the reasonable control of either the commissioner or the contractor, could not have been avoided or mitigated with reasonable care and has had a material effect on the fulfilment of the contract.
5.2.4 Examples of events that may invoke the force majeure provisions are as follows:
- fire
- flood
- severe weather conditions and for which precautions are not ordinarily taken to avoid or mitigate the impact: for example, a severe hurricane
- industrial action which significantly affects the provision of public services or services on which the party is reliant
- death of a significant performer or close relative
- pandemic disease or circumstances that might otherwise be considered ‘an act of God’
- war
- civil war (whether declared or undeclared)
- riot or armed conflict
- radioactive, chemical or biological contamination
- pressure waves caused by aircraft or other aerial devices travelling at sonic or supersonic speed
- acts of terrorism
- explosion
5.2.5 Examples of events that would not be considered force majeure events are as follows:
- refurbishment of practice premises
- adverse weather in the winter months (including snow and ice)
- planned events (including elective surgery, leave, weddings and similar events)
- long-term sickness, maternity/paternity or adoption leave
5.3 Contract compliance
5.3.1 All contractors will likely be obliged under the terms of their contracts to promptly notify the commissioner of a force majeure event, detailing the cause or event, what service provision is being delayed or prevented and what business continuity action(s) within their power they are taking to comply with the terms of the contract as fully and promptly as possible.
5.3.2 Failure to notify the commissioner will mean that the contractor is not absolved from its obligations under the contract.
5.3.3 Neither party will be responsible to the other for any failure to delay in performing its obligations and duties under the contract which is caused by an event of force majeure.
5.3.4 Annex 86 provides a contractor’s preliminary notice of force majeure event which the commissioner can send to the contractor for completion.
5.3.5 The commissioner will record that the event has happened and provide the contractor with an acknowledgment letter. Annex 87 provides a template letter.
5.4 Clinical governance and risk management/termination
5.4.1 If the consequence of the contractor’s failure to deliver services is significant and poses a risk to patient safety or the efficiency of wider primary care services, the commissioner may wish to consider recording the incident on the risk register or whether it may invoke its termination rights.
5.4.2 If the service provision is delayed or prevented for a continuous period of 3 months, then either party will likely be able to terminate the agreement by notice in writing within a period which is reasonable (and no less than 28 days). This termination will not take effect where the service is resumed within the period of notice or if the contractor consents to this.
5.5 Appeals
5.5.1 The parties should refer to the chapter 4: Managing disputes for the process in relation to a dispute.
5.6 Payment and contract system
5.6.1 The parties should discuss the effect of force majeure on payments by the commissioner to the contractor. The commissioner should use its reasonable discretion in determining payments with regard to the need for the contractor to continue to provide services once it is no longer affected by the force majeure event provided the contract has not been terminated.
Part D: General
1. GP IT operating model: data and cyber security arrangements
1.1 Introduction
1.1.1 This chapter provides an overview of GP IT operating arrangements, as outlined in the GP IT operating model published by NHS England.
1.1.2 Particular references are made to data and cyber security arrangements and to providing GP IT services to practice sub-contractors.
1.2 Background
1.2.1 NHS England is accountable for the delivery of GP IT services, with responsibility for the commissioning of GP IT services delegated to ICBs under the NHS Act 2006 (as amended).
1.2.2 The contract requires the contractor to use and/or offer certain digitally enabled services to patients, including electronic patient records systems, patient online services, remote service provision, etc.
1.2.3 The ICB–practice agreement v3, which is signed by ICBs as commissioners and each constituent contractor, enables the ICB (NHS) to fund and provide and contractors to receive and use digital services related to the contract commitments. It also defines the responsibilities and obligations of the parties. This replaces the CCG–practice agreement v2 which remains applicable until such time as the contractor and commissioner sign the new ICB–practice agreement.
1.2.4 The GP IT operating model directs the commissioner on the digital services and support to be offered to the contractor and the standards applicable. The contract references the GP IT operating model for the applicable specification requirements and technical standards.
1.2.5 The Good practice guidelines for general practice electronic patient records (GPGv5) advises contractors on using these digital services effectively, safely and in accordance with the law and other standards. The contract requires that the contractor has regard to these guidelines.
1.3 GP IT services to be provided
1.3.1 The GP IT operating model provides a detailed schedule of ‘core and mandated’ requirements. These include:
1.3.1.1 Capability requirements for patient clinical systems (foundation solutions) and patient online digital services are met through national framework contracts (using the DSIC Framework Catalogue). The ICB–practice agreement and GP IT operating model describes the responsibilities of the practice and the ICB in choosing and selecting these solutions.
1.3.1.2 A range of requirements met through National Digital Services (for example, Electronic Prescription Service, NHS Mail, GP2GP and NHS App). There is no local choice for these solutions.
1.3.1.3 Enabling requirements (to support the above). Support services and IT infrastructure to meet these requirements must be offered to practices. These services must be provided in a manner which does not disadvantage any practice because of their choice of patient clinical system (foundation solution).
1.3.1.4 ICBs may also agree to meet ‘enhanced’ requirements to facilitate local service improvement and transformation supporting local strategic priorities to improve service delivery. It includes standards to ensure that all services provided through the GP IT operating model are compliant with regulations and controls for data protection, cyber security and clinical safety. ICBs are responsible for ensuring all these requirements are provided to the standards described in the GP IT operating model.
1.3.2 Practices will not be entitled to funding in lieu of services to be provided under the GP IT operating model (unless specifically stated in the GP IT operating model).
1.3.3 The following will be included in the appendices of each ICB–practice agreement (between the ICB and the practice):
- details of the services to be provided to the practice
- the supported premises
- sub-contractors with approved to access the practice digital services
- local support and maintenance levels
- local escalation procedure
- local data processing deed
1.3.4 Each practice needs to work with the ICB and any locally commissioned GP IT delivery partner(s), as described in the ICB–practice agreement, to enable effective and safe support of the IT infrastructure, respond to service incidents and maintain compliance with security standards, in line with national standards and locally agreed service level agreements.
1.3.5 ICBs should work in partnership with practices to develop a local digital strategy and delivery plans and set priorities and local direction for digital support services and technology.
1.3.6 As end users of the digital services, GPs and their staff need to be familiar with the GP IT services being provided locally, their responsibilities as end users and for the support arrangements and any local contingency and recovery processes in place when technology fails, particularly in cases of cyber security incidents.
1.4 Data security and protection
1.4.1 The NHS Data Security and Protection Toolkit (DSPT) is an online self-assessment tool that enables organisations to measure and publish their performance against the National Data Guardian’s 10 data security standards. The ICB–practice agreement requires practices to complete the DSPT annually. Local commissioned GP IT delivery partners (providers) are also contractually required to complete the DSPT.
1.4.2 The DSPT provides individual organisations with the necessary tools to assess adherence to the standards and level of cyber capability, as well as providing a national picture of data security across the health and social care system and intelligence for independent assurance processes. Through the Data Security Centre and the Cyber Security Programme, NHS England supports organisations to put those standards into practice.
1.4.3 An incident reporting tool for data security and protection incidents is provided within the DSPT.
1.4.4 Information from the DSPT will support CQC inspections, which include the importance of meeting the 10 data security standards:
The 10 data security standards:
Category: People Ensure staff are equipped to handle information respectfully and safely, according to the Caldicott principles
- Data security standard 1: All staff ensure that personal confidential data is handled, stored, and transmitted securely, whether in electronic or paper form. Personal confidential data is shared for only lawful and appropriate purposes
- Data security standard 2: All staff understand their responsibilities under the National Data Guardian’s data security standards, including their obligation to handle information responsibly and their personal accountability for deliberate or avoidable breaches
- Data security standard 3: All staff complete appropriate annual data security training and pass a mandatory test, provided through the redesigned Information Governance Toolkit
Category: Process Ensure the organisation proactively prevents data security breaches and responds appropriately to incidents or near misses:
- Data security standard 4: Personal confidential data is only accessible to staff who need it for their current role and access is removed as soon as it is no longer required. All instances of access to personal confidential data on IT systems can be attributed to individuals
- Data security standard 5: Processes are reviewed at least annually to identify and improve any which have caused breaches or near misses, or which force staff to use workarounds which compromise data security
- Data security standard 6: Cyber-attacks against services are identified and resisted and CareCERT security advice is responded to. Action is taken as soon as possible following a data breach or near miss, with a report made to senior management within 12 hours of detection. Significant cyber-attacks are to be reported to CareCERT immediately following detection
- Data security standard 7: A continuity plan is in place to respond to threats to data security, including significant data breaches or near misses, and it is tested once a year as a minimum, with a report to senior management
Category: Technology Ensure technology is secure and up to date:
- Data security standard 8: No unsupported operating systems, software or internet browsers are used within the IT estate
- Data security standard 9: A strategy is in place for protecting IT systems from cyber threats, based on a proven cyber security framework such as Cyber Essentials. This is reviewed at least annually
- Data security standard 10: IT suppliers are held accountable via contracts for protecting the personal confidential data they process and for meeting the National Data Guardian’s data security standards
1.4.5 Practices are supported to ensure patient data and information is used safely and securely and to prepare their own resilience to cyber security threats and to respond effectively and safely when they occur by:
- national services and security advice offered by NHS England’s Data Security Centre
- locally commissioned cyber security and information governance support services
1.4.6 The Network and Information Systems (NIS) Regulations 2018 gives further legal backing to the 10 data security standards by requiring those organisations identified as ‘operators of essential services’ to comply with defined security requirements.
1.5 Business continuity and critical incident management
1.5.1 Each practice will have a business continuity (BC) plan as part of its DSP toolkit (DSPT) compliance which will include responses to data security and cyber security threats/incidents, significant breaches or near misses and responses to a loss of access to patient records.
1.5.2 BC plans should also consider practice resilience arrangements including the capability for home and remote working, alternative consultation channels (for example, online, video) and exceptional demand management.
1.5.3 The ICB will provide advice/guidance to support the development of the digital element of the practice BC plan. ICBs should approve practice BC plans. In the event of the practice BC plan being invoked, the ICB will ensure specialist technical support is available as necessary.
1.5.4 All practices must register with the MHRA Central Alerting System which will be utilised as required, to support any national cyber security incident, including urgent out of hours contact.
1.5.5 It is important for all practice staff to understand their roles when the BC plans are invoked. The team will need to work together to do the right thing at the right time and to ensure that the right people are in place with the right support. All practice staff must complete the annual NHS data security awareness level 1 training.
1.5.6 The recovery process after an incident is equally important to ensure that electronic patient records are kept up to date and lessons are learned on how the response to the incident was managed.
1.5.7 BC plans should be reviewed as required under the terms of the ICB practice agreement.
1.5.8 BC plans must always be reviewed following their invocation.
1.5.9 The review of BC plans will need to consider those circumstances where the practice may be unaffected but providers are. For example, the shutdown of a secondary care provider that supplies pathology services may delay the availability of test results or of discharge advice notes. While these may be beyond the scope of the practice, planning and agreement with the ICB on how to handle these circumstances will be of benefit to the practice and its patients.
1.5.10 Local (ICB) commissioned GP IT delivery partners (providers) are also contractually required to prepare and maintain BC and disaster recovery plans for those services relevant to the delivery of GP IT.
1.6 Locally procured third-party digital systems, services and IT architecture
1.6.1 Consideration needs to be given to cyber security, data protection and clinical safety arrangements for any locally procured digital system, service or architecture which is provided by suppliers outside the DSIC framework, the local commissioned GP IT services and national digital services.
1.6.2 The responsible procuring authority – for example, the ICB or the practice – must ensure that any digital services and infrastructure procured locally which are provided by third-party suppliers are compliant with the applicable standards in the GP IT operating model. A standards checklist for local off-framework procurement is provided in the GP IT operating model.
1.6.3 Practices remain responsible for choice and funding of their practice telephony system but must ensure that any new contract or other arrangement relating to relevant telephony services is procured under the advanced telephony better purchasing framework. Useful guidance on using practice telephony to improve practice services is given in How to improve telephone journeys in general practice.
1.6.4 Clear support arrangements are essential and should describe how these align with local GP IT delivery arrangements. This is critical in effective incident management.
1.7 Sub-contractors, third parties and other premises
1.7.1 A practice may choose to commission services from a third party as a sub-contractor (subject to any provisions for sub-contracting of clinical services in the contract – see chapter 13: Sub-contracting of clinical services: assurance framework. The NHS obligations to provide digital services, as described in the contract, the ICB–practice agreement and the GP IT operating model do not automatically extend to providing these services to a third party.
1.7.2 Where the practice wishes a sub-contractor or other third parties to have access to the digital services available to the practice, it will follow the processes described in the ICB–practice agreement and the GP IT operating model.
1.7.3 The practice will make this request to the ICB and the ICB will consider the following:
- the organisational status of the sub-contractor and its relationship to the contractor
- assurance of the sub-contractor compliance to the standards and conditions required in the GP IT operating model by either:
- the sub-contractor having provided to the commissioner a signed letter using the template in appendix 5 of the ICB–practice agreement
- the sub-contractor is supplying services through a framework agreement which requires compliance with the standards and conditions required in the GP IT operating model
- whether the cost of providing the GP IT services to both the practice and the sub-contractor is proportionate to other similar practices supported (based on a cost per registered patient basis)
- whether the practice and the ICB comply with the conditions and liabilities described in the ICB–practice agreement
- any licensing conditions which prevent or limit access to certain GP digital services by other parties
- limitations on providing GP IT services to locations other than the practice premises
- the availability of NHS owned GP IT equipment
- use of NHS software/applications on non-NHS managed devices
1.7.4 When the ICB approves access to the services by a sub-contractor, appendix 1 of the ICB–practice agreement will be updated.
1.7.5 On-site services – for example, IT infrastructure, HSCN, WiFi, IT equipment, IT support – will be provided to the following locations:
- practices operating at the practice premises
- sub-contractor operating at practice premises providing the ICB has agreed the sub-contractor can access the services
- other premises listed in appendix 1 of the ICB–practice agreement
1.7.6 On-site services – for example, IT infrastructure, HSCN, WiFi, IT equipment, IT support – may, at the commissioner’s discretion, be provided to the following locations:
- practices delivering remote services from remote premises
- sub-contractor delivering remote services from remote premises providing the ICB has agreed the sub-contractor can access the services
1.7.7 Support for authorised users at personal domestic residences and mobile locations will be limited to the provision of remote access as described in the GP IT operating model.
1.8 Further information
Commissioners seeking further information on the GP IT operating model and associated support materials and guidance can visit the digital primary care section of the NHS England website or contact the NHS England Digital Primary Care (GP IT) team: england.digitalprimarycare@nhs.net
For further information about the DSP toolkit please visit DSP toolkit help section or contact cybersecurity@nhs.net
2. Protocol in respect of locum cover or GP performer payments for parental and sickness leave
2.1 Background
2.1.1 The General Medical Services Contracts Statement of Financial Entitlement (Amendment) Directions 2025 (SFE) sets out the provisions, conditions and payments relating to reimbursement to GP practices for GP performers covering parental leave and sickness leave.
2.1.2 This protocol applies only to GMS practices, but commissioners should ensure they treat PMS practices equitably.
2.1.3 For the purposes of this protocol:
- ‘parental leave’ means ordinary or additional maternity leave, neonatal leave, paternity leave, ordinary or additional adoption leave or shared parental leave. Note: subject to SFE amendment directions in July 2025, neonatal leave will be eligible for locum reimbursement with backdated effect to 6 April 2025
- ‘full-time’ means 9 sessions of clinical work per working week
- ‘working week’ is defined as the core hours set out in the National Health Service (GMS contracts) Regulations: “the period beginning at 8:00 am and ending at 6.30 pm on any day from Monday to Friday except Good Friday, Christmas Day or bank holidays”
2.1.4 The commissioner will not make payments in respect of locum or GP performer cover outside of core hours.
2.1.5 This protocol applies to GPs funded via the Additional Roles Reimbursement Scheme (ARRS) who are employed by a PCN member practice. The cover arrangements for ARRS funded GPs who are employed by a third-party organisation are set out in annex E of the Network Contract DES specification (subject to updated 2025/26 Network Contract DES specification)
2.2 Parental and sickness leave payments
2.2.1 Providing the relevant provisions of the SFE are met, GP practices are entitled to claim reimbursement of the cost for providing GP performer cover when a GP performer is on parental leave or on sickness leave.
2.2.2 The reimbursement of costs can be claimed where the cover is provided by:
- a locum
- a salaried GP on a fixed-term contract
- a GP already working in the practice but who is not full-time (either employed or a partner)
2.2.3 Payments will not be made on a pro-rata basis having regard to the absent performer’s working pattern and will be the lower of actual invoiced costs or maximum amount.
The SFE sets out the maximum amount of reimbursement for a GP performer providing cover as follows:
2.3 Parental leave
2.3.1 In respect of maternity leave or adoption leave where the GP performer going on leave is the main care provider, or shared parental leave, the maximum amount payable is £1,475.17 per week for each of the first 2 weeks and then £2,238.03 per week for each of weeks 3 to 26. In the case of neonatal leave, where the GP performer going on leave is the main care provider, or shared neonatal leave, the maximum amount payable is £1,475.17 per week for each of the first 2 weeks and then £2,238.03 per week for each of weeks 3 to 12.
2.3.2 Commissioners should reimburse shared parental leave in the same way as maternity leave. It will be for the practice to demonstrate that a GP performer is eligible for shared parental leave either under statute (for salaried GPs) or under the terms of a partnership agreement. See annex 88: sample declaration of eligibility and information on eligibility for shared parental leave.
2.3.3 In respect of paternity leave where the GP performer going on leave is not the main care provider or special leave (which is equivalent to the terms and duration of paternity leave: for example, bereavement leave), the maximum amount payable is £1,475.17 per week for each of the first 2 weeks.
2.4 Sickness leave
2.4.1 In respect of sickness leave, for each period of sickness leave there is a qualifying period of 2 weeks during which time no payments are made.
2.4.2 After 2 weeks, payments start and the maximum amount payable is £2,238.03 per week for each of weeks 3 to 28. Thereafter, the maximum amount payable is £1,119.02 per week for each of weeks 29 to 54.
2.4.3 As set out in the SFE, for weeks 29 to 54 the commissioner will pay half of whatever it determined was payable for weeks 3 to 28. The SFE also sets out a methodology for calculating these periods with respect to any payments made in the previous 52 weeks and that methodology continues to apply.
2.5 Sickness leave and phased return to work.
2.5.1 Commissioners support the safe return to work of GP performers and recognise that GP practices exercise flexibility in managing sickness absence (where GP performers under a fit note are declared they may be fit to work, subject to advice and agreement on phased return or adjusted hours). The fit note in such cases is continuing to declare sickness absence for the period, subject to and excluding any agreed working arrangements. For example, if a GP performer is advised they may be fit to work 2 days out of 5 for 2 weeks, then the other 3 days in each week for that period remain as sickness absence.
2.5.2 Payment in respect of necessary cover for this sickness absence under a fit note advising phased return or adjusted hours may however be mandatory or discretionary, subject to the requirements of the SFE being met.
2.5.3 In respect of a GP performer who is a partner, the SFE makes no distinction on sickness leave, meaning paragraph 10.3 of the SFE applies whether a GP partner is under a fit note declaring they are unfit to work or may be fit to work subject to advice given on phased return or adjusted hours. Mandatory provision for payment therefore applies and commissioners should continue to reimburse locum cover costs as per 2.4 above.
2.5.4 In respect of a GP performer who is an employee, the SFE applies a further requirement at paragraph 10.3 to qualify for payment – which is that the contractor is required to pay the GP performer statutory sick pay (SSP) or their full salary during sickness leave under their contract of employment.
2.5.5 A phased return or adjusted hours arrangement may interfere with a contractor meeting these requirements – SSP is subject to forming a period of incapacity to work of 4 consecutive days. Where these requirements are not met, payment to reimburse any locum cover costs would be discretionary (see section 2.8: Discretionary payments in respect of cover for employed GP performers on phased return or adjusted hours arrangement following sickness absence).
2.5.6 Where these requirements continue to be met under a phased or adjusted hours arrangement, commissioners should continue to reimburse locum cover costs as per section 2.4: sickness leave.
2.6 Further discretionary payments
2.6.1 This protocol details (as required under part 7, paragraph 22 of the SFE) a number of policies the commissioner is obliged to set out:
- how the commissioner is likely to exercise its discretionary powers to make payments (including top-up payments) in respect of locum cover for parental or sickness leave where it is not obliged to make such payments
- where the commissioner is obliged to make payments in respect of cover for parental or sickness leave pursuant to part 4 of the SFE, the circumstances in which it is likely to make payments of less than the maximum amount payable
- how the commissioner is likely to exercise its discretionary powers to make payments in respect of cover for absent GP performers, which is provided by nurses or other healthcare professionals
- how the commissioner is likely to exercise its discretionary powers to make payments to a partner or employee who is providing locum cover
- how the commissioner is likely to use its discretionary powers to make payments in respect of long-term sickness leave exceeding 52 weeks
- how the commissioner is likely to exercise its discretionary powers to make payments in respect of a sole practitioner who is absent for the purposes of attending an accredited postgraduate educational course
2.7 Discretionary powers in respect of cover for parental and sickness leave
2.7.1 The commissioner has the discretion to make payments in circumstances where it is not obliged to under the terms of the SFE, including top-up payments above the level of the agreed weekly maximum.
2.7.2 The commissioner may exercise these discretionary powers to make payments only in exceptional circumstances: for example (but not limited to), consideration of:
- demonstrable financial hardship
- areas of significant deprivation
- GP recruitment difficulties
- applications from single-handed GPs
- applications from nurse-led PMS practices
2.7.3 Where practices plan to apply for reimbursement in such circumstances, they should always ensure they have written agreement from the commissioner prior to arranging cover.
2.8 Discretionary payments in respect of cover for employed GP performers on phased return or adjusted hours arrangement following sickness absence
2.8.1 The commissioner has the discretion to make payments where employed GP performers are returning to work under a phased return or adjusted hours arrangement following sickness absence.
2.8.2 The commissioner will make payments in the following circumstances:
- where the employed GP performer’s phased return or adjusted hours arrangement directly follows sickness absence leave which attracted a locum payment under section 10 of the SFE
- where the phased return or adjusted hours arrangement has been advised under a fit note (and for the period only that fit note covers or advises)
- where the contractor is paying the employed GP performer their full salary in respect of their phased return or adjusted hours arrangement; that is, taking account of both working and sickness absence days/sessions
2.8.3 In these circumstances the commissioner will pay the lower of actual invoiced costs or maximum amounts payable calculated in line with 4.2.
2.9 Circumstances where it is likely payments will be less than the maximum amount payable
The commissioner will pay the maximum amount payable except in the following circumstances:
- where actual invoiced costs are less than the maximum amount payable, then the commissioner will pay the actual invoiced costs subject to the provisions of this protocol including the bullet point below:
- with respect to parental leave, where the commissioner agrees to make payments for any week between weeks 27 to 52 for cover for additional maternity leave or adoption leave, the commissioner will pay the lower of either 50% of the weekly rate it paid for weeks 3 to 26 or 50% of the actual invoiced costs
2.10 Payments for locum cover provided by nurses or other healthcare professionals
2.10.1 The commissioner will not pay for cover provided by nurses or other healthcare professionals.
2.11 Payments to a partner or employee who is providing cover
2.11.1 Where a contractor wishes to engage the services of a partner or shareholder in, or an employee of, that contractor, payments will be made to the GP practice in accordance with the normal provisions set out above. However, the GP performer providing cover would only be permitted to work up to the full-time limit of 9 clinical sessions per working week. The maximum of 9 clinical sessions per working week is to include any existing/normal commitments by the GP performer providing the cover.
2.12 Discretionary payments in respect of long-term sickness leave exceeding 52 weeks
2.12.1 Where a GP performer is on long-term sickness leave and locum payments are no longer payable under section 10 of the SFE, it will be at the commissioner’s discretion whether to continue to make payments.
2.12.2 In any case, those payments will not exceed the half rate payable in the second period of 26 weeks under paragraph 10.7(b) of the SFE or the amount that would be payable under the NHS Pension Scheme regulations if the performer retired on grounds of permanent incapacity, whichever is the lower.
2.13 Discretionary payments in response of sole practitioners who are absent for the purposes of attending an accredited postgraduate educational course
2.13.1 The commissioner will not pay for locum cover in respect of a sole practitioner’s attendance at an accredited postgraduate educational course.
2.14 Claims and payments
2.14.1 For parental leave, payments start from the day the GP performer goes on parental leave for the periods set out above and payment weeks are 5 working days.
2.14.2 For sickness leave, payments start 2 weeks from the day the GP performer goes on sick leave for the periods set out above and payment weeks are also 5 working days.
2.14.3 Annex 86 provides a sample claim form and frequently asked questions are available at annex 87.
3. Guidance note: GP practices serving atypical populations
3.1 General
3.1.1 The GMS funding formula (Carr-Hill formula) is an attempt to fund practice workload regardless of the population they serve.
3.1.2 It is recognised that there are some practice populations that are so significantly atypical that using the GMS funding formula would not support or ensure the delivery of an adequate general practice service.
3.1.3 NHS England guidance has looked at 3 such atypical populations – unavoidably small and isolated, university practices and those with a high ratio of patients who do not speak English – and encourages commissioners to review the support needs of identified atypical practices in their area.
3.1.4 Support for atypical practices should directly impact on patient care as well as the long-term viability of practices. Without such support, identified atypical practices may be unable to maintain an adequate service and as a result health outcomes may suffer.
3.1.5 Please refer to the guidance on GP practices serving atypical populations.
4. Provision of occupation health services
4.1 Introduction
4.1.1 Occupational health (OH) is “a specialist branch of medicine focusing on the health of staff in the workplace. OH professionals aim to find out what impact work has on staff health and make sure that staff are fit to undertake the role they are employed to do both physically and emotionally. OH specialists can support organisations through advising on work-related illnesses and accidents, carrying out assessments for new starters and existing employees, monitoring the health of employees and prevention. OH services are also used to assist organisations in managing both short and long-term absence situations”. (NHS Employers).
4.1.2 “Employers are required by law to prevent physical and mental ill health in their workers that may occur as a result their business activities. An important part of occupational health is concerned with how work and the work environment can impact on workers’ health, both physical and mental. It also includes how workers’ health can affect their ability to do their job. In health and safety law, there are things organisations must do to make sure workers’ health is not adversely affected by their work and that workers are medically fit to carry out their work safely. This includes:
- implementing health or medical surveillance when necessary, ensuring workers are medically fit to undertake the role required (your industry may produce such standards)
- reviewing your risk assessment when a worker is returning to work following sickness absence or declares a health condition
- have a responsibility to make available occupational health services for their staff and it is important that staff know how to access their service provider”. (Health and Safety Executive)
4.2 Provision of occupation health services – services funded by the primary care contractor
4.2.1 This section outlines what primary care services contract holders are responsible for funding as part of their employer responsibilities to their staff. These services include:
- OH pre-employment screening/clearance: OH assessments as required for all staff working in their organisation, as required
- virology testing, vaccination for bloodborne viruses (BBVs) and immunisation: available to all staff who are not already immunised and includes hepatitis B, varicella, tuberculosis (BCG), diphtheria, pertussis and tetanus, measles mumps and rubella
- enhanced/other OH assessments: these may include a range of different OH assessments or support needed for all staff including:
- assist in the appropriate placement of people at work, considering their physical and mental health, and prevent ill health arising as a result of work done or the conditions in which work is done
- enhancing staff performance and morale through reducing risks at work which lead to ill health, staff absence and accidents
- protect the public from any adverse consequences arising as a result of ill health or infected primary care staff
- review prolonged/recurrent sickness absence and support return to work after sickness absence or following an accident
- advice on ill health retirement
- periodic health assessment: for example, radiation, COSHH regulations or where risk assessment has indicated that this is required
- advice on onward referral to other services that could support staff: for example, counselling
4.3 Provision of specific occupational health services – applicants to join the national performers list
Performers seeking to apply to join the national performers list (NPL) will need to self-fund for the following OH services:
- pre-employment screening
- virology testing
- vaccination for BBVs
- immunisation
4.4 Provision of specific occupational health services – funded by the commissioner
4.4.1 For all primary care staff (general practice, community pharmacy, dentistry and optometry) – management of staff on exposure to and working with BBVs: this includes specialist support for the management of staff who have a BBV, and urgent and longer-term advice to all staff working in primary care settings (including trainees) on exposure to potential BBV: for example, following needle stick injury. Post exposure risk assessments, blood testing and post-exposure prophylaxis (PEP) treatments are included. Mainstream NHS services are responsible for ongoing treatment if BBV is contracted: for example, anti-retroviral medication.
4.4.2 For performers already on the NPL – OH services funded by the commissioner include: virology testing, vaccination for BBVs and immunisation.
4.4.3 For performers who are under review or investigation by responsible officer/medical director: any OH referrals made by responsible officer/medical director in respect of formal proceeding as part of the national performers list.
Summary of ‘who pays’ for what occupational health services
Management of staff on exposure to and working with bloodborne viruses | Virology testing, vaccination for bloodborne virus (BBV) and immunisations | OH pre-employment screening/ | Enhanced/other OH assessments | |
|---|---|---|---|---|
|
Commissioner pays for |
All staff working in primary care |
All performers registered on NPL |
Nothing |
Referrals related to NPL investigations |
|
Primary care organisation pays for: |
Nothing |
All (other) staff working for their organisation |
All staff joining their organisation |
All staff working for their organisation |
|
Performer (NPL) pays for: |
Nothing |
As required for their NPL application |
As required for their NPL application |
If not affiliated with organisation: for example, locums |
4.5 Role of the commissioner in enabling occupational health access for primary care workforce
Joint approach to procuring OH services
4.5.1 Although the different OH provisions are a shared responsibility – that is, commissioners fund part and primary care organisations fund part – commissioners should take steps to support primary care staff to access OH services in a consistent and efficient way.
4.5.2 Commissioners are much better placed to procure system-wide OH services on behalf of primary care organisations and should enable this by procuring OH service providers for all OH requirements set out above, with the option for primary care organisations to access these OH services on a fee basis for services they are responsible for funding.
4.5.3 It is strongly advised that commissioners collaborate with other primary care commissioners (that is, general practice, community pharmacy, dentistry and optometry) and local NHS organisations/ICB to ensure a cross-system sustainable and consistent access to OH services.
4.5.4 We have previously published a service specification for OH in primary care; we are currently reviewing this to better align to the work of the NHS People Plan and system transformation.
4.6 Good communications are essential
4.6.1 Commissioners must ensure information about how to access OH services is clearly communicated to primary care organisations and their staff. Many believe OH services are not available in primary care, which is not true. We must therefore do more to promote available OH services. As a minimum communications should clearly present information as set out below, but practices should work with their OH supplier on promotional materials and posters as required.
| Service Type | Description | Contact Information |
|---|---|---|
| Urgent Occupational Health Services | Management of staff on exposure to and working with blood borne viruses e.g., needle stick injury | Working hours: (contact phone numbers/instructions) Out of hours: (add phone number/instructions) |
| Routine Occupational Health Services | Virology testing, vaccination for Blood Borne Virus and immunisation OH pre-employment screening/clearance Enhanced/OH assessments | OH provider: (supplier name) supplier phone number Website: (for more info on offer/prices) Email: [email address] |
5. Provision of clinical waste services
5.1 Introduction
5.1.1 Under the Delegation of primary medical, pharmaceutical, ophthalmic and dental functions agreement Schedule 2A, Section 18 (Commissioning ancillary support services), ICBs must procure and undertake the management and monitoring of contracts for collection and disposal of clinical waste.
5.1.2 This section offers commissioners guidance and support on what this includes and relevant duties which they or their GP contractors must fulfil.
5.2 Why is this a commissioner responsibility?
5.2.1 Waste and environment regulations are clear that the waste producer is legally responsible for all aspects of on-site management, collection and disposal (whether internal or through third parties) of all waste it generates. Therefore, the general practice is legally responsible, not the commissioner.
5.2.2 However, under paragraph 47 “Payments in respect of running costs” of The National Health Service (General Medical Services Premises Costs) Directions 2024 general practices can apply to commissioners for financial assistance for costs which are or relate to the collection and disposal of clinical waste. The commissioners must consider that application and, in appropriate cases (having regard, among other matters, to the budgetary targets it has set for itself), grant that application. This in effect makes this a funding responsibility for commissioners.
5.2.3 While practices may lead the management and monitoring of contracts for collection and disposal of clinical waste (and seek re-imbursement of costs), the delegation agreement instructs commissioners to take on this responsibility to improve cost management of waste services, improve consistency of waste services performance and reduce burden on individual practices managing these complex markets.
5.2.4 In the majority of cases commissioners now commission clinical waste services on behalf of general practices (with the exception of property services companies and a handful of individual practices) and commissioners are encouraged to continue to consolidate these exceptions into their waste services contracts where possible.
5.2.5 What is the commissioner actually responsible for?
On behalf of general practices as the waste producers, commissioners must:
- procure, and undertake the management and monitoring of contracts for collection and disposal of clinical waste
- have good working knowledge of the Health Technical Memorandum (HTM) 07-01: Safe and sustainable management of healthcare waste and ensure all applicable duties are met by the waste producer or commissioner on the waste producer’s behalf
- have regard to the NHS clinical waste strategy in respect of how it approaches its responsibilities and ensures that its waste producers (general practices) are practising compliant and sustainable waste management
5.2.6 Commissioners may appoint a third-party specialist organisation (also referred to as a waste management agent) to fulfil the above duties on behalf of the commissioner and its waste producers.
5.3 Types of waste the commissioner is responsible for funding
5.3.1 The definition of clinical waste is set out in the Health Technical Memorandum (HTM) 07-01: Safe and sustainable management of healthcare waste, but this can be confusing when getting into the specific categorisation of different types of healthcare waste (for example, understanding from a regulatory perspective what is and is not technically clinical waste).
5.3.2 For the purpose of this guidance and clarifying what commissioners are responsible for funding, reference to clinical waste typically refers to the following waste streams (generated in the general practice setting):
- infectious waste (orange bags)
- medicinal/pharmaceutical or chemical contaminated waste (yellow bags)
- cytotoxic or cytostatic waste (purple lidded containers)
- sharps waste (yellow or orange lidded containers)
- offensive waste (tiger striped bags)
- medicine returns/expired waste (blue lidded container)
- anatomical waste (red bags/containers)
and anything else the commissioner considers reasonably applicable in parallel to the above
5.3.3 Waste streams not considered in scope of clinical waste and it is not the responsibility of commissioners to manage or re-imburse costs for:
- general/domestic/commercial wastego
- recycling waste
- confidential waste
- food waste
5.4 What about clinical waste generated in the community / patients own home?
5.4.1 There is often conflict between what the regulations say, resulting in a significant variation in how this clinical waste is managed across different areas across England.
5.4.2 In simple terms, the following apply:
5.4.2.1 Where clinicians (usually employed or affiliated with general practices) attend a patient’s home to administer treatment, any clinical waste generated should be returned to the general practice. In some cases, clinical waste may be collected from the patient’s homes (so long as the patient agrees and the commissioner on the waste producer’s behalf arranges collection of any clinical waste left on site).
5.4.2.2 Where a patient generates the clinical waste themselves through self-administration of treatments, then local authorities are responsible for appointing and funding the collection and disposal of clinical waste produced in a household, as set out in the Environmental Protection Act 1990, s45(1) and The Controlled Waste (England and Wales) Regulations 2012, Regulation 4 and Schedule 1, paragraph 3, item 12.
5.4.2.3 In some cases, local authorities may not have any processes in place for collection and disposal of clinical waste generated in a home setting. Therefore, commissioners may wish to work with their local authorities to try and improve this experience for their patients, for example:
- allowing NHS commissioned clinical waste services to collect waste from patients’ homes, subject to reimbursement by the local authority
- allowing patients to take home generated clinical waste to primary care sites (as permitted under Waste exemption: NWFD 4 temporary storage at a collection point), subject to agreement of primary care sites accepting this waste and reimbursement by the local authority.

