Publication reference: B1569
Summary
The purpose of the social prescribing link worker (SPLW) workforce development framework is to:
- Provide clear and consistent standards for SPLW practice, including their knowledge, skills and behaviours
- Provide guidance on the support, supervision, and learning and development offer required from employers to support SPLWs
- Promote the development of a strong and capable workforce of SPLWs and their future development
- Support improved quality and consistency of social prescribing and reduced variation in outcome and access standards.
- Demonstrate the benefits of SPLWs working as part of a multidisciplinary team (MDT).
The framework includes core competencies for the role and links to resources to support employers to recruit and embed SPLWs in services. Organisations employing SPLWs, including primary care networks (PCNs), can use this framework to support recruitment and retention. It will help them develop a greater understanding of the role, its scope of practice and the training and development SPLWs need to enable them to practice safely and effectively.
SPLWs give people time over several sessions to offer a person-centred conversation based around asking, “what matters to you?”. They work with people to connect them with community-based services, groups and activities that meet practical, social, and emotional needs that affect their health and wellbeing.
SPLWs may be employed by PCNs, or by a host organisation that provides social prescribing services, such as local voluntary, community and social enterprise sector organisations (VCSE) that have existing links and relationships within communities.
As with any role in a health, care or community setting, SPLWs need to be supported and enabled to succeed in their role. Before employing a SPLW, employers should be clear on the purpose of the role and how it can contribute to meeting people’s needs and neighbourhood/place/system priorities, and that they have the capacity to manage and support the roles.
SPLWs will be recruited with relevant skills and experience, and they will complete the Link Worker Learning e-learning programme and other initial training as set out by the Personalised Care Institute (PCI). Employers are responsible for funding any necessary training, and for ensuring the SPLW workplan includes time for training and for community outreach activities, reporting, case work and research, as well as face to face client work.
Good supervision arrangements for SPLWs are crucial to ensure they practice safely and effectively. SPLWs should have an initial point of contact within a PCN, a GP supervisor, and monthly clinical supervision with a relevant professional, to manage any emotional issues and to develop their SPLW practice. They may also have a day to day line manager. Supervisors should have relevant experience of the SPLW role, and be supported in their own development as supervisors.
SPLWs manage their own caseload. The maximum safe caseload is 200-250 per year and may be less, based on the complexity of cases and the maturity of the social prescribing service. Workloads should be set based on this maximum rather than other targets.
Employers should support SPLWs in their continuous professional development (CPD), giving them dedicated time, and where necessary funding, for training and CPD. Regular supervision sessions, appraisals and personal development planning should all be used as opportunities to focus on specific needs to progress and/or meet the competencies for the role, as well as future career aspirations. SPLWs themselves, their supervisors and employers have collective responsibility for CPD.
Personalised care is uniquely placed to help tackle growing health and wellbeing needs, including complex or multiple long-term conditions and unmet health needs. SPLWs play a key role in empowering individuals and communities to improve health and wellbeing, and social prescribing is an important part of tackling health inequalities and responding to issues caused by the social determinants of health.
1. Introduction
The workforce development framework for social prescribing link workers (SPLWs) has been developed to support SPLWs and their employers to maximise impact of the role.
Organisations employing SPLWs, including primary care networks (PCNs), can use this framework to support recruitment and retention. It will help them develop a greater understanding of the role, its scope of practice and the training and development SPLWs need to enable them to practice safely and effectively.
It is intended as a useful resource for organisations across the health and care sector including the NHS, voluntary, community and social enterprise (VCSE) partners, and local authorities. The framework also includes specific information for PCN SPLWs that are funded through the Additional Roles Reimbursement Scheme (ARRS).
The framework has been developed by NHS England in collaboration with range of stakeholders (full list at item 13).
It focuses on the core functions, skills and competencies of the SPLW role, alongside the professional support and development SPLWs need to enable them to practice safely, work effectively, and support improved outcomes for people and communities. The framework purpose is to:
- Provide clear and consistent standards for SPLW practice, including their knowledge, skills and behaviours
- Provide information about the training, support, supervision and continuous professional development (CPD) needed to enable them to succeed. Provide guidance on the support, supervision, and learning and development offer required from employers to support SPLWs
- Promote the development of a strong and capable workforce of SPLWs and their future development
- Support improved quality and consistency of social prescribing and reduced variation in outcome and access standards
- Demonstrate the benefits of SPLWs working as part of a multidisciplinary team (MDT).
This document brings together, simplifies and clarifies key information about employing, supporting and getting the best out of social prescribing link work.
2. Context
Social prescribing and community-based support is part of the NHS Long Term Plan commitment to make personalised care business as usual across the health and care system.
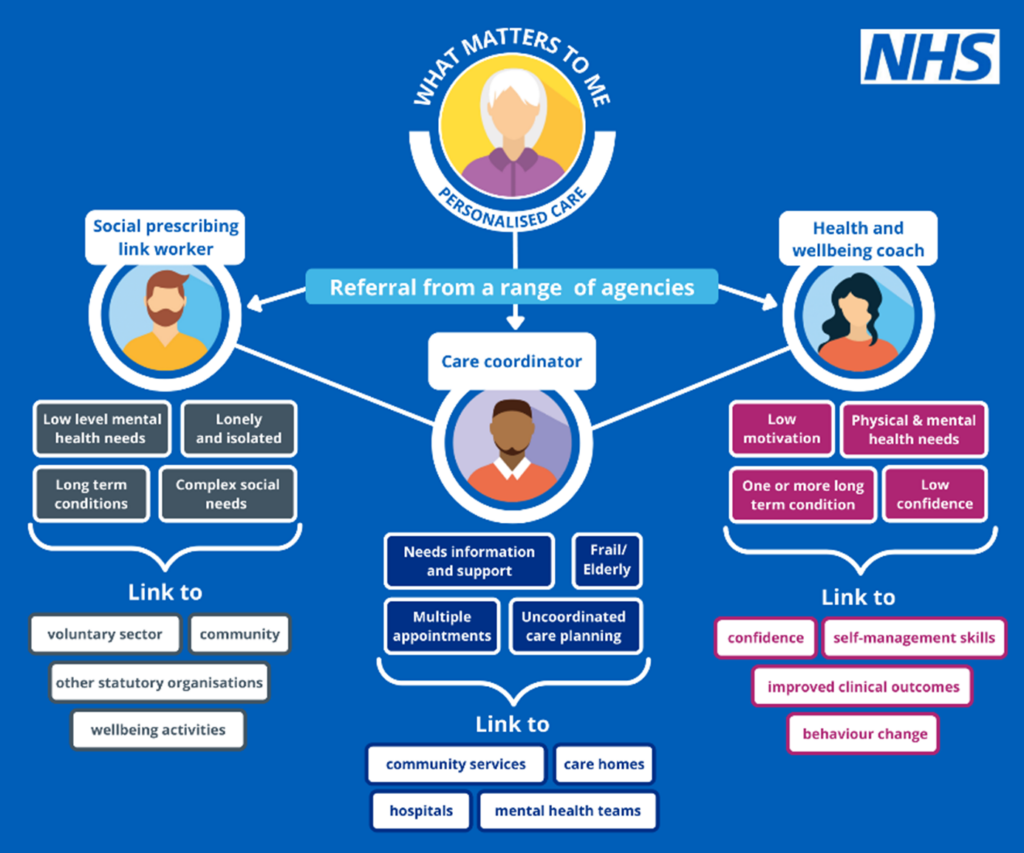
SPLWs, along with health and wellbeing coaches and care coordinators are dedicated, to providing personalised care. SPLWs are important members of a PCN’s MDT and wider multi-agency integrated teams. They work in partnership with other personalised care roles and health and care professionals to optimise health outcomes for people and populations, and reduce health inequalities. They can also contribute to community outcomes, including strengthening resilience and building connections and empowering community action (Marmot, 2018).
The SPLW workforce development framework has been created alongside similar frameworks for health and wellbeing coaches and care coordinators.
3. What is a social prescribing link worker?
People’s physical and mental health and wellbeing is influenced by a range of factors, including their housing, finances, personal relationships, and existing health conditions. Not all the factors that affect health and wellbeing can be resolved through conventional health services, and up to 20% of people who go to see their GP present with an issue that is primarily a social problem (University of Westminster, 2017).
Social prescribing is a way to connect people with community-based services, groups and activities that meet practical, social, and emotional needs that affect their health and wellbeing, and increase people’s active involvement with their health and their community. Social prescribing works for a wide range of people, particularly those with one or more long-term conditions, people who need support with their mental health, people who are lonely or isolated and those with complex social needs.
3.1 Role of a social prescribing link worker
SPLWs give people time over several sessions to offer a person-centred conversation based around asking, “what matters to you?” They:
- Are part of an all-age, whole population social prescribing approach and work with people who are lonely, have complex social needs, low level mental health needs and long-term conditions
- Help people to identify issues that affect their health and wellbeing, and co-produce a simple personalised care and support plan
- Support people by connecting them to non-medical community-based activities, groups and services that meet practical, social and emotional needs, including specialist advice services and the arts, physical activity, and nature
- Use coaching and motivational interviewing techniques to support people to take control of their own health and wellbeing
- Support accessible and sustainable community offers by working with VCSE organisations, local authorities and others to identify gaps in provision and deliver activities and groups to meet population needs.
SPLWs provide support to tackle issues caused by the wider determinants of health, alongside colleagues providing conventional medical interventions. SPLWs and their PCN work in partnership with local agencies to proactively reach out to populations who might benefit from social prescribing, taking a preventative approach. People can be referred to SPLWs from a wide range of local agencies including NHS services, local authority services, pharmacies, emergency services, job centres, housing associates, VCSE organisations and self-referral.
4. Employing social prescribing link workers
4.1 Employment
PCNs may directly employ SPLWs or sub-contract provision of the service to another provider in accordance with the Network Contract Directed Enhanced Service (DES) contract specification.
SPLWs employed by VCSE host organisations are well-connected to wider agencies that support health and wellbeing, including statutory services, VCSE-led activities and groups, and hyper-local support offerings and opportunities such as volunteering.
While primary care staff are not on the NHS Agenda for Change pay scale, the SPLW role in PCNs is designed to be equivalent to NHS Agenda for Change Band 5 in terms of responsibilities and remuneration. This reflects the complexity of the situations people present with, the level of autonomy SPLWs work with, and the need for a significant level of multi-agency working, including supporting community groups to receive referrals.
PCNs are responsible for ensuring SPLWs are included in the PCN wider team and are supported appropriately within surgeries. Where SPLWs are employed by a host organisation, this will involve working together on supporting SPLWs.
Considerations for setting up a social prescribing service are set out in the Reference guide for primary care networks reference guide for social prescribing and includes a checklist, social prescribing planning, recruitment support including a sample job description and advert, and an induction checklist.
Employers should be confident that they have the necessary resources and support in place to embed the SPLW in the team. This includes having appropriate supervision arrangements in place, which is essential, and provision for training and ongoing CPD.
4.2 Caseload
SPLWs tend to support people for an average of 6-12 contacts over a three-month period, but this will be flexible, depending on the support the person needs. A full time SPLW can have a typical annual caseload of up to a maximum of 200-250. This may be lower depending on the complexity of peoples’ needs, the maturity of the social prescribing scheme and wider work they may be undertaking, such as community development activities or outreach.
Other case number targets, such as the Investment and Impact Fund (IIF) should be viewed in the context of this maximum caseload per SPLW, and staffing levels set accordingly.
SPLWs should manage their own caseload to work with people in a format that works for them, including face to face appointments, home visits and community-based activity.
5. Training and development in post
Investing in learning and development is one way that employers can support the delivery of excellent healthcare and health improvement, along with quality supervision and management support. It helps ensure that the workforce has the right skills, knowledge and behaviours to do their role effectively.
SPLWs should receive accredited training and on-going development to support their role. It is the responsibility of the employer to ensure that SPLWs have the appropriate level of training, and/or to support their training needs by funding and allowing time to attend training.
In primary care, while the ARRS funds relate to the salary costs of the SPLW (and a contribution to hosting costs, where SPLWs are employed by a VCSE organisation), there are a range of other funding streams already available to PCNs and to Systems for the development and management of PCNs and their workforce, including SPLW, employed through the ARRS.
As the background skills and experience of SPLWs will be varied, the training or development needs at each stage of employment as a SPLW needs to be led by the individual’s needs, based on a joint understanding by their supervisor and the staff member, and knowledge of the needs of the local community. The Portfolio of Evidence template tools at Annex B, will help with this understanding, and section 6 on supervision sets out expectations around the supervisory relationship, with recommendations on supervisor skills and training resources in Annex C.
The broad phases we have set out below are a general guide, and decisions need to be made by the employer about readiness to work independently, and with the SPLW about individual training and development needs.
While all SPLWs will go through the first two phases, it is not necessarily expected that they will move on to specialise or become managers, as this will depend on individual career aspirations (see Career pathways).
5.1 New SPLWs
Before SPLWs can work independently with people, they should complete an induction and onboarding and training process. This will ensure that SPLWs understand their role, have basic skills to start working with people, and can keep themselves and the people they work with safe. It will also help SPLWs to prepare for the challenges of the role and identify their base skills, knowledge and competencies.
5.1.1 Induction
PCNs as employers will want to ensure that all staff are valued and are treated with dignity and respect. Local induction is necessary for onboarding of new SPLWs, and this should promote good working relationships within the PCN, and with other areas of the NHS and external agencies, to help SPLWs feel supported and valued at work. Local induction should also include information for the wider workforce about the SPLW role and appropriate referrals and allow SPLWs to work as part of the MDT effectively.
Employers may wish to include shadowing colleagues, being observed and receiving feedback, and establishing peer support relationships with other SPLWs as part of the onboarding process. It may also be helpful to establish reflective practice at the outset, and employers should think about the learning environment for SPLWs, as with all staff.
Sole SPLWs working in PCNs may need additional support during induction to establish peer support relationships across organisational boundaries. Employers are encouraged to support SPLWs to connect with regional networks and to provide protected time to attend peer support sessions.
The Primary care reference network guide and technical annex includes an induction checklist.
5.1.2 Initial training
In line with the Network Contract DES, SPLWs employed in or by primary care networks (PCNs) must:
- Complete the mandatory HEE e-learning programme, found at: HEE e-learning for healthcare
- Enrol in, undertake or qualify from appropriate training as defined by the Personalised Care Institute (PCI)
- Attend the peer support networks delivered at place or system by the integrated care system (ICS) and/or NHS England in the region.
The e-learning programme provides a brief overview of the role, expectations, evidencing impact, and a range of population- or issue-specific modules. The PCI set out further initial training expectations for SPLWs including core skills modules and personalised care and support planning, which will allow SPLWs to understand working in a personalised way.
Health Education England regional training hubs provide information about primary care workforce, education and development based on local needs. They bring together education and training resources from a range of providers. They support every practice and PCN with access to information, resources, apps and contacts as well as national and local networks that can offer practical guidance, support and advice.
All new staff will do their mandatory and statutory training including safeguarding and data protection. This is a good time to introduce new team members to outcomes measurement tools used and ensure familiarity with case management systems and any reporting needed.
For information about these, contact your ICS.
5.2 Continuing professional development
Following induction SPLWs will begin working independently, using and developing the skills, knowledge and behaviours in the Competency Framework (Annex A) to support clients.
SPLWs and supervisors are expected to work together to undertake continuing personal and professional development, taking an active part in reviewing and developing their roles and responsibilities.
Professional development planning takes place through clinical supervision, using experiential learning and workplace feedback as opportunities to engage in reflective practice, and to provide feedback to the SPLW. It is a key part of ensuring patient safety and positive outcomes. SPLWs should be offered supervision on a frequent basis and at least monthly. Supervision expectations are set out in section 6 and supervisor standards in Annex C.
We recommend using the Competency Framework (Annex A) and Portfolio of Evidence (Annex B) to provide structure for conversations about CPD during supervision sessions.
CPD can be undertaken through a range of methods, including through formal or accredited training, but also as part of the PCN or host organisation learning environment. For example, shadowing with colleagues, reflective practice, group supervision or case discussions, pair reflection sessions, community-based projects, independent reading and research are all valid forms of CPD. SPLWs need appropriate protected time in their work schedule for CPD in any format.
A wide range of other training is available for SPLWs. For example, many local authorities provide training for community and care workers that may be appropriate for SPLWs. This will also provide learning in a local context and allow for relationship building with colleagues in other sectors.
National learning offers are outlined in the resources section.
6. Supervision
Supervision is a process by which individual SPLWs work with another person to meet their professional, organisational and personal objectives, which together promote best outcomes for the patient.
Supervision covers the various types of support a SPLW will need to practise safely and effectively. It includes day-to-day management and clinical and professional expertise. Supervisors should have a good understanding of the level of skills and competencies a SPLW has, where they are now, and what they need to do to progress. They are enablers that support good working relationships and help to address issues and celebrate achievements. They encourage reflection and ongoing development and improvement.
Health and care providers regulated by the Care Quality Commission (CQC) are expected to offer staff regular supervision to ensure staff are competent and confident to do their role.
SPLWs starting in their role will already bring knowledge and skills, and will continue to develop these through formal learning and CPD after identifying training and development needs through supervision. They will also gain support from their peers through formal and informal peer support networks, and from the wider team within the practice, PCN, wider NHS, host organisation or other organisations.
Across England, SPLWs are employed by a variety of different host organisations:
- VCSE organisations including faith organisations
- Local authorities (LA)
- Clinical commissioning groups (CCG)
- PCNs
- Other organisations, such as hospitals and agencies supporting discharge from hospital
All SPLWs will need supervision, which should be provided by their employer. Regardless of which host organisation employs the SPLW, if the role is funded through the Network Contract DES the PCN’s contractual obligations regarding supervision are the same, and are set out below. However, in practice, SPLWs may be supported by a number of people depending on who the host organisation is.
6.1 Supervision of SPLWs in primary care networks
The Network Contract DES (Section B3.4 2022/32) requirements on supervision are in the boxes below, accompanied by advice for implementation.
6.1.1 First point of contact in each GP practice
The role of the first point of contact will be to enable the SPLW to develop effective working arrangements with all staff within the member practices and to ensure that all staff can support the SPLW role. This role could become a designated ‘social prescribing champion’ within each member practice.
6.1.2 GP supervisor
SPLWs may also have a non-GP supervisor to line manage their work on a day to day basis.
The supervisor(s) should meet regularly with the SPLW to provide line management and supervision, discuss address any issues or concerns and ensure the SPLW can succeed in the role. This will include patient-related concerns, for example, abuse, domestic violence, or other safeguarding issues, and refer individuals back to other health professionals as relevant, for further support, review or monitoring.
Where the SPLW is employed by a host organisation, the GP supervisor is still required. In this arrangement, the GP supervisor may find it helpful to involve the partner organisation in regular progress updates about the SPLW role, to enable clear lines of accountability, seamless joint working and problem-solving challenges together.
6.1.3 ‘Clinical’ or non-managerial supervision
‘Clinical’ or non-managerial supervision will enable the SPLW to manage the emotional impact of their work and be guided by clinicians on dealing effectively with patient risk factors.
Clinical supervision supports continued professional development to enable a SPLW to develop in their role, ensure patient safety and high-quality care, by identifying training and development needs and supporting reflective practice. It is important that the supervisor possesses the skills and competencies needed to offer a constructive supervisory relationship and environment.
How is clinical supervision different to workplace supervision?
| Workplace supervision | …includes the day to day oversight of the SPLW role by the GP supervisor and line manager. It is a space to discuss how you’re getting on with referrals, discuss issues relating to your schedule and contract. It is also a place to access emergency support (via the named GP) when there are concerns over specific cases, particularly in relation to safety and safeguarding. |
| Clinical supervision | …is the space to reflect more deeply on professional practice with a supervisor, ideally independent from the immediate work area. They will be skilled in supporting SPLWs to work through and develop their practice, themselves and the relationship with clients and the wider service. It is a place to discuss where the boundaries of practice are tested and explore options and solutions. |
6.2 Supervisor roles and skills
The Personalised Care Institute (PCI) have developed supervision recommendations for staff supervising SPLWs, exploring how the different types of supervision are delivered, and the skills needed by supervisors (Annex C). It aims to describe the supervisors’ roles in working with their staff member to use a structured approach to orientate and embed skills in the workplace.
Alongside the competency framework (Annex A), the PCI’s supervision recommendations are designed to create a partnership between SPLW and supervisor, to promote safe and effective practice. It provides a foundation for personal and professional training and development for supervisors as well as giving a framework for support for the SPLW.
7. Ways of working: professional framework
7.1 Working with people
SPLWs will support a wide variety of people from diverse backgrounds, including people with a range of conditions and disabilities. They should be able to adapt their communication approach to individual needs, including using plain language and culturally appropriate communication. SPLWs should ensure the people they support are able to say:
- I am listened to and understood, and ‘what matters to me’ is central to all our work together
- I am respected and treated with dignity as an individual
- My human rights are protected, and I do not experience discrimination
- I experience warm, compassionate, personalised care and support
- If I raise a concern or make a complaint, it is acted on quickly
SPLWs should work with people to set clear expectations around their expertise and knowledge and how they can support the individual. This includes establishing boundaries and being clear on issues around confidentiality and safeguarding.
7.2 Multidisciplinary teams
A multidisciplinary team (MDT) is a group of professionals working together with the person at the heart. MDTs can be in place in primary, secondary and community settings. Working this way allows a wrap-around, holistic approach to supporting individuals, looking at everything that affects their health and wellbeing, and allows professionals to work together to explore problems and reach shared solutions. The MDT allows a wide range of experts to work with an individual, including those from health services, social care and the VCSE sector.
In line with the Network Contract DES, SPLWs must be embedded within the PCN’s core network practices and be fully integrated within the MDT. They must have access to other healthcare professionals, to electronic ‘live’ and paper-based record systems of the PCN’s Core Network Practices, as well as access to admin/office support and training and development as appropriate.
SPLWs are not responsible for leading or convening MDT meetings, but they may present a patient in the same way other colleagues do.
SPLWs should attend MDT meetings to offer expertise on where SPLW support or community support would be beneficial to a patient, and enable the MDT to support patients with their social, emotional and practical needs through community support as well clinical treatments.
Considering care from this perspective will also enable patients to make the most of clinical treatment available, by building support networks and connections and reducing barriers to accessing care to enable the best outcomes. Where there is doubt, or the clinical situation is complex, SPLWs should ensure that the goals and plan have been checked with a clinician involved in that individual’s care. This level of MDT working helps to secure patient safety and can provide case-based learning for the SPLW’s portfolio.
SPLWs will need an induction to MDT working and the range of roles within the MDT, and likewise MDT colleagues also require an introduction to the SPLW role, their offer to patients, and the process for referrals (Network Contract DES B3.9). This could be done through regular practice team training, mutual job shadowing, or share and learn sessions.
SPLWs also work closely with a range of community agencies. SPLWs need protected time to build strong working relationships with these services to work effectively and bring external colleagues to the MDT where this adds value.
7.3 Personalised Care roles
SPLWs also work closely with other personalised care roles, including health and wellbeing coaches and care co-ordinators.
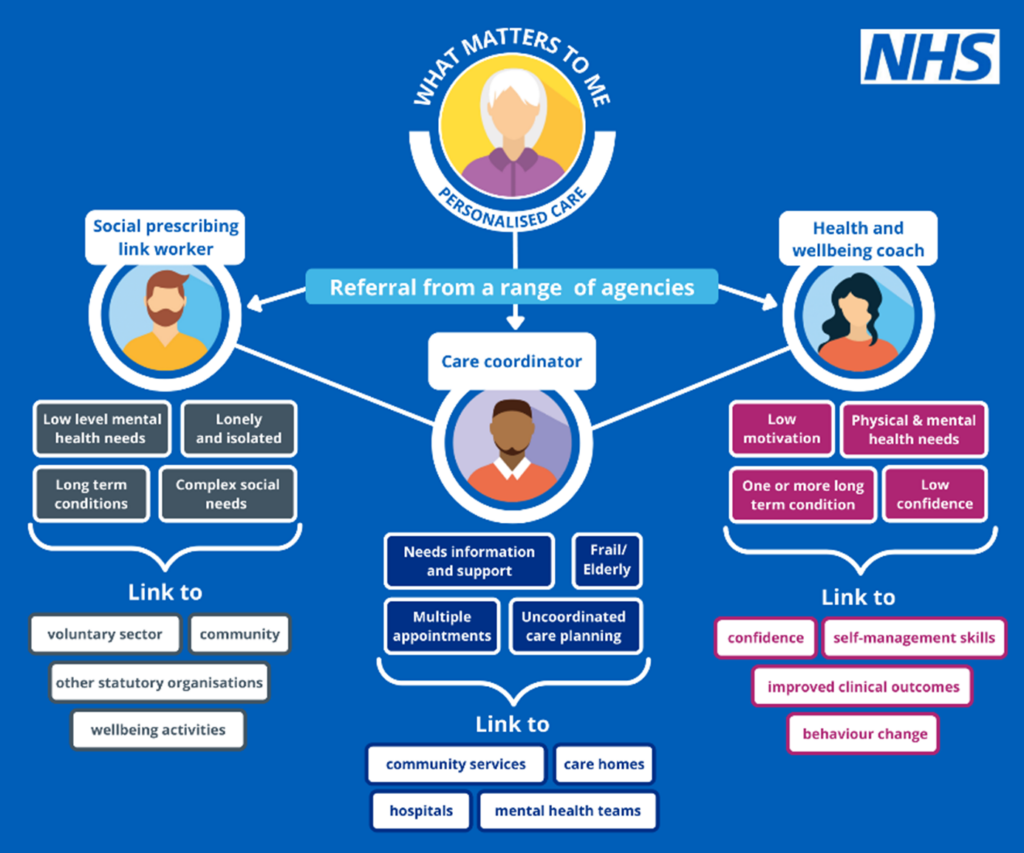
All three of these roles have expertise in personalised care approaches and working with people to understand their situation and needs, but each has a distinct role and skills. Information about the roles of health and wellbeing coaches and care co-ordinators can be found on the NHS England website.
8. Professional values and behaviours
SPLWs should believe in and be committed to the values set out in the NHS Constitution, along with the principles of personalised care and focusing on what matters to the person.
There are six NHS values that all staff are expected to demonstrate:
- Working together for patients
- Respect and dignity
- Commitment to quality of care
- Compassion
- Improving lives
- Everyone counts
As SPLWs sit in both the health and community worlds, and are not uniquely employed within PCNs, employers may have their own set of values and professional behaviours that they expect of all staff. It is the responsibility of the employer to communicate their values and expectations around these to SPLWs during recruitment, induction and supervision.
There are also existing voluntary codes of practice which SPLWs and employing organisations can sign up to if they choose to be members of support organisations.
9. Competency Framework
The Competency Framework (Annex A) sets out the core competencies that all SPLWs working in or with PCNs need in order to deliver their role, and is designed to assist those who employ or direct the activities of SPLWs to understand the competencies for practicing safely and effectively in their role, and how these competencies can be achieved.
It should be used to ensure that people with the right skills and abilities are being recruited to the SPLW role, and as a tool to support CPD.
These competencies are aligned to the NHS England sample job description for SPLWs and the Core Curriculum for Personalised Care published by the PCI).
The framework is divided into four areas:
- Competencies to engage and connect with people
- Competencies to enable and support people
- Competencies to enable community development
- Competencies for safe and effective practice
For those in specialist roles or working with specific population groups, these core competencies will still apply. Specialist SPLWs will also need appropriate skills, experience or qualifications in working with specific client groups.
Recruitment, induction and supervision of SPLWs should include consideration of the competencies and plan how SPLWs will be supported to demonstrate and develop their skills. The competency framework can be used in combination with the Portfolio of Evidence (Annex B).
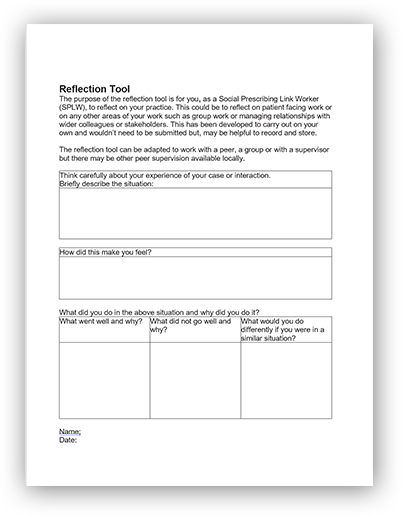
10. Portfolio of evidence
The Portfolio of Evidence (Annex B) enables SPLWs and clinical supervisors to evidence the depth of their knowledge, skills and behaviours. The Portfolio of Evidence is not a formal assessment tool, but a supportive toolkit for SPLWs to build their reflective practice.
It provides tools to:
- Evidence and reflect on practice
- Identify CPD needs and opportunities
- Demonstrate the impact of social prescribing
- Demonstrate how SPLWs can work as part of the MDT
- Support supervisors to understand the SPLW role
The Portfolio of Evidence includes:
- Observation sheet and a pre observation guidance sheet
- Reflective practice tool
- Case study template
- Patient feedback survey
The Portfolio provides suggestions on how and when to use each tool, but SPLWs and employers are encouraged to use the portfolio in the way that works best for them, including agreeing frequency of use and format. SPLWs may find protected time to use the tools and reflect on their practice useful.
The Portfolio of Evidence has been developed by the National Academy of Social Prescribing (NASP) on behalf of NHS England.
11. Career pathways
11.1 Entry into the SPLW role
There is no single route into being a SPLW, and the wide range of backgrounds is a strength given the wide range of issues that SPLWs support people with, and when building teams of SPLWs and working with a range of population groups.
Research by National Association of Link Workers (NALW) shows a wide range of entry routes, previous experience, existing qualifications of SPLWs, and an equally wide range of progression routes (see Annex D). This research shows a wide range of prior professional roles and levels of academic qualification which provide a potentially large pool of skilled and experienced candidates for recruitment into SPLW roles.
As the SPLW profession grows, further work on developing career pathways and progression routes would be welcome.
Informal routes into employment and tackling inequality
In addition to entry routes based on prior professional experience, social prescribing can offer a route into employment for those who may have lived experience, but few formal qualifications, given the emphasis on personal qualities and life experience in the sample job description and competency framework.
A community health and wellbeing worker apprenticeship is one route into the role of SPLW. The purpose of a community health and wellbeing worker is to work in partnership with individuals and their communities to identify and address health and wellbeing needs, improve health, prevent ill-health and reduce inequalities. After completing the apprenticeship people may choose a career as a SPLW. However, they would still need to demonstrate the necessary competencies, be committed to personalised care and have the necessary SPLW training set out in earlier sections.
Similarly, those who take a route to employment through volunteering in community services may find that this experience offers a route into SPLW and other similar roles. In this way, social prescribing can be a powerful force in tackling inequity in employment opportunities as well as health inequalities.
11.2 Career development
The competency framework, the portfolio of evidence and clinical supervision will help SPLWs to identify how their skills and experience can be transferrable to new roles.
For example, the core personalised care skills essential to working with people may lead SPLWs into careers in coaching, counselling or to other clinical roles in the NHS, such as occupational therapy; skills of managing and reporting on data may lead to a route into evidence and service development; ability to manage multiple relationships and SPLW colleagues may lead to managerial roles within social prescribing services.
As well as progression into senior, specialist or managerial SPLW roles, or moving to SPLW roles in other organisations, the NALW research shows SPLWs moving on to community development roles, allied health professional roles, or assistant allied health professional roles such as dietetic assistant, occupational therapist or psychology, and to lifestyle roles such as coaching or counselling.
11.3 Progression into specialist roles
Developing SPLW specialisms may be important for the PCN in response to local health needs identified through the SPLW service or through population health management analysis or development of the local proactive social prescribing plan.
SPLWs may also be interested in developing specialisms related to their personal interests and strengths identified through their ongoing supervision. Specialisation is an emerging career pathway which enables retention of skilled and experienced SPLWs within PCNs.
Specialties that are emerging include supporting:
- Children and young people
- Mental health
- Financial inclusion and advice
- Refugees and asylum seekers
- Secondary care, including hospital discharge
The approach to developing specialist roles should be tailored to local needs. Models that are emerging include:
- Matrix approaches that develops theme lead roles within a team, where SPLWs have specialist knowledge but also take generalist cases
- Individual SPLWs specialising exclusively or primarily on a specific population cohort
- Specialist SPLWs acting as advisors on SPLW colleagues’ cases
Specialist roles can be developed as part of plans to proactively expand the local social prescribing offer. This could include increasing the number of SPLWs working in a service and providing both specialist and generalist support, building teams of SPLWs who complement each other.
While the SPLW Competency Framework describes core competencies for all SPLWs, employers should ensure that SPLWs moving into specialist roles are appropriately skilled, experienced and qualified, especially where they involve working with children and young people or vulnerable populations.
In addition, employers should ensure supervisors have the skills and experience to provide appropriate supervision for specialist roles.
11.4 Social prescribing management and leadership roles
Line management of social prescribing teams may be a natural progression for experienced SPLWs, and effective management can improve retention of the workforce.
Management is necessary to deliver high-quality social prescribing services, including elements outlined in this document on supervision and line management. Service managers may also have a service development function, working to ensure social prescribing is understood across the PCN and partners, building strategic relationships across organisations, creating a supportive and empowering environment for SPLWs to thrive, and using population health management data and developing proactive social prescribing services.
The template SPLW job description for PCNs is intentionally broad and includes elements that PCNs or employers may choose to separate out into a social prescribing managerial role.
As there is a growing workforce of skilled and ambitious professionals within systems, and organisations that wish to invest in the roles and maximise the benefit, it is natural that there are already programmes to enable SPLWs to develop and lead and we expect to see more similar programmes develop in the future.
12. Useful resources
12.1 Resources about social prescribing
- Welcome and induction pack for SPLWs in PCNs
- Making sense of social prescribing – University of Westminster Report
- What is social prescribing? – The King’s Fund explainer
12.2 Training and CPD related resources
- PCI website
- Social prescribing – learning for link workers e-learning modules
- NHS England social prescribing webinar series (you will need to register: Social Prescribing Collaboration Platform – FutureNHS Collaboration Platform).
12.3 Personalised care focused resources
- Personalised care and support planning
- Shared decision making
- Health and wellbeing coach
- Care co-ordination
- Supported self-management summary guide
- Measuring supported self-management
12.4 Primary care specific resources
- Network Contract Directed Enhanced Service specification: https://www.england.nhs.uk/publication/network-contract-directed-enhanced-service-contract-specification-2022-23-pcn-requirements-and-entitlements/
- Network Contract Directed Enhanced Service guidance: https://www.england.nhs.uk/publication/network-contract-directed-enhanced-service-guidance-for-2022-23-in-england/
- Further Network Contract Directed Enhanced Service links: https://www.england.nhs.uk/gp/investment/gp-contract/network-contract-directed-enhanced-service-des/
- Reference guide for primary care networks (PCNs)
12.5 Support for SPLWs working in the NHS
- Looking after you too – for staff working in primary care
- Looking after your career – for staff working in primary care
- Looking after your team – for staff working in primary care
- Supporting our NHS people
- Staff mental health and wellbeing hubs
13. Design group members
- Health Education England (HEE)
- Office of Health Improvement and Disparities (OHID)
- Personalised Care Institute (PCI)
- National Academy of Social Prescribing (NASP)
- National Association of Link Workers (NALW)
- Social Prescribing Network (SPN)
- University of Salford
- Regional advisors from range of NHS regions, systems, PCNs
- VCSE organisations
- NHSE Primary Care Workforce team
- PMA (formerly Practice Managers’ Association)
14 Annex A – SPLW competency framework
Overview
This competency framework has been designed to outline competencies for working in or with PCNs. This framework is aligned to the NHS England sample job description for SPLWs. This framework is also aligned to the Core curriculum for personalised care published by the Personalised Care Institute (PCI), which acts as the foundational framework for both personalised care and specific personalised care roles in primary care.
The Framework is divided into 4 competency areas:
- Competencies to engage and connect with people
- Competencies to enable and support people
- Competencies to enable community development
- Competencies for safe and effective practice
The content is designed to assist those who employ or direct the activities of SPLWs working in or with PCNs to understand the competencies for practicing safely and effectively in their role, and how these competencies can be achieved.
These competencies are applicable to all SPLWs working in or with PCNs.
This competency framework was co-produced by NHS England with stakeholders including the PCI, employers of SPLWs, and SPLWs. The template SPLW job description for PCNs is intentionally broad and includes elements that PCNs or employers may choose to separate out into a social prescribing managerial role.
1. Competencies to engage and connect people
A key element of successful social prescribing is the relationship built between SPLWs and the individuals they support. This relationship is built through meaningful conversations centred on the question “what matters to you?”
Competencies to engage and connect people are essential skills for all SPLWs to demonstrate. This includes how they communicate with individuals, how they listen, their non-verbal communication, and the personal values they hold and apply to their interactions. These skills are essential to gather and share information with individuals about how they can be supported , but they also create conversations that engage and motivate the individual they are working with and nurture trust. More information on skills to engage and connect people that are applicable to all personalised care roles can be found in the Personalised care curriculum.
|
Competency |
Description | Suggested route to achieve competency |
|
Gathers information and adapts questioning style for individual needs
| SPLWs should understand the importance of gathering accurate information from individuals and be able to adapt their questioning style to suit the individual they are working with. This includes, but is not limited to: Use open questions that cannot be answered with yes or no, e.g. “tell me more about…” allowing individuals to direct the conversation to what matters to themUse closed questions to focus around topics or subjects and to clarify key information, e.g. “do you think your caring responsibilities are manageable?” | Interactive skills training and e-learning, including module 1: Introduction to the social prescribing link worker role Assessed through observed practice and feedback from supervisors, colleagues and individuals
|
|
Demonstrates active listening | SPLWs should understand how active listening techniques to build a relationship with the individual they are working with and ensure the information they gather is accurate. This includes, but is not limited to: Demonstrate listening through body language and non-verbal cues, including being aware of posture, proximity, body movements and features, facial expression, eye contact, using pauses and silence to allow time for the individual to speak, cues such as nods and other vocal cues including agreementDemonstrate being present psychologically, socially and emotionally, making a conscious effort to remove distractions and hear and understand what the individual is communicating Reflect what they have heard back to the individual using the same language, helping them to feel heard and build rapport. | Interactive skills training and e-learning including module 1: Introduction to the social prescribing link worker role Assessed through observed practice and feedback from supervisors, colleagues and individuals
|
|
Clarifies and summarises information as appropriate | SPLWs should understand the importance of clarifying and summarising the information they have gathered with the individual for accuracy and to ensure they have covered all topics that matter to the person. This includes, but is not limited to: Adapt their questioning style to check understanding and confirm meaning with the individual, which may include further questioning on points that are unclear, clarifying background information, the situation or the meaning of words the individual has usedUse explicit verbal summaries of the information they have gathered from the individual they are supporting. This includes both internal summaries focusing on specific topics in the conversation, and a final summary at the end of the conversation Use summarised information to review where the conversation has got to, order the information in a way that makes sense, identify gaps in the information and consider next steps in personalised care and support planning | Interactive skills training and e-learning including module 1: Introduction to the social prescribing link worker role Assessed through observed practice and feedback from supervisors, colleagues and individuals
|
|
De-mystifies information and checks understanding | SPLWs should understand that different people have different perspectives, interpretations and understanding of situations and understand the need to check shared understanding. This includes, but is not limited to: Use models such as Benefits, Risks, Alternatives and outcomes from doing Nothing (BRAN) to check shared understanding and discuss what each possibility means within the context of the individual’s life and situationUse appropriate language to de-mystify information, including helping an individual to work through individual steps of a situation, translating jargon (for example, where an individual is experiencing financial difficulties) and adapting communication to meet individual needs. | Interactive skills training and e-learning including module 1: Introduction to the social prescribing link worker role Assessed through observed practice and feedback from supervisors, colleagues and individuals
|
|
Empathises with individuals, their thoughts, feelings and actions | SPLWs should understand the importance of building a relationship with individuals and adapt their behaviour to do this, while maintaining appropriate boundaries. This includes but is not limited to: Use affirmative statements about an individual’s actions, making positive statements and acknowledging efforts and achievements of the individual; for example, “you told me you tried to change this before, that shows great determination” Demonstrate acknowledgement that an individual’s thoughts, feelings and symptoms are normal reactions and that other people report similar experiences in response to their circumstances Demonstrate empathy by reflecting and using words to let the individual know the SPLW is trying to understand how situations feel for them. This includes looking at things from the perspective of the individual, avoiding judgement, recognising emotions, and communicating key observations. | Interactive skills training and e-learning including module 1: Introduction to the social prescribing link worker role Assessed through observed practice and feedback from supervisors, colleagues and individuals
|
|
Confidently approaches difficult conversations | SPLWs should understand that individuals may find it difficult to have conversations on difficult topics such as their mental health and domestic abuse situations and understand why this is. SPLWs should be able to establish rapport and build trust, in order to enable possibility for difficult conversations to be held. SPLWs should demonstrate other competencies contained within section 1 to build positive relationships SPLWs should demonstrate confidence in exploring difficult topics, using appropriate tools to structure conversations if required | Interactive skills training and e-learning including module 1: Introduction to the social prescribing link worker role Assessed through observed practice and feedback from supervisors, colleagues and individuals
|
|
Communicates according to needs and preferences | SPLWs should demonstrate excellent communication skills with individuals, using appropriate methods and mechanisms including non-verbal communication skills. This includes but is not limited to: Understand how communication can be adapted including how to adapt information according to the Accessible Information Standard for people with learning disabilities and/or autism, the right to have an interpreter or to be accompanied during appointments, and the right to have written information translated Ask if the individual has communication preferences, including when they would like to receive information and the format in which they would like to receive it Adapt to meet communication needs in line with an individual’s identified preferences, needs and rights | Interactive skills training and e-learning, including training on the Accessible Information Standard and including module 1: Introduction to the social prescribing link worker role Assessed through observed practice and feedback from supervisors, colleagues and individuals.
|
|
Demonstrates environmental awareness | SPLWs should know the impact of environment in providing a safe space to build a relationship and explore “what matters to you”. This includes but is not limited to: Adapt the environment by physically rearranging space to provide a welcoming and safe environment to have difficult conversations; such as ensuring privacy in a practice setting, rearranging chairs and providing a welcoming environment Adapt the setting to suit an individual’s needs and preferences; for example, meeting in a neutral space in the community or a person’s home where appropriate or offering virtual appointments |
Interactive skills training and e-learning including module 1: Introduction to the social prescribing link worker role.
Assessed through observed practice and feedback from supervisors, colleagues and individuals.
|
|
Able to utilise a range of consultation methods | SPLWs should understand the positives and negatives of these consultation methods, including digital exclusion and how to adapt consultation methods for people with additional access needs; including sensory disability, learning disability or additional language needs. SPLWs should demonstrate adequate skills in using technology, telehealth and remote consultations and adapt consultation when required | Interactive skills training and e-learning including module 1: Introduction to the social prescribing link worker role Assessed through observed practice and feedback from supervisors, colleagues and individuals |
2. Competencies to enable and support people
SPLWs should demonstrate competencies in using information gathered through the relationship to enable and support individuals to connect with their community for health and wellbeing through co-producing a personalised care and support plan, setting goals, and exploring options to meet that goal.
|
Competency |
Description |
Suggested route to achieve competency |
|
Undertakes personalised care and support planning |
SPLWs should understand the importance of personalised care and support planning with individuals and that this process should be led by the individual. SPLWs should be able to demonstrate this process, including: Use competencies from Section 1 to undertake a first holistic assessment with an individual around their health and wellbeing and supporting an individual to come up with a plan that records conversations, decisions and agreed outcomes in a way that makes sense to the individual, using their own words Use this first holistic conversation to discuss potential options and the way forward, sharing and checking understanding of the full range of options, including taking no action Co-produce outcomes with an individual that are achievable and effective, considering an individual’s levels of confidence, capability and opportunity, with a clear route forward to achieve these outcomes Demonstrate the ability to record the conversation in an organised structure allowing the individual to tell their story once and so that information can be updated in the future |
Interactive skills training and e-learning, including module 2: Developing personalised care and support plans with people Assessed through observed practice and feedback from supervisors, colleagues and individuals |
|
Assesses and adapts to individual levels of activation |
SPLWs should define patient activation as the knowledge, skills and confidence a person has in managing their own health and care. This includes: Know the impact patient activation has on an individual’s ability to engage with health and care services and manage their own health and understand that this can vary from day to day, situation to situation Assess an individual’s level of activation through informal or formal assessment, using relevant tools Adapt practice to support individuals with different levels of activation, including adapting practice with the same individual as their activation levels fluctuate |
Interactive skills training and e-learning including module 2: Developing personalised care and support plans with people Assessed through observed practice and feedback from supervisors, colleagues and individuals Consider specific training on patient activation |
|
Assesses and adapts to levels of health literacy |
SPLWs should define health literacy as individuals having enough knowledge, understanding, skills and confidence to use health information to be active partners in their care and successfully navigate health and social care systems. This includes: the impact health literacy has on an individual’s ability to navigate health and social care systems and how this may impact upon their ability to engage with social prescribing Assess an individual’s health literacy through informal or formal assessment, using relevant tools Adapt the information given to an individual accordingly to meet their current levels of health literacy Plan a route to increasing health literacy in a way to support achievement of outcomes identified through personalised care planning, e.g. through working on a specific topic or service an individual may need to interact with for their health and wellbeing |
Interactive skills training and e-learning including module 2: Developing personalised care and support plans with people
Assessed through observed practice and feedback from supervisors, colleagues and individuals |
|
Promotes and supports behaviour change through coaching and motivational interviewing techniques
|
SPLWs should understand that behaviour change is a dynamic process and be able to use specific techniques to engage individuals, explore strengths and aspirations, explore motivation for change and promote autonomy in decision making. This includes but is not limited to: Understand theoretical models of behaviour change as they apply to social prescribing; for example, the COM-B model of behaviour change or the transtheoretical model of change Demonstrate and apply the theory behind health coaching approaches to interactions with individuals Demonstrate and apply motivational interviewing approaches in interactions with individuals Understand the theory behind ‘making every contact count’ and use all interactions with individuals to have conversations about health and wellbeing |
Interactive skills training and e-learning including module 2: Developing personalised care and support plans with people. Assessed through observed practice and feedback from supervisors, colleagues and individuals. Consider specific training on behaviour change, including health coaching, motivational interviewing and making every contact count. |
|
Demonstrates cultural competence and understanding of equality, diversity and inclusion |
SPLWs should understand the concept of cultural competence and define this as how culture influences the way individuals think and act, their values and their understanding of health and wellbeing. SPLWs should: Demonstrate awareness and respect of difference and diversity Apply this knowledge and understanding in order to adapt the way in which they work with individuals from different cultures to facilitate conversations, considering individual values and needs Reflect on their own attitudes and behaviour towards all forms of difference and diversity, and adapt behaviour and approach when required |
Interactive skills training and e-learning including module 2: Developing personalised care and support plans with people Assessed through observed practice and feedback from supervisors, colleagues and individuals
|
|
Assesses progress against personalised care and support plan goals
|
SPLWs should understand the importance of working with individuals to reach the outcomes they have identified through personalised care and support planning Assess progress towards outcomes through personalised conversations with the individual, demonstrating skills from sections 1 and 2 of this Competency framework Adapt the plan to support individuals to meet their desired outcomes through flexible exploration of new routes and opportunities according to changing circumstances |
Interactive skills training and e-learning including module 2: Developing personalised care and support plans with people Assessed through observed practice and feedback from supervisors, colleagues and individuals |
3. Community development
Effective social prescribing relies on a range of activities and support to refer people to in the community. The following competencies relate to the SPLW role in community development, including identifying, nurturing and supporting the development of community resources.
| Competency | Description | Suggested route to achieve competency |
|
Understands the importance of patient and public involvement in social prescribing services | SPLWs should understand the meaning and importance of co-production and co-design and build co-production principles and values into all interactions. This includes: SPLWs should know the requirements for NHS organisations to demonstrate patient and public involvement in designing and delivering health services Facilitate the gathering of information on services and experience through patient and community feedback forms, surveys, focus groups or other forms of feedback Apply co-production principles to their work with the community in understanding gaps in service provision, and in supporting service planning, design and delivery Apply skills and knowledge to identify and support individuals who may want to use their experience to support other people in their community or to become involved in coproduction, including promoting the Peer Leadership Development Programme to those individuals | Interactive skills training and e-learning, including module 4: Introducing people to community groups and VCSE organisations Assessed through observed practice and feedback from supervisors, colleagues and individuals Consider specific training in strategic co-production |
|
Identifies and maps community assets, including essential information | SPLWs should understand the Asset-Based Community Development (ABCD) approach as a process that facilitates the sustainable development of communities based on strength and potential opportunity SPLWs should apply the ABCD approach to their role in supporting community development, including: SPLWs should know how to identify and map community assets such as groups, services and support organisations, community strengths and potential to support health and wellbeing SPLWs should record mapping and alignment opportunities including referral pathways and criteria, and objectives of groups and services SPLWs should collaborate with community partners in mapping assets, provision and opportunities in local areas | Interactive skills training and e-learning including module 3 Developing partnerships and module 4: Introducing people to community groups and VCSE organisations Assessed through observed practice and feedback from supervisors, colleagues and individuals |
|
Contributes to asset-based community development and community resilience | SPLWs should use mapping to identify gaps in provision especially regarding health inequalities, recording these gaps and escalating through formal feedback routes eg to a supervising GP, SP service manager, CCG, or appropriate VCSE organisation SPLWs should facilitate co-production and co-design as outlined in Section 3 of this Competency Framework to support community development with the individuals at the centre SPLWs should collaborate with partners in other organisations when supporting community development in order not to duplicate or undermine existing development or provision | Interactive skills training and e-learning including module 4: Introducing people to community groups and VCSE organisations. Assessed through observed practice and feedback from supervisors, colleagues and individuals Consider specific training on asset-based community development (ABCD) |
|
Supports people to attend community groups and/or services | SPLWs should apply the knowledge they have about asset-based community development approaches to identify appropriate of community assets for individuals, including: Assess quality of offers considering issues such as safeguarding or transparency of group organisational structures using formal or informal approaches, eg a checklist Identify offers that are appropriate to meet an individual’s outcomes, activation, health literacy and wider needs as identified by the individual in the personalised care and support planning process Apply knowledge about practical barriers to community participation such as transport and communication needs and plan how and if these can be overcome with individuals | Interactive skills training and e-learning including module 4: Introducing people to community groups and VCSE organisations Assessed through observed practice and feedback from supervisors, colleagues and individuals
|
|
Supports accessibility of community groups and/or services | SPLWs should know the requirements for community groups and services regarding accessibility and understand the ways in which they can support and promote accessibility in the community SPLWs should apply this knowledge to make appropriate and achievable recommendations to facilitate access for individuals, both to the individual (e.g. seeking transport) and to the group or service (e.g. contacting in advance to discuss accessibility; discussing adaptations individuals may need to attend) | Interactive skills training and e-learning including module 4: Introducing people to community groups and VCSE organisations Assessed through observed practice and feedback from supervisors, colleagues and individuals |
|
Demonstrates awareness of grants and commissioning processes | SPLWs should understand that funding and commissioning arrangements can enhance or reduce community resilience if not co-ordinated effectively SPLWs should know which national and local grants are available to support community development and individuals and facilitate this process through providing appropriate supporting information to contribute to grant applications and commissioning. This may apply to commissioning and grants for services or individuals. Where appropriate SPLWs should be sufficiently skilled to support individuals to apply for grants on their own behalf | Interactive skills training and e-learning including module 4: Introducing people to community groups and VCSE organisations Assessed through observed practice and feedback from supervisors, colleagues and individuals |
|
Demonstrates awareness of PHBs | SPLWs should know what a personal health budget is and how they may be used to support delivery of a personalised support plan. SPLWs should apply this knowledge and support individuals to access personal health budgets where appropriate, and to support them to meet their personalised health and wellbeing outcomes | Interactive skills training and e-learning including module 4: Introducing people to community groups and VCSE organisations. Assessed through observed practice and feedback from supervisors, colleagues and individuals |
4. Competencies for Safe and Effective Practice
SPLWs work with individuals who may have complex health or care needs. It is essential that SPLWs are competent to practice safely and offer individuals evidence-based interventions, and that they record outcomes from their work. This includes SPLWs working to standards set in the NHS and working within approved models and frameworks to ensure both the SPLW and individual they are working with remain safe and working together in a professional relationship.
| Competency | Description | Suggested Route to Achieve Competency |
| Is an effective and trusted member of the multidisciplinary team (MDT) | SPLWs should behave as an effective and trusted member of the MDT and understand the roles of colleagues, making their own unique contribution to the team. This includes: Understand the boundaries of the SPLW role and how and when to escalate or refer individuals to other health professionalsUnderstand the role of other health and care professionals, their remit and limitations of the service they offer Reflect on own knowledge levels and seek out ways to develop understanding of other roles e.g. shadowing members of the MDT or VCSE service colleagues, and provide this in return to promote the SPLW roleDemonstrate respect for colleagues and use professional behaviours and language at work | Interactive skills training and e-learning including module 3: Developing partnerships Assessed through observed practice and feedback from supervisors, colleagues and individuals |
|
Maintains compliance with mandatory and statutory training | SPLWs should understand the requirement to complete mandatory and statutory training in line with their primary care or VCSE employing organisation, and how this ensures their safety at work SPLWs should take responsibility for maintaining and updating training as appropriate.SPLWs should apply knowledge gained through their mandatory and statutory training in all situations Training may include but is not limited to:
| Mandatory and statutory training Assessed through completion of mandatory and statutory training and application to the workplace through observed practice and feedback from supervisors, colleagues and individuals |
|
Understands obligation to safeguard individuals from harm | SPLWs should understand their responsibility to safeguard children and adults and understand the importance of this when working with vulnerable individuals SPLWs should apply knowledge gained through mandatory and statutory training in safeguarding to identify those who may be at risk of harm and follow appropriate processes to safeguard individuals, including escalation to a named supervisor when appropriate, and understand the risks and implications of not doing so | Mandatory and statutory training and e-learning, including module 5: Safeguarding vulnerable people Assessed through completion of mandatory and statutory training and application to the workplace through observed practice and feedback from supervisors, colleagues and individualsConsider specific training on local safeguarding systems |
|
Understands and maintains compliance with information governance principles and protocols
| SPLWs should understand the principles of information sharing and governance as set out in law and guidance SPLWs should apply information sharing processes including use of secure emails and information storageSPLWs should understand consent and information sharing processes when working with young people under the age of 16 years, as per Gillick Competence as applied to consent for non-medical support and intervention SPLWs should understand consent and information sharing processes when working with adults as per the Mental Capacity Act 2005 | Mandatory and statutory training Assessed through completion of mandatory and statutory training and application to the workplace through observed practice and feedback from supervisors, colleagues and individuals |
|
Understands obligations to keep and maintain accurate records | SPLWs should understand their responsibility to maintain accurate and timely records on their work with individuals and understand how this protects both themselves and the individuals they work with SPLWs should also understand the benefit to individuals of them telling their story once and not having to repeat this multiple times and apply this knowledge to record-sharing with other agencies or professionals | Mandatory and statutory training and e-learning including module 6: Keeping records and measuring impact Assessed through completion of mandatory and statutory training and application to the workplace through observed practice and feedback from supervisors, colleagues and individuals |
|
Understands the social/wider determinants of health, health inequalities and population health | SPLWs should understand key terminology around the wider determinants of health and the interface with health inequalities SPLWS should understand how the wider determinants of health impact on health and wellbeing, including the dynamic between person, environment and occupation and the biopsychosocial model as it applies to social prescribingSPLWs should understand the concept of social prescribing as a public health intervention and how it can positively contribute to prevention of physical and mental ill health at a primary, secondary and tertiary level SPLWs should understand summary evidence for social prescribing for specific population groups at risk of experiencing health inequalitiesSPLWs should know information relating to their local population and the health inequalities it experiences SPLWs should apply this knowledge to target specific health inequalities in their practice, particularly where resources are scarce. This may include working to make services more accessible to individuals e.g. those from inclusion health groups, or by targeting population groups to offer proactive access to social prescribing SPLWs should use this knowledge to contribute to decisions made in the wider MDT on which groups are a priority for social prescribing, including but not limited to:
| Interactive skills training and e-learning. Assessed through observed practice and feedback from supervisors, colleagues and individuals. |
|
Utilises available evidence base for social prescribing interventions and activities | SPLWs should understand summary evidence for social prescribing interventions including arts and creativity, sports and physical activity, and nature-based activities to promote health and wellbeing Understand summary evidence for practical support for needs that affect their health, such as housing, debt management and relationship difficultiesApply this knowledge to the way they work with individuals and services and select those most appropriate to an individual and their desired outcomes | Interactive skills training and e-learning Assessed through observed practice and feedback from supervisors, colleagues and individuals |
|
Records and demonstrates impact through multiple routes | SPLWs should understand the importance of measuring outcomes to demonstrate the impact of social prescribing and how evidence can contribute to community development through commissioning for outcomes. SPLWs should know appropriate outcome measures for use in social prescribing eg the ONS4 and apply this knowledge to select and use appropriate outcome measures for individuals, including recognising when these measures are not appropriate.SPLWs should know other approaches to recording outcomes outside formal outcome measurement and apply this knowledge within a personalised approach to demonstrate impact, including promoting individual stories and case studies, and measuring satisfaction of the service. | Interactive skills training and e-learning including module 6: Keeping records and measuring impact. Assessed through observed practice and feedback from supervisors, colleagues and individuals. |
15 Annex B – Portfolio of evidence
Introduction to Portfolio of Evidence
1. Background
The National Academy of Social Prescribing (NASP), has been commissioned by the Personalised Care team at NHS England to develop a portfolio of evidence, to evidence practice and skills of social prescribing link workers (SPLWs). In early 2022, NASP called on SPLWs and their supervisors to test and feedback on a draft version of the portfolio of evidence.
We had a diverse representation of over 60 SPLWs and supervisors that provided feedback and suggestions. This varied from new to established SPLWs as well as varied employment arrangements. We also had stakeholder input including the Personalised Care Institute (PCI).
After collating extensive feedback from SPLWs supervisors and stakeholders we are proud to present the portfolio of evidence resource for SPLWs and their employers/supervisors to use.
2. Purpose
The purpose of the Portfolio of Evidence is to allow SPLWs to evidence the depth of their knowledge, skills and competencies in line with the draft NHS England social prescribing link worker competency Framework.
We encourage all SPLWs and their supervisors to use this Portfolio of Evidence to:
- Evidence and reflect on practice
- Identify any training development opportunities
- Demonstrate why social prescribing matters to people
- Demonstrate how a SPLW can work as part of a multidisciplinary team
- Help supervisors to better understand the SPLW role
The Portfolio of Evidence is not for formal assessment purposes but a tool for SPLWs to record and evidence their skills and practice. Additional guidance and suggestions on how and when to use each tool has been provided, and NASP and NHS England encourage SPLWs and their employers to use the portfolio of evidence in the way that works best for them, including frequency. We also suggest SPLWs are provided with protected time to use the tools and reflect on their practice.
The Portfolio of Evidence includes:
Observation sheet (and a pre observation guidance sheet)
- Frequency of use can be decided between SPLW and supervisor, but we would encourage use every 6-12 months. Further guidance in the Guidance for SPLW observation.
Reflective practice tool
- This is a reflective practice tool for SPLWs and not for submission to supervisors. This can be adapted for peer supervision and regional and local peer supervision may also be available.
Case Study template
- Some employers and commissioners request case studies as part of continuing professional development or general communications and evidencing impact of SPLW role on people.
Feedback survey
- Some employers and professional supervisors may find this helpful when trying to demonstrate impact of social prescribing within primary care or other settings.
- Two feedback surveys available; one for service users and one for wider colleagues if appropriate.
3. How to embed Portfolio of Evidence in practice
All ARRS funded SPLWs will be encouraged by NASP and NHS England to use the Portfolio of Evidence. The Network Contract Directed Enhanced Service contract sets out requirements for SPLW training, development and supervision which includes:
Mandatory completion of the NHS England online learning programme.
- Enrolled in, undertaking or qualified from appropriate training as set out by the Personalised Care Institute.
- Attendance at peer support networks run by NHS England delivered at integrated care system (ICS) level.
- Provide monthly access for SPLWs to clinical supervision with a relevant health professional within the primary care network (PCN) multidisciplinary team.
Completing the portfolio of evidence can help SPLWs and their employers and supervisors to meet the above requirements.
4. Who supervises a SPLW?
There are many Additional Role Reimbursement Scheme (ARRS) funded SPLW employment arrangements and it is useful to understand how roles are employed (e.g. hosted by a VCSE organisation on behalf of a PCN or employed directly by a PCN) as this will help supervisors to understand the support available to SPLWs.
It is important to clarify the various functions of supervisors.
A workplace supervisor means supervising SPLWs in their day-to-day practice to ensure that they have opportunities to develop their role within the limits of patient safety service provision, their scope of practice and their professional and personal competence.
Supervision should be readily accessible on a daily basis, and flexible according to the needs of the individual, working context, and complexity of their role.
A clinical supervisor (refers to monitoring and supporting the professional progress of individual SPLWs over time. It aligns learning needs with curriculum and competency framework learning outcomes. Clinical supervision uses experiential learning and workplace feedback as opportunities to engage in reflective practice, provide feedback and undertake professional development planning.
Here, we recommend the clinical supervisor leads on the Observation tool. The other tools are for SPLWs to record their practice and available to share to both workplace and professional supervisors if appropriate or needed.
5. Summary
This Portfolio of Evidence was developed in response to a need for SPLWs to evidence their practice and skills. We always appreciate feedback and view the Portfolio of Evidence as an evolving piece of work. Therefore we are keen to hear more from you.
Please contact NASP at workforce@nasp.info
Reflection tool
Download the reflection tool form as a word document
SPLW Observation sheet
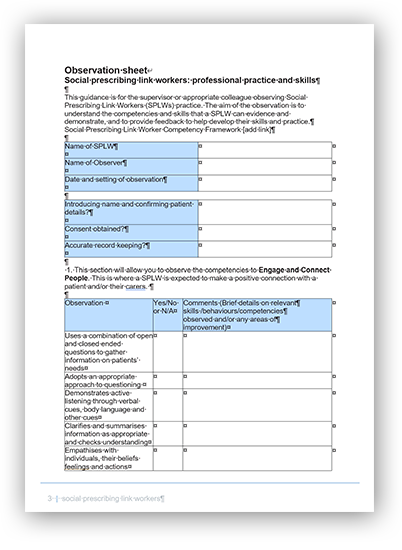
Download the observation sheet as a word document
Observation Sheet for SPLWs – Community Development
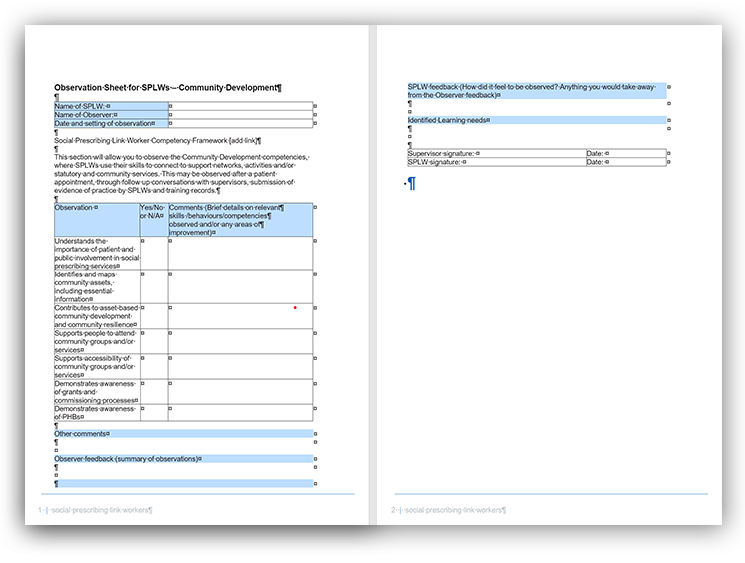
Download the Observation sheet for SPLWs – community development as a word document
Colleague’s Social Prescribing Link Worker Feedback
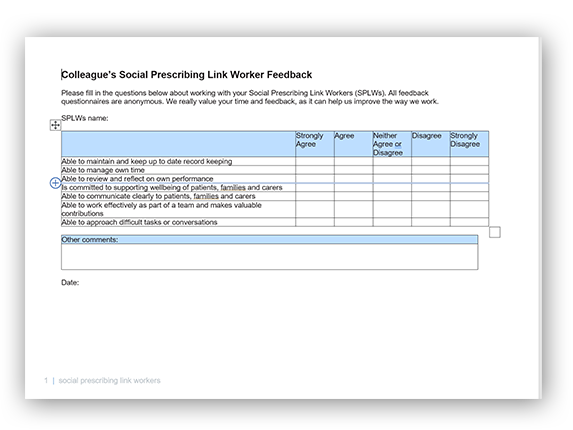
Download Colleague’s Social Prescribing Link Worker Feedback as a word document
Patient Social Prescribing Link Worker Feedback
Download Patient Social Prescribing Link Worker Feedback as a word document
Case study template
Introduction to the case study template
This template offers some guidance on how to communicate key focus areas on a case study. A good case study should be clear, concise and ideally not too long.
It’s also important to understand who the audience is and therefore this can be adapted quite easily (e.g. a case study to bring to a formal Action Learning Set / Group Supervision may need more detail, but a case study aimed for general communications to the public will need to be very brief with only key messages detailed).
The headlines provide some prompts and can be either included or removed as part of your case study.
Why write a case study?
Case studies can be useful in many ways. They can:
- motivate us – especially when we can see the impact of our work on people’s lives and what difference we’re making
- provide powerful stories for senior leaders and commissioners, who are always keen to hear more about what impact our work is making
- help us to learn from practice, to reflect and improve our work
- make the people we work with feel important and valued
- can help promote the importance of social prescribing
- provide a snapshot on how social prescribing link workers (SPLWs) work.
Questions to consider
For external facing/public facing case studies you may want to consider the following:
- Think about what would draw you to a case study?
- What is the key information you want to communicate?
- Who is this for? (Patients? Carers? Specific population groups?)
- Consider the language you use and how you present it, don’t use acronyms and write in Plain English
Case study template
Consent
Written consent should always be gained prior to use of a service user or colleague story, quotes and any pictures that may supplement the case study. Be explicit in the use and purpose of these i.e. are they being used in leaflets, website, social media or verbal presentations etc. Your Primary Care Network (PCN) or employer may be able to advise. Check if there is a local communications team that can help you. Your case study could also be used as a local, regional or national media story to help promote and spread the positive impact that SPLWs have on people’s health and wellbeing.
Consider capturing or asking for photos to go with the case study particularly if using on social media.
How to write a good case study
Case studies are a way to demonstrate how you work, or provide understanding to your work or role. They can be used for different purposes such as submission for commissioners; to understand how you work, or raising the profile of the Social Prescribing service locally.
Whilst it’s important to record facts and the narrative of an event for context, it’s equally important to explore the ‘why?’, which is helpful for reflection and learning. Therefore, consider reflective questions on the challenges and opportunities headlines (What went, well, less well, or could be done differently). The reflection tool can also be used as part of this to provide additional structure.
- Background (Brief explanation of case/situation/background (Age, gender, referral reason)
- Describe the approach (How were issues identified or how was the event you’re describing planned or discussed. Think about the ‘How’ here)
- Needs identified jointly (if case study related to service user interaction)
- What was the support offer and goal setting?
- Challenges (What didn’t go so well?)
- Opportunities (What went well? Did you learn anything here?)
- What happened after the appointment or event you’re describing?
- What was the outcome (Did patient / family / carer feel supported; were they engaged; were there any changes to their needs; do any ongoing needs still need to be addressed?)
- List of assets and services connected to this case study (optional)
- Quotes
- Conclusion (What’s next and how do you feel as a SPLW)
16 Annex C – Supervisor roles and skills
Personalised Care Institute recommendations for supervision of SPLWs
Supervision is a process by which individual SPLWs work with another person to meet their professional, organisational and personal objectives, which together promote best outcomes for the patient.
Workplace supervision means supervising SPLWs in their day-to-day practice to ensure that they have opportunities to develop their role within the limits of patient safety service provision, their scope of practice and their professional and personal competence.
Supervision should be readily accessible on a daily basis, and flexible according to the needs of the individual, working context, and complexity of their role.
Clinical supervision refers to monitoring and supporting the professional progress of individual SPLWs over time. It aligns learning needs with curriculum and competency framework learning outcomes. Clinical supervision uses experiential learning and workplace feedback as opportunities to engage in reflective practice, provide feedback and undertake professional development planning.
The delivery of clinical supervision is more formalised, usually external to the workplace, and planned at regular intervals, and at least monthly.
Group supervision refers to providing peer support through a small group or learning set as an additional or alternative format to individual clinical supervision of SPLWs. It provides opportunities for shared experience, peer learning, and a supportive environment. It is organised and facilitated by a suitably trained and experienced professional and is planned at regular intervals.
On the following pages we set out how the different types of supervision are delivered, and by whom, and what the supervisors own training needs may be.
Workplace supervision
Tasks | Criteria for supervisory role |
|
|
Clinical supervision
|
Tasks |
Criteria for supervisory role |
|
|
Group supervision
| Tasks | Criteria for supervisory role |
|
|
Training and supporting SPLW supervisors CWorkplace supervisors
|
Potential learning needs |
Resources |
|
Clinical supervisors
|
Potential learning needs |
Resources |
|
|
Group supervisors
|
Potential learning needs |
Resources |
|
Those of clinical supervisor plus:
|
|
17 Annex D – Career pathways research
Undertaken by National Association of Link Workers (NALW) on behalf of NHS England in Jan-March 2022
| Entry routes into SPLW role | Previous experience, knowledge and skills reported by respondents |
| A range of learned experience, skills and knowledge gained from various frontline client- facing jobs in health and social care, charities, local councils, other public and private sector, such as:
|
| Qualifications of SPLW respondents included Masters, Degree, NVQ, Diplomas in | Roles people reported moving onto |
|
|