June 2023
Foreword
The founding of the NHS 75 years ago was a huge milestone in our national history. It was born out of hope, and for millions of people it represented the chance of a healthier future for them and their families. But as a new national service it faced real challenges. Chief among them was building a workforce capable of meeting the needs of a population suffering the effects of war, poverty and diseases as yet untamed by science, including tuberculosis.
Fast forward to 2023: the NHS in England now has many times the number of staff, including doctors, nurses, therapists and scientists, and is therefore capable of delivering a far greater volume and breadth of care. But, at the same time, local services report vacancies totalling over 112,000. This is a reflection of how the needs of our population have grown and changed, thanks in large part to the role better care and advances in medicine have played in increasing life-expectancy by 13 years since 1948.
That change will continue; the number of people aged over 85 is estimated to grow 55% by 2037, as part of a continuing trend of population growth which outstrips comparable countries. Inaction in the face of demographic change is forecast to leave us with a shortfall of between 260,000 and 360,000 staff by 2036/37. The lack of a sufficient workforce, in number and mix of skills, is already impacting patient experience, service capacity and productivity, and constrains our ability to transform the way we look after our patients. A growing shortfall would mean growing challenges and lost opportunities.
If the NHS is to continue to be the health service the public overwhelmingly wants and is proud of – one which provides high quality care for patients, free at the point of need – it needs a robust and effective plan to ensure we have the right number of people, with the right skills and support in place to be able to deliver the kind of care people need.
The publication of our NHS Long Term Workforce Plan is therefore one of the most seminal moments in our 75-year history. This is the first time the government has asked the NHS to come up with a comprehensive workforce plan; a once-in-a-generation opportunity to put staffing on a sustainable footing and improve patient care.
We have grasped that opportunity. Our Plan is ambitious, and it is bold, while being rooted in the reality experienced by patients and staff now, and it is rigorously aligned to the improvements in care that we aspire to make for patients. Even more crucially, it doesn’t just herald the start of the biggest recruitment drive in health service history, but also of an ongoing programme of strategic workforce planning – something which is unique amongst other health care systems with national scale.
In the pages that follow, we set out a strategic direction for the long term, as well as concrete and pragmatic action to be taken locally, regionally and nationally in the short to medium term to address current workforce challenges. Those actions fall into three clear priority areas:
- Train: significantly increasing education and training to record levels, as well as increasing apprenticeships and alternative routes into professional roles, to deliver more doctors and dentists, more nurses and midwives, and more of other professional groups, including new roles designed to better meet the changing needs of patients and support the ongoing transformation of care.
- Retain: ensuring that we keep more of the staff we have within the health service by better supporting people throughout their careers, boosting the flexibilities we offer our staff to work in ways that suit them and work for patients, and continuing to improve the culture and leadership across NHS organisations.
- Reform: improving productivity by working and training in different ways, building broader teams with flexible skills, changing education and training to deliver more staff in roles and services where they are needed most, and ensuring staff have the right skills to take advantage of new technology that frees up clinicians’ time to care, increases flexibility in deployment, and provides the care patients need more effectively and efficiently.
Taking these actions will allow the NHS to make sustainable progress on our core priorities for patients, such as improving access to primary and community care, providing safe and timely urgent and emergency care, and continuing to reduce the COVID-19 backlog for elective care. And we welcome the government’s commitment to the Plan and investment to provide the additional education and training places we need over the next five years.
Developing a workforce plan that stands the test of time is a hard thing to do in any sector, and particularly so in the NHS. The evidence from our history tells us that the pace of technological and scientific progress means we cannot predict with certainty how the workforce needs of the NHS will look in 15 years’ time. The pressures of the present – felt by patients and staff alike – can also make the needs of the future feel less important.
But we can set a direction of travel, and commit – as we are – to this being the start of an ongoing process to refresh the Plan and ensure it is aligned with wider service planning. The coming together of NHS England, Health Education England and NHS Digital into a new, single organisation means we are now much better equipped to undertake this task, and therefore to ensure the health service is geared up to meet the evolving challenges – and take the emerging opportunities – that the next 15 years hold.
The strategy and actions set out in this Plan have been developed by the NHS, but done so in close partnership with staff groups and wider experts, with the support of the government. The number of organisations and individuals who deserve thanks for their contribution stretches into the hundreds. This Plan belongs to all of us.
As we now embark on the equally important job of delivering on its contents, and to the ongoing review and development needed to ensure it remains relevant to the changing needs of the people we serve, it will continue to take all of us to achieve success – an ambitious, sustainable and resilient NHS, there for patients now and for future generations.
Amanda Pritchard, NHS Chief Executive
Overview
We will ensure the NHS has the workforce it needs for the future.
Train – Grow the workforce
By significantly expanding domestic education, training and recruitment, we will have more healthcare professionals working in the NHS. This will include more doctors and nurses alongside an expansion in a range of other professions, including more staff working in new roles. This Plan sets out the path to:
- Double the number of medical school training places, taking the total number of places up to 15,000 a year by 2031/32, with more medical school places in areas with the greatest shortages, to level up training and help address geographical inequity. To support this ambition, we will increase the number of medical school places by a third, to 10,000 a year by 2028/29. The first new medical school places will be available from September 2025.
- Increase the number of GP training places by 50% to 6,000 by 2031/32. We will work towards this ambition by increasing the number of GP specialty training places to 5,000 a year by 2027/28. The first 500 new places will be available from September 2025.
- Increase adult nursing training places by 92%, taking the total number of places to nearly 38,000 by 2031/32. To support this ambition, we will increase training places to nearly 28,000 in 2028/29. This forms part of our ambition to increase the number of nursing and midwifery training places to around 58,000 by 2031/32. We will work towards achieving this by increasing places to over 44,000 by 2028/29, with 20% of registered nurses qualifying through apprenticeship routes compared to just 9% now.
- Provide 22% of all training for clinical staff through apprenticeship routes by 2031/32, up from just 7% today. To support this ambition, we will reach 16% by 2028/29. This will ensure we train enough staff in the right roles. Apprenticeships will help widen access to opportunities for people from all backgrounds and in underserved areas to join the NHS.
- Introduce medical degree apprenticeships, with pilots running in 2024/25, so that by 2031/32, 2,000 medical students will train via this route. We will work towards this ambition by growing medical degree apprenticeships to more than 850 by 2028/29.
- Expand dentistry training places by 40% so that there are over 1,100 places by 2031/32. To support this ambition, we will expand places by 24% by 2028/29, taking the overall number that year to 1,000 places.
- Train more NHS staff domestically. This will mean that we can reduce reliance on international recruitment and agency staff. In 15 years’ time, we expect around 9– 10.5% of our workforce to be recruited from overseas, compared to nearly a quarter now.
Retain – Embed the right culture and improve retention
By improving culture, leadership and wellbeing, we will ensure up to 130,000 fewer staff leave the NHS over the next 15 years. We will:
- Continue to build on what we know works and implement the actions from the NHS People Plan to ensure the NHS People Promise becomes a reality for all staff by rolling out the interventions that have proven to be successful already. For example, ensuring staff can work flexibly, have access to health and wellbeing support, and work in a team that is well led.
- Implement plans to improve flexible opportunities for prospective retirees and deliver the actions needed to modernise the NHS Pension Scheme, building on changes announced by the government in the Spring Budget 2023 to pension tax arrangements, which came into effect in April 2023.
- From autumn, recently retired consultant doctors will have a new option to offer their availability to trusts across England, to support delivery of outpatient care, through the NHS Emeritus Doctor Scheme.
- Commit to ongoing national funding for continuing professional development for nurses, midwives and allied health professionals, so NHS staff are supported to meet their full potential.
- Support the health and wellbeing of the NHS workforce and, working with local leaders, ensure integrated occupational health and wellbeing services are in place for all staff.
- Explore measures with the government such as a tie-in period to encourage dentists to spend a minimum proportion of their time delivering NHS care in the years following graduation.
- Support NHS staff to make use of the change announced in the Spring Budget 2023 that extended childcare support to working parents over the next three years, to help staff to stay in work.
Reform – Working and training differently
Working differently means enabling innovative ways of working with new roles as part of multidisciplinary teams so that staff can spend more time with patients. It changes how services are delivered, including by harnessing digital and technological innovations. Training will be reformed to support education expansion. We will:
- Focus on expanding enhanced, advanced and associate roles to offer modernised careers, with a stronger emphasis on the generalist and core skills needed to care for patients with multimorbidity, frailty or mental health needs.
- This includes setting out the path to grow the proportion of staff in these newer roles from around 1% to 5% by the end of the Plan by:
- Ensuring that more than 6,300 clinicians start advanced practice pathways each year by 2031/32. We will support this ambition by having at least 3,000 clinicians start on advanced practice pathways in both 2023/24 and 2024/25, with this increasing to 5,000 by 2028/29.
- Increasing training places for nursing associates (NAs) to 10,500 by 2031/32. We will work towards this by training 5,000 NAs in both 2023/24 and 2024/25, increasing to 7,000 a year by 2028/29. By 2036/37, there will be over 64,000 nursing associates working in the NHS, compared to 4,600 today.
- Increasing physician associate (PA) training places to over 1,500 by 2031/32. In support of this, around 1,300 physician associates (PAs) will be trained per year from 2023/24, increasing to over 1,400 a year in 2027/28 and 2028/29, establishing a workforce of 10,000 PAs by 2036/37.
- Grow the number and proportion of NHS staff working in mental health, primary and community care to enable the service ambition to deliver more preventative and proactive care across the NHS. This Plan sets out an ambition to grow these roles 73% by 2036/37.
- Work with professions to embrace technological innovations, such as artificial intelligence and robotic assisted surgery. NHS England will convene an expert group to identify advanced technology that can be used most effectively in the NHS, building on the findings of the Topol Review.
- Expand existing programmes to demonstrate the benefits of generalist approaches to education and training and ensure that, at core stages of their training, doctors have access to development that broadens their generalist and core skills.
- Work with partners to ensure new roles are appropriately regulated to ensure they can use their full scope of practice, and are freeing up the time of other clinicians as much as possible – for example, by bringing anaesthesia and physician associates in scope of General Medical Council (GMC) registration by the end of 2024 with the potential to give them prescribing rights in the future.
- Support experienced doctors to work in general practice under the supervision of a fully qualified GP. We will also ensure that all foundation doctors can have at least one four-month placement in general practice, with full coverage by 2030/31.
- Work with regulators and others to take advantage of EU exit freedoms and capitalise on technological innovation to explore how nursing and medical students can gain the skills, knowledge and experience they need to practise safely and competently in the NHS in less time. Doctors and nurses would still have to meet the high standards and outcomes defined by their regulator.
- Support medical schools to move from five or six-year degree programmes to four- year degree programmes that meet the same established standards set by the GMC, and pilot a medical internship programme which will shorten undergraduate training time, to bring people into the workforce more efficiently so that in future students undertaking shorter medical degrees make up a substantial proportion of the overall number of medical students.
- The Plan is based on an ambitious labour productivity assumption of up to 2% (at a range of 1.5–2%). This ambition requires continued effort to achieve operational excellence, reducing the administrative burden through technological advancement and better infrastructure, care delivered in more efficient and appropriate settings (closer to home and avoiding costly admissions), and using a broader range of skilled professionals, upskilling and retaining our staff. These opportunities to boost labour productivity will require continued and sustained investment in the NHS infrastructure, a significant increase in funding for technology and innovation, and delivery of the broader proposals in this Plan.
Summary
- Hard-working staff are the bedrock of the NHS.
- However, for decades, the NHS workforce has not been planned in a co-ordinated way. This has limited our ability to best use the skills of NHS staff, the ability to set out forecasts of future need and then act on them, and being able to properly link workforce, service and financial planning to fully maximise return on investment.
- This has been a major challenge in the NHS since its inception. These challenges have combined with the impact of the COVID-19 pandemic, imposing new demands on services and pressures on staff that are unprecedented in the NHS’s history.
- The NHS was therefore commissioned by the government to produce an NHS Long Term Workforce Plan setting out future demand and supply requirements, and the actions and reforms needed to support the overall strategy for the NHS.
- This Plan sets out modelling of NHS workforce demand and supply over a 15-year period and the resulting shortfall. It details the actions that will be taken in the coming years to address the identified shortfall in addition to, and building on, actions and investment already committed over the next two years.
- It shows that, without concerted and immediate action, the NHS will face a workforce gap of more than 260,000–360,000 staff by 2036/37.
- We set out, for the first time and in the NHS’s 75th year, a comprehensive plan to close this shortfall and address the changing needs of patients over the next 15 years. It is a plan for investment and a plan for change: to train more staff, retain our dedicated workforce and reform the way we work.
- This Plan expands on the previous work and recommendations that set the direction for the NHS workforce [see references 1, 2 and 3]. In addition, it relies on valuable perspectives from over 100 stakeholders across more than 60 organisations (Annex A).
- It is the first step in a new iterative approach to NHS workforce planning. We will regularly update the model to inform operational and strategic planning, in light of changing circumstances. We will now work with NHS staff, NHS employers, clinical leaders, royal colleges, professional regulators, as well as integrated care boards (ICBs) and integrated care systems (ICSs) and others, to implement and build on the actions and ambitions set out.
The case for change
- The number of NHS staff has grown materially in the past decade. Since 2010, NHS staffing has increased by 263,000 full-time equivalent (FTE) staff, [see references 4, 5 and 6] including 42,000 more doctors and 55,000 more nurses, health visitors and midwives, with an estimated increase of 4,600 doctors and 2,400 nurses in general practice. However, healthcare need has also been growing significantly, driven by ageing and increasing morbidity, and outstripping the growth in workforce FTEs. We know the NHS is facing clear and pressing workforce challenges.
- Rising demographic pressures and a changing burden of disease are increasing demand for NHS services. Over the next 15 years, the population of England is projected to increase by 4.2%, but the number of people aged over 85 will grow by 55% [see reference 7]. Patients’ needs are changing with increasing levels of multimorbidity and frailty leading to increasing complexity of service delivery. By 2037, unless more is done to moderate current trends, two-thirds of those over 65 will have multiple health conditions and a third of those people will also have mental health needs.
- Historically, while the education and training pipeline has increased and the workforce has grown by 25% since 2010, [see reference 8] the number of staff trained has not kept pace with demand for NHS services. To fill service gaps and ensure safe staffing levels, the NHS is firmly reliant on temporary staffing and international recruitment [see reference 9]. Of the doctors who joined the UK workforce in 2021, 50% were international medical graduates [see reference 10]. And, in 2022/23, about half of new nursing registrants in England were trained overseas [see reference 11]. This leaves the NHS exposed to high marginal labour costs and risks the sustainability of services in the longer term given the growing global demand for skilled healthcare staff.
- The need for our workforce to grow and evolve is evidenced by the fact that there were over 112,000 vacancies across the NHS workforce in March 2023 [see reference 12]. Compared to other OECD countries, the UK sits below the average for numbers of nurses and medics per size of population.
- These are challenges faced by other countries across the developed world. In England, staffing shortages limit the capacity of the NHS to deliver the quantity and quality of services that people expect, impact on staff wellbeing, and hinder the NHS’s ability to reform and provide value-for-money for taxpayers.
- The current NHS workforce largely concentrates on responding to care and health needs, rather than doing more to fulfil the role it can play in preventing ill health. Likewise, we will need to continue the shift over the coming years away from episodic care, towards a newer paradigm of ongoing, chronic care to support the increasing number of people with multimorbidity, frailty and complex needs. New and emerging roles, including advanced practice, are growing but not at a sufficient rate to fundamentally alter the overall shape of the workforce. There is a growing professional consensus that meeting the needs of patients, and changing population demands, will require a more flexible workforce with more generalist and core skills, alongside specialist skills.
- The NHS Long Term Plan [see reference 13] described the changes needed for an NHS fit for the 21st century, including boosting primary and community care, investing in mental healthcare, diagnosing cancer earlier, and focusing on population health, integration and prevention. We are seeking to achieve these changes throughout the NHS in a way that learns from and builds on the experience of the COVID-19 pandemic (for example, the rapid roll out of telemedicine systems across primary care), recognising the long-lasting impact on the NHS. Scaling of NHS care delivered in the community requires rapid expansion of the necessary workforce and the development of more flexible and integrated teams.
- NHS staff, learners and volunteers do not always have an equally good experience of work in the NHS. The NHS workforce is the most diverse it has ever been; for example, nearly 25% of staff come from an ethnic minority background [see reference 14]. We want everyone working in the NHS to have a positive experience, but we recognise this is not always the case.
- Developments in science, research, technology, digital and data will continue. Genomics and artificial intelligence (AI) in particular will transform our ability to prevent, diagnose, treat and manage disease, supporting a shift towards better prevention of disease and more personalised care outside hospital. Harnessing these opportunities requires NHS staff to continue to build digital skills and capabilities and will change ways of working, releasing staff time to focus on patient care. With strong local leadership and management, combined with enabling technology, the use of more diverse roles will change the skills required to meet patient needs and will expand the capacity of community services to deliver this type of care.
- Given the unique challenges facing the NHS workforce and the length of time it takes to train new clinical staff (particularly new consultants and GPs), a comprehensive and long-term approach to workforce planning is required.
Putting the workforce on a sustainable footing for the long term
- Over the course of the Plan, concerted action will need to continue, supported by increased investment to expand education and training, as well as increasing recruitment from the wider labour market. Action will need to be sustained across improving culture and retention, training the workforce differently, evolving the skills mix and delivering productivity. The Plan assumes an ambitious labour productivity assumption of 1.5–2%. This ambition requires a combination of delivering care closer to home while avoiding costly admissions, achieving operational excellence, reducing administrative burden through better technology and infrastructure, and capturing the benefits appropriately in productivity measurement. The productivity ambition will require continued and sustained investment in the NHS infrastructure, a significant increase in funding for technology and innovation, and the delivery of the broader proposals in this Plan.
- The ongoing speed and scale of action in each area will determine how quickly workforce shortfalls can be closed, services can be reshaped and the NHS’s dependence on international recruits and temporary staffing can be scaled back.
- The modelling used throughout the Plan provides a set of broad ranges to quantify the potential impact of actions over its 15-year timeframe. The suggested impact is inevitably subject to a degree of uncertainty.
Figure 1: Drivers of NHS workforce demand and supply in 2021/22 and as projected for 2036/37, FTEs 000s
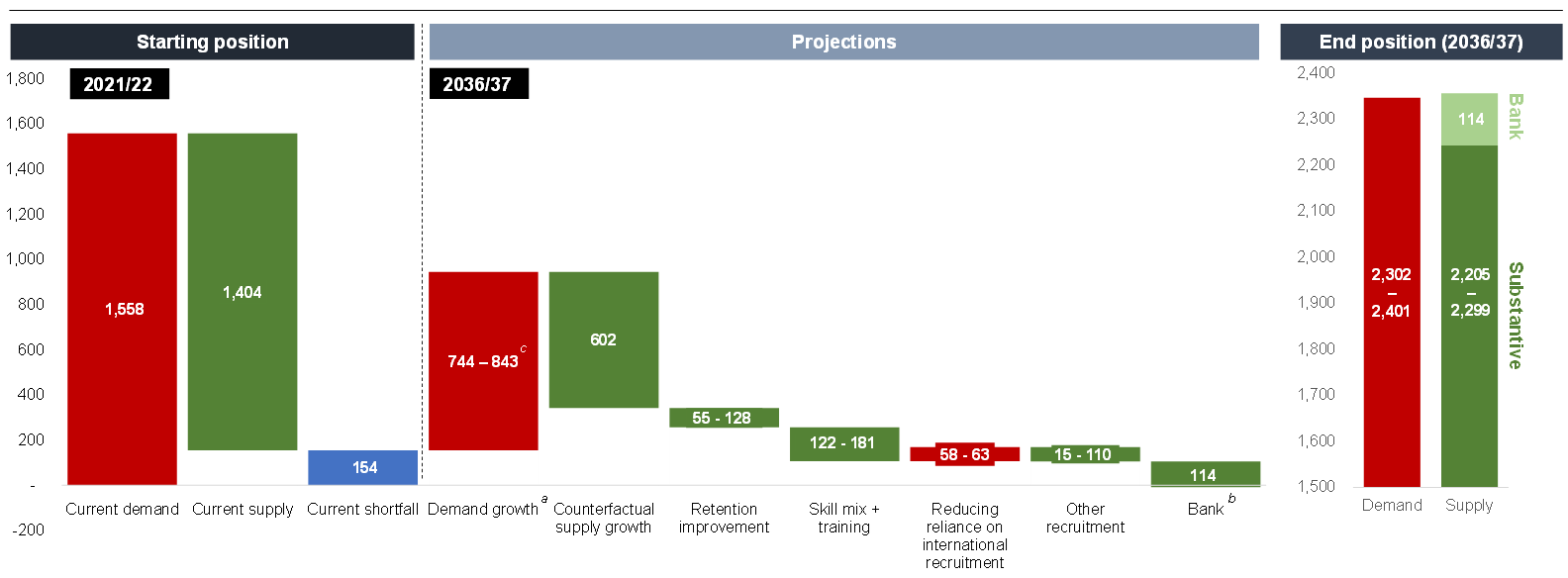
a) Demand growth is net growth, once taking into account workforce required to improve performance, service and pathway reforms to deliver care in the most appropriate setting, mitigating demand growth through prevention and proactive care, and productivity improvement.
b) This assumes that the proportion of NHS staff who choose to work solely on bank contracts will stay the same.
c) Ranges are driven by different assumptions used in the modelling to reflect uncertainty in key factors, including productivity (which impacts on demand), retention, training, and the estimated levels of education and international recruitment required to reduce staff shortfalls, and the broader recruitment required to meet demand. These are further set out in Annex B.
- The modelling estimates that the starting shortfall between demand and supply for NHS staff is approximately 150,000 full-time equivalents (FTEs), a gap that is filled with temporary staffing. Before any of the interventions set out in this Plan, and even after factoring in ambitious expectations for improved productivity, the workforce shortfall across NHS organisations will grow to 260,000–360,000 FTEs by 2036/37. Most professions will see shortfalls grow, but this trend will be more pronounced for some professions.
- The shortfall in qualified GPs is projected to be 15,000 FTEs by 2036/37. The model assumes a boost in doctors in GP specialty training and newly qualified GPs from interventions in recent years, but more will be needed to keep up with expected demand.
- By 2036/37 the FTE shortfall in community nurses will be at least 37,000; it was 6,500 in 2021/22. The mental health nursing and learning disability nursing shortfall will grow to more than 17,000 FTEs, while that for critical care nurses will remain at around 4,000 FTEs.
- Among the allied health professions (AHP), shortfalls will increase the most for paramedics, occupational therapists, diagnostic radiographers, podiatrists, and speech and language therapists.
- Within the non-registered workforce, healthcare support workers are anticipated to have the largest shortfall.
Longer term assessment of actions needed to support change
- Even with the highest projected impact of retention and productivity, there will be a workforce shortfall and significant reliance on international recruitment at the end of 2036/37 under current trends without further investment in education and training. We will therefore need to grow our workforce; our long-term assessment is that domestic education and training needs to expand by around 50% to 65% over the next 15 years.
- To meet the growth needed in the future, NHS organisations will need to do more to recruit staff from the wider labour market, particularly into direct entry and support worker roles. The Plan estimates that more than 204,000 new support workers will be required to meet demand over the next 15 years. The detailed actions to grow the workforce are set out in Chapter 2.
- The collective impact of proposed actions to embed the right culture and improve retention, aligned to increases in capacity, would help reduce the number of NHS leavers by between 55,000 and 128,000 FTEs over the 15-year timeframe. Chapter 3 sets out the detail of what systems, NHS England and our partners will need to focus on to make this a reality over the longer term.
- Increasing capacity and working differently is anticipated to reduce projected shortfalls and improve labour productivity. Chapter 4 sets out the case for taking full advantage of digital and technological innovations, such as speech recognition, robotic process automation, remote monitoring and AI. Building on the Topol Review, [see reference 15] NHS England and government, will convene an expert group to ensure the NHS takes advantage of the opportunities that AI can offer. Chapter 4 also outlines the training reforms needed to support the expansion set out in the Plan and discusses the need for NHS workforce plans to offer modernised careers, with a stronger focus on the generalist and core skills needed to care for patients with multimorbidity, frailty or mental health needs.
- With the combined impact of interventions on productivity improvement, retention, recruitment, the adoption of new roles, training and education, the shortfall is expected to fall over the modelled period. It is anticipated that, while shortfalls persist, they will continue to be largely covered by use of temporary staffing, including a mixture of bank and agency. The position for individual professions varies.
Education and training expansion
- As a first and significant step, this Plan commits to a new suite of actions over the next six years to support and develop the NHS workforce with an immediate boost in training numbers.
- The government will invest more than £2.4 billion to fund the 27% expansion in training places by 2028/29. This will enable more than half a million trainees to begin clinical training over the next six years, an addition of nearly 60,000 compared to maintaining current training levels. This is a significant first step on the path to increasing education and training by 64% by 2031/32. As part of this ambition, we aim to:
- Double the number of medical school places, taking the total number of places to 15,000 by 2031/32. We will work towards this expansion by increasing medical school places by a third, to 10,000 by 2028/29. We will also ensure there is adequate growth in foundation placement capacity, as those taking up these new places begin to graduate, and a commensurate increase in specialty training places that meets the demands of the NHS in the future. We will work with stakeholders to ensure this growth is sustainable and focused in the service areas where need is greatest.
- Increase the number of GP specialty training places by 50% to 6,000 by 2031/32. To support this ambition, GP specialty training places will initially grow by 500 places by 2025/26, increasing to 1,000 additional places (5,000 overall) by 2027/28.
- Increase adult nursing training places by 92%, taking the total number of places to nearly 38,000 by 2031/32. We will work towards this ambition by increasing adult nursing training places over the next six years so that, in 2028/29, at least 8,000 more adult nurses will start training compared to current levels. Over this same time period, to 2028/29, training places will increase by 38% for mental health nursing and 46% for learning disability nursing. By 2028/29, there will be a total of 40,000 nursing places funded. This will put us on the path to increase nursing training places by 80% to over 53,500 by 2031/32.
- Increase training places for nursing associates (NAs) to 10,500 by 2031/32. In support of this, over the coming six years, we will increase training places by 40% to 7,000 by 2028/29.
- Increase AHP training places to 17,000 by 2028/29, putting us on the path to increasing places overall by a quarter to more than 18,800 by 2031/32.
- Increase training places by 26% for both clinical psychology and child and adolescent psychotherapy by 2031, taking the combined number of training places to over 1,300. Training places will be more than 1,000 each year up to 2028/29.
- Expand training places for pharmacists by 29% to around 4,300 by 2028/29. This will put us on the path to increasing training places by around half overall to almost 5,000 by 2031/32. The number of pharmacy technicians will also grow in future years.
- Increase training places for dental therapists and hygiene professionals to more than 500 by 2031/32, and increase training places for dentists by 40% to more than 1,100 by this same year. In support of this, we will increase training places for dental therapy and hygiene professionals by 28% by 2028/29, with an increase of 24% for dentists to 1,000 places over the same period.
- Increase training places for healthcare scientists by 13% to more than 850 places by 2028/29, putting us on the path to increase training places by more than 30% to over 1,000 places by 2031/32.
- Expand advanced practice training by 46%, so that 5,000 clinicians are starting advanced practice pathways each year. This puts us on the path to increasing training places so that more than 6,300 clinicians start advanced practice pathways each year by 2031/32.
- Provide 16% of clinical training places as apprenticeships by 2028/29 compared to 7% now. This will offer greater access to training opportunities for local communities and put us on the path to offering 22% of clinical training places through apprenticeship routes by 2031/32.
- These actions build on the steps that NHS England is already taking to grow and train the NHS workforce. Investment in education and training is planned to increase from £5.5 billion to £6.1 billion over the next two years, and actions are underway to:
- Train 5,000 nursing associates (NAs) and around 1,300 physician associates (PAs) in 2023/24 and 2024/25. This Plan emphasises the need to target more PA roles towards primary care and mental health services.
- Ensure at least 3,000 clinicians start advanced practice pathways in both 2023/24 and 2024/25, tailored to support service demand.
- Continue funding the shortened midwifery course for registered nurses in 2023/24 and 2024/25.
- Complete the planned increase in medical specialty training places by September 2024 to more than 2,000 over three years, as well as 1,000 additional specialty training places focusing on areas with the greatest shortages. This expansion is both supporting existing planned growth for mental health, cancer and diagnostic services, as well as elective recovery, urgent and acute care, maternity services and public health medicine.
- These actions are on top of progress already made over recent years including:
- Growth in medical training places since 2018 – a 25% increase from 6,000 to 7,500.
- Growth in GP specialty training places (with over 4,000 doctors accepting GP specialty training places in 2022, compared to 2,671 in 2014), which is beginning to increase frontline capacity.
- Investment in additional direct patient care staff in primary care, with over 29,000 FTE staff in post now compared to March 2019 [see reference 16].
- Progress towards growing the permanent nursing workforce by 50,000 with over 44,000 more nurses working in the NHS in March 2023, compared to September 2019, [see references 17, 18].
- A 13% planned increase in the number of midwives in training by 2024/25, compared to 2021/22.
- Substantial changes by the government in the Spring Budget 2023 [see reference 19] to pension tax arrangements (from April 2023), which ensures that experienced clinicians are not pushed out of the workforce for tax reasons and alleviates disincentives for taking on additional work or responsibilities.
- The extension in the Spring Budget 2023 [see reference 20] of childcare support to working parents over the next three years, which will support NHS staff to stay in work and increase participation rates (the proportion of a full-time role individual staff members can fulfil).
Impact of the NHS Long Term Workforce Plan
- Implementing this Plan will have a significant impact on the NHS workforce of the future, and the delivery of care for patients.
- Staff shortfalls would fall significantly by 2028 and would continue to fall, with sustained investment in education and training in line with this Plan, at a steadier rate over the rest of the modelled period, which means we will be materially reducing the NHS’s reliance on agency staff.
- With full implementation over the longer term, the NHS total workforce would grow by around 2.6–2.9% a year, with an expansion of the NHS permanent workforce from 1.4 million in 2021/22 to 2.2–2.3 million in 2036/37, including an extra 60,000–74,000 doctors, 170,000–190,000 nurses, 71,000–76,000 allied health professionals (AHPs), and 210,000–240,000 support workers alongside the expansion of new roles such as physician associates and nursing associates, and greater use of apprenticeships. If the Plan is fully implemented, by 2036/37, this will be equivalent to the number of nurses per 1,000 population growing to around 9.5, and the number of doctors per 1,000 population growing to around 4.3, in the NHS in England.
- A higher proportion of new joiners to the NHS workforce would come from domestic routes rather than from overseas and, within those, a greater proportion would train via apprenticeship routes. In 15 years’ time, we expect around 9–10.5% of our workforce to be recruited from overseas, compared to nearly a quarter now.
- Leaver rates would improve by around 15% over the course of the Plan, and retention will be at rates better than the average pre-pandemic.
- The NHS would be enabled to improve productivity, overcoming the impact from COVID-19, and improve to a level above the historical trend, with sustained and continued investment in workforce, technology, infrastructure and innovation.
Scope and key considerations
- We recognise that the challenges described are not unique to the NHS, and the NHS does not operate in a vacuum. There are many different factors outside the NHS’s control that impact on the demands it experiences.
- Pressure in social care, which impacts patient flow through the healthcare system and builds demand by increasing the burden of disease and complexity of conditions over the longer term.
- However, this Plan focuses on the workforce employed by the NHS and delivering NHS-funded services in NHS trusts and primary care. We recognise that people’s careers can span health and social care, and factor into the proposals that staff in the private, social care, social enterprise and voluntary sectors are critical to the overall provision of services and delivery of the best and most appropriate care for the population [see references 21, 22, 23, 24].
- This Plan’s actions are interdependent. For example, retention and productivity cannot improve to the degree this Plan projects without increasing the size of the workforce and the capacity of the NHS. Likewise, it is not exhaustive. The Plan does not cover every action needed to support workforce development across the NHS over the next 15 years. Rather, it is the first step in regular planning that will evolve and develop in line with service need.
- Beyond core terms and conditions, which are outside the scope of this Plan, we will need government to support this Plan by providing the necessary continued and sustained investment in infrastructure, reforming education funding and strengthening social care provision on which the success of this Plan depends.
- Infrastructure – Significant training expansion and workforce growth are only possible if there is sufficient physical capacity for staff to be trained in and work in. Labour productivity is dependent on the quality and capacity of physical and digital infrastructure. Government has invested in the New Hospital Programme, community diagnostic centres and surgical hubs. Building on these, continued and sustained investment in NHS estate and equipment, including in primary care and a rolling new hospital programme, will be critical to achieving the labour productivity ambitions in this Plan. It also requires sustained investment in technology and digital innovation to modernise the environment NHS staff work in.
- Education funding – NHS England and the Department of Health and Social Care (DHSC) are working together to reform the funding of healthcare education and training provided nationally in England to ensure accountability, transparency and the best return on the additional investment set out as part of this NHS Long Term Workforce Plan.
- Social care provision – Health and care services are interdependent, and if efforts in this Plan to tackle the current challenges in the NHS are to yield success, then capacity needs to increase across both [see reference 25]. This Plan is predicated on access to social care services remaining broadly in line with current levels or improving. The government set out a vision for adult social care reform in the December 2021 white paper, [see reference 26] and allocated additional funding to support this. Earlier this year, an update was published which focused on improving the quality and accessibility of care [see reference 27].This confirmed funding of £250 million for workforce recognition and career development, including funding for continued professional development for registered nurses and other regulated professionals, and guiding principles to enable safe and effective delegation of healthcare activities to care workers.
- While the Plan’s model is founded on data, evidence and analysis, its projections are made with assumptions that are, by their nature, subject to a degree of uncertainty. This is unavoidable for any modelling over a 15-year timeframe. It is also dependent on decisions made by organisations outside the NHS; for example, local authorities that commission NHS services. To avoid a misleading impression of precision, the assumptions are often applied uniformly, without necessarily differentiating between geographical areas and, in some cases, professions and projections are reflected as ranges. We have, however, assessed community pharmacy and dental demand and supply separately, taking account of the unique circumstances in these settings. The model, and ranges presented, should be treated as strategic insights to inform policy choices relating to training, education, recruitment and retention.
- We will continue to develop the model and Plan, publishing a refreshed projection every two years, or aligned with fiscal events as appropriate.
- While we recognise the need for continued growth, this Plan does not cover the demand and supply of medical specialties, except for where these are already planned. This is partly because the available data is not yet sufficiently granular to give a clear enough picture for all specialisms to enable highly detailed national decisions on specialist workforce planning. It also reflects that it is incredibly difficult to predict which specialist roles will be most in demand in 15 years’ time, particularly where further work is needed to consider a future shift towards a more flexible specialist workforce. As this Plan is iterated, the objective is to establish the data and methodologies to enable a view to be formed with a richer and more granular range of information from across the NHS.
Next steps
- The Plan builds on the changes already happening in the NHS to have more people, working differently, in a compassionate and inclusive culture. The Plan sets out actions the NHS will begin implementing now, alongside proposals about how to close the anticipated staffing shortfalls in the longer term. We will work with government, stakeholders and local health systems to put the workforce on a sustainable footing to meet patients’ needs for the long-term.
- The merging of Health Education England, NHS Digital and NHS England has provided the opportunity to align and co-ordinate planning and action in the short and long term, so we can have the greatest possible collective impact for staff and, by extension, patients and citizens. In line with NHS England’s operating framework, [see reference 28] NHS England has an important role by providing co-ordinated support to equip systems to lead and innovate.
- This Plan is therefore intended to be the start of an ongoing programme of work that becomes an established part of how the NHS plans for, and delivers, its services for patients and the public. It is crucial we embed an integrated approach to planning and delivery, bringing together workforce planning with service and clinical strategies and financial planning for the long term, so we have a sustained and responsive approach that reflects changes in demand, services and wider factors. Following publication, we will continue to work with system leaders and stakeholders to refine the detail of the actions, and to support effective implementation and delivery of the ambitions in the Plan.
1. The case for change
- The size and shape of the NHS workforce need to change to meet patient need now and in the future. When a person turns to the NHS for help, it needs to have enough people with the right skills, and in the right place, to meet their needs.
- Rising demographic pressures and a changing burden of disease mean that demand is increasing and will be further impacted by the development in our ability to treat disease in areas like cancer or obesity. Maintaining the current size of the workforce, and the skills mix within, will not be sufficient to deliver the care needed in the future. Over the next 15 years, the population of England is projected to increase by 4.2%, but the number of people aged over 85 is projected to increase by 55% [see reference 29]. The use of health and social care resources rises rapidly with age. Between 25% and 50% of people aged over 85 will have frailty, compared to around 10% over 65 [see reference 30]. Average (public) health spending was five times greater for an 85-year-old than for a 30-year-old in 2015, [see reference 31] and for every 10 years beyond the age of 70, the risk of admission for an inpatient episode rises rapidly [see references 32, 33].
- People experiencing health inequalities develop long-term conditions earlier, accumulate them faster and live with them longer. This leads to a loss of productivity and higher healthcare expenditure. Stark variations in healthy life expectancy (HLE) exist; at birth for boys in the most deprived areas it is 52.3 years, compared with 70.5 years in the least deprived areas. Likewise for girls, HLE is 51.9 years and 70.7 years for the most and least deprived areas respectively (2018–2020 data), [see reference 34]. The proportion of patients with multimorbidity (two or more health conditions) is steadily rising and in higher income countries this increase is largely, but not exclusively, linked to age [see reference 35]. The increase in demand from an ageing population is not uniform across the UK, but concentrated outside metropolitan areas and in particular rural areas [see reference 36, 37. In 2037, a third of people aged over 85 will be living in rural communities like Cornwall, Somerset, Cumbria and North Yorkshire, compared to a quarter now. On current trends, two-thirds of those over 65 will have multiple health conditions, and a third of those people will also have mental health needs. We are also seeing more people from younger cohorts with multimorbidity, likely associated with low socio-economic status and deprivation, [see reference 38]. Multimorbidity challenges the specialised approach to medicine, which has improved our ability to successfully treat single diseases. As we move forward, we will increasingly need medical and other clinical professionals with generalist and core skills to manage and support patients with seemingly unrelated diseases. Additionally, government intends to publish a new major conditions strategy that will aim to improve prevention, diagnosis and treatment of six major conditions (cancer, cardiovascular diseases including stroke and diabetes, chronic respiratory diseases, dementia, mental ill health, musculoskeletal disorders).
- There is a clear need for the NHS workforce to continue to grow and evolve. There were over 112,000 vacancies across the NHS workforce in March 2023 (an 8% vacancy rate) but with significant variation across regions and professional groups. Moreover, vacancy data might even underestimate the true staff shortfall across the NHS. There is no perfect measure of workforce shortage at the national level currently. Vacancy statistics do not reflect the fact that in some instances temporary staffing will be deployed even where there are no recorded vacancies. The NHS employs 1.6 million people [see references 39, 40] and around a further 286,000 are training in the service at any given time [see reference 41]. The NHS workforce has seen significant growth since 2010 and has grown by 12% in the last three years [see references 42, 43]. However, only 26.4% of respondents to the 2022 NHS Staff Survey said there were sufficient staff in their organisation for them to do their job properly – a 11.9 percentage point decline from 38.3% in 2020 [see reference 44].
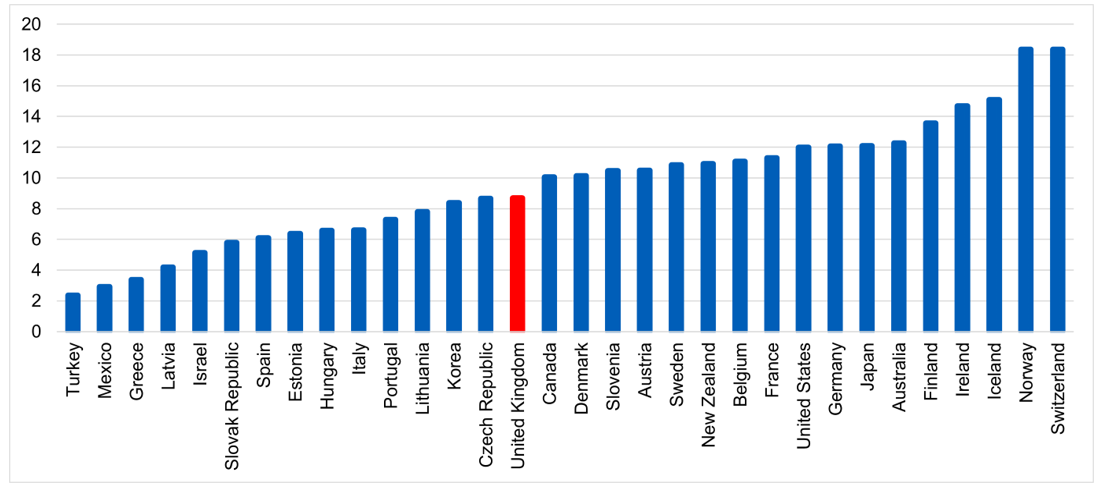
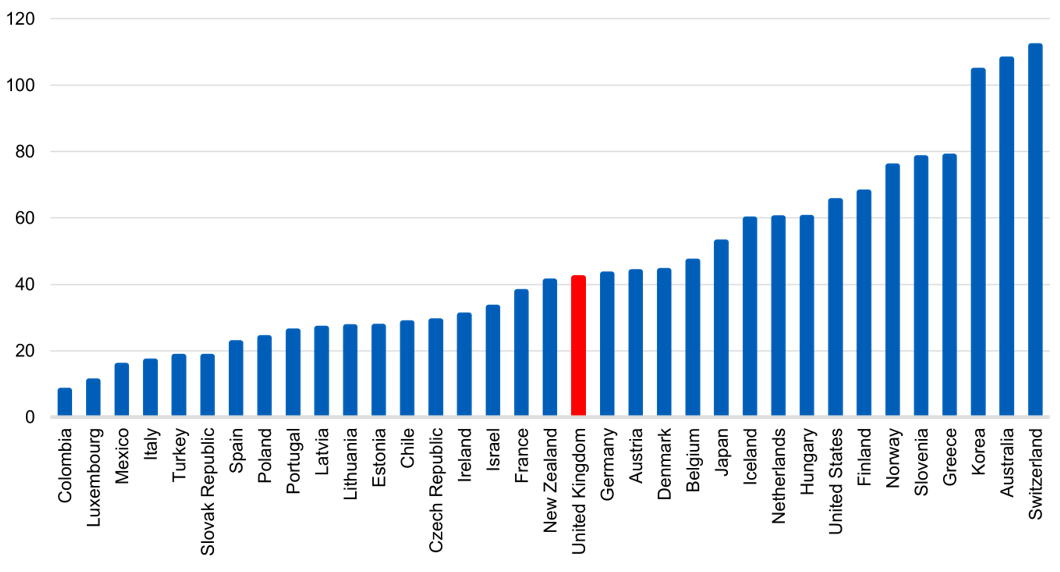
- Compared with other health systems internationally, the UK sits below the OECD average for the number of practising doctors as a proportion of the population [see reference 45] and we have fewer GPs per 1,000 population compared to most other OECD countries [see reference 46]. The UK has fewer than half the number of practising nurses compared to Norway and Switzerland, while Germany and Australia have 39% and 41% more nurses respectively (per 1,000 population), [see reference 47]. Global trends demonstrate that the health and care workforce is increasing as a proportion of total population across OECD countries and other international comparators, reflecting the changing demographic structure across comparable countries, [see reference 48]. Due to key factors such as differing health system types and structures, different skills mix models, variations in education and training and differences in statistical and regulatory arrangements, these comparisons should be interpreted cautiously and with recognition of these differing contexts. These comparisons are however helpful as an indication of possible similarities, differences and opportunities for learning.
Figure 2: Practising doctors per 1,000 population, 2021 (or latest available)
Data extracted May 2023
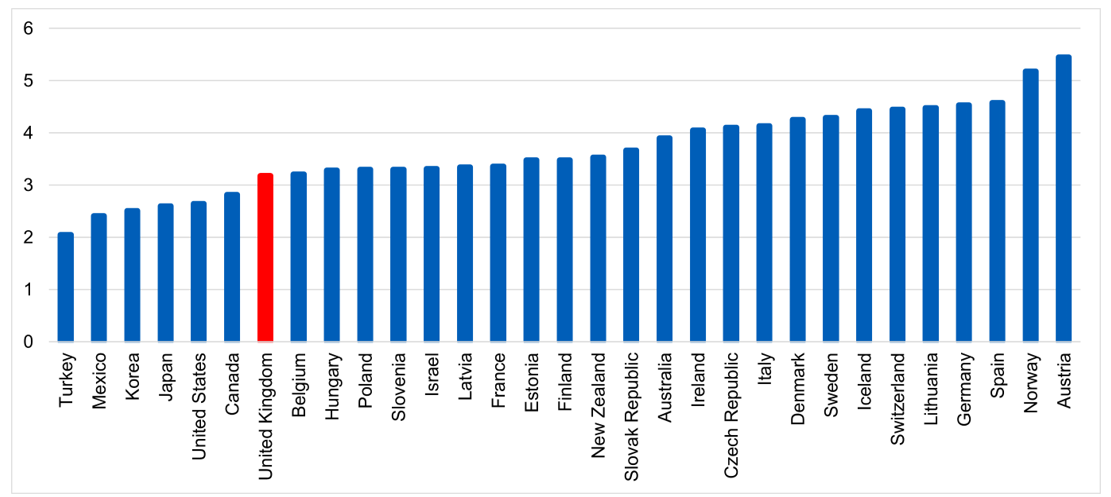
Figure 3: Practising nurses per 1,000 population, 2021 (or latest available)
Data extracted May 2023
- Historically, over decades, growth in NHS services has not been matched by investment in the education and training pipeline. Despite increases in recent years, the UK sits below many other developed countries in terms of the number of people trained per size of population.
Figure 4: Medical graduates per 100,000 population, 2021 (or latest available)
Data extracted May 2023
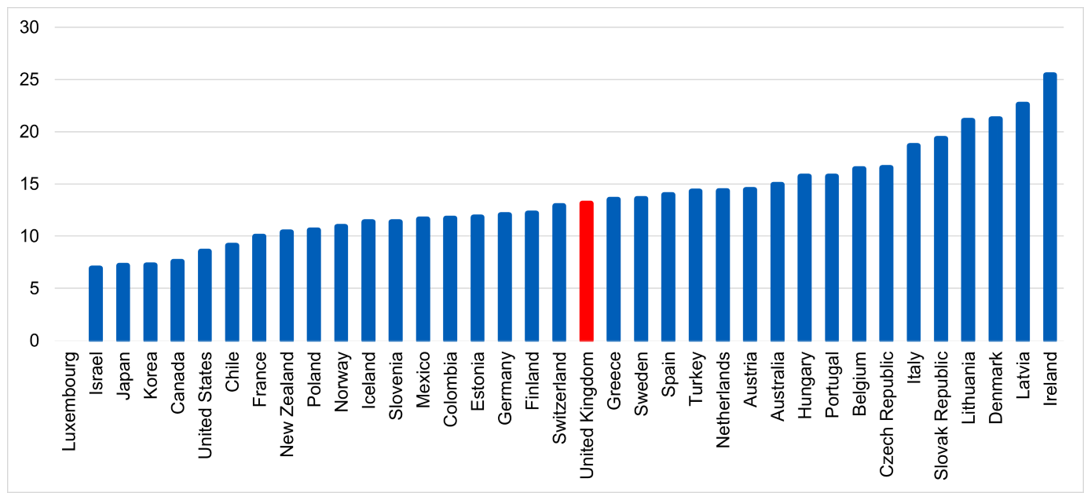
Figure 5: Nursing graduates per 100,000 population, 2021 (or latest available)
Data extracted May 2023
- Attracting and retaining a highly engaged workforce is becoming more challenging and the NHS is operating in an increasingly competitive labour market. The COVID-19 pandemic saw NHS staff go above and beyond to care for patients, and during this time the number of staff leaving the service was low. However, this trend is now reversing. Notably, healthcare services are competing with other sectors of the economy to attract and retain staff. Staff in lower paid, direct entry positions – clinical and non-clinical – can often transfer relatively easily into other jobs in the economy with better pay, and greater flexibility and benefits.
- To fill service gaps and ensure safe staffing levels, the NHS has relied too much on temporary staffing. Over the three years up to 2021/22, expenditure on bank and agency staff has increased by 51% (from £3.45 billion to £5.2 billion) and 23% (£2.4 billion to £2.96 billion) respectively, reflecting some of the challenges of responding to the COVID-19 pandemic [see reference 53]. Use of agency staff is expensive and offers poor value for money for the taxpayer. There is also increasing evidence that use of temporary staffing – particularly agency staff – can negatively impact on patient and staff experience, and continuity of care [see reference 54].
- The NHS is particularly reliant on international recruitment to fill workforce gaps and deliver patient care in comparison to other healthcare systems globally [see reference 55]. The total proportion of NHS workers with non-UK nationalities (across all professions) has grown to over 17% (although there is significant variation between regions and staff groups), [see reference 56]. While employing international graduates supports the sharing of global learning and skills, and all international colleagues are highly valued, recent data shows a 2% increase in UK trained medical graduates joining the workforce since 2017, compared to a 121% rise in international medical graduates, [see reference 57]. International recruitment has supported necessary increases in some staff groups, such as doctors and nurses, but does not offer a universal solution to rising workforce demand; for some professions where scope of practice differs from England (for example, community nursing, mental health nursing, learning disability nursing, oncology and podiatry), overseas recruitment is not a readily available option.
- A heavy reliance on overseas staff leaves the NHS exposed to future global shocks and fluctuations in international workforce supply. The COVID-19 pandemic highlighted the fragility of using international recruitment to plug workforce shortages, and any future global shocks such as pandemics, armed conflicts and climate change may present similar challenges. The international healthcare labour market is likely to become increasingly competitive as healthcare systems around the world face increasing demand. It is estimated that between 2015 and 2050, the proportion of the world’s population over 60 years will nearly double from 12% to 22%, and that by 2050, 80% of older people will be living in low- and middle-income countries [see reference 58]. This will drive up global demand for healthcare staff, making it more challenging to recruit from overseas. Other countries such as Canada and the USA do not currently rely on international recruitment to the same extent as the NHS.
However, any change in the workforce requirements of those countries could constrain the NHS’s ability to compete internationally, [see reference 59] particularly if they offer better opportunities for pay or quality of life, limiting the NHS’s competitive advantage.
- Demographic changes will present some opportunities when it comes to recruiting to the future healthcare workforce. There will be a ‘bulge’ in the 18- year-old population over the next few years, which possibly will not be seen again for the rest of the century [see reference 60]. As such, there is an imminent narrow window to offer as many routes as possible to school leavers into careers in healthcare.
- The current NHS workforce largely concentrates on responding to care and health needs rather than prevention. The NHS Long Term Plan [see reference 61] identified the service changes needed to deliver an NHS fit for the 21st century. These include boosting primary and community care, focusing on population health, integration and prevention, investing in mental healthcare, diagnosing cancer earlier and making sure everyone with cancer has access to a clinical nurse specialist or other support worker, and having an efficient NHS focused on outcomes. However, according to OECD data, in the UK, more healthcare spending is allocated to hospital services than its peers, and less to preventative medicine, residential and outpatient care [see reference 62]. We also know that the overall balance of the NHS workforce has remained somewhat resistant to change in recent decades. For example, the number of full-time equivalent (FTE) nurses working in adult hospital nursing grew by almost 4.6% in the year to February 2023, while the number working in community nursing grew by 2.7% [see reference 63]. In other words, NHS resources are being used to treat an increasingly sick population, with a declining proportion being used to prevent people from becoming unwell in the first place. The UK has one of the highest admission rates for asthma and chronic obstructive pulmonary disease, for example [see reference 64]. Beyond meeting patient needs and expectations, the current skills mix within teams could better optimise productivity and value, and empower more existing staff to use their full scope of practice.
- New and emerging roles are growing but not at a sufficient rate to fundamentally alter the overall shape of the workforce. In future, healthcare teams will continue to be led by clinical experts, but wider skills will be needed to help offer personalised, responsive care to patients, supporting them to be independent. This may involve digital monitoring of remote care and coaching to help patients manage their health, as well as expert practitioners to support rehabilitation, and drive care planning and decision-making. In addition to providing better care for patients, broader multiprofessional teams will mitigate some of the challenges in recruiting to traditional workforce roles.
- Upskilling the workforce and offering opportunities for enhanced, advanced and consultant practice will help retain NHS staff delivering clinical care, grow the total number of senior clinical decision-makers and enable the delivery of better patient care. Traditional career structures for healthcare professionals can be too rigid, with some staff opting to leave clinical practice because they feel they cannot progress their careers. Associate and support roles across professions will also help widen access to NHS careers, with a particular emphasis on apprenticeships and targeted recruitment, supporting a diversity of new entrants who reflect the communities we serve. As the number of skilled roles within the existing workforce increases, a parallel focus will be needed on recruiting to entry level roles to maintain balanced teams.
- The impact of COVID-19 is still affecting delivery, and this is likely to be one of the biggest challenges for NHS recovery over the coming years. The pandemic caused long-lasting disruption to NHS services, resulting in additional demand on the workforce while constraining the NHS’s ability to deliver care for patients. Various contributing factors had an impact, including the direct effects of managing COVID-19, delays to discharge and longer non-elective length of stay (therefore constraining elective capacity), and higher staff sickness and absence. Comparable pressures are being seen in mental health services. The proportion of adults experiencing depression almost doubled during the pandemic [see reference 65]. By June 2022, there were 1.23 million people waiting for their second contact from a mental health service and there are increasing needs of children who require NHS mental healthcare [see reference 66].
- These challenges are not unique to the NHS. The adult social care sector in England employs around 1.5 million people, with a further 165,000 posts currently vacant [see reference 67]. Care workers make up most of the adult social care workforce; they are less well paid on average than people performing equivalent roles in the NHS [see reference 68] and are leaving at rates higher than they are replaced [see reference 69]. There are also fewer nurses in the sector compared to 10 years ago and Skills for Care estimates that 44% of nurses in adult social care left their role in 2021/22, [see reference 70]. While putting in place mitigations and increasing the number of staff working in direct entry roles will form a critical part of this Plan, this should not come at the expense of exacerbating workforce shortages that exist elsewhere in the social care sector.
- Pressures in adult social care directly impact on the NHS. Workforce challenges in adult social care mean that meeting people’s physical and mental healthcare needs at home or in the community is challenging, leading to poorer health outcomes and increased likelihood of hospital admissions. They also contribute to delayed discharges, which impacts on the wider health system.
- The introduction of integrated care partnerships provides a unique opportunity. NHS systems and local authorities will be able to work more effectively together to provide integrated care that meets the health and wellbeing needs of the population they serve. This will include integrated workforce planning to best develop and deploy staff; for example, through opportunities for joint teams, joint training and rotation between NHS and social care settings. This will be important for services like public health, which improve population health and prevent ill health, and are vital as the population becomes sicker and has greater healthcare needs. Workforce planning, development and training for public health areas such as sexual and reproductive health and alcohol and drug treatment should benefit from improved joint working between ICBs and local authorities.
- Developments in science, research, technology, digital and data will continue. The evidence available suggests developments such as genomics and artificial intelligence (AI) will transform our ability to prevent, diagnose, treat and manage disease, supporting a shift towards better prevention, health and wellbeing, and more personalised, empowered care [see references 71, 72]. To deliver the benefits of these advances, we need to upskill the workforce with core skills and increase the number of expert roles across digital, genomics and personalised care. The use of more diverse roles and skills, combined with enabling technology, will lead to more care being delivered remotely, closer to home or in the community, such as in virtual wards, and will enable more teams to work across organisational boundaries.
- Developments in AI may increase productivity by giving the workforce ‘the gift of time’, [see reference 73] as more routine tasks are automated, augmenting rather than replacing clinical professions. These advances will not materially lessen the need for staff overall but, combined with a greater focus on prevention, could help reduce the forecasted rate of growth in workforce demand.
- Upskilling the workforce is key to unlocking the potential of science, research and technology to deliver the care of the future. There is a growing convergence between what people say they want (more personal, preventative and productive care), the advancements to make this possible, and the collaborative place-based systems to deliver it. With the right capacity and skills, NHS staff will be able to make this a reality.
- Staff want to work in multiprofessional teams, with time to provide personalised, proactive care to patients. The 2022 NHS Staff Survey [see reference 74] results demonstrated that while progress has been made in key areas, the impact of the COVID-19 pandemic and long running trends such as workload pressures mean there is still a lot of work to do together to make the ambitions of the NHS People Promise [see reference 75] a reality for everyone.
- We must do more to ensure staff, learners and volunteers have equal opportunity within a compassionate and inclusive culture. We know having a diverse workforce will enable us to provide better care for our diverse patient groups and reduce inequalities. The NHS workforce is more diverse than at any other point in its history and we want everyone to have a positive experience working in the NHS, but we recognise this is not always the case. Progress has been made in some areas. For example, ethnic minority representation at very senior manager level in NHS trusts has increased from 7.9% in 2020 to 10.3% in 2022, and in 2022 13.2% of NHS trust board members were from an ethnic minority background compared to 10.0% in 2020, as reported in the NHS Workforce Race Equality Standard [see reference 76]. However, there is still much to do. Higher levels of disabled staff experience bullying, harassment or abuse from managers, and women tend to have worse experiences than men related to harassment, discrimination from a manager and equal opportunities for progression [see reference 77]. White applicants are 1.54 times more likely to be shortlisted for a job compared to applicants from ethnic minority backgrounds [see reference 78]. NHS staff who are LGBT are still much more likely to face physical violence, bullying and harassment in their workplace than other staff [see reference 79].
The scale of the challenge
- The NHS Long Term Workforce Plan offers an approach to project our potential staffing needs for the short, medium and long term and better understand the scale of the challenge to come over the next 15 years. This will inform national policy decisions about how to ensure the NHS can sustainably meet the needs of patients.
- After factoring in ambitious expectations for improved labour productivity (above the long-term trend), our assessment is that, with no further intervention, the shortfall will grow to 260,000–360,000 FTEs by 2036/37.
- Most professions will see current shortfalls grow without the interventions in this Plan, but there will be notable shortfalls:
- Within medical staffing, the model assumes some boost in GP numbers as a result of interventions in recent years, but the projected growth over the long term fails to keep up with expected demand. In 2022/23 the overall FTE GP workforce (including GPs in training) grew by 1.4%; however, there were 512 (1.8%) fewer FTE fully qualified GPs in April 2023 compared to April 2022 [see reference 80]. The shortfall in fully qualified GPs is projected to be around 15,000 by 2036/37 without intervention.
- Among nursing staff, by 2036/37 there will be a 37,000 FTE shortfall in community nurses compared to a 6,500 FTE shortfall in 2021/22. The current shortfall in mental health nursing is of particular concern, with the greatest vacancy rates in inpatient services, impacting on patient safety and quality of care. The total mental health nursing shortfall will reach 15,800 FTEs in 2036/37. The learning disability nursing shortfall will grow to 1,200 FTEs and for critical care nurses it will be 4,200 FTEs in 2036/37, up from 3,800 FTEs now. This is due to fewer nurses taking up training and education in these areas and limited opportunities to fill the domestic shortfall with international recruitment.
- Among the allied health professions (AHPs), the greatest shortfalls will be seen for podiatrists, paramedics (and ambulance technicians), occupational therapists, diagnostic radiographers and speech and language therapists (both adult and child), with limited supply growth projected. This is due to the education and training pipeline not keeping pace with expected demand.
- Within the non-registered workforce, healthcare support workers are anticipated to have the largest shortfall between demand and supply. This is driven by limited supply growth and a high leaver rate for existing staff.
- The starting point for assessing the shortfall between workforce supply and demand is the reliance on temporary staffing in the NHS in 2021/22, which is estimated to have been approximately 150,000 FTEs. In other words, the total demand for workforce is defined by all the workforce deployed (including substantive and temporary staff), and supply is defined by staff in post (substantive). This is not a perfect measure and for some professions other methodologies have been used. For GPs, temporary staffing is not a comparable measure due to the different contracting mechanisms. Therefore, historical patient-to-qualified GP ratios are used to estimate the opening position. In some professions and specialties, access to the temporary market is limited and therefore the use of temporary staffing may underestimate the actual workforce shortfall. In such cases, growth rates should reflect the workforce challenges each profession faces. In addition, the starting point does not take into account unmet demand, and the modelling attempts to address this in future growth to recover services and performance. Overall, temporary staffing is chosen as it better reflects demand for workforce than vacancy rates (which are subject to organisational variances and reporting practices.
- To estimate the future workforce demand, known and expected changes to NHS demand have been applied to the starting point. The drivers of demand are presented in Table 1 and include the additional demand required to recover NHS services and improve performance. Supply projections consider historical trends in supply growth (joiner and leaver rates), the education and training pipeline, planned expansions and observed flows in international recruitment.
- To mitigate the anticipated shortfall position over the 15-year timeframe, this Plan sets out actions that will be taken in the near term, alongside an assessment of the required additional actions over the medium to long term. These are described against three broad areas: train – growing the workforce (Chapter 2); retain – embedding the right culture and improving retention (Chapter 3); and reform – working and training differently (Chapter 4).
Table 1: Demand drivers underpinning modelling
| 1. Demographic growth and the burden of disease |
| Aligned with ONS demographic growth projections, and non-demographic growth based on analysis of growing complexity of needs and historical trends. |
| 2. The service ambition to move care upstream and deliver more NHS care out of hospitals will increase demand in the community |
Community and primary care growth reflects NHS Long Term Plan and service plans to move care upstream, investing more in prevention and early intervention, as well as rehabilitation and reablement to mitigate avoidable growth in secondary care. These incorporate existing service plans including Professor Sir Mike Richards’ review of diagnostics demand, and virtual ward and intermediate care expansion |
| 3. Additional demand required to improve access and performance |
| In acute care, this means tackling long waits in line with the Elective Recovery Plan; and reducing emergency care pressures, by improving flow through the system, reducing acute bed occupancy and length of stay, and improving ambulance call response times, in line with the Urgent and Emergency Care Recovery Plan. This assumes a return to pre-pandemic level of length of stay, which will require social care capacity to stabilise and increase alongside intermediate care capacity. For mental health, this means growth rates based on the NHS Mental Health Implementation Plan and Mental Health Investment Standard. For maternity services, this means reflecting the Ockenden review of maternity services [see reference 81] recommendations in determining the opening shortfall for midwives. Growth reflects changing birth rates as well as higher complexity of need. For primary care, this means using the 2015 ratio of patients to qualified GPs to assess the demand for GPs, and growth in primary care takes into consideration the service plans to enhance access to primary care, such as the Primary Care Access Recovery Plan. For community services, this means improving access and meeting the needs of an ageing population. |
2. Train – Growing the workforce
Overview
- Our assessment is that, compared to 2022, domestic education and training will need to increase between 50% and 65% by 2030/31 (through a variety of training routes). This level of expansion is put forward because, despite accounting for improvements in staff retention and productivity, under current trends, at the end of 2036/37 there would still be a workforce shortfall and significant reliance on international recruitment. And with interest in courses currently surpassing the student places available, there is considerable opportunity to achieve this level of growth.
- To begin realising this expansion, additional funding of more than £2.4 billion cumulatively will be invested in education and training over the next six years, on top of current education and training budgets. This will support a 27% expansion in training places by 2028/29. The growth set out in the Plan builds on the steps already being taken to train more people, and builds on investment already planned, which is increasing from £5.5 billion to £6.1 billion over the next two years.
- For each profession, the Plan sets out a bespoke approach to optimise domestic supply by detailing expansions to entry routes and increasing training and education to meet demand (Table 2), especially for professions with a heavier reliance on international recruitment. This means estimating the potential maximum education and training intake for each profession, and balancing apprenticeships with more traditional university courses. When looking to reduce levels of international recruitment, the Plan has considered the maximum level of international recruitment that could be influenced nationally (such as excluding non-UK nationals who do not need a visa to work in the NHS) alongside the level of overseas recruitment the NHS would always want to retain to give providers flexibility and a source of wider and diverse talent. With these considerations, the Plan sets a reasonable trajectory to increase domestic training and recruitment to materially reduce workforce shortfalls by 2028/29, and largely close shortfalls for most professions by 2031/32. For each profession, as well as assessing the longer-term growth ambitions, the Plan sets out the immediate steps that will be taken to expand education and training for each group, alongside the funding that will be committed to support this. The phasing of planned expansion recognises that additional education and training capacity will take time to put in place, balancing the need to address workforce shortfalls as soon as possible with deliverability.
- Several professions will, even with targeted interventions, likely see medium-term shortfalls and may continue to rely on temporary staff (such as mental health nursing, learning disability nursing and podiatry) or international recruitment (such as adult nursing and doctors). National programmes will examine options for the future of these professions, including how targeted international recruitment or training, and changes in roles or skills mix can help to meet demand.
- Some professions have received recent investment to increase education and training, reducing the magnitude of the expansion they will need compared to other professions. For example, paramedic training places have increased from around 2,100 in 2015 to just over 3,850 in 2022 [see reference 82]. This means that a continued projected average supply growth of 3.7–4.0% per year is possible within the 15-year modelling period with an increase in training places of 5–18% a year.
- Full expansion cannot happen immediately, but rather by incremental but significant increase in education and training capacity. Successful expansion will be contingent on there being an expanded and fully trained supervisory workforce to support evolving learner and workforce need. The initial steps being taken to achieve this are detailed throughout this chapter. Several important reforms will need to accompany expansion, to improve the experience of learners and ensure clinicians of the future have the skills they need to provide high quality care.
- The Plan assumes that the whole health education pipeline will need to grow at least in line with the demand required to deliver NHS services. The proposed training intakes have been adjusted to accommodate this additional demand (Annex C). The proportion of staff who go from training to non-NHS employers is assumed to remain the same. Service models may change the balance of care provided in NHS settings compared to the independent sector or within social care, in either direction, but by increasing the whole pipeline the entire sector has flexibility across regulated health professions irrespective of the organisation services are commissioned by or from.
Table 2: Increase required in education and training by profession
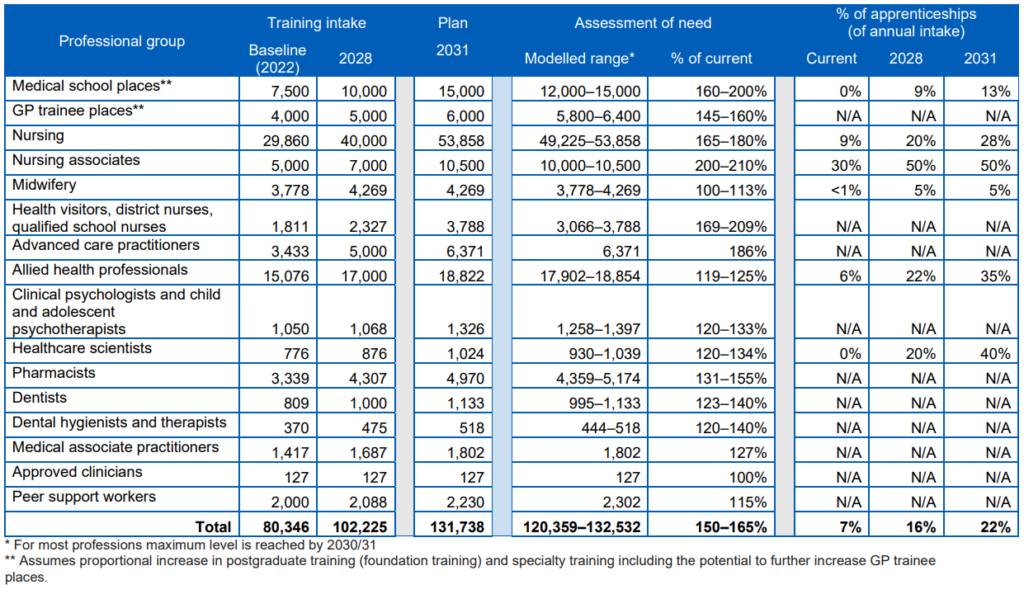
* For most professions maximum level is reached by 2030/31
** Assumes proportional increase in postgraduate training (foundation training) and specialty training including the potential to further increase GP trainee places.
Medical training
- The required increase in medical school places is estimated to be 60–100%, providing 12,000–15,000 places by 2030/31. This can be delivered by the expansion of existing medical schools and establishment of new ones, and the introduction of medical degree apprenticeships. The scale of expansion set out would require close working with medical schools, higher education institutes and the further education sector, the regulator and other stakeholders. This Plan sets out an ambition to double the number of medical school training places, taking the total to 15,000 places a year by 2031/32. Over the next six years, we will work towards this level of expansion by increasing medical school places by a third, to 10,000 by 2028/29.
- To meet the demand for GPs, this Plan outlines a need to increase the number of GP specialty training places by 45–60% by 2033/34. Our ambition is to increase the number of places by 50% to 6,000 by 2031/32. In 2018 the government expanded the number of medical school places by 1,500 and the first of these graduates are now starting to join the workforce. This Plan commits to initially growing GP specialty training by 500 places in 2025/26, timed so that more of these newly qualifying doctors can train in primary care. Further expansion of GP specialty training places will then take place with 1,000 additional places (5,000 in total) in 2027/28 and 2028/29. This will offer the same opportunity to a bigger pool of doctors graduating as a result of the increase in undergraduate places outlined in this Plan.
- We will need to ensure adequate growth in foundation year placements and expansion of specialty training in future years, commensurate with the growth in undergraduate medical training. The increased number of domestically trained doctors will work as GPs and consultants in those parts of the country with the most need, and they will have expertise in treating the conditions prevalent in those areas. We will work with partners to understand the best way to do this, including defining the relevant service demands and workforce supply patterns over time to ensure patient need is met sustainably, and identifying priority areas for investment. Future specialty growth would be in addition to completing the remainder of the planned growth in medical specialty training places by September 2024, which will take the total increase to more than 2,000 places over three years (2021 to 2024). Future expansion would support existing planned growth for mental health, cancer and diagnostic services, as well as 1,000 more specialty training places for those areas that support wider NHS pressures and have the greatest shortages, such as elective recovery, urgent and acute care, maternity services and public health medicine. There are already some 1,500 more places across these combined priority areas.
- NHS England is piloting a medical degree apprenticeship from 2024 [see reference 83]. This will enable the NHS to attract and recruit from a wider pool of people in local communities and enable individuals from under-represented backgrounds to start medical training who otherwise would not have done so through full-time higher education and training routes. 200 apprenticeship places are currently funded for pilots running in 2024/25, with an ambition for up to 400 places by 2026/27. Subject to evaluation, we propose increasing the proportion of medical students training as apprentices, as the overall number of medical school places grows. Our overall ambition is to have 2,000 medical students training via this route by 2031/32. We will work towards this ambition by growing medical degree apprenticeships to more than 850 by 2028/29.
- The shape of the medical workforce is expected to change over the next 15 years, with more specialty and associate specialist (SAS) doctors and doctors in training choosing alternative career paths rather than core and specialty training routes. In assessing expansion requirements, we have considered this, as well as the trend for more doctors choosing to work less than full time and the associated implication of needing more doctors to achieve the equivalent FTE level. Likewise, the Plan has considered the future need for more generalist doctors and those with generalist skills, and the modelled increases are particularly targeted towards general practice. This is reflective of a growing progressive professional consensus over the past decade that training should change, supporting a better balance of generalist and specialist skills so that doctors are equipped to provide the joined-up care required for people with multiple morbidities. This is an important strategic objective, and we will work closely with medical schools, royal colleges, the GMC and employers to support the profession in making this agenda a reality.
Nursing education and training
- To meet the demand for nursing, this Plan outlines a need to increase nursing training places by 65–80% by 2030/31. Our ambition is to increase training places by 80% to over 53,500 by 2031/32. To support working towards this ambition, we will increase nursing training places by 34% to 40,000 by 2028/29.
- We estimate a need to increase the education intake for adult nursing by 76– 92% by 2030/31, through a combination of increasing traditional undergraduate and postgraduate training and apprenticeship places. The range reflects the different choices that could be made about how quickly international recruitment for adult nursing could be reduced. This Plan sets out an ambition to increase adult nursing training places by 92% to nearly 38,000 by 2031/32.
- To support this growth, we will begin by increasing training places by 41% to nearly 28,000 over the next six years, so that in 2028/29 at least 8,000 more adult nurses will start training compared to current levels. The nursing growth set out in this Plan follows the expansion planned as part of the 2019 government manifesto commitment to the 50,000 Nurses Programme.
- Estimates for required increases in training for mental health nursing and learning disability nursing are 74–93% and 92–100% by 2030/31 respectively. Our ambition is to increase training places for mental health nursing by 93% to more than 11,000 places by 2031/32, and to double training places for learning disability nursing over the same time period (to over 1,000 places). To support this ambition, by 2028/29 we will increase training places by 38% for mental health nursing and 46% for learning disability nursing, with increases of 13% and 16% seen by 2025/26, respectively. Our assessment is that there is currently a sufficient number of training places to meet demand for children’s nursing, but we will keep this under review.
- The health visiting workforce is fundamental to improving the health and wellbeing of families from pregnancy to starting school by promoting health, preventing ill health and reducing inequalities. And by providing support in the community, they help alleviate pressures on hospital care. The Plan’s assessment is that education and training routes into the health visiting workforce would need to expand by between 32% and 74% by 2030/31. Our ambition is to expand training places by 74% to over 1,300 by 2031/32. To support working towards this expansion, training places for health visitors will grow by 17% by 2028/29. Over the same timeframe to 2028/29, training places for district nurses will grow by 41% (supporting an ambition to increase places by over 150% to nearly 1,800 by 2031/32) and training places for school nurses will grow by 28% (supporting an ambition to nearly double training places to over 650 by 2031/32). Service plans in these areas will need to be kept under review to determine whether further growth in training is required to meet demand.
- Our modelling indicates that by 2031/32, 28% of registered nurses could train through a degree level apprenticeship route and our ambition within this Plan is to meet that level of growth. This includes 42% of learning disability nurses and 30% of both adult nurses and mental health nurses training via an apprenticeship route. Currently, only approximately 9% of nurses qualify through apprenticeships. We will work towards this ambition by expanding nursing apprenticeships so that by 2028/29, 20% of registered nurses are qualifying through this route, including 33% of learning disability nurses, 20% of adult nurses and 28% of mental health nurses.
- The Plan sets out a need for broader and longer nursing career pathways, and further opportunities for career progression through more enhanced, advanced and consultant practitioners, some of whom will be nurses. There are currently 4,600 nursing associates (NAs) working in the NHS. Supported by a 40% increase in training places to 7,000 by 2028/29, and an ambition to grow this further to 10,500 places by 2031/32, it is estimated there will be 64,000 NAs by the end of the modelled period. The number of nurses is projected to increase significantly from nearly 350,000 now to between 545,000 and 565,000 in 2036/37. The nursing training pathway will be supported by a higher proportion of apprenticeships, both at foundation degree level for NAs and for degree-level registered nurses, as well as increased opportunities for progression. For example, the NHS is determined to continue to invest in training opportunities and the development of career pathways for nurses who wish to become clinical nurse specialists working with people with cancer, supporting the NHS Long Term Plan commitment of ensuring that all cancer patients, including those with secondary cancers, have access to specialist care and support. The education and training pathway will be developed through working closely with professional groups, regulators and other key stakeholders.
Midwifery education and training
- The Plan sets out a need to grow midwifery education and training, in line with the conclusions of the Ockenden review, [see reference 84]. Although birth rates are projected to fall for the remainder of this decade (before stabilising and then rising in the 2030s), [see reference 85], the complexity of births is rising [see references 86, 87]. We know we currently have a shortfall of midwives and leaver rates are high. The assessment of the workforce required has been adjusted to reflect the staffing levels needed to deliver safe maternity services, and we envisage that trusts will meet establishment levels set by midwifery staffing tools and achieve fill rates by 2027/28 [see reference 88]. Recent investment in midwifery of 650 training places in 2019 and 1,000 in each of the following three years means we expect to see solid growth in midwives of 1.8–1.9% per year over the course of the Plan. These increases are being measured against the 2018/19 baseline of 2,715 starters. And in early 2022, a funding offer was agreed to support 300 places for adult nurses on the shortened midwifery programme until 2024. We anticipate upwards of 4,270 starters on midwifery programmes are likely in 2023/24, a 13% increase compared to 2021/22 levels. We will train more midwives through traditional, shortened and degree-level apprenticeship routes.
- The Plan sets an ambition for 5% of the annual intake for midwifery training to come through apprenticeship routes, and we are supportive of this being higher in geographies where there is a need. Alongside this, maternity support workers and registered nurses should be employed in appropriate places to complement the unique contribution made by midwives. There will also be a strong focus on retention in midwifery, such as through a new preceptorship for newly qualified midwives.
Public health training
- We will expand the specialist public health workforce by providing 13% more training places in 2023/24 than we do currently. We will work with national, regional and local system partners, including DHSC and the UK Health Security Agency, to address the demand and supply challenges of the public health workforce in future years.
Allied health profession training
- Education and training places for the AHP workforce are estimated to need to grow by 19–25% by 2030/31. This Plan sets out an ambition to increase AHP training places by 25% to over 18,800 by 2031/32. To support this level of ambition and work towards this level of expansion, AHP training places will increase by 13% to 17,000 by 2028/29, with an increase of 8% by 2024/25.
- This expansion would need to focus on both apprenticeship routes and traditional undergraduate courses. More than a third of AHPs could train through apprenticeships, compared to 6% now, but this would vary by professional group. The Plan sets out the following assessment for proportion of entrants joining the AHP workforce via an apprenticeship route by 2031/32:
- at least 80% for operating department practitioners, therapeutic radiographers and podiatrists
- 25–50% for paramedics, diagnostic radiographers, occupational therapists, dietetics, prosthetists and orthotists
- up to 5% for speech and language therapists and physiotherapists.
- Implementing the Plan’s recommendations would enhance the scope and reach of AHP roles to help manage demand most productively. This includes increasing the number of advanced practitioners and independent prescribers, and AHPs acting as senior decision-makers in appropriate settings. Alongside this, education and training expansion and reform will be important to address shortages in particular allied health professions, such as diagnostic radiography, therapeutic radiography, occupational therapy, and speech and language therapy. For example, our assessment is that the paramedic workforce will need to increase by around 14,200– 15,600 over 15 years, to deliver services in ambulance and other care settings, as well as creating a pipeline of staff who will go on to work as advanced practitioners. To enable this, the Plan proposes that paramedics have more rotational training placements across hospital, community and primary care settings. For podiatry, we propose expanding apprenticeships significantly, so they become the main entry route into the profession.
- In 2022/23, NHS England made a significant investment to build international recruitment pipelines for AHPs, which we estimate will result in 1,500 additional AHPs working across the NHS in 2023. The activity set out in this Plan builds on this committed funding and planned growth.
- We will work to ensure that AHPs are able to find quality work in the NHS once they graduate, so that the assessed expansion in training results in increased capacity for the NHS and more varied roles for individual AHPs.
Psychological professions training
- Psychological professionals, comprising psychologists, psychological therapists and psychological practitioners, are making a rapidly growing contribution to the NHS across mental health and physical health services. Education and training places for clinical psychology and child and adolescent psychotherapy are estimated to need to grow by at least 20–33%, reaching 1,258–1,397 by 2033/34. Our ambition is to grow these training places by 26% by 2031/32. To support working towards this ambition, training places for clinical psychology and child and adolescent psychotherapy will be more than 1,000 each year up to 2028/29.
- In addition to education and training for clinical psychologists and child and adolescent psychotherapists, over the next three years NHS England has committed funding of over £600 million to grow the wider psychological professions workforce through training approximately 15,000 more individuals to undertake psychological therapist and psychological practitioner roles.
- Psychological professions are a key example of a professional group where service plans and ambitions will need to be kept under review to determine whether further growth in education and training is required in the future, beyond what this Plan sets out.
Pharmacy training
- Education and training places for pharmacists are estimated to need to grow by 31–55% to meet the demand for pharmacy services, reaching 4,359–5,174 by 2032/33. This Plan sets out an ambition to increase training places for pharmacists by nearly 50% to around 5,000 places by 2031/32. To support this level of growth, we will expand training places for pharmacists by 29% to around 4,300 by 2028/29, starting with initial growth in 2026/27 when places will increase by 15%. We will also continue to grow the pharmacy technician workforce to ensure expansion of this professional group to support growth and transformation across the pharmacy workforce.
- In future, all newly qualified pharmacists will be independent prescribers, shortening the time it takes for pharmacists to prescribe independently from approximately eight years to around five years. We are also supporting 3,000 existing pharmacists to develop these skills to ensure they and the wider pharmacy team can play a greater role as part of multidisciplinary clinical teams. We will continue to ensure clinical pharmacist and pharmacy technician roles provide high quality, safe hospital care following the success of the Hospital Pharmacy Transformation Programme.
- There is potential to continue expanding training via the apprenticeship route for pharmacy technicians and consideration is being given to the potential of a pharmacist degree apprenticeship.
Dentistry training
- To support NHS service delivery plans, the Plan assesses that programmes for dental therapy and hygiene professionals need to expand by 20–40% and for dentistry places by 23–40% as soon as possible, although scaling places in the right geographies may take several years. Our ambition is to increase training places for both of these workforce groups by 40% by 2031/32, increasing places to over 500 for dental therapists and hygiene professionals, and to over 1,100 for dentists.
- To support this ambition, by 2028/29 we will grow training places for dental therapy and hygiene professionals by 28%, with an increase of 24% for dentists (to 1,000 places) over the same period. In 2022/23, NHS England made an investment in postgraduate dental specialty training, focused on areas currently underserved by existing provision, which will improve access to specialist dental services in future. The growth set out in this Plan builds on this investment.
- We recognise the important contribution to dental care that the wider dental workforce makes, including dental nurses. While training of dental nurses is largely the responsibility of dental practices, we will work with dental practices and other stakeholders to support the wider dental workforce to meet NHS service delivery plans for dentistry.
Healthcare scientists’ training
- Healthcare scientists provide the scientific backbone of the NHS; their work underpins 80% of all diagnoses, supports high quality research and is important for technological innovation. To meet the needs of the NHS, the Plan assesses that education and training places for healthcare scientists need to increase by 20– 34%, reaching 930–1,039 by 2033/34. The ambition set out in this Plan is to increase training places for healthcare scientists by 32% to over 1,000 places by 2031/32. We will work towards achieving this ambition by increasing training places by 13% to over 850 by 2028/29. Apprenticeship routes for healthcare scientists are also being made available, with 20% of training places delivered via an apprenticeship route by 2028/29 (supporting an ambition to have 40% of healthcare scientists starting their training via an apprenticeship by 2031/32).
Implications for international recruitment
- Investment in domestic education and training would support the NHS to become less reliant on international recruitment for workforce supply in the medium to long term, while targeted international recruitment in the short term would continue to ease workforce shortages in certain professions. The pace at which international recruitment can be scaled back will be contingent on the rate of expansion of and investment in domestic training and education, and the other uncertainties outlined in this Plan.
- With implementation of the education and training expansion outlined in this Plan, we could expect a corresponding decrease in international recruitment across the NHS from the current 24% of all new joiners to 9.0–10.5% a year by 2036/37. This includes general practice but excludes dentistry and community pharmacy, which have been modelled separately.
- Most notably, a near doubling of nursing education and training places would reduce the proportion of new adult nursing joiners who need to be recruited from overseas from 57% in 2022/23 to approximately 15–17% in 2036/37. Under all modelling scenarios, reliance on international recruitment will materially decrease from 2030. To meet workforce demand in the short and medium term, ethical international recruitment [see reference 89] of adult nurses would need to remain at least around current levels in the coming years. The level of international recruitment depends on the assumed level of demand, productivity levels, speed of training and education expansion. The modelling estimates that the maximum level of international recruitment for adult nurses will be 16,200–17,900 a year, and cumulatively could be around 164,000–170,000 over the 15-year modelling period.
- The NHS will always retain some level of overseas recruitment to give providers flexibility and as a source of wider and diverse talent. However, for doctors, the Plan’s assessed expansion – 60% to 100% for medical school places – would support a significant reduction in international recruitment from the current position of around 6,000 FTEs a year. Depending on the level of productivity achieved, lower training and education expansion could mean a continued level of reliance on international recruitment. Using prospective medical workforce intelligence and modelling, we would work with employers, educational stakeholders and the royal colleges to align the expansion in domestic medical training set out here with future workforce needs.
- More broadly, if productivity levels are towards the higher end of the range used in the modelling, this helps, alongside the requirement for growth in education and training, to moderate long-term requirements for international recruitment.
Implications for temporary staffing
- Investment along these lines would also reduce reliance on temporary staffing over time, particularly of agency staff whose engagement should be the exception rather than the norm. In parallel, while staff banks are a flexible and valuable resource, it is not prudent for the NHS to depend on staff offering additional hours, often on top of full-time substantive contracts. The Plan sets out a path to reduce the NHS’s reliance on agency over the modelling period, while still retaining the ability to utilise bank staff in a cost-effective way. We estimate that the reliance on temporary staffing in FTE terms would reduce from 9% in 2021/22 to around 5% from 2032/33 onwards, with mostly bank staff fulfilling the requirement for temporary staffing.
Therefore, the ambition is to reduce over time the proportion of work currently done as bank shifts, particularly by already substantively employed staff. The need for some bank shifts will remain due to unexpected absences and fluctuations in demand, and because offering some level of flexibility for substantive staff can help make substantive employment the most attractive option.
Apprenticeship expansion
- Apprentice training routes are employer led and support entry into clinical professions, from support worker roles or directly through registered degree-level entry, and into wider healthcare roles. Expanding apprenticeship routes can help address key workforce shortages and particularly benefit those professions that historically lack a consistent route for training and career development, such as non-clinical professionals in corporate services, estates and facilities and general management. Equally, they are beneficial for clinical professions such as learning disability nursing, therapeutic radiography and operating department practitioners, which may not be as visible to school leavers, and may be of more interest to people with greater life experience.
- Apprenticeships also widen opportunities for people from all backgrounds and in underserved geographical areas to join the NHS workforce, in turn making the NHS a more inclusive place to work [see reference 90]. Alongside initiatives like the Lifelong Loan Entitlement and other technical and vocational programmes, including T-Levels and Higher Technical Qualifications, aimed at equipping young people and adults with the skills needed to succeed in their chosen careers, apprenticeships enable people to gain a qualification while earning a salary.
- Apprentices contribute to patient care during the period of their training. Apprentice routes support the NHS to build multidisciplinary teams with the right skills mix for the future, as well as support staff to advance in their careers by opening routes into enhanced and advanced practice roles.
- Emerging evidence shows that apprentices are less likely to leave training compared to those in traditional undergraduate training programmes. For example, attrition rates for all current cohorts of the registered nurse degree apprenticeship programmes are 4%, [see reference 91] compared to over 15% for traditional nursing undergraduate and postgraduate courses [see reference 92]. And there is evidence of better retention of apprentices; some trusts have been able to retain 100% of their registered nurse apprentices [see reference 93].
- To implement this Plan, NHS England will develop an apprenticeship funding approach that better supports employers with the cost of employing an apprentice. NHS England is committed to working with NHS employers, ICSs, providers and other partners to develop a national policy framework that can be used locally to guide the use of funding, targeting those apprenticeship schemes that would have the greatest impact on patient outcomes.
- NHS England will work jointly across government to ensure that any changes to NHS England’s apprenticeship funding approach are supported by, and align with, wider government apprenticeship funding policy. For example, NHS England and DHSC will work with the Department for Education (DfE) to enable apprenticeship levy funds to be more easily transferred between employers in an ICS and ensure that data on the use of apprenticeship funding in the NHS is more visible to decision-makers at national and local level. Working collaboratively will help us deliver a joined-up apprenticeship funding approach that more effectively supports employers and ICSs to plan and deliver apprenticeships strategically across their local footprint.
- This Plan commits to supporting ICSs to develop local apprenticeship strategies that maximise benefits from changes to funding approaches and to focus on workforce shortfalls and the deployment of roles that enhance patient outcomes. A system-level apprenticeship strategy – with system-level oversight and planning – would better support organisations to grow and recruit their own staff, and enable ICSs to collaborate on their approaches to using apprenticeships with education providers both nationally and locally. Local strategies would support quality apprenticeship programmes targeted at specific occupational shortages and skills gaps, and transformation across primary, community, mental health and acute care. System-level working would help employers engage their local population, schools and colleges to improve access to apprenticeship programmes and maximise innovative approaches to delivery. NHS England is committed to supporting ICSs through provision of annual ICB-level education and activity funding statements, to enable them to manage education capacity and to support education plans.
Case study:
Staffordshire and Stoke-on-Trent Health and Care Apprenticeship Scheme
Staffordshire and Stoke-on-Trent ICS and partners offered provider-based rotational apprenticeships to new recruits as part of a wider programme to increase the participation of young people from diverse and hard-to-reach backgrounds in health and social care careers. The apprenticeship scheme aims to give young people a clearly defined vocational pathway into a registered profession.
The team worked with partners in the NHS, Skills for Care and local authorities to agree a joint approach to developing a series of health and social care rotational apprenticeships. This developmental programme allowed apprentices to gain experience working in different health and social care settings. A total of 53 apprentices have been recruited since the schemes were created, with 76% remaining in health or social care or pursuing higher level qualifications.
Anchor institutions – the role of NHS organisations in their local communities
- In line with the ICS people function guidance [see reference 94], and as part of their plans to grow their workforce, all ICSs will be supported to build partnerships to develop a sustainable supply of locally recruited staff, support the health of communities and reduce inequalities. Every NHS organisation across the country forms a critical part of its local community. There is increasing evidence that NHS organisations, as anchor institutions, can make a meaningful impact on the long-term health of their communities [see reference 95]. The evolving role of ICSs and establishment of ICBs provides a further opportunity for local health and care systems to make the most of the NHS’s role as an anchor institution.
- We have worked with NHS Employers to offer all NHS organisations support to add value to their local communities through innovative access to employment programmes and the provision of education and training, [see reference 96]. The Health Anchors Learning Network [see reference 97] provides resources and support to healthcare organisations seeking to develop their role as an anchor institution, and is free to join.
- With this Plan’s proposed expansion and development of staff, NHS employers have the opportunity to add social value, benefit communities and reduce inequalities through direct employment practices. This can be achieved by:
- recruiting more people from local communities with a particular focus on those who may experience health inequalities
- proactively facilitating skills development including digital skills, career progression and social mobility programmes
- supporting the health and wellbeing of all staff.
Recruitment and supply
Recruiting to support worker roles
- This Plan commits to developing healthcare support workers, giving them opportunities to build specialist knowledge and skills that will enable them to develop in their careers and also support the NHS in addressing specific workforce shortfalls. Implementation of this Plan would see a greater portion of people recruited to the NHS clinical workforce by direct entry to a support worker role and in role development. By ensuring greater flexibility in the way that the NHS trains staff, such as through apprenticeships, our people will be able to develop their skills, knowledge and experience to gain formal qualifications and progress on a lifetime career ladder.
- Apprenticeships are already available that allow a support worker to train as a nursing associate, and then gain a degree-level qualification to practise as a nurse. The actions set out earlier in this chapter would enable employers and staff to make increased use of these ‘in-house’ development pathways. For example, in renal services we will train clinical support workers to become dialysis healthcare assistants with specialist renal knowledge and skills, and in podiatry services we will train support workers to take on podiatry assistant practitioner roles working under the direction of a podiatrist’s treatment plan.
- Over the coming years, we would need to significantly increase direct entry roles, to build a sufficient and sustainable pipeline of people who the NHS trains to progress to more advanced clinical roles. Over the past 18 months, a national recruitment programme has brought 46,000 people into the NHS as healthcare support workers. This has opened up opportunities for those new to health and social care; in 2022/23, 46% of those that joined the NHS were new to care. We will continue this programme over the next two years, and work with systems to improve local recruitment processes.
- We anticipate that NHS organisations will need to recruit from the wider labour market to a much greater extent in future. We estimate that to meet the anticipated demand in 15 years’ time, 204,000–230,000 more staff are needed to support those in clinical roles, 47,500–56,500 of whom are healthcare support workers. The NHS will need to compete in the wider labour market to achieve this. Support worker roles would then open up pathways to become registered healthcare professionals or clinical assistants. NHS systems would need to take a co-ordinated approach to recruiting to these roles and ensure the employment offer attracts the best candidates. To support local systems, NHS England will look to run recruitment exercises at scale for entry-level NHS jobs, including healthcare support workers, and work in partnership with Jobcentre Plus where appropriate.
Attracting staff
- The NHS has a well-recognised brand and values, and national careers campaigns under the ‘We are the NHS’ banner have been effective in boosting applications to nursing degrees, and interest in health careers more generally. Through this Plan and targeted programmes of work, we will support local NHS systems and organisations to build on the strong reputation and the unique employee value proposition the NHS has to offer. We will do this by highlighting the flexibility and autonomy that NHS staff enjoy and setting out the opportunities for development across the workforce. We will deliver actions that welcome new people to the NHS and support them as they embark on a long and fulfilling career; for example, by continuing to implement the actions in the NHS estates and facilities workforce action plan [see reference 98]. This is a critical step to ensuring the NHS can attract the staff it needs, including 204,000–230,000 new support workers over the next 15 years.
- We will continue the successful national advertising campaigns to promote NHS careers where there is a national shortfall in the workforce. This activity will be supported with materials and other resources that ICSs can tailor to promote job opportunities for those roles that are in greatest need locally.
- This Plan proposes that we overhaul national recruitment practices and systems, so they are modern, flexible and provide a good experience for candidates and recruiters, and allow local adaptation where this is required. The NHS must also ensure its employment offer is attractive to people across all generations, including those who have yet to join the workforce.
- We know that recruiting managers in the NHS lose good candidates, particularly for direct entry roles (such as healthcare support workers), as candidates can secure a quicker start date with other big employers. We are working with system partners and industry experts to understand how NHS systems and practices could change to address this. We will work to deliver a number of key actions, including to ensure it takes no longer than six weeks from the placement of an NHS advert to the completion of a candidate’s pre-employment checks. We will change NHS recruitment practices, so they do not disadvantage any protected groups and encourage people with lived experience of services to apply. We know from Workforce Race Equality Standard (WRES) data that staff from an ethnic minority background have a poorer experience of NHS recruitment processes than their white colleagues. This is also the case for staff with disabilities, as shown in the Workforce Disability Equality Standard (WDES).
Providing flexibility of work through temporary staffing
- Temporary staffing solutions are integral to the running of the NHS. Secondary care providers have developed a flexible range of approaches to engage people through staff banks, and made concerted and focused efforts to reduce reliance on agency staff. By 2022, all systems had introduced a primary care flexible staff pool supported by a digital solution to help match GPs and practices. Over the next 15 years, the NHS will need to further strengthen its approach to offering a blended career. Staff should have certainty through substantive roles and the opportunity for extra income by working additional shifts. We know that staff appreciate the flexibility that working in an NHS bank can offer; however, while this should not be the only route staff have to secure the working pattern that best suits them and earn additional income, it should be the most attractive one – to help fill short-term shortfalls and reduce the NHS’s reliance on agency providers. Subject to the implementation of the other actions in this Plan, we aim to reduce agency expenditure in secondary, community and mental health providers as shortfalls reduce.
- We will support the NHS to take measures that allow greater mobility of staff across boundaries and sectors through collaborative banks. All ICSs now have a primary care flexible pool that supports staff to work across a locality’s different primary care settings. There are 23 collaborative banks across NHS trusts, with 10 more planned, representing a 50% increase since the NHS People Plan was published in 2020 and covering nearly half of all trusts in England. The wider NHS will be supported to adopt these practices, building on the learning from primary care. This can be achieved by, for example, fostering effective relationships between partners and trusts and investing in technology that makes it easier for staff to accept a temporary shift.
- We propose to support NHS providers to develop and implement policy that prevents substantive staff from offering their services back to the NHS through an employment agency, and instead do so through their local collaborative bank.
Leveraging the impact of volunteers
- The health service has always benefited from the generous and significant support of volunteers and voluntary sector organisations. Their involvement complements and extends the NHS workforce but does not replace it. Volunteers help improve services across the NHS, and support better outcomes for patients and the wellbeing of staff, [see references 99, 100, 101 and 102] but, as seen during the pandemic, also provide additional capacity and flexibility in how services are delivered. Volunteering can also improve people’s mental and physical health, and gives them the opportunity to acquire skills that enhance their ability to gain employment.
- Volunteering opportunities are an important aspect of the NHS’s role as an anchor institution. However, support for volunteering varies across NHS organisations and potential volunteers often find it difficult to find the right opportunity. As a result, the NHS has not fully tapped the true potential of volunteering, both its impact on service delivery and patient experience, and in providing a route into the NHS workforce. An NHS Volunteering Taskforce was established in 2022 to develop recommendations for improving the quality, range and quantity of volunteering opportunities. The taskforce heard examples where volunteering had strengthened and extended integrated care and we will work with ICSs to achieve a more resilient, interconnected and inclusive volunteering infrastructure, [see reference 103]. This is being supported by expansion of the existing NHS and Care Volunteer Responders programme [see reference 104] into adult social care in summer 2023, to develop a long-term health and social care programme to benefit both sectors. In addition, in 2023/24 NHS England will develop a new health and care volunteering recruitment portal and scope the potential for an NHS volunteering quality standard, to be rolled out in subsequent years.
- ICBs should embrace volunteering as part of their overall workforce plan, giving due consideration to programmes that support volunteering as a route into the workforce, such as NHS Cadets [see reference 105] and Volunteer to Career [see reference 106].
Case study: NHS Cadets
Launched in 2020, NHS Cadets is a programme delivered in partnership with St John Ambulance to reach young people from communities that are under-represented in the NHS workforce. Cadets are offered volunteering opportunities in the NHS and the chance to learn valuable skills such as first aid. They also learn about the variety of careers available in the NHS.
To date 65% of NHS cadets identify themselves as being from a Black or ethnic minority background and 16% as young carers, and 22% receive free school meals. Many of these young people identify as belonging to more than one of these groups.
3. Retain – Embedding the right culture and improving retention
Overview
- While training more staff is critical, if the NHS does not embed the right culture and improve staff retention, then NHS workforce shortfalls will continue to persist. Various factors influence why people leave the NHS workforce. In 2022, where people have chosen to leave an NHS trust, some of the most common reasons were pay and reward, work-life balance, progression and continuing professional development (CPD), as well as health and wellbeing [see reference 107]. Recent evidence from the Institute for Fiscal Studies highlights the complexity of factors that influence staff retention in the NHS acute sector – retention rates vary significantly by professional group and factors such as an individual’s age and recent sickness absence [see reference 108]. The collective impact of the Plan’s proposals, aligned to increases in capacity, would help reduce the overall leaver rate for NHS employed staff from 9.1% in 2022 to between 7.4% and 8.2% over the course of the modelling period. This is equivalent to retaining 55,000–128,000 FTEs.
- This range provides a stretching but realistic trajectory – it falls between the pre- pandemic low and average leaver rates (between 2015 and 2019) for each profession and factors in several key considerations. Some of the elements that influence retention, such as wider economic and labour market conditions, are outside the scope of this Plan. The anticipated improvement in leaver rates is phased over the modelling period. In the short term, leaver rates increase; this is in part because staff who chose to defer leaving or retiring so that they could work during the COVID-19 pandemic are now taking the decision to leave. In the longer term, significant improvements in retention will depend on a changed culture across the NHS and more flexible working options.
- The NHS People Promise, [see reference 109] in the words of NHS staff, describes the action we must all take to make the NHS a good, modern employer of choice and to improve staff experience over the long term. This Plan builds on the seven elements of the People Promise and NHS People Plan [see reference 110] to set out a consistent approach for all staff. It recognises the differing needs of the workforce based on factors such as generational differences and career stage.
- The NHS National Retention Programme [see reference 111] and NHS People Promise exemplar sites [see reference 112] demonstrate that single retention interventions have limited efficacy. Therefore, this Plan recommends actions to deliver sustained gains across the whole workforce. These address some of the key retention issues partner organisations have identified previously, [see references 113, 114, 115].
- Beyond this, Our Leadership Way [see reference 116], and the recommendations of the Kark [see reference 117] and Messenger [see reference 118] reviews, describe the management capabilities and compassionate and inclusive behaviours leaders need to give staff the backing they require to deliver for patients. Managers, both clinical and non-clinical, and people professionals will have a key role to play. The future of NHS human resources and organisational development report [see reference 119] sets out how people professionals need to work differently to create a consistently compassionate, inclusive and values-driven culture that delivers better staff experience now and in the future. This Plan builds on these previous pieces of work.
- In addition to this Plan, the recent deal agreed between government and the NHS Staff Council sets out a further programme of work through DHSC and the NHS Staff Council to support the workforce and aid retention of NHS staff. It outlines a series of commitments on career development and building a workforce for the future. This includes, but is not limited to, reviewing the support newly qualified staff receive and ensuring existing NHS staff, who have agreed development plans in place through apprenticeships, are not financially penalised.
- Currently, staff across the country are working in hugely pressured environments. We must recognise the influence staff shortages have on organisational culture, and an individual’s experience at work and their decision to leave. In addition to the actions set out here, increased workforce supply will help achieve the retention ambitions in this Plan.
- We know there is an association between staff experience and engagement, productivity, patient outcomes and safety [see reference 120]. In addition to improving retention, embedding the right culture will mean the NHS supports staff to lead the transformation needed to provide sustainable, high-quality services. Evidence demonstrates that meeting three core needs of staff – supporting them to have a sense of autonomy, belonging and contribution – transforms working lives, facilitating better productivity and effectiveness and improved patient safety and care, [see references 121, 122].
- The proposed actions set out here can be considered as a minimum standard the NHS should aim to meet. Implementation will require co-ordinated and supportive working at national, system and provider level. In line with NHS England’s new operating framework [see reference 123] and guidance on ICS people functions, [see reference 124] we propose that system partners work together to determine how these actions are best implemented to provide a consistent staff experience across organisational boundaries. We will work with ICSs to ensure that the proposed actions can be applied appropriately in primary care settings, in line with the recommendations in the Fuller Stocktake [see reference 125].
We are compassionate and inclusive
- We must do more to ensure our staff, learners and volunteers are treated fairly within a compassionate and inclusive culture. Our NHS workforce is more diverse than at any other point in history, with nearly 25% of staff coming from an ethnic minority background [see reference 126]. Progress has been made in some areas. For example, ethnic minority representation at very senior manager level in NHS trusts has increased from 7.9% in 2020 to 10.3% in 2022, and 13.2% of NHS trust board members were from an ethnic minority background in 2022 compared to 10% in 2020 [see reference 127]. The number of very senior managers with a disability increased from 2.8% in 2020 to 3.4% in 2021 [see reference 128]. And the proportion of people who choose not to declare their sexual orientation in the NHS Staff Survey decreased from 6.6% in 2018 to 5.9% in 2022 [see reference 129]. However, there is much more to do to make progress through systematic improvements to recruitment and promotion practices, leadership diversity, disciplinary processes, governance and accountability, and training and education. The NHS must embed a compassionate culture built on civility, respect and equal opportunity. This is critical to tackling wider health inequalities as well; for example, in mental health [see reference 130] and maternity services [see reference 131] where we know people from ethnic minority backgrounds experience worse health.
- NHS England has recently published the first ever equality, diversity and inclusion (EDI) improvement plan for the NHS [see reference 132]. The EDI improvement plan sets out six high impact actions that will help ensure the NHS continues to make progress on tackling the prejudice and discrimination that some staff experience when they come to work, building on the progress made to date. There has also been further welcome action taken nationally to support tackling racism, including the recent resource Combatting racial discrimination against minority ethnic nurses, midwives and nursing associates [see reference 133] developed by NHS England and the NMC, which provides practical examples and tools to support staff to explore and challenge safely and effectively.
- NHS organisations are encouraged to undertake a cultural review on a regular basis to understand how to improve working environments so that all staff can thrive. To embed a consistent experience for staff, this would be best undertaken in collaboration with system partners and peers. Doing so would allow us to take a more practical and structured approach to understanding culture, the perspectives of the NHS workforce, patients and partners, and to support targeted and relevant action. The NHS Culture and Leadership Programme [see reference 134] provides a well-established tool and evidence base that NHS systems can use to conduct reviews.
We are recognised and rewarded
- Everyone working in the NHS should be recognised and rewarded fairly to help ensure we attract and retain the staff we need to provide the best possible care for patients. The total reward package – which goes beyond headline pay – will need to be attractive and competitive to respond both to changes in people’s career aspirations and the labour market.
- NHS England will work with government to deliver actions to modernise the NHS Pension Scheme. During 2023/24, DHSC will introduce reforms to the legacy pension scheme so staff can partially retire or return to work seamlessly and continue building their pension after retirement if they wish to do so. With the support of their employers, this will enable a ‘decade of retirement’ approach through which older staff can draw down their pension, work more flexibly and remain in the workforce longer. The NHS will continue to benefit from the skills and experience of these staff members, and individuals will be supported to have a more sustainable work pattern in the late stages of their careers. This is in addition to the substantial pension tax reforms in the Spring Budget 2023 [see reference 135], which ensure doctors are not disincentivised from continuing their NHS work or taking on extra hours or responsibilities.
- Every staff member should be given the opportunity for regular conversations to discuss their wellbeing and what will keep them in work, including discussions about pension flexibilities, flexible working options, and health and wellbeing.
- From 2023/24, it is proposed that NHS organisations work with system partners to develop a clear employee value proposition (EVP) and promote this across the workforce. This EVP would cover national and local benefits, including pensions, salary sacrifice schemes and local financial wellbeing support initiatives, as well as other elements of the NHS People Promise [see reference 136] such as employee voice, flexible working and development.
- We will support ICSs to agree plans across their system for implementing flexibilities – where permissible – within national terms and conditions (such as local incentives for new recruits and bank rates), to facilitate a more strategic and aligned approach to improving reward and recognition for staff. ICSs will be encouraged to work with partners to support the recommendations of the Fuller Stocktake for innovative employment models and adoption of NHS terms and conditions in primary care [see reference 137].
We have a voice that counts
- We want NHS staff to feel valued and respected at work and to know their views are welcomed. To do this, we need to provide the best possible working environment, where speaking up is not only welcomed, but valued as an opportunity to learn and improve.
- To ensure continuous feedback mechanisms are in place, all NHS organisations will be encouraged to assess the effectiveness of current methods of staff communication and ensure they have a listening approach in place which best engages staff and ensures feedback is acted on. National guidance is available to support organisations with developing listening approaches [see reference 138].
- Building on existing policy [see reference 139], every NHS organisation should have a clear and regularly communicated Freedom to Speak Up approach, which focuses on creating an inclusive culture that supports learning and improvement.
- There is opportunity for organisations to make better use of national tools [see references 140,141,142] and to more regularly use employee engagement metrics to inform improvement plans, so staff are involved in developing services and improving working environments. This is particularly important when considering how to better capture and improve the experiences of staff with protected characteristics.
We are safe and healthy
- Looking after the health and wellbeing of NHS staff is paramount. Significant workforce shortages and rising demand for care are increasingly stretching NHS staff. We are seeing more staff absent from work due to mental ill health than ever before. In the 2022 NHS Staff Survey, 34.0% of staff said they often or always felt burnt out because of their work and 4% said they often or always found their work emotionally exhausting [see reference 143].
- Monthly NHS staff sickness absence rates peaked in January 2022 at 6.7% and are now declining, although rates remain higher than those observed pre- pandemic [see reference 144]. Sickness absence rates vary across the country and by care setting; rates are highest in ambulance services. Likewise, some staff groups are affected more than others – the staff group ‘support to clinical staff’ saw the highest rate of sickness absence in January 2023 at 7.2%, with ‘support to ambulance staff’ having the highest rate as a sub-group within this (9.1%). ‘Ambulance staff’ and ‘midwives’ were the staffing groups with the second and third highest rates of sickness absence at 6.7% and 6.1% respectively. Although down compared to the same time last year (by 3.4% from January 2022) [see reference 145], anxiety, stress, depression and other mental health illnesses remain the most commonly recorded reason for sickness absence, followed by musculoskeletal problems and coughs, colds and influenza [see reference 146].
- Well-established evidence demonstrates a correlation between staff health and wellbeing and patient outcomes [see reference 147]. We also know an integrated approach to staff wellbeing can increase employee engagement [see reference 148], which plays an important role in patient experience, satisfaction and mortality rates [see reference 149]. Evidence demonstrates that focused support for staff wellbeing through restorative supervision can have a positive impact on both staff and patients [see reference 150].
- ICSs need to develop and implement plans to invest in occupational health and wellbeing services. These should align with the national Growing Occupational Health and Wellbeing (OHWB) Together strategy along with the ICS design framework. The Growing OHWB Together strategy [see reference 151] sets an approach to improve health and wellbeing support practices to keep people well. It goes beyond reducing sickness absence, taking a preventative approach through system-wide, integrated and multidisciplinary services. Such approaches make good business sense. For example, the University of East Anglia and RAND Europe [see reference 152] demonstrate that investment of £80 per member of staff in mental health support can achieve net gains of £855 a year through savings from absenteeism and presenteeism. While local context will drive priorities, a core offer could include rapid access to mental health and musculoskeletal advice, guidance and treatment services. As set out in the Fuller Stocktake report, ICSs should look to extend occupational health and wellbeing provision across primary care organisations [see reference 153]. NHS England will work with systems and stakeholders to consider how best to complement local investment in OHWB services to keep staff well and therefore increase workforce capacity and productivity.
- Leaders and managers play a key role in creating a culture that empowers teams with the skills and resources to take ownership of their health and wellbeing, supported by health and wellbeing champions and professional nurse advocates who can provide expert advice. It is recommended that OHWB services and interventions to improve health and wellbeing are overseen by the wellbeing guardian (or equivalent leadership role), [see reference 154] and reviewed continually by local boards, drawing on evidence to assess impact and priorities for further improvement [see reference 155] – this should include data from using the NHS Health and Wellbeing Framework [see reference 156], the findings from the ‘we are safe and healthy’ section of the NHS Staff Survey [see reference 157], and the wellbeing dashboard in The Model Health System [see reference 158], where applicable.
- Good physical working environments are important for staff wellbeing, experience and retention; staff need to be given the time and space to rest and recover from their work, particularly when working on-call or overnight. The NHS Health and Wellbeing Framework [see reference 159] highlights that the importance of getting the basics right, such as providing access to good quality rest areas, food and drink options and safe storage of personal possessions, should not be underestimated. NHS organisations should review the NHS Health and Wellbeing Framework [see reference 160] and the National Standards for Healthcare Food and Drink [see reference 161] to ensure that all staff are working within an environment that supports their health and wellbeing.
- NHS England will work with ICBs and their partner trusts to ensure that their joint forward plans set out evidence-based policies, training and support for staff who experience domestic abuse and sexual violence (DASV). As part of this, ICBs and trusts have been asked to appoint DASV leads. In the UK it is estimated that 2.4 million adults (1 in 20) experienced domestic abuse in 2021/22 [see reference 162] with evidence to suggest that staff working within some healthcare professions are even more likely to experience domestic abuse than the average adult [see reference 163]. NHS England’s commitment as part of the Women’s Health Strategy [see reference 164] is to ensure women and girls who are victims of violence and abuse are supported by the healthcare system and in the workplace; this includes showing national leadership in how the NHS supports all staff experiencing DASV crimes, building on current policies and training, and ensuring that best practice is available to ICBs and trusts.
- The government is committed to reforming the system of regulation for healthcare professionals, making it faster, fairer, more flexible and less adversarial. This modernised regulatory framework will be introduced first for anaesthesia associates and physician associates, who will be brought into regulation under the GMC by the end of 2024, before the reformed legislation is rolled out to doctors, and to the professions regulated by the NMC and the HCPC over the following two years. These reforms will provide all professional regulators with similar powers, allowing them to operate a modern, fit for purpose regulatory system that ensures their registrants can be better supported and experience proportionate and efficient regulation. For example, improved fitness to practise processes will enable the safe and quick conclusion of many cases without the need for expensive and lengthy panel hearings. A more efficient system of regulation should in turn help to minimise the costs to registrants. We will encourage regulators to maximise the benefits of these reforms, ensuring that we collectively take all opportunities to enhance the contribution of regulated professions. The reform of professional regulation extends across the whole of the UK, and as such, suggested changes would have an impact on and need to be agreed across the devolved nations.
We are always learning
- NHS staff need to be supported to meet their full potential. A continuous approach to the development of staff skills, knowledge and expertise is vital to the provision of high quality care, supporting, delivering and leading high quality research, maintaining professional registration and ensuring staff have rewarding careers. Ensuring staff have access to continuing development, supportive supervision and protected time for training is a core responsibility for all employers. From 2020, employers began receiving national funding equivalent to £1,000 per person over three years to support the personal learning and development of all nurses, midwives and AHPs working in trusts and in general practice [see reference 165]. To supplement local employer investment for staff CPD, we are committed to continuing national CPD funding for nurses, midwives and AHPs. The operation of this scheme will be kept under review, to ensure subsequent funding is in line with workforce growth and inflation, well targeted and achieving the desired outcomes.
- We want to create an environment where staff are supported in their careers and where there is equality of access to learning and development opportunities. NHS organisations have a role in ensuring available career pathways frameworks and training opportunities, such as those offered through the ACCEND Programme for cancer [see reference 166], are promoted to all staff and there are plans in place to optimise uptake of apprenticeships. Similarly, Lord O’Shaughnessy’s independent review of commercial clinical trial delivery [see reference 167] highlighted some specific challenges facing research workforce careers. NHS England will work with partners to explore how best to address the issues raised. To improve the equity of learning opportunities, NHS organisations and systems are encouraged to identify how inequalities in learning and development are experienced locally and address these. Line managers should hold regular conversations with individuals about learning and development opportunities and career progression.
We work flexibly
- Our expectations of work and work-life balance are changing. Across the NHS, staff want opportunities to work more flexibly and we know delivering this is key to attracting and retaining talent. This is also true for learners, with nearly 30% of student midwives citing flexible working as a reason they were likely to recommend their placement [see reference 168]. Recognising some professions, such as nursing and midwifery, have a high proportion of women who are likely to have parental and/or caring responsibilities, flexible working is critical to supporting people to thrive. We need to evolve our approach to different employment models and shift patterns to fully embed a culture of flexible working.
- Our ambition is that the NHS continues to go beyond statutory requirements in terms of flexible working. In 2022 – to complement recent changes to the NHS Terms and Conditions of Service [see reference 169] – we worked with partners and developed a set of flexible working principles [see reference 170] for the NHS to work towards. Organisations and systems are encouraged to consider these principles and, where possible, support individuals, managers and teams to work together to explore the flexible working options available.
- Access to childcare enables people who have caring responsibilities to achieve a better balance between their work and home responsibilities. Government set out its intention in the 2023 budget to dramatically increase the availability of childcare, reduce costs and increase access.
- Building on the success of the NHS Flex for the Future programme [see reference 171], there are opportunities for organisations to work closely with system partners to consider flexible working options for every job and clearly communicate these to staff. And organisations and systems should ensure e-rostering and e-rostering metrics are regularly reviewed at board level.
- Spurred by the changing expectations of different generations, we are seeing a decline in traditional linear career models and a rise in portfolio working and employment mobility. Coupled with the need to provide more personalised care, closer to home, we need to develop the tools and infrastructure to support systems to work in new ways. In 2023/24, NHS England will work with partners to develop a national, multiprofession, integrated community and primary care core capability and career framework to support workforce development. This framework will inform flexible career pathways and support staff retention. It will build on existing frameworks to enable the development of enhanced generalist and core skills and post-registration development, and will promote routes to professional qualifications for support workers in community and primary care roles.
- The NHS should keep the door open to those who leave and encourage them to return if they choose to do so. The experience of the pandemic showed the enormous value of returners. We have continued to bring back staff through the NHS Reservists Programme [see reference 172], which expands clinical and non-clinical capacity to respond to surges in demand or emergency situations when they arise. We will improve flexible opportunities for prospective retirees to keep them for longer; and make it easier for those who have already left NHS employment to return by creating more options to come back in flexible, contracted roles or as part of the temporary staffing workforce (such as through the CaReforMe programme for doctors).
- NHS England recently announced that, from autumn 2023, all recently retired [see reference 173] consultant doctors (who hold an active registration on the GMC specialist register) will be able to sign up to a new digital platform pilot where they will be able to offer their time to the NHS and help increase capacity to deliver outpatient appointments, either virtually or in person.
- ICSs are responsible for building the workforce across health and social care settings. Flexible, integrated career pathways between health and social care can create seamless and system-wide career development opportunities for staff in both sectors, through shared recruitment, education and training, and qualifications. Employers and training providers should prioritise the development of integrated career pathways to enable the health and social care workforces to grow and thrive together.
- NHS England is working closely with ICSs and partners to review existing people management systems. The NHS Digital Staff Passport enables staff to move easily between NHS organisations, reducing unnecessary duplication of employment checks and mandatory training. Subject to successful completion of a pilot phase that is currently underway, ICSs will be encouraged to adopt the NHS Digital Staff Passport at pace. Full roll out of the Digital Staff Passport is expected to be available by August 2025.
We are a team
- The NHS is made up of hundreds of thousands of small teams and the experience of staff is largely determined by who they work with every day and their line manager’s behaviour [see reference 174]. Organisations should consider how they best support team development, using tools such as the Do OD TEAM Toolkit published by NHS Employers, [see reference 175].
- The task of leading health and care teams is changing, with managers increasingly expected to lead staff to work beyond traditional boundaries between professions and organisations, and to work as part of local systems to transform services. Collective, inclusive, and compassionate leadership is increasingly recognised as essential for delivering high quality care and cultural change throughout the NHS. The Messenger Review [see reference 176] describes how the NHS can strengthen multidisciplinary leadership and management across the NHS and adult social care through more partnership working, a greater drive on positive equality, diversity and inclusive action, and a system approach to talent attraction and development. NHS England will continue to deliver talent, leadership and management improvement interventions and will focus on the related Messenger recommendations, as well as ensuring the continued success of the NHS Graduate Management Training Scheme.
4. Reform – Working and training differently
Overview
- Growing the NHS workforce, on its own, is not enough to ensure the NHS can meet the changing needs of patients. We need staff to work in different ways, including with each other and with patients, and for clinicians to be able to spend more time with patients providing high quality care.
- We will grow the skills and capacity required to move care further upstream, delivering care closer to home and supporting people to keep well for longer. This means growing the number of NHS staff working in primary, community and mental health services as a proportion of the overall workforce.
- We will need to reform how we educate and train our staff, to support the ambitious level of expansion set out in this Plan, and ensure that we train the healthcare professionals of the future – professionals with generalist skills, who can work effectively in multidisciplinary teams. The future will also see more staff in new and enhanced roles, who will both be able to maximise their own skillset and free up the time of staff in traditional roles to maximise theirs. We will work with clinical leaders to ensure the impact of these new roles on ways of working is used to best effect.
- Productivity recovery in the short-term and continued improvements in the medium to longer-term are projected to help mitigate the scale of workforce growth that would otherwise be required. Recovering productivity is categorically not about staff working harder. NHS staff put in an incredible effort in enormously challenging circumstances – simple productivity measures will never be able to fully capture the vast amount of work carried out across the NHS every single day.
- Historically the NHS had been able to achieve productivity improvement in the acute sector through a combination of medical and operational advancement (for example, moving planned care from overnight stays to day-case settings, with surgical techniques becoming less invasive) and reducing lengths of stay for medical admissions, meaning the NHS was able to deliver more care with our workforce and infrastructure. However, limited historical investment in estate and technology is negatively impacting labour productivity.
- Looking ahead, the NHS will serve an increasingly older population with more complex needs. Productivity improvement needs to come from a combination of delivery of the same care in lower cost settings (for example, moving treatment from theatres into outpatient settings, moving hospital admissions to hospital at home, moving care upstream to reduce downstream care needs), reducing the administrative burden on clinicians through technological advancement, such as AI and robotic process automation, and delivering large-scale skills mix opportunities as well as upskilling and retaining our staff.
- These opportunities to boost labour productivity will require sustained investment in the NHS infrastructure, a significant increase in funding for technology and innovation, and delivery of the broader proposals in this Plan. The NHS is also recovering from, and adjusting to living with, COVID-19 and endemic demand on health services, which means a level of productivity recovery is also expected despite significant operational challenges health services are facing now.
- The current labour productivity measurement calculates the amount of output (activity) delivered by a given amount of input (workforce). This is largely limited to acute care only, and often not including impact from care pathway changes and service reforms across care settings. The modelling assumes that the NHS could deliver a higher level of productivity than the long run trend, with a possible range of 1.5–2% through the delivery of opportunities set out above and capturing the impact of pathway and service changes in productivity measurement. Given the inherent uncertainty of productivity impact, it is important that a range is considered to inform the likely impact on workforce demand.
- We also understand that clinicians sometimes encounter barriers that prevent them from innovating or working differently. For some clinicians, this can feel as though they are prevented from making improvements to the way they work. We will work closely with clinicians and other professionals working in the NHS, and with government and other partners, to better understand what these obstacles are and how we can work together to overcome them.
Shift skills and capacity into community
- To enable moving more care out of hospital and invest in primary, community and mental health care, the Plan will deliver a material impact on the size and proportion of NHS staff working in non-acute settings. For example, the total nursing staff working outside acute settings is projected to increase from the current 30% to 37%; and the total community workforce nearly doubles in size over the modelling period. Overall mental health and learning disability workforce demand is growing the fastest at 4.4%, community at 3.9%, primary care at 2.7% (with faster growth among non- medical professions to enhance skills mix) and 2.1% in acute settings. It is important to note that the modelling assigns all staff to a given care setting depending on their employer and their role, but does not reflect the fact that staff will increasingly be working in integrated teams regardless of their primary employment.
Digital and technological innovations
- To meet the changing healthcare needs of the population in a cost-effective way, the NHS workforce will need to take full advantage of digital and technological innovations as set out in the Topol Review (2019) [see reference 177], Data Saves Lives strategy (2022) [see reference 178] and A Plan for Digital Health and Social Care (2022) [see reference 179]. The widespread safe, effective and ethical adoption of these innovations will be one of the most important ways of delivering the stretching productivity ambitions in this Plan.
- Established in 2020, the NHS AI Lab [see reference 180] is one of the world’s largest programmes on the evaluation of healthcare AI products. The AI Award currently has 86 projects in 444 live settings, with 99 hospitals and 344 PCNs involved with 3–5-year trials showing promising results; for example, in lung cancer screening, stroke, COPD and dermatology pathways. From the developing evidence base, it is expected that AI can free up staff time and improve efficiency of services including:
- Diagnostic support: AI has the potential to free up clinical time and improve accuracy and efficiency of diagnostics in services such as ophthalmology, imaging, pathology and dermatology by acting as a first reader on images and eventually automating some clinical decisions where safe to do so. One example is the use of first reader AI technology, which will support the radiology workforce and accelerate diagnostic screening times. Emerging evidence from other trials has shown that using AI software can speed up the diagnostics pathway for patients, for example, reducing the wait for a CT scan following a chest x-ray from seven to less than three days, decreasing the amount of reporting being outsourced, and saving costs.
- Administrative automation: significant workforce benefit can be gained from the automation of administrative processes, including through AI applications such as speech recognition. Some studies have shown that over 70% of a clinician’s working time is spent on administrative tasks [see reference 181] and 44% of all administrative work in general practice can be mostly or fully automated [see reference 182]. A number of hospitals and general practices have already begun to use speech recognition technology to record clinical documentation, allowing staff to focus on patients as well as minimising manual record keeping and improving the quality of data input. The Topol Review [see reference 183] used a conservative estimate of one minute saved per patient consultation, which equates to approximately 400,000 hours of emergency department consultation time and 5.7 million hours of GP consultation time, with further savings possible should all functionalities be optimised. Wider benefits of using speech recognition include potential cost savings through bringing outsourced administrative activity, such as transcription, in-house, and reducing clinic letter turnaround times, contributing to improved patient experience.
- The potential impact of AI in the medium to long term is even greater. For example, AI is expected to support predictive health analytics, patient triage and preventive healthcare and is anticipated to speed up the process of drug discovery and design by helping with patient recruitment and data analysis. Furthermore, the impact of rapid advancements in generative AI is currently being debated across many sectors, including health. Foundational AI models inclusive of generative AI or Large Language Models, which can understand and produce an image, text and audio, are predicted to transform work across all sectors. Building on the Topol Review [see reference 184], and to ensure we take advantage of the opportunities that AI can offer, NHS England, working with government, will convene an expert group to work through in more detail where AI can best be used, and what steps need to be taken so that it supports NHS staff in the coming years.
- The successful adoption of these innovations requires continued, sustained investment in digital technologies and ongoing work to understand the impact of these technologies on staff and workforce planning, transformation and skills development. This includes capturing and driving potential changes in workflows, upskilling and training staff to maximise technologies and avoid the risk of de-skilling, the creation of new roles and responsibilities, and further ethical and legal considerations to ensure safety, accountability and fairness. To achieve this, NHS England is delivering actions including:
- Reviewing initial evaluations from the AI Award (to be completed by the end of 2024), pilots with the genomic medicines service, AI Deployment Platform [see reference 185], Medtech strategy [see reference 186] and other examples of AI implementation [see reference 187] to demonstrate further efficiencies for the workforce and provide evidence of risks that need to be addressed.
- Supporting the government’s Foundation Model Taskforce, which is set to unlock the next generation of AI, to support and optimise implementation across the NHS to improve productivity and deliver high quality, safe patient care.
- Ongoing investment in the Fellows in Clinical Artificial Intelligence programme, which has initially focused on diagnostics and is now supporting more clinical AI programmes aligned to solutions for radiotherapy, disease surveillance and patient transfers [see reference 188].
- Building the workforce’s confidence in AI, for which former Health Education England and the NHS AI Lab have set out two core foundations. Firstly, by establishing trustworthiness through governance and robust implementation of AI technologies [see reference 189] and secondly, driving AI-related education training including fundamentals for the full workforce and advanced training where it is required [see reference 190].
- Leading workforce development in AI and digital healthcare technologies as informed by the AI and Digital Healthcare Technologies Capability framework, [see reference 191] which was published in March 2023. Workforce development opportunities will be created and refined, building on the multidisciplinary nature of lessons learnt from clinical fellowships.
- Developing our understanding of the implications for the workforce and working with partners, including royal colleges, to plan for these – including considerations for specialist roles and teams as well as the wider workforce – and on system efficiencies, as technology continues to develop.
- Time spent on administrative processes can also be significantly reduced by using robotic process automation (RPA) to automate back-office tasks in the RPA increases operational capacity and speed and improves safety; it is available 24/7 and can undertake tasks 4–10 times faster with fewer errors. Most organisations report 20–30% cost reduction and 30–50% return on investment on RPA projects [see reference 192]. In 2021, NHS England set out a vision for automation capability across all healthcare systems by 2023 and the leveraging of intelligent automation to transform service delivery by 2025 [see reference 193]. All 42 ICSs now use RPA, including 38% of community or mental health trusts and 61% of acute trusts, but there are opportunities for further uptake. If all trusts implemented processes that have been ‘time validated’, this could save more than 7.2 million hours annually, equivalent to over 965,000 working days released. Over the next 10 years, this could be nearer 22 million hours saved, equivalent to more than 2.9 million working days released.
- Robotics is also transforming surgical care, through robotic assisted surgery (RAS), a newer form of minimally invasive surgery (key-hole surgery). There has been a global rise of RAS over the past 20 years across surgical specialties and it has revolutionised surgical treatment, offering benefits both to the surgeon and patient. The benefits for the surgeon include improved 3D views and better access to confined spaces by increased manoeuvrability of the ‘wrist like’ instruments. The patient benefits include smaller incisions and better cosmesis, as well as a shorter recovery time. Despite the rapid growth in RAS, there is no formal process for providing robotic training in the UK or Europe, and unregulated adoption has the potential to lead to significant patient harm. NHS England is collaborating with the Royal College of Surgeons of England, the accrediting surgical bodies, and the robotic industry providers to build a framework for a robotic curriculum. The aim is to create a roadmap for implementing the curriculum, which will identify barriers to training and offer solutions to overcome them. This will lead to provision of a fully trained, accredited RAS surgical workforce with demonstrable patient benefit.
- There are also opportunities to use technology in primary care. In future, hub and spoke models and automated dispensing will reduce the time pharmacists, pharmacy technicians and dispensers spend on direct medicines supply. Modelling estimates that hub and spoke dispensing will increase 2% a year, which will release capacity across the community pharmacy workforce to support a greater focus on delivering clinical services. We also anticipate that with the right support and investment community pharmacies can make efficiency savings by switching to paperless systems.
- Remote monitoring brings diagnostics and monitoring closer to the patient across primary, community and acute services. It provides up-to-date intelligence to support care decisions, relieve pressure on the workforce and empower patients to self-manage conditions, and facilitates earlier detection of escalation of conditions. Use of remote monitoring increased during the COVID-19 pandemic; this reduced emergency department attendances and hospital admissions from care homes, and improved patient experience [see references 194, 195]. NHS @home was a key contributor to the pandemic response, introducing COVID-19 Oximetry @home, COVID-19 virtual wards and Blood Pressure @home. Since November 2020, over 1 million pulse oximeters have been distributed to support safe management at home and provide faster access to care when needed. In the 12 months to March 2023, 1.9 million people used a blood pressure monitor at home, submitting readings to their GP, supporting self-management and saving GP time. Work is underway to expand NHS @home pathways and this includes developing and testing new approaches for managing major conditions such as cardiac and respiratory disease. Investment in 2023/24 via the Adult Social Care Technology Fund is also supporting testing of remote monitoring solutions to help people live more independently in their own homes and communities, reducing incidents such as falls, increasing people’s quality of life and reducing avoidable hospital admissions.
- Government’s data strategy for health and social care [see reference 196] sets out guidance and support for ICSs to make digitally enabled care mainstream, confirming the requirement for good quality data and data systems to underpin effective, integrated working. Data platforms can support effective staff deployment and strategic workforce decision-making through e-rostering and e-job planning. Benefits include improved workforce data at every level, financial savings, fewer unfilled shifts and faster rostering.
- In 2023/24 NHS England is procuring a Federated Data Platform (FDP) to better connect the NHS. The FDP will connect existing systems, making it easier for staff to access the information they need in a safe and secure environment so that they are better able to co-ordinate, plan and deliver high quality care. This software will be ‘federated’ across the NHS, meaning providers and ICBs will have their own platforms which can connect and collaborate with other platforms as a ‘federation’, making it easier for health and care organisations to work together. A digitised, connected NHS can deliver services more effectively and efficiently, with people at the centre. The ICS workforce will have the insights they need to proactively plan services around people’s needs and co-ordinate care across the services in their geography. Trust staff will be able to access the information they need, in one secure place, freeing up time spent on administrative tasks and enabling them to deliver the most appropriate care for each patient. Several pilot programmes are already making an impact in trusts across England focusing on elective recovery and effective hospital discharge.
- An example of innovative technologies being accelerated to improve flow of clinical data and process across a pathway is the Diagnostics Digital Capability Programme, where investment and support into pathology and imaging networks to implement new technologies is expected to increase productivity across imaging and pathology services by up to 10% by March 2025. Investment is also expected to enable faster turnaround times for diagnostic test results (supporting the delivery of national service delivery standards, such as urgent faster diagnosis standards for suspected cancer cases and six-week diagnostic waits), improved patient and staff experience, and reduced outsourcing spend.
Bringing people into the workforce more efficiently
- To support ongoing reforms, including enhancing students’ experience as they complete academic and clinical requirements, and to expand placement capacity, we will:
- Promote uptake by education institutions of the opportunity for newly qualified nurses to join the NMC register on qualification at the end of the third academic year. This permits new registrants to be in paid employment up to four months earlier and can reduce employers’ reliance on temporary staff, reduce costs and vacancies. It also gives new joiners time to get embedded ahead of the winter months when pressures on health services are typically at their highest. Some education institutions already enable this.
- Work with the NMC on its welcomed commitment to explore the potential for further changes to nursing degrees. To train staff more flexibility, taking into account the opportunities presented by EU exit and leveraging new technologies, we encourage the NMC to consider how graduate nurses can join its register after fewer practice hours, mirroring the approach in many other countries, and enabling the increase in training capacity set out in this Plan. A reduction in placement hours from 2,300 to 1,800 over the course of a nursing degree would reduce pressure on our learners while significantly increasing placement capacity across the NHS to give pre-registration students the high-quality learner experience they need to prepare to work in the NHS.
- Funding will continue for the shortened midwifery course in 2023/24 and 2024/25. This provides registered nurses with a two-year programme to become registered midwives and will lead to the registration of over 1,000 more midwives by 2026.
- Likewise, as part of paramedic expansion, and so that training delivers system-facing graduate paramedics, we will ensure funding for MSc two-year paramedic programmes. Students will be able to enter the workforce as a registered clinician within two years, rather than the traditional three years, therefore increasing supply.
- We will continue to work with higher education institutions (HEIs) to maximise recognition of prior learning (RPL) and accredit prior experiential learning (APEL). Learning or practical experience that is gained in one field of practice can, in some circumstances, be accredited and used to reduce the time it takes to gain another qualification. There are a number of examples of where this is already working in practice. For example, a nursing associate who has completed their two-year training programme (achieving a Level 5 foundation degree) can go on to complete a nursing degree programme and have their previous training accredited so that it counts towards 50% of the credits needed to complete their nursing degree. Expanding these opportunities will help support multiple entry routes into health careers and make education pathways as efficient as possible; widening access and attracting more students. It will also support learners to progress. NHS England has commissioned Middlesex University and partners to establish standardised approaches for recognising previous learning within the healthcare sector, to support people who do not follow a traditional career path. These are due to be published in 2023/24.
- For medical training, EU exit provides the potential for greater flexibility to recognise prior learning and experience towards attaining a degree, which goes beyond what is currently recognised – one year for graduate entry programmes. We will work with the GMC and medical schools to explore options for a shortened medical degree programme which would be available for some existing healthcare professions such as pharmacists and paramedics. Individuals and employers benefit from APEL as the route to registration is faster and individuals can join the workforce more quickly. It also frees up HEI and clinical placement capacity as programmes can be delivered over a shorter timeframe. Doctors training in this way would of course need to achieve all the usual required standards and outcomes for graduates set by the GMC.
- We will support changes to the registration processes for domestic graduates and international recruits, to make entry into NHS employment more efficient. Regulators should have the right tools to continue to develop their registration processes through legislative changes that provide them with the flexibility they need.
- The medical support worker programme provides a stepping stone for permanent UK residents who hold a non-UK primary medical qualification but are non-practising, to gain clinical experience in the NHS while they work towards GMC registration. In the past two years we have supported about 1,000 medical support workers to attain a full licence to practise, allowing them to seek employment as a doctor. We will promote and develop this programme in the short to medium term, as a sustainable cost-effective option for supporting the medical workforce.
- We are committed to seeking better value for the significant investment that the taxpayer makes in the education and training of the dental workforce. This Plan proposes we do more to support and encourage qualified dental professionals to spend a greater proportion of their time delivering NHS dental care. One approach we will consider with government is to introduce incentives or other measures, such as a tie-in period, that encourage dentists to spend a minimum proportion of their time delivering NHS care in the years following graduation. We will also explore opportunities to support the professional development of dentists and dental care professionals, and to give the NHS workforce fulfilling career paths with potential to use their full scope of practice, and consider how to minimise the bureaucracy around starting to practise in the NHS.
- We will work with stakeholders to explore the potential for contractual or other mechanisms to better incentivise doctors and other healthcare professionals to work in known underserved geographical areas, and to encourage retention during the early stages of their careers.
Educating and training the workforce differently
- As well as the need to train more people, education and training needs to be fundamentally different. To care for ever increasing numbers of older people with multiple and complex conditions, health and care professionals will need to continue to enhance their specialist knowledge while also maintaining and developing their generalist and core skills. This will support health and care professionals to work in multidisciplinary, integrated teams that respond to population health needs and effectively deliver care in communities [see reference 197]. The way we train staff also needs to address predicted future workforce shortfalls [see reference 198], match differing generational expectations and meet the needs of those joining the workforce in future.
Improving student and learner experience
- In 2023/24 we will work with students, HEIs, royal colleges and clinical placement providers to understand and address the reasons students leave training and the variation in their experiences. Training attrition varies across the country, particularly for nursing. This Plan supports the existing commitment to reduce the proportion of students who leave nursing training from 16% in 2019 [see reference 199] to 14% by 2024. We will also aim to bring the attrition rate down to 14% for paramedics and operating department practitioners (ODPs).
- Preceptorships provide a structured start for newly registered nurses, nursing associates and midwives, to help them integrate into their new team and place of work. However, we know that the quality of preceptorships varies. To ensure consistent delivery, and a high-quality preceptorship experience for all early career nurses and midwives, we will support trusts to adopt the National Preceptorship Framework [see reference 200]. Likewise, good quality preceptorship is key for the wider workforce as well and guidance is available to set out best practice.
- Working with partners, we propose to introduce a single, consistent policy for funding excess travel and accommodation costs incurred by students undertaking placements. Currently, this funding is inconsistently paid to students, creating inequity.
- In 2023/24 we plan to continue the development of a national learning hub, providing a single point of access for learning. The Learning Hub platform [see reference 201] will offer high quality, educational material at scale across the NHS, enabling ease and equity of access for all, at a time and place of the learner’s choosing. This will improve user experience and utilisation and save learners the time and costs of travelling to in-person training. It also has the potential to drive the adoption of innovative methods and practices in all areas of the workforce, crossing organisational boundaries and boosting system working.
Widening participation and supporting all to succeed
- We will work to widen participation in education and training, so the NHS workforce is representative of the communities we serve, and students gain the skills, knowledge and experience they need to deliver high quality care to a hugely diverse population. Implementation of this Plan will help tackle health inequalities by increasing the supply of staff in underserved areas and targeting investment to achieve equitable access to education, drawing on programmes such as the Core20PLUS5 [see reference 202]. ICBs would need to work with their system partners to maximise how the NHS works as an anchor institution to expand access routes into training in the NHS. An example programme is Halo Southend [see reference 203], which offers entry-level training to eligible unemployed people who are looking to pursue a career in health and social care, and is funded by Southend Council. And the internship programme for young people with a learning disability and autistic young people, run in partnership with South Essex College, that is giving students work experience across hospital departments [see reference 204].
- We are committed to ensuring that all NHS-managed education and training, either through NHS-employed trainees or where we directly commission education, represents best practice in ensuring inclusivity and diversity. We will work in partnership with the Office for Students, Department for Education and HEIs to achieve this. We will build on the Medical Schools Council’s framework that supports medical schools to make their environments and processes more inclusive [see reference 205].
More diverse and integrated clinical placements
- We anticipate that as ICSs become more involved in education and training planning, there will be an opportunity to develop more multiprofession, system-based rotational clinical placements. This would include extending the provision of placements across primary, community and social care, and in the independent and voluntary sectors, to give students valuable experience in the delivery of care outside hospitals and introduce them to wider career opportunities.
- We will ensure that all foundation doctors can have at least one four-month placement in general practice by 2030/31. At present, opportunities for such placements are variable across deaneries. This will give doctors in foundation training an understanding of work in primary care. We will also increase training and supervision capacity in primary care so GPs in training can spend the full three years of their training in primary care settings.
- Planning the NHS workforce over a proper long-term timeframe provides a major opportunity to support the medical profession in reshaping itself to meet future patient needs. Over the past decade there has been a growing professional consensus that medical training needs to change with a better balance of generalist and specialist skills that equips them to provide joined-up care for patients with multiple morbidities. This is an important strategic objective and we will work closely with medical schools, royal colleges, the GMC and employers to support the profession in making this agenda a reality. We will support ICSs by expanding the seven existing pilots (trailblazers) to demonstrate the benefits of more generalist approaches to education and training. The pilots were launched from August 2022 with around 200 learners – wider implementation is planned from August 2023. The ambition is to expand the trailblazers so there are pilots across all medical specialties and regions by August 2025. Subject to pilot outcomes this will become an established part of medical education training. They present opportunities for existing trainees to develop and maintain their generalist and core skills by undertaking placements across a range of healthcare settings. Trainees support integrated care for patients with multiple chronic conditions and apply knowledge and learning to reduce health inequalities and address local health priorities.
- Building on that, we will expand the NHS’s Enhance Programme [see reference 206], a professional development programme to enhance generalist skills across the first five years of postgraduate medical education, so that this programme is in place for all doctors in training by 2025. This complements current medical training and aims to broaden the generalist and core expertise of clinical professionals during early training, expanding across different specialties and more locations; for example, expanding the pilot training programme in general internal medicine without specialisation. These initiatives will help ensure all doctors have access to enhanced generalist skill development at core stages of their training, and greater support to develop these skills as they progress through their careers.
New approaches to medical education
- SAS doctors form an increasing proportion of the medical workforce, including at a senior level. Traditionally, these roles predominantly focused on clinical service provision, although feedback from this group indicates their growing desire for greater opportunities in a non-patient facing capacity, such as leadership, mentoring, and education and training. We are committed to working with DHSC, legislators and employers to support SAS doctors to have a better professional experience, by improving equitable promotion and ensuring options for career diversification.
- Locally employed doctors (LEDs) are another rapidly growing group. The number of SAS doctors and LEDs on the GMC’s medical register has increased at six times the rate of GPs [see reference 207]. LEDs are a huge asset to the NHS. They generally undertake more junior roles, requiring direct or indirect supervision. Despite their considerable input to the medical workforce, we have limited data on their experience, skills, ethnic diversity and geographical distribution, and they have few structured career development options outside specialty training. We are committed to working with partners to review medical career pathways and identify ways to better support postgraduate career progression for LEDs, including routes to progress their careers into high demand specialties such as cancer.
- To support doctors in training pathways and those in LED posts, building on the Out of Programme Pause (OOPP) pilot, we will work with the GMC and devolved nations so that taking out of programme opportunities becomes a more accepted part of the training pathway. This would retain more doctors in training by facilitating the return of those who want or need to take a break, and on their return accelerate their training when they have gained competencies working as an SAS doctor or LED. The pilot is ongoing at present, accepting new trainees until the end of July 2023. It is undergoing a three-year external evaluation to be published in summer 2023. Subject to outcomes, the aim is to offer this broader approach to out of programme opportunities and valuing the competencies gained to all trainees in England as early as 2024/25.
- Autonomy and flexibility around career planning is of growing importance to the junior medical workforce and we know that active acknowledgment of this will facilitate a valued and healthy professional experience, in addition to supporting long-term workforce retention. Portfolio careers of senior medics balances clinical responsibilities with educational, leadership, management and research roles, a practice that when replicated for doctors in training would generate a more generalist, agile medical workforce. We will work with partners so that there is more flexibility and a broader range of career pathways and opportunities are available to the medical workforce from early in their careers.
- We will work with stakeholders and government to ensure that doctors other than GPs are more easily able to work in primary care. This will give general practice additional capacity, improving patient access as well as creating opportunities for these doctors to develop and progress in their careers.
- The Certificate of Eligibility for Specialist Registration (CESR) and Certificate of Eligibility for GP Registration (CEGPR) [see reference 208] are alternatives to traditional specialty training; they support progression to gain specialist registration and thus the ability to work as a consultant or GP. These exemplify the GMC’s work to provide pathways that add flexibility to specialty and GP specialty training to help doctors, including those trained overseas or working in a non-training grade role in the NHS, gain entry to the specialist registers. We will work with the GMC and NHS employers to support doctors to develop their skills and progress through their careers.
- Through the Medical Education Reform Programme, [see reference 209] we are working with partners to improve training to meet the changing needs of patients and citizens, and to support the aspirations of doctors in training. We know that to generate a skilled medical workforce, and one that feels valued, all elements of training must be optimally and equitably delivered across the country. Quality assurance is intrinsic to the patient care we deliver as a system and should be to the training delivered to those who provide care. In 2023/24, we will use our established quality assurance training framework to share best practice with ICSs, supporting them to ensure all providers meet the required standards to deliver robust, high-quality training. This will improve outcomes for patients and optimise retention of doctors in postgraduate medical training within the NHS.
- In 2024/25, we aim to pilot an internship model for newly qualified doctors to trial shortening undergraduate training time, with a view to improving preparedness for practice. This will involve medical students graduating six months earlier and entering a six-month remunerated internship programme. We will work with partners to ensure internships can be delivered safely and effectively.
- The introduction of a Medical Licensing Assessment from 2024 will ensure that graduating doctors have met a common set of outcomes-based standards. We welcome this and will work closely with medical schools and the GMC to develop four-year undergraduate medical degree programmes so that in future students undertaking shorter medical degrees make up a substantial proportion of the overall number of medical students.
Addressing geographical inequity
- The location of training posts, often based on historical arrangements, does not always mirror current or future patient need, leading to inequitable access to services in some areas. There are, similarly, entrenched inequalities in the distribution of staff – with disadvantaged areas, particularly some coastal communities, finding it harder to attract and retain staff – that need to be addressed. As we begin to reform education and training, we aim to tackle these inequalities where possible, without unnecessarily delaying the expansion of training. With a period of growth that would result in doctors in training, we would aim to align additional posts to areas of greatest need.
- To level up undergraduate training we propose focusing new medical schools and additional places in geographical areas with the greatest staff shortfalls and unmet healthcare need. This will also promote applications from local populations, bringing employment opportunities to more socially deprived locations. A good example is the partnership between the University of Cumbria and Imperial College London to launch a new graduate entry medical school in Carlisle. Accepting its first graduates from 2025, training will have a community healthcare focus, to provide doctors who can respond to the complex health and care challenges locally. By the time the students qualify they will have become embedded into the local ICS, encouraging them to continue living and working in the local area after graduation. We will work with partners to ensure these proposals give doctors autonomy and flexibility across their career paths.
- As part of this Plan, we would aim to further adjust the distribution of postgraduate specialty training places. A higher proportion of the new 2024/25 cohort of 1,500 additional medical students will carry out their postgraduate training in parts of the country with the greatest shortages and in services such as primary care, mental health and cancer. For future increases, we will continue to apply distribution methodology so there is a continuous pipeline to grow the future permanent medical workforce where it is needed most. This will mean training posts in obstetrics and gynaecology, anaesthetics, internal medicine stage 1 training and core surgical training would better reflect population needs.
- Imbalances in geographical distribution of training posts is not confined to medical training. Other professional groups also require a more equitable spread of training opportunities, based on current and future patient need. ICSs will be able to consider local needs and respond to geographical inequity, via reform of education funding policy, and increased use of apprenticeships and blended learning opportunities. Work is already underway within pilot ICSs as part of the rural and coastal workforce transformation programme to implement education, training and workforce transformation solutions, aimed at improving attractiveness of jobs and retention of the healthcare workforce in these locations. We will work closely with systems to consider the best approaches to reviewing geographical distribution of training posts for wider professional groups.
- In dentistry, work is already underway through the establishment of Centres for Dental Development to bring together dental education and training with service delivery models, particularly in areas where there is a shortage of workforce relative to population need. More detail will be provided in the upcoming Dental Plan.
Adapting the structure and delivery of education and training
- This Plan commits to doing more to leverage opportunities to fully embed digital technology in training pathways, to support more efficient and effective ways of learning and improved learner experience. We have developed an innovative blended learning nursing degree, which uses a method of teaching that integrates technology and digital media with traditional instructor-led classroom activities, giving students more flexibility to customise their learning experiences. This will both increase capacity and help attract a more diverse student nurse population as an element of online learning can make it easier for those in areas that lack clinical placements, for example, remote, rural and coastal areas, to participate. Nationally we awarded tenders to seven universities and the first blended learning registered nurse programmes started in early 2021. Due to interest, this model has been expanded to midwifery, anaesthesia associates and medicine. NHS England is commissioning an independent evaluation of all the blended learning programmes, to be completed in the next year.
- The significant growth in use of immersive technologies is beginning to revolutionise healthcare education, and in 2023/24 we will continue to support their adoption. Technologies such as extended reality, combined with virtual learning environments, can support hybrid education and the workforce to deliver high quality, safe care, and have the potential to deliver significant efficiencies compared to traditional classroom education [see reference 210]. We will further expand the Virtual Hybrid Learning Faculty and Simulation Faculty programmes [see reference 211]. These support educators to design and deliver simulation to underpin growth in education capacity, including with the use of immersive learning technologies and blended learning approaches.
- Increased simulated learning provides learners with opportunities to enhance their critical thinking and decision-making skills and gain insights into complex areas of healthcare provision that they may not otherwise access in their training. Simulation also enables greater flexibility in how clinical hours are achieved, improving consistency for students and facilitating expansion of placement capacity. We will encourage and support HEIs to adopt – at pace – the NMC’s new standard allowing up to 600 hours of practice learning to be undertaken via simulation, an increase from 300 hours in November 2021. As well as benefitting students, this can reduce the pressure on health and care providers of providing sufficient practice placements. Where simulation training is equivalent to clinical placements, this will attract the national clinical education tariff. In addition, national funding of £300,000 is being made available to HEIs to develop expertise to support the initiative. To support the expansion of simulation training for nurses, £15 million of investment to HEIs was made available in 2021/22 to increase simulation capacity for AHPs and doctors.
- We will work with regulators, education providers and students to review the structure of undergraduate degree programmes on improving the structure of pre- registration training across professions. For example:
- We will work with partners to develop opportunities to extend dual registration courses in children and young people and learning disability nursing. These courses allow students to train in two areas of nursing and provide the opportunity to become a registered nurse in both fields. Students are expressing growing interest in dual registration courses, and they can encourage more registrations in areas of nursing, such as learning disability, that over recent years have not attracted sufficient numbers to deliver standalone courses. We will work with partners and stakeholders to ensure that there are opportunities for dual registrants to maintain their skills and develop across both registrations.
- For ODPs, level 1 theatre first assist training and increased critical care skills are being built into pre-registration training. This will maximise the workforce benefit they bring on graduation and drive transformation through overt recognition of skills.
- For paramedics, this will include building increased community and primary care preparation into pre-registration training.
- We plan to work with the Medical Schools Council, Dental Schools Council, HEIs and other partners to incorporate compassionate leadership and workforce psychological wellbeing within undergraduate curricula, and to promote informed postgraduate career guidance.
- To address the unwarranted variation in clinical placement hours in some professions – for example, ODPs and paramedics – we will support a review of the variation, aligned to the outcome-based clinical hours models in the college curricula.
- We will consider training requirements for specialised services, both in terms of training for specialist staff and the wider upskilling that may be needed across the workforce to support patients. For example, we will implement four to six thrombectomy training academies across England to provide sufficient trained staff to operate a universal 24/7 thrombectomy service. Additional specialist training in gender dysphoria will be provided to meet the workforce shortage in this specialist service; we will raise the awareness of this patient group across the workforce and support healthcare professionals to signpost and support patients.
Enablers supporting education and training expansion and reform
- We will work with HEIs and system partners to plan and deliver the education expansion and reforms set out in this Plan. For all clinical professions, successful expansion would be contingent on there being an expanded and fully trained supervisory workforce to support evolving learner and workforce need.
- As well as expanding educator capacity, we need to address the challenge of expanding the physical estates capacity for supervision to take place in parallel. This is particularly critical in primary care where insufficient physical space across an ageing estate limits GPs’ ability to increase training placements. Various initiatives are planned or underway to explore models of supervision and estates that increase access and capacity, but as this is a broader challenge than training and equipping the workforce to deliver for patients, it is outside the scope of this Plan and will require continued, sustained investment in the primary care estate.
- Clinical academics – within medicine, nursing, midwifery and other professional groups – work across healthcare providers and academic institutions, combining clinical work in the NHS with research and/or teaching activities. They provide a bridge between the two; insights from clinical practice inform research, and innovation and research can rapidly be translated into improving care for NHS patients. This close working between the NHS and academic partners ensures the UK remains a scientific powerhouse. Clinical academics are crucial to training future generations of healthcare professionals, by leading on research and delivering much of the teaching of students. As the number of training places increases across professions, more clinical academic posts will be needed.
- We are working with DHSC to review the NHS education funding policy and deliver the Education Funding Reform Programme (EFRP). The aim of the EFRP is to develop a new and agile education funding policy for healthcare education and training in England. This should be transparent and encourage quality and productivity, while representing value for money and aligning with wider service and education strategies.
Capacity of educators, supervisors and trainers
- We recognise educators’ important role in developing the current and future workforce, both in universities and across clinical practice. A new Educator Workforce Strategy [see reference 212] was published in 2022/23 setting out the actions that will lead to sufficient capacity and quality of educators to allow the growth in the healthcare workforce needed now and in the future. This includes planning for career pathways both in practice and in higher education institutions and across sectors and professions. Recognising educators and their value, and detailing initiatives to support them, will raise the profile of this essential workforce, and help to expand the educator pool.
- Management of the number, spread and quality of clinical placements is a concern across healthcare education and training, and for learners. Growth in placements has been challenging for several years, usually attributed to a lack of capacity and supervision, and this restricts the breadth of learning opportunities on offer to students. We will work with stakeholders, informed by the issues we identified through a discovery exercise in 2022/23, to ensure clinical placements are designed into health and care services, and placement providers know what core standards they need to meet. Co-design of a nationwide approach to clinical placement management will place students at the centre of placement management and practice, with consistent and clear national core standards for placement providers. It will enable a more strategic view of capacity so that the NHS can work more effectively with the education sector to ensure the right volume of training, in the right settings, for each profession and better support for placement providers, as well as better meet the needs of students.
- Placements are important for attracting new staff to those specialised services that can find it particularly hard to recruit. For example, in the health and justice workforce and secure mental health services, increasing the number of clinical placements and preceptorship opportunities would help to raise the profile of services and attract more staff to the sector. The same can be said about the need to raise the profile of those services concerned with less prevalent diseases, by increasing placement opportunities. For example, the NHS will introduce 10 clinical fellow posts into sickle cell disease services from 2024/25.
The step change needed in education and training planning
- Implementation of this Plan will need a new approach to system-wide integrated workforce planning and redesign, and adequate education supply is central to this. Service providers, ICSs and NHS England will all have a role in leading and commissioning sustainable education supply, including the supply of educators. To support this, we will continue to build strong relationships with the education sector and our key partners in HEIs and other education bodies.
- To support ICSs, from 2024 we are committed to moving to a position where nationally, education and training plans are formulated at least three years in advance. This would support a more strategic approach to delivering the right pipeline of staff across the NHS, thereby minimising inefficiencies and delivering better value for money.
- Planning at system level will strategically focus NHS investment in education on medium and long-term system workforce needs and will ensure that education placement capacity is integrated into service planning within annual operational plans. In their first joint forward plans, ICBs will aim to plan across settings, including primary care, and will consider all modes of education and training, including apprenticeships, peer-to-peer learning and accredited programmes. They will consider the development and retention of existing staff and how education capacity should be developed in key service areas, including the support required to provide high quality education such as supervision and clinical placements.
Optimising multidisciplinary teams
- This Plan sets out an expansion of new and extended roles to increase the breadth of skills within multidisciplinary teams, better meet the needs of patients, their families and unpaid carers, and enable more care to be delivered in primary and community settings. The NHS is determined to continue to invest in training opportunities and the development of career paths for the whole workforce. Some of the key roles for expansion are identified in Table 3, and examples of how they can be used are detailed below. The assumed impact of these roles is based on a combination of literature review, case studies and clinical and professional engagement.
Table 3: Key roles for expansion
| Roles | Estimated supply by 2036/37 |
|---|---|
| Nursing associates | 64,000 |
| Physician associates | 10,000 |
| Anaesthesia associates | 2,000 |
| Advanced practitioners | 39,000 |
| Approved clinicians (mental health) | 1,000 |
| Roles covered by further expansion of primary care MDTs | 15,000 |
| Roles covered by primary care nurse expansion | 5,400 |
- Expanding these roles will release time for more experienced clinical professionals to provide the training and care delivery that only they can do. When implemented successfully, these roles can increase productivity by ensuring there is sufficient workforce capacity, making reliance on temporary staffing less likely.
- As the number of older people with multiple and complex conditions increases, clinicians and care professionals will need to enhance their specialist knowledge while also maintaining and developing their generalist and core skills. This focus on skills is a vital part of this Plan, to spread and embed future models of care that meet the needs of our population, such as virtual wards, same day emergency care (SDEC) or community models of mental healthcare. The assumptions about the skills required reflect the ambition to deliver more care closer to home wherever possible, reserving acute hospital care for those who need it most. In addition, staff with enhanced generalist and core skills will have the potential to move into a variety of different areas and care settings throughout their careers.
- We can support professions with the largest shortfalls by increasing the numbers of supportive and complementary staff. Overall, the Plan will increase the proportion of these wider team roles from 1% in 2022 to 5% by 2036/37. In addition, this Plan focuses on expanding those roles that have a particularly diverse range of skills and can contribute in many care settings, including 3.7–4.0% growth in paramedics, 3.4– 3.7% growth in occupational therapists and 3.3% growth in physiotherapists (assessment of average growth rates per year).
- The need for parity of esteem between physical and mental health is also reflected in the anticipated workforce shift between care settings, with the proportion in community care, primary care and mental health needing to increase substantially.
- To help facilitate an optimised skills mix, we will train more nursing associates (NAs), with 5,000 NAs due to start training in 2023/24 and 2024/25. This Plan estimates a need to incrementally increase that number to 10,000-10,500 per year from 2031/32. Our modelling suggests that if this were implemented, growth across new and traditional roles means that in future, there will be 64,000 nursing associates working in the NHS, compared to about 4,600 now [see reference 213]. This Plan sets out an ambition to more than double NA training places to 10,500 by 2031/32. To support this, training places will increase by 40% to 7,000 by 2028/29. This expansion is set out alongside the assessment for substantial growth in the registered nursing workforce, detailed earlier in this Plan, and could be achieved via both apprenticeship and direct entry routes. NAs work as part of the wider nursing team, bridging the knowledge and skills gap between healthcare support workers and registered nurses. The role was introduced following the Shape of Caring Review [see reference 214] to add capacity to the nursing workforce; the skilled support they bring for delivery of treatment and care allows registered nurses to lead care planning and assessment. NA roles provide opportunities for healthcare support workers to progress in their careers and grow their skills, helping improve their retention in this critical workforce group. Research has shown that over two thirds of NAs would like to go on to train as a registered nurse, providing an additional route to expand nursing numbers [see reference 215]. It is anticipated that a large proportion of the new NAs suggested as part of this Plan would be existing healthcare support workers, but they would also be recruited from the wider labour market and other NHS roles.
- From 2023/24, around 1,300 physician associates (PAs) will be trained a year. This will increase to over 1,400 a year in 2027/28 and 2028/29, supporting an ambition to increase training places to over 1,500 by 2031/32. This Plan emphasises the need to focus this expansion on primary care and mental health services. PAs are medically trained generalist healthcare professionals with an undergraduate degree in a life science and/or a significant background in healthcare. Bringing PAs into regulation by the General Medical Council (GMC) will enable expansion of their scope of practice, with the potential for them to be given prescribing responsibilities in the future, subject to the necessary approvals. Regulation will therefore enable PAs to make an even greater contribution to the NHS workforce. We would commit to doing further work with partners to develop appropriate career pathways for these roles as the number employed increases.
- Anaesthesia associate (AA) training places will increase to 250 by 2028/29. This will support our ambition to increase places to 280 a year by 2031/32. AAs are highly trained, skilled practitioners that work within an anaesthetic team under the direction and supervision of a consultant anaesthetist. They help alleviate the surgical backlog and reduce the future workforce shortfall created by increases in demand as part of the wider anaesthetic team. In 2022, there were 160–180 AAs registered on the Royal College of Anaesthetists’ AA Managed Voluntary Register [see references 216, 217, 218]. National funding is supporting the training of 120 a year over two years until March 2024. Despite the help they offer in alleviating the surgical backlog, uptake and deployment of AAs is currently variable, but it is anticipated this will improve with the upcoming move to bring AAs into regulation by the GMC, with the potential for them to be given prescribing responsibilities in the future, subject to the necessary approvals.
- Enhanced practitioners are qualified health and social care practitioners who have attained specific applied knowledge and skills in their field. National funding is available to train 150 enhanced practice radiographers a year to support the diagnosis of cancer and other conditions, and to support every general practice to have a musculoskeletal first contact practitioner (FCP) by 2032/33, two roles that have demonstrated considerable service benefits. There is now an enhanced clinical practitioner apprenticeship standard to enable employers to invest in developing this workforce through the apprenticeship levy. An enhanced clinical practitioner apprenticeship with critical care outreach specific content will be launched in 2023, through collaboration with the Intensive Care Society. The two-year programme will be aligned to the Critical Care Outreach Practitioner Framework [see reference 219] and will be open to both existing and new entrants to critical care outreach. With funding available for 300 places in 2023/24, the course will help upskill the adult critical care workforce, bolstering retention and recruitment. This work is central to the development of the upcoming adult critical care workforce strategy and implementation of the NHS People Plan.
- Over 3,000 clinicians will start advanced practice pathways annually from 2023/24, tailored to support service demand. This will increase by 46% to 5,000 by 2028/29, supporting this Plan’s ambition to have over 6,300 clinicians starting advanced practice pathways each year by 2031/32. Advanced practitioners work at the next level, after enhanced practice. They are experienced, registered health and care practitioners who have completed advanced practice education and training at master’s degree level. Areas of demand for advanced practice include emergency medicine, primary and community care, mental health, learning disability and autism services, acute care services and specialist services like those for breast cancer.
- SDEC will require more advanced practitioners and this Plan sets out a need to train around 150 advanced paramedics a year from 2023/24 to support this. Intermediate care, which aims to reduce length of stay for those who no longer meet the criteria to reside in an acute hospital, will need more non-registered staff and support with their wider retention, such as through the increased use of apprenticeship schemes. In support of this, work to establish community advanced practice credentials is planned over the next two years to 2024/25.
- Advanced practitioners increase the number and type of senior clinical decision- makers supporting patients and offers options for clinical career progressions for more experienced staff. For example, advanced practice dietitians working in primary care in Birmingham are employed and supported by the community trust. This model enables people to access early expert diagnosis and treatment in primary care and stay in control of their symptoms to remain in school or work. In the first year it has avoided 600 appointments that otherwise would have been with a GP, reduced prescribing costs of oral supplements by £70,000, supported the education and training of the wider team and care home staff, as well as met a local need for more weight management and respiratory services [see reference 220].
- Within NHS specialist services, advanced practice can increase capacity in areas with a limited workforce and offer career development opportunities, for instance, within community diagnostic centre teams. Advanced practitioners are making a real difference to the support patients receive – for example, pre and post cardiac surgery – and are proving vital for the delivery of quality care for patients.
- Work is underway to develop formal pathways to facilitate the transition for the most experienced and skilled staff from advanced to consultant practice roles, and to create pilot development programmes for consultant practitioners, with an initial focus on learning disability and autism, cancer, integrated imaging and musculoskeletal pathways [see reference 221]. The multiprofession consultant-level practice capability and impact framework sets out the capabilities consultant practitioners need to demonstrate and their potential impact across the four pillars of the multiprofession consultant-level practice capability and impact framework [see reference 222]. Consultant practitioner roles have been developed largely in services that already have an established, experienced advanced practice workforce with the capability to develop their skills further.
- Expanding skills across MDTs by upskilling and introducing new roles should be done with the service model in mind, ensuring there is alignment between the skills of the workforce and patient need. In acute hospital settings, development of the extended surgical, anaesthetic and perioperative care team and promoting a modern, inclusive culture, can improve training, safety and the quality of care, and meet the demands of elective and emergency care for the future by improving surgical productivity. The extended surgical team can include advanced practitioners, surgical care practitioners, physician associates or medical support workers among others, offering career development for the wider non-medical workforce. Evaluation of the first two years of a three-year pilot demonstrates that this multidisciplinary way of working improves the consistency of clinical care to surgical patients, smoothing transition and handover. Similarly, the perioperative care team supports patients on their journey from contemplation of surgery through to the procedure itself and onto post-operative care and follow-up. Improvements to the perioperative care model, incorporating earlier preoperative health screening and optimisation, and increased access to day surgery, enhanced recovery pathways and enhanced care services, will be supported by expanding our core workforce to include associates, support workers, care co-ordinators and advanced practitioners.
- In general practice, we will seek to extend the success of the Additional Roles Reimbursement Scheme (ARRS), which has delivered an additional 29,000 multiprofessional roles in primary care [see reference 223]. This would build extra capacity and free up available appointments by increasing the number of non-GP direct patient care staff by around 15,000 and primary care nurses by more than 5,000 by 2036/37. This expansion would be carefully managed taking into account additional training of pharmacists, to ensure the growth in workforce is sustainable, and considers the additional capacity required to staff roles across primary care.
- Community pharmacies are increasingly providing clinical services, such as vaccinations and blood pressure checks, as well as piloting initiation of contraception. The opportunity for this transformation will continue to accelerate, with all newly qualified pharmacists becoming independent prescribers from 2026, shortening the time it takes for a pharmacist to prescribe independently from approximately eight years to around five. NHS England will support 3,000 pharmacists who have graduated but not completed an independent prescriber course to gain the required skills, knowledge and qualification to prescribe as independent clinicians. Pharmacists and pharmacy technicians are also increasingly working within primary care networks to provide enhanced clinical services alongside GPs and a wider multidisciplinary team. In hospital pharmacy, the growth of specialist clinical and technical roles will continue to be central to high quality medicines optimisation. Through proportionate regulatory reform, pharmacy technicians will be able to supply medicines and services through Patient Group Directions. This, combined with legislative changes to enable the NHS, and particularly community pharmacies, to make better use of the available skills mix and technology in pharmacies, will ensure pharmacy technicians can work most effectively as part of wider primary care teams and across the NHS. Government intends to consult on these changes in due course.
- Primary eye care providers have the knowledge and skills required to deliver more eye care services in the community. Working closely with secondary care specialists and using technological innovation, such as digitally enabled image sharing, to deliver more eye care services on the high street could help alleviate pressure in general practice and hospital eye services, and improve patient outcomes.
- In dentistry, workforce challenges increased during the COVID-19 pandemic, with dentists offering fewer NHS services, making these harder for the public to access. Nationally, NHS England is reforming contractual arrangements to encourage more dentists back into NHS practice and to make it easier for therapists and hygienists to provide NHS care directly [see reference 224]. By the end of the modelling period, the Plan aims to deliver 15% of dental activity through dental therapists and dental hygienists, as opposed to the current estimate of 5%. A national Return to Therapy programme is being developed to enable dental therapists working as hygienists to fulfil their full scope of practice [see reference 225].
- Support workers, both clinical and administrative, are an important part of wider multidisciplinary teams, enabling more effective and efficient working. They contribute to addressing critical workforce capacity constraints while providing high quality, personalised care to patients. These include assistant practitioner and technician roles, such as occupational therapy assistants, which can be key integrators across health and social care. There will be a continued focus on supporting the recruitment and retention of these groups, including:
- maternity support workers through the Competency, Education and Career Development Framework [see reference 226]
- AHP support workers, through growth of apprenticeships and the development of a Competency, Education and Career Development Framework [see reference 227]
- healthcare support workers, through the NHS England programme [see reference 228] (recruitment, induction and career pathways)
- cancer support workers, through the ACCEND (Aspirant Cancer Career and Education Development) programme [see reference 229].
- There are considerable opportunities for better deployment of the administrative workforce to free up clinicians’ time and support patient flow, alongside using technology to reduce administrative burden. For example, East Sussex Healthcare NHS Trust has successfully introduced doctor’s assistants to undertake specific tasks to reduce doctors’ workload. This was in response to an evaluation that found doctors were spending 44% of their time on administration and that 78% of overtime/ exception reports could be carried out by doctor’s assistants [see reference 230]. Qualitative feedback indicated a reduction in workload following the role’s introduction, as well as positive impacts on patient care and hospital flow [see reference 231]. GPs have indicated that, among other reasons, their clinical and administrative workload is a key reason for leaving the profession. General practice already employs around 600 GP assistants who provide both administrative and clinical support, and we anticipate this number will grow with the role having been reimbursed via the ARRS since October 2022.
- It is estimated that one in five people who go to their GP do so with concerns that cannot be addressed with medical treatment [see reference 232]. As part of service and workforce redesign, specific roles are being embedded within multidisciplinary teams to support self-care and facilitate access to broader local support services. Some of these roles are fulfilled by people who have lived experience of a health condition who can support others to develop the knowledge, skills and confidence to effectively manage their conditions. Expansion should be targeted at primary care, mental health, and learning disability and autism services, where need is greatest. The figures in Table 4 below are indicative based on current projections. They will be monitored and refined over time, based on continuous learning of the most effective MDT skills mix and impact of technology and digital opportunities.
Table 4: Personalised care roles potential expansion
| Personalised care role | Estimated expansion |
|---|---|
| Care co-ordinators | Increase from over 4,000 current posts (September 2022) to 12,000 by 2036/37 |
| Health and wellbeing coaches | Increase from over 1,000 current posts (September 2022) to 6,000 by 2036/37 |
| Social prescribing link workers | Increase from over 3,000 current posts (September 2022) to 9,000 by 2036/37 |
| Peer support workers (mental health services) | 4,730 staff in post by the end of 2023/24. Extend growth so there are over 6,500 by 2036/37 (NHS Mental Health Implementation Plan), [see reference 233] |
| Peer support workers (autism services) | Autism Peer Support Workers Capability Framework in place to support autism service providers to develop these roles. In 2023/24 support services will pilot these roles and develop an Autism Peer Support Worker Training programme |
- Evolving the skills mix of multidisciplinary teams is vital for the continued growth of new models of care such as virtual wards, SDEC, intermediate care and expanded community services. Investment in preventative interventions and early diagnosis would alleviate pressure on the NHS. The development of services such as family hubs, community diagnostic centres and pulmonary rehabilitation services recognises that early intervention improves healthy life expectancy, and government will build on these initiatives in its forthcoming major conditions strategy. Another key example is virtual wards, where over 7,500 virtual ward ‘beds’ across the NHS are providing hospital-level acute care to patients in their own homes, enabled by technology. The ambition is to have 10,000 virtual ward beds by winter 2023, and longer-term 40–50 virtual ward beds per 100,000 population and covering a broad range of health conditions. Virtual ward workforce models benefit from a range of professionals, drawing on the talent across sectors. While they are best designed locally, an estimated 8,500 new staff, including advanced practitioners, community nurses, administrative staff and healthcare support workers, would need to be recruited to meet this longer-term ambition. Some of these staff would come from the existing workforce (through redesigned or extended roles, for example), demonstrating the need for collaboration across organisations to implement the shift to out-of-hospital care successfully and safely. Key to developing further capacity in virtual wards is the successful integration of education and training opportunities and the expansion of innovative student placements.
- The forthcoming government consultation on ways to boost occupational health coverage intends to identify the composition of the multidisciplinary workforce required to deliver employment-focused interventions to support the wider working age population. Responses will be used to inform ongoing occupational health workforce planning. Occupational health professionals can advise on employment and support people to return to and remain in work, which benefits individuals and the wider economy, as well as the delivery of NHS services.
- In mental health, the ambition is to increasingly shift care towards early intervention and prevention, primarily delivered in the community. Within general practice a mental health practitioner (MHP) role was introduced in 2021 for adults with severe mental health needs, funded jointly by ARRS reimbursement and mental health NHS Long Term Plan funding. Children and young people’s MHPs within general practice can work with young people with any level of mental health need. There has been a steady increase in these roles and 68% of primary care networks had at least one adult MHP in Q4 2022/23. This Plan determines that growth is needed across psychological professions (across physical and mental health), building on investment made by NHS England in 2022/23. These include psychologists and psychological therapists as well as new roles; examples are:
- Clinical psychologists work within mental health, learning disability and autism, and physical health services. 1,065 training places were commissioned in 2022/23 with a similar level projected in 2023/24.
- Psychological therapists work within NHS Talking Therapies for anxiety and depression, community mental health services for adults and with children. 2,556 training places were commissioned in 2022/23 with more than 3,000 projected in 2023/24.
- Mental health and wellbeing practitioners are trained to provide wellbeing focused, psychologically informed interventions for adults with severe mental ill health in collaboration with people who use services, and their carers/supporters. 560 training places were commissioned in 2022/23, the first intake started their training in March 2022 and their impact is being evaluated in 2023/24.
- Children’s wellbeing practitioners are trained to assess and support children and young people with common mental health difficulties such as mild to moderate symptoms of anxiety, depression and behavioural difficulties, by offering a range of low intensity interventions that are based on cognitive behavioural therapy and guided self-help. 387 training places were commissioned in 2022/23 with around 400 projected in 2023/24.
- Educational mental health practitioners are trained to deliver evidence-based interventions for children and young people with mild to moderate mental health issues. They work in Mental Health Support Teams (MHSTs) based in schools and colleges. Around 500 MHSTs are expected to be operational by 2024.
- This Plan aims to increase the number of approved clinician roles across mental health services so that by 2036/37 there are at least 1,000 more than in 2022/23. This will include expanding the number of multiprofessional approved clinicians. Within mental health settings, multiprofessional approved clinicians have delegated responsibilities under the Mental Health Act and can significantly enhance quality of care by matching clinical specialism to service user needs. This continued expansion, along with wider mental health workforce expansion, will improve access to services and quality of care. In addition, a 24-month pilot scheme started in 2022/23 giving 43 SAS doctors access to the same learning opportunities as the eligible non-medical professions so they can undertake the role.
- Linked to this, government’s 10-year drug plan (2021–2031) sets out the expansion and development needed for the drug and alcohol treatment and recovery workforce, and committed an additional £532 million for drug and alcohol treatment and recovery services from 2022 to 2025. NHS England will work with DHSC to develop the drug and alcohol treatment and recovery workforce over the coming years, in line with the 10-year plan.
- There are also opportunities to pool more specialist workforces across systems and providers to support workforce and training capacity for the whole system; for example, for specialist services for long-term conditions including cancer or multiple sclerosis, and in imaging networks. Over the 22 imaging networks, workforce plans and strategies are being developed to leverage skills mix and support career development opportunities [see reference 234].
- Improving the links between employers and professional regulators will be fundamental to the development of the workforce to meet future needs. This includes how standards of practice might need to evolve to support multidisciplinary working. For example, during the pandemic, emergency regulations were introduced that allowed other doctors to deliver care in general practice (providing they were on the GMC register, not exempt from revalidation and already connected to a designated body). DHSC is consulting on reforms to the Medical Performers List to retain the flexibilities introduced during the pandemic to allow doctors other than GPs to work as part of a general practice team in a safe and supported way.
Upskilling the workforce
- We will need to upskill our workforce to maximise the opportunities from technological and digital innovations, and embed new and different ways of working. Successfully harnessing technological advances will require staff to work in fundamentally different ways, and will necessitate the growth of specialist digital, technology and genomics roles.
- Nationally, the NHS Digital Academy [see reference 235] has been established as the home for digital learning and development. A digital skills assessment tool [see reference 236] which addresses digital literacy needs across the workforce will be rolled out by the end of 2023/24. The Digital Learning Solutions [see reference 237] platform provides health and social care organisations with access to online digital skills training content created both centrally and locally. Over the last three years there has been a 440% increase in enrolments, with most popular courses providing training in triage software for 111 services, as well as Microsoft Teams, telephony and local electronic patient records. The NHS Digital Academy provides development opportunities including the Digital Leadership Programme [see reference 238] through Imperial College London; the Topol Digital Fellowships [see reference 239], now expanded to include the social care and non-clinical workforce and the Health Innovation Placements Programme [see reference 240]. This is supported through Informatics Skills Development Networks [see reference 241], which are key to adoption and development of learning products, ensuring consistency, sharing and collaboration. With NHS Providers, the Digital Boards Programme [see reference 242] has delivered over 80 trust board development sessions to date, and engaged many others, improving understanding at the most senior level. The Fast Futures programme [see reference 243] is supporting school leavers and building partnerships with University Technical Colleges to establish routes into the NHS to help grow the digital workforce.
- The Phillips Ives Review, which is nearing its conclusion, will inform strategy to prepare the nursing and midwifery workforce for the digital future. Similarly, the ARRS has introduced digital and transformation leads to support primary care to identify and implement improvements to ways of working, and to help make the most of existing and new technology.
- The recently published NHS Genomics Strategy outlines the vision for embedding genomics in the NHS over the next five years [see reference 244]. The specialist genomic workforce needs to grow and skills across the wider workforce need embedding as genomics becomes more integrated into clinical pathways, such as cancer and cardiovascular disease. As part of the strategy, NHS England will explore the future genomics training and development model with academia and industry over the next 3–5 years, particularly for specialist staff such as bioinformaticians, to secure future supply for the NHS and to share experience and knowledge.
- Maximising the potential of genomics will require sufficient workforce capacity across the multidisciplinary Genomics Medicine Service. Training places through the three-year Scientist Training Programme expanded 65% by 2022/23, to increase bioinformatics and genomics staff and genetic counsellors supporting services such as cancer. This is alongside other academic and training courses to enhance the scope of practice of existing staff. We will continue to introduce innovative training and education models through the national Genomics Training Academy, and over the next year we will work with partners and the Genomics Medicine Service to deliver more training virtually and share best practice across NHS regions.
- Personalised care and public health core skills and knowledge must be embedded across the wider NHS workforce to improve population health. With over one million patient interactions daily, NHS frontline staff have an important role in supporting people, including those with long-term conditions such as diabetes, to improve their health and wellbeing. ICSs should look to expand secondary prevention expertise by working with DHSC to increase uptake of the Level 3 Community Health and Wellbeing Worker apprenticeship standard among the frontline workforce, and identify opportunities to upskill enhanced and advanced practitioners in population and public health. A range of accredited training resources through the Personalised Care Institute [see reference 245] are already included in some pre- and post-registration frameworks, and there is also a dedicated Population Health Fellowship programme [see reference 246]. The aspiration is to have a fellow working in every ICS to support the development of local expertise. The CARE programme [see reference 247] empowers general practice nurses and other primary healthcare professionals to help their primary care network to shape services based on population health needs.
- We will equip the NHS workforce with the right skills and knowledge to shift care towards prevention and early intervention, including by broadening training for the wider NHS workforce to increase capacity and confidence in these areas. Staff should be better equipped to deliver smoking cessation advice and to use recognised screening tools, such as ASSIST-Lite [see reference 248], to help identify potential harmful and hazardous levels of alcohol and drug use. Mental health staff in particular should be trained and competent in the recognition, treatment and care of adults and young people with co-occurring mental health and drug and alcohol use conditions. This is vital since 70% of adults starting drug and alcohol treatment in 2021/22 said they had a mental health treatment need [see reference 249]. We will develop healthy weight coaches and roll out training for wider professionals on having sensitive conversations about weight, supporting onward referrals into weight management services. By March 2024, NHS England will develop a plan with system partners to support the workforce with delivering interventions that detect and optimally manage major conditions such as cardiovascular disease (CVD) and cancer over the medium term. From April 2023, ICBs, as part of their responsibilities to improve population health, should work with their local authority public health teams and partners to train and upskill their local primary care workforce so they have the competencies to improve CVD outcomes, as described in the 2023/24 operational planning and contracting guidance, and deliver interventions such as the NHS Health Check. This includes rolling out to frontline staff the Behaviour Change Development Framework [see reference 250] and e-learning modules in Making Every Contact Count (MECC) [see reference 251] and All Our Health [see reference 252], and promoting the health inequalities e-learning offer [see reference 253], which is free to the entire NHS workforce.
- Wider health and care workforce development and training is also needed to support the delivery of care. For instance, work is underway to test approaches to upskilling social care staff to take on healthcare tasks, where appropriate, such as insulin administration in the community for patients with diabetes. Similarly, the Oliver McGowan mandatory training was launched in November 2022, with face-to-face sessions beginning this year. It aims to equip staff with the knowledge and skills to reduce health inequalities and supports the Health and Care Act 2022 requirement that all regulated health and social care providers must ensure their staff receive training on learning disability and autism, appropriate to their role. In addition, a national autism trainer programme is being rolled out in children and young people’s and adult mental health inpatient services and community mental health services, with a pilot due to launch in 2023/24 in a wider range of health and care settings.
- The workforce also needs the skills to be more active in research and education. For example, in 2021, the Chief Nursing Officer for England published a strategic plan to empower nurses to lead, participate in and deliver research [see reference 254]. This was followed by a Chief Midwifery Officer strategy [see reference 255] in 2023 setting out similar ambitions for the midwifery profession. Providing roles across professions with dedicated time for research drives best practice and evidence-based care; and can also boost retention [see reference 256]. Equally, staff need access to high quality learning at all stages of their career. To meet the workforce growth outlined in this Plan, the NHS would need more trainees, students, apprentices and advanced practitioners, and to build educator and supervisor capacity and capability alongside. There are opportunities for ICSs to establish effective clinical academic roles across professions and organisations to boost the educator and research workforce, retain staff in part-time service delivery roles and ensure registered staff have access to both experienced academics and those at the forefront of innovative delivery of care.
- Building knowledge of and the capabilities for workforce redesign and improvement can enable a culture of innovation and a focus on research and systematic evaluation to capture and learn from robust evidence. A joint project is already underway across NHS England, Academic Health Science Networks and The Health Foundation to improve skills around adoption of innovation both through curation of resources on NHS England’s Enhance e-learning platform [see reference 257] and the incorporation of education resources in existing leadership programmes [see reference 258].
- The NHS Health Education England framework for spread and adoption of workforce innovation sets out an approach for systems to follow [see reference 259]. NHS England, Health Education England (HEE) and NHS Digital are now a single organisation and can develop tools, training and resources to support workforce redesign in practice, such as:
- skills mix blueprints for local adaptation and adoption
- training programmes to build ICB capability in workforce transformation approaches such as the HEE Star [see reference 260] and the six-step workforce planning approach [see reference 261].
- Improving the evidence base for new ways of working will be a collective effort across local, regional and national partners. Work is underway across NHS England, in partnership with DHSC, the National Institute for Health and Care Research (NIHR) and higher education institutes to identify and collectively address cross-professional strategic research workforce priorities [see reference 262]. Locally, systems should be adopting the principles of learning health systems [see reference 263], and ensure they are systematically gathering and applying evidence and data to support continuous learning, and aid clinical decision-making and improvement.
5. Next steps
Delivering and embedding the Plan into our new NHS structures
- This Plan assesses the scale of the workforce challenge the NHS currently faces, and how it is likely to evolve if action is not taken. Our analysis gives a better understanding of where workforce pressures are particularly acute, and what action is needed over the next 15 years to address them. Further engagement will follow the Plan’s publication to develop the detail of the actions and plans for implementation with stakeholders.
- The Plan recommends actions at every level of the NHS. Employers, systems and national organisations will all need to contribute, so that local actions shape, and are shaped by, NHS England’s analysis and support. NHS England is investing more than £500 million in 2023/24 and 2024/25 on top of education and training budgets, to ensure no time is lost, and the further actions set out in this Plan are backed by more than £2.4 billion up to 2028/29, funded by the government. To aid transparency, NHS England will separate out education and training expenditure in our regular financial reporting.
- NHS England will refresh the plan at least every two years, to ensure that our assessment of demand for staff continues to improve, remains up to date, and is consistent with the approach we take for wider operational, financial and education planning – including aligning with fiscal events as appropriate. The modelling underpinning the Plan will also be independently verified to help inform future updates.
- This Plan is intended to be the start of an ongoing programme of work that becomes an established part of how the NHS plans for, and delivers, its services for patients and the public. An integrated approach to planning and delivery, bringing together workforce planning with service and clinical strategies and financial planning, must be embedded for the long term to respond to changes in demand, services and wider factors. This approach must be carried through every part of the NHS.
ICSs will play a critical role
- ICSs bring NHS organisations together with local authorities and wider system partners to improve population health and healthcare, tackle unequal outcomes and access, enhance productivity and value for money, and help the NHS support broader social and economic development. Systems are already making progress in delivering against the 10 outcomes-based functions for ‘one workforce’ [see reference 264], to make the local area a better place to live and work.
10 outcomes-based functions to be delivered by NHS leaders and organisations in collaboration with their ICS partners
- Supporting the health and wellbeing of all staff
- Growing the workforce for the future and enabling adequate workforce supply
- Supporting inclusion and belonging for all, and creating a great experience for staff
- Valuing and supporting leadership at all levels, and lifelong learning
- Leading workforce transformation and new ways of working
- Educating, training and developing people, and managing talent
- Driving and supporting broader social and economic development
- Transforming people services and supporting the people profession
- Leading co-ordinated workforce planning using analysis and intelligence
- Supporting system design and development.
Building strong integrated care systems everywhere: guidance – ICS people function (NHS England, August 2021)
- This Plan recommends actions for systems that align to these functions, to improve the experience for staff. Most urgently, it recommends that ICBs and wider system partners prioritise actions that drive recruitment and retention of their ‘one workforce’ across health and care.
- System colleagues will determine their approach in light of local needs and opportunities. NHS England’s teams and partners will offer them direction and support, including tools such as the System Workforce Improvement Model (SWIM) and the Six Steps Methodology to Integrated Workforce Planning [see reference 265].
- ICBs and their partner trusts will set out their priorities for workforce action in their five-year joint forward plans (JFPs), to be published in due course. Drawing on the support of Cancer Alliances and other local partners, JFPs will describe their steps to provide the workforce and services required to meet the physical and mental health needs of their population over the next five years. They serve as the shared delivery plan for the system’s integrated care strategy – produced by the integrated care partnership with their whole system, including local authorities and voluntary, community and social enterprise organisations.
- Effective system-level delivery is dependent on having sufficient capacity and technical capability for workforce planning at every level in the service. A joined-up approach is also vital, not only to bring together workforce, service and finance planning, but also for education and training so there is closer alignment and more opportunity to be proactive and deliver our shared objectives. NHS England is expanding its support offer for systems, including through a new tool that provides additional system-level workforce intelligence, and facilitating an accredited Strategic Workforce Planning course – contextualised for the NHS and health and social care – through the Chartered Institute of Professional Development (CIPD).
- The merger of Health Education England, NHS Digital and NHS England allows us to better align and co-ordinate planning and action, at every level of the service, so we can have the greatest possible impact for staff and, by extension, patients and citizens.
- NHS England is refreshing its oversight mechanisms to reflect its new functions and responsibilities. This refresh will take account of the oversight needed for this Plan, and ensure we align how we oversee delivery of system-level five-year JFPs, NHS operational planning guidance, the NHS Long Term Plan and the shared local priorities of individual ICSs.
Planning over the long term requires an adaptable approach
- Planning over a 15-year horizon is inherently difficult, and assessing future shortfalls and potential mitigating actions is not an exact science. With all key assumptions in the modelling, it is worth considering the implications and choices that would arise should they prove to be overly optimistic or should they be exceeded, as well as where there are key dependencies which will affect delivery. We will need to keep the position under assessment and make informed choices about what further action may be needed.
- Over the next few years, modelling needs to be refreshed to assess progress against critical assumptions. This will enable us to make judgements about the required further training and education expansion and the necessary speed of expansion post 2028/29, as well as the likely timeline for reducing reliance on international recruitment and temporary staffing beyond 2028/29.
- The immediate actions for the next few years to boost training and education are based on a set of assumptions about demand, productivity and retention over the modelling period. For example, the modelling recognises the balance of risk around productivity. If productivity improvements are towards the lower end of the range, predicted shortfalls in NHS staffing would persist. This could impact on our ability to deliver services to the agreed standard, or meet access ambitions. Addressing the shortfalls may require a choice to increase levels of international recruitment in the short term or increase reliance on more expensive temporary staffing, until additional staff could be trained and recruited.
- Achieving the productivity improvements assumed in the Plan is dependent on two key factors. First, it requires a sustained increase in capital investment in the ageing NHS estate, including in primary care, to replace equipment that has passed its recommended lifespan, and expand capacity to accommodate the increased demand for healthcare from an ageing population. This would enable staff to function more efficiently, and shorten diagnosis and treatment times in areas such as cancer. Second, it requires investment in digital infrastructure throughout the NHS, including appropriate training and support, to enable NHS staff to make the most of new technologies.
- The modelling for this Plan assumes that the balance of care between the NHS and social care will remain broadly the same. However, an increase in the capacity of and access to social care would likely contribute to reducing the assumed growth in demand for NHS services, by broadening access to preventative and rehabilitative care, and supporting the more effective discharge of patients who have ongoing care needs, shortening their time in hospital. Alongside social care and community care, NHS rehabilitative services play a vital role in supporting people to leave hospital- based care at the right time and recover in their communities.
- Taking a long term approach to workforce planning means that having a surplus of staff is unlikely, however if that were to occur then action can be taken accordingly, for example by scaling back international recruitment even further.
Ongoing refinement of the NHS Long Term Workforce Plan
- Stakeholders have informed and shaped the proposals set out in the NHS Long Term Workforce Plan, including by helping us to develop the modelling that underpins the Plan and the case for change. We are grateful for their constructive partnership and for faithfully reflecting the views of the individuals and groups they represent.
- This Plan represents our current best assessment of how to close the gap between supply and demand for staff. However, the intention has always been for the Plan to be iterative. Actions and assumptions will be sharpened as new and better data is collected and we gather further opinion from stakeholders and partners, and to respond to wider changes in the health and social care system, higher education sector and wider jobs market.
- To refine the Plan and arrive at an agreed set of actions for the longer term, we will build on the collaborative way of working already established. The workforce model will continue to be refined as deeper and higher quality workforce data becomes available, and to reflect changes to service demand and ambitions, informed by NHS planning rounds.
- Having a clear understanding of the different roles and skill sets within the workforce, and how staff are deployed, will help to develop ever-more accurate workforce plans. This is particularly true for staff with a wider variety of specialist roles, such as consultants and healthcare scientists, and where there is opportunity to use new workforce models and mixes of skills. We will work with system leaders, employers and stakeholders, including the royal colleges, to gather better data on specialist staff and establish clearer demand signals so we can set out the demand and supply position for specialties and tailor training and recruitment to best meet pressures.
- Following publication, we will continue to work with system leaders and stakeholders to refine the detail of the actions, and support effective implementation and delivery of the ambitions in the Plan. We will ensure we use every lever at every level by considering how best to deliver the Plan through the NHS England operating framework [see reference 266], working with the service to strengthen the feedback loop between local, regional and national planning, and aligning education and training planning with service, financial and operational workforce planning. We welcome the continued commitment and partnership of our stakeholders as we collectively work to put the NHS workforce on a sustainable footing for the years ahead.
Annex A: Organisations engaged in forming the NHS Long Term Workforce Plan
Royal colleges
- Academy of Medical Royal Colleges and members
- Royal College of Anaesthetists
- Royal College of Emergency Medicine
- Royal College of General Practitioners
- Royal College of Midwives
- Royal College of Nursing
- Royal College of Obstetricians and Gynaecologists
- Royal College of Occupational Therapists
- Royal College of Paediatrics and Child Health
- Royal College of Pathologists
- Royal College of Physicians
- Royal College of Podiatry
- Royal College of Psychiatrists
- Royal College of Radiologists
- Royal College of Speech and Language Therapists
- Royal College of Ophthalmologists
- Royal College of Surgeons
Professional bodies
- The Society of Radiographers
- Institute of Osteopathy
- College of Operating Department Practitioners
- British Association of Art Therapists
- British Association of Drama Therapists
- British Association for Music Therapy
- British Dietetic Association
- British and Irish Orthoptic Society
- British Association of Prosthetists and Orthotists
- College of Paramedics
- The Chartered Society of Physiotherapy
- College of General Dentistry
- Faculty of Sexual and Reproductive Healthcare
- Queen’s Nursing Institute
- Institute of Health Visiting
- British Society of Rheumatology
- Royal Pharmaceutical Society
Other organisations
- Mental Health Policy Group
- Local Government Association
- Skills for Care
- Care Provider Alliance
- Association of Directors of Adult Social Services
- Cancer charities group
- The Richmond Group of Charities
- Parkinson’s UK
- World Health Organization
Think tanks
- Nuffield Trust
- The Health Foundation
- The King’s Fund
Trade unions
- British Dental Association
- British Medical Association
- Social Partnership Forum
- Unison
- Managers in Partnership
NHS organisations
- The Shelford Group
- ICS leaders
- NHS Confederation
- Community Providers Network
- NHS Employers
- NHS Providers
Regulators
- General Medical Council
- Care Quality Commission
- Health and Care Professions Council
- Nursing and Midwifery Council
- General Pharmaceutical Council
- Professional Standards Authority
- General Dental Council
Education
- Council of Deans of Health
- Medical Schools Council
- Universities UK
- University Alliance
- Office for Students
Annex B: Modelling approach and assessment
- This annex sets out how we have assessed the demand for NHS staff over the 15- year timeframe, and how that demand might be met. The model, and ranges presented, should be treated as strategic insights to inform policy choices relating to education, training, recruitment and retention, rather than operational insights, targets or precise values.
Definitions
Table 1: Concepts underpinning the model
| Terminology | Definition |
|---|---|
| Current demand | The number of substantive staff employed by the NHS as of March 2022 and temporary staff (FTE) deployed in the financial year 2021/22. The number of substantive FTE staff is recorded via the NHS Electronic Staff Record (ESR). Temporary staff FTE numbers (bank and agency) are calculated from shift data which is converted to FTE using the following assumptions: medical and non-medical staff are assumed to undertake shifts of 12 hours in length, and the standard working hours are assumed to be 160 hours per month for medical staff and 150 hours per month for non-medical staff; therefore the shifts are converted by assuming that for medical staff 13.3 shifts per month are equivalent to 1 FTE, and for non-medical staff 12.5 shifts per month are equivalent to 1 FTE. For GPs, demand was calculated using demographic data assuming we need to restore the qualified GP-to-patient ratio observed in September 2015. The current demand for dentists, dental therapist or hygienists is defined by current number of FTEs delivering NHS services, plus opening shortfall (see shortfall definition below). The estimated number of FTE pharmacists required to deliver care to the England population in all settings (ie community, NHS, primary care), based on assessment of shortfall and current supply. |
| Future counterfactual demand | The expected required number of FTE staff. This is based on activity projections calculated from population projections, non-demographic growth assumptions and service plans. Vacancy rates data is used to apportion staff across professions. |
| Current supply | The number of substantive FTE staff employed by the NHS (and recorded via ESR or other collections), as of March 2022 (financial year 2021/22). The estimated current capacity of FTE dentists/dental therapists assumed to be delivering NHS dentistry based on NHS BSA Dental Statistics in August 2022 (financial year 2021/22). The number of staff employed in pharmacy in all settings in November 2021 as reported in the community pharmacy workforce survey (community), NHS Digital (primary care) and Electronic Staff Record (NHS HCHS services). |
| Future counterfactual supply | The expected number of substantive FTE staff. This is based on projections driven by historical data on the training pipeline, transition to the NHS, retention and international recruitment, as well as agreed and funded interventions to boost or upskill supply. The expected capacity of substantive FTE dental/dental therapy staff providing NHS dentistry services. This is based on NHS England projections driven by historical data on the training pipeline, transition into the workforce and NHS, retention and international recruitment, as well as agreed and funded interventions (within current Spending Review) to boost or upskill workforce capacity providing NHS dentistry services. The expected number of substantive FTE pharmacy staff in all settings. This is based on NHS England projections driven by historical data on the training pipeline, transition to the NHS, retention and international recruitment, as well as agreed and funded interventions to boost or upskill supply. |
| Shortfall | The shortfall measures the amount of workforce demand that cannot be met by NHS substantive FTE staff. The starting shortfall is estimated by measuring the amount of temporary staff deployed in 2021/22 where possible. For GPs, the opening shortfall is the gap between the estimated starting demand (using historical GP-to-patient ratio) and GP supply. In dental, the opening shortfall is estimated using the percentage of the population who would like to access NHS dental care but are unable to. In community pharmacy, the opening shortfall is estimated using historical staffing and NHS service delivery, including dispensing and self care, compared with current. |
| Baseline | Financial year 2021/22 (March 2022 starting point) |
| Current Spending Review | Financial year 2021/22 to 2024/25 |
| Labour productivity | Labour productivity overall measures the changes to the amount of output delivered by a given amount of labour input. The overall labour productivity includes a wider range of consideration including delivering care in a more efficient setting, improvement through skill mix opportunities and reducing temporary staffing. The workforce modelling primarily uses activity-to-FTE ratio to assess the impact of productivity on workforce demand. |
| Interventions | Proposed demand and supply-side actions to address the shortfall. These interventions are additional to those already agreed through the current Spending Review and are included in the counterfactual. |
Timelines and granularity
- The model projects potential staffing shortfall in the short, medium, and long term, to inform the national levers required to address the shortfall. It does not precisely forecast how many staff will be needed; rather it provides a reasonable basis for workforce planning.
- The model covers the workforce employed by the NHS and delivering funded services in all NHS trusts and primary care. Some professions with unique characteristics (such as dentistry and community pharmacy) have been modelled separately.
- The workforce model outputs can be disaggregated by year, profession and care setting as set out in Table 2.
Table 2: Workforce model factors
| Model factor | Details |
|---|---|
| Time period | Model starts at financial year 2021/22 (March 2022) and projects forward until 2036/37. Outputs can be generated for each year of the years between. |
| Profession | 52 output professions have been mapped to 8 staff groups (medical, nursing and midwifery, AHP, other, ambulance service, support to clinical, infrastructure support, GP) |
| Care setting | Five care settings (acute, mental health, ambulance, primary care, and community) |
Supply projections counterfactual
Acute, ambulance, community, mental health and learning disability
- The starting shortfall is calculated using two sources of data: temporary staffing shifts (converted to FTE at profession group level) and vacancy data in operational plans (to apportion across individual professions).
Primary care
- The starting shortfall is estimated from historical staff-to-patient ratios (September 2015).
Supply counterfactual assumptions
- The counterfactual supply forecast is informed by historical data, mainly that from the last 3–5 years. This means it will reflect the impact of recent policy decisions such as the 50,000 Nurses Programme [see reference 267], a key element of which is international recruitment.
- The components of the counterfactual supply side forecast and associated assumptions are:
- Education and training intake: The number of people starting training each year, calculated using the NHS Health Education England Student Data Collection [see reference 268].
- Completion of training: The percentage of students completing the full training pathway, calculated using the five-year historical average.
- Transition to working in the NHS: The percentage of individuals completing training who go on to work in the NHS (as opposed to a private provider or another sector), calculated using the five-year historical average.
- Leaver rate: The percentage of the workforce who leave the NHS every year, calculated using March to June 2022 FTE data. The LTWP model restricts the definition of a ‘leaver’ to those leaving NHS employment entirely, rather than those leaving active service (eg those on maternity leave or a career break). This data differs to the Official Statistics leaver rate data published by NHS England (formerly NHS Digital) for the period concerned due to key differences in methodology.
- Within NHS movement: The percentage of staff joining from/leaving to go to another region or profession within the NHS, as well as FTE lost through reduced hours calculated using the five-year historical average.
- Wider labour market: The number of new joiners with UK nationality who join the NHS via routes other than education and training, calculated using the five-year historical average.
- International recruitment: The number of new joiners to the NHS with non-UK nationality, as observed from the Electronic Staff Record. This provides an approximation of international recruitment as those with a non-UK nationality on ESR can still study and qualify within the country. Greater detail separating out nationality and country of primary medical qualification could be obtained for medics but the same is not possible within non-medical professions. Therefore, this proxy has been used to allow for simplification and consistency within the modelling.
The number of new joiners primarily counts staff who have joined the NHS within a given 12-month period. The baseline is calculated from the mean number of joiners in FTE with non-UK nationality between March 2017 and March 2022 (in other words, a five-year average). The exception is for nursing, which takes a three-year average covering March 2019 to March 2022. This reflects that international recruitment for nursing increased sharply from 2019 through the 50,000 Nurses Programme [see reference 269].
Within the modelling of international recruitment, it is assumed that while it can be influenced through government policy, a significant proportion of international recruitment is not centrally influenced.
Modelling uses internal management information from UK Visas and Immigration, separated by profession between 2020 and 2022, and observed international recruitment on ESR over the same period as a proxy for influenceable international recruitment.
- Apportionment to care setting and sector: We have mapped staff to care settings using data from ESR and a combination of care setting and occupational codes. We have resolved any overlap by apportioning staff according to care setting, occupational code and type of organisation. This means the baselines in this modelling may differ from previous categorisation of data published by NHS Digital. The mapping of where staff are based (including between different care settings, or between NHS and the independent sector) could change over time depending on the approach taken to service provision. For modelling purposes, this is broadly assumed to remain constant. Should it change, the staff needed to deliver services will still be required even if they are based in a different organisation or setting.
Demand projections counterfactual
Current workforce demand
- Current workforce demand, calculated as staff in post in 2021/22 plus temporary staffing, is the starting point for demand projection calculations across all care settings.
Growth rate
- Demographic growth is applied to capture the expected changes in population size and age distribution.
- Non-demographic growth is also applied to recognise other demand drivers such as changing user expectations and needs, changes in the service offer, advances in technology and care delivery. This is estimated using historical data.
- Where relevant, demand growth rates are aligned with existing delivery plans; for example, the elective recovery plan or urgent and emergency care recovery plan. Growth rates also capture the need to strengthen primary care and out-of-hospital care offer (eg virtual wards and intermediate care).
- From 2025/26 onwards a case mix adjustment is added to capture increasing complexity of treatment in areas like cancer, dementia and stroke and work requirements, based on observed trends over time.
- Provisions are made to account for the need to improve access and recover performance: ambulance response times, elective waiting times, general and acute bed occupancy, in addition to opening shortfalls.
- Mental health and learning disability service demand are calculated separately by extrapolating from the observed growth since the implementation of the Mental Health Investment Standard.
Labour productivity
- The final demand counterfactual numbers for acute and ambulance services are adjusted by a productivity recovery factor, to account for the impact on productivity from COVID-19.
- Under the central scenario, an FTE-to-activity ratio improvement of 0.8% a year is applied, although this is not the totality of labour productivity assumed to be delivered by the NHS over this period of time, as this figure does not take into consideration other productivity drivers such as delivering care in more cost effective settings.
Interventions modelling
- Combining counterfactual demand and supply forecasts provides us with the initial FTE shortfall. This is followed by an iterative process of applying workforce interventions to assess their impact and address the projected shortfall.
- Key considerations in this approach are:
- Shortfall to be narrowed: using the baseline scenarios, we can establish the counterfactual demand and supply shortfall to be addressed through supply
- Timeframe: the model covers 15 years from 2021/22 to 2036/3.
- Maximum education intake: the likely maximum education intake for each profession is estimated by considering application numbers, education and training capacity, and feasible phasing of expansion. See Annex C for more detail.
- International recruitment: the model assesses the international recruitment required to address shortfalls in the intervening years while education and training capacity ramps up. The current level of international recruitment is estimated by assessing the number of professionals granted health and care visas as a proxy for non-medics; and for medics, it is estimated by the number of non-UK primary medical qualification holders.
- This Plan makes a set of assessments to reflect service ambitions and reduced reliance on temporary staffing and international recruitment:
- Improved retention: Leaver rates reduce to between the historical low and historical mean values for each profession, excluding the rate during the COVID- 19 pandemic period.
- Skills mix improvement: Addition of new roles and upskilling of existing staff shift shortfalls from the more highly skilled to the less highly skilled groups, while enhancing quality of care and improving productivity.
- Education and training: Training places increase to the level required to meet demand while reducing reliance on international recruitment, within the limit of maximum practical levels (based on places, applicants and training capacity).
- Recruitment from the wider labour market: Recruitment from the domestic labour market increases for roles without an education and training route.
- Reduced reliance on international recruitment: Most professions see reduced reliance on international recruitment as the impact of having more education and training places ramps up. However, some professions will see an increase in international recruitment in the short to medium term to address the shortfalls, depending on the scenario.
Sensitivity analysis
- The ranges in the modelling are driven by the following considerations to illustrate key areas of uncertainty:
- Staff leaver rate: Modelling considers three The leaver rate falls to the 1) historical mean; 2) the historical low; 3) the central scenario which assumes leaver rate falls to the midpoint between the historical mean and low points. Compared to the counterfactual baseline (which assumes no improvement on leaver rate), the impact on supply from retention will be 55,000 to 128,000 FTEs.
- Labour productivity: Recovery and continuous improvement of labour productivity. The total impact of labour productivity (1.5-2%) is broader than what’s included in the workforce modelling. Impact such as pathway reforms (eg moving care to lower cost points of delivery, eg outpatient procedures), delivering care in alternative settings (virtual wards), are already assumed in the underlying activity modelling. The sensitivity analysis considers in particular FTE-to-activity ratios, which includes 1) central scenario of 0.8% pa; 2) downside scenario of 0.6% pa; and 3) an upside scenario of 0.93% pa driven by higher productivity gains in the final years of the Plan from wide-scale roll-out of timesaving innovation and technology. The impact on demand from FTE-to-activity assumptions alone is 170,000 FTE to 215,000 FTE compared to the counterfactual (assuming no productivity improvement).
- Other considerations: Sensitivity analysis has also been considered on other assumptions including: 1) length of stay; 2) case mix; 3) impact of effort to move care out of hospital (for example, virtual ward and intermediate care); 4) impact of pathway reforms. These are not included in the final ranges to avoid duplication with other factors.
Modelling outputs
- The table below summarises the modelling outputs by profession for:
- Workforce demand by 2036/37 based on upside, downside and central productivity scenarios.
- Counterfactual supply growth based on historical trends and confirmed education and training pipeline.
- Retention impact on supply compared to the counterfactual (no improvement on baseline), based on upside, downside and central leaver rate assumptions. Retention impact not separately modelled for medics as already assumed in the counterfactual modelling.
- Skills mix and training impact on supply, including the net impact of skills mix opportunities on FTEs at profession level (eg expansion of nursing associates, advanced practitioners) ; and supply increase from education and training (ie number of FTEs joining the workforce from the increase in education and training proposed in this Plan).
- Impact of international recruitment on supply FTEs compared to the counterfactual which assumes the baseline number of staff recruited from overseas were to continue.
- An end supply position in 2036/37 by profession and the projected workforce supply for year five, 10 and 15 of the modelling period.
Table 3: Modelling outputs by professional groups
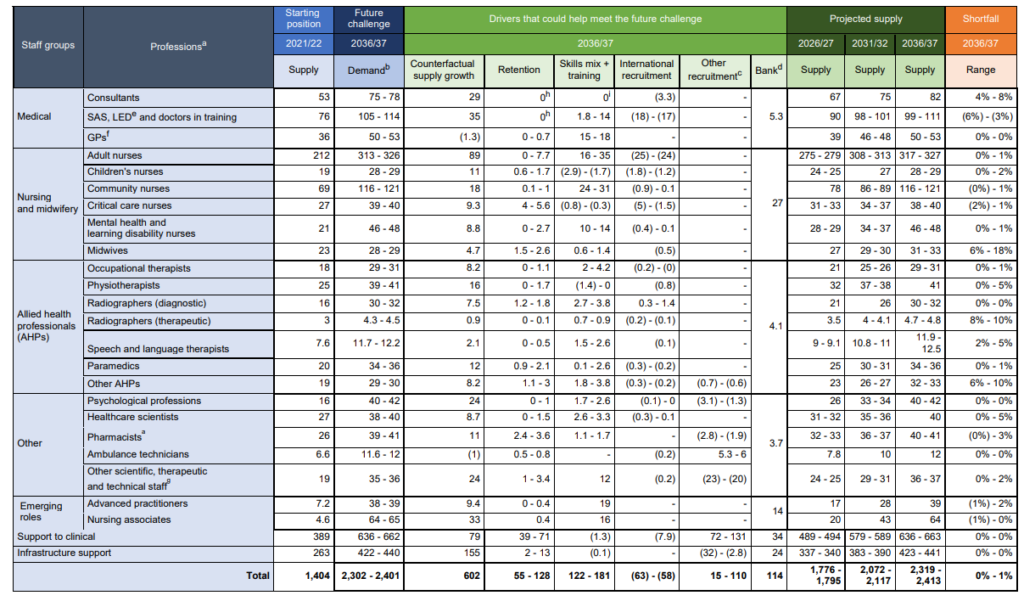
a) Includes all NHS staff; excludes dentistry and community pharmacy
b) Range is shown where the difference is larger than 1,000 FTEs or larger than 100 FTEs for small numbers
c) Recruitment from UK’s wider labour market where training route is not needed (such as from non-NHS sectors)
d) This assumes the proportion of NHS staff who choose to work solely on bank contracts will remain the same
e) SAS, specialty and associate specialist doctors; LED, locally employed doctors
f) Includes fully qualified GPs and GPs in training
g) Includes anaesthesia associates and physician associates
h) Changes to medical staff retention are included within the counterfactual model
i) Increases to medical undergraduate numbers proposed within the LTWP are not expected to impact significantly on consultant supply until after 2036/37
Table 4: Modelling outputs for dentistry and community pharmacy
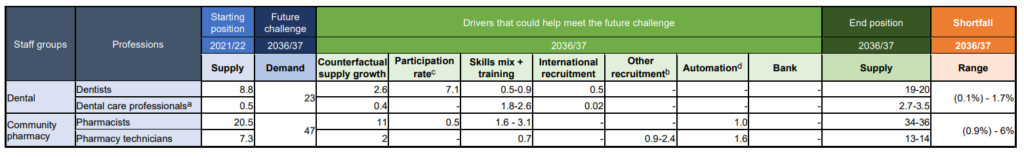
a) Includes dental hygienists and dental therapists; excludes dental nurses
b) Recruitment from UK’s wider labour market where training route is not needed (such as from non-NHS sectors)
c) The proportion of full-time equivalent staff providing NHS commissioned services
d) This assesses the impact of paperless dispensing systems and automated remote assembly
- Modelling outputs by care setting shows the differentiating growth rates as a result of service ambitions to move care out of hospital, investing in primary and community care, as well as mental health. This means a material impact on the size and proportion of workforce working in non-acute settings. For example, total nursing staff working outside acute settings is projected to increase from the current 30% to 37%; and the total community workforce nearly doubles in size over the modelling period. It is important to note that the modelling maps all staff to a given care setting depending on their employer and their role, but does not reflect the fact that staff will increasingly be working in integrated teams regardless of their primary employment.
Table 5: Growth rates (compounded annual growth rate) by care setting 2021/22- 2036/37
| Care setting | Demand – compound annual growth rate |
|---|---|
| Mental health and learning disability | 4.4% |
| Primary care | 2.7% |
| Community | 3.9% |
| Ambulance | 3.8% |
| Acute | 2.1% |
Annex C: Education and training
- Our assessment is that the education and training of doctors, nurses, AHPs and other healthcare professionals will need to change, for the NHS to have enough clinicians working in the NHS, and for them to have an improved experience of training and develop the right skills now and in future.
- This annex sets out further detail on:
- the approach for determining the potential education and training expansion, including apprenticeship expansion
- education and training expansion by profession
- considerations for the wider health and care sector and anticipated destination of learners who enter non-NHS roles
- priorities for working differently and education and training reform
- next steps for implementation, and the necessity of collaborative working with partners and stakeholders across the NHS and education sector to support delivery of the proposed actions.
- There are a range of opportunities to study, train and work in the NHS and wider health and social care sector. The domestic routes into the NHS are: (a) apprenticeships; (b) undergraduate degrees and (c) postgraduate This includes opportunities to gain dual qualifications and undertake advanced and enhanced training.
Modelling
Approach for determining education and training expansion
- This Plan sets out an assessment of the increase in domestic education and training needed to meet demand in the future. For each profession we estimated the maximum level of training intake to meet demand, balancing apprenticeships with undergraduate and postgraduate degrees, by considering the following aspects:
- Assumed size of and growth in the market: There will be a finite pool from which the NHS can draw its workforce, but this is broader than that currently tapped into and there is opportunity to increase the number of people working in health care. We determined a theoretical ‘ceiling’ for the domestic labour market, one based on proportion of the employed population working in the health and care sector alongside the size of the 18-year-old cohort. Although variable across professions, many undergraduate programme applicants are 18-25 years old and this age group will bulge in the coming years [see reference 270].
- Number and quality of potential applicants: For most healthcare professions applications to undergraduate and pre-registration courses exceed the places available, suggesting many good candidates are disappointed and more places can be filled. In 2020/21, only 14% of the 527,000 UK residents who started undergraduate courses in England in 2020/21 were enrolled on healthcare courses that lead to a professional registration and potential for employment in the NHS and social care sector. The assessed expansion set out here would result in education and training levels which are in line with average numbers per size of population in comparable OECD countries.
- Conversion rate: The Plan assumes that on average universities achieve higher student conversion rates (the number of university applicants to number of places) of up to 75% across all professions.
Apprenticeship expansion
- The Plan articulates that apprenticeships are an effective way of both growing the workforce and widening participation, as expanding these routes appeals to a broader diversity of applicants and particularly those who have wider life experience.
- The size and speed of the increase in delivery of apprenticeships for each profession depends on:
- The student conversion rate for courses; for professions where this is already high, there will be less opportunity to expand via undergraduate routes, and so a greater proportion of the expansion set out would need to be via apprenticeship routes. These professions include adult nursing, learning disability nursing, mental health nursing, podiatry, operating department practitioners and occupational therapy.
- Whether apprenticeship standards already exist for professions, or need to be developed.
- The availability of ‘feeder’ support professional groups such as nursing associates for the registered nurse degree apprenticeship.
Education and training expansion by profession
- The proposed increase for each profession depends on the identified shortfalls, the routes to employment and the level of reliance on international recruitment, in addition to the factors outlined above.
Table 1: Increase required in education and training by profession
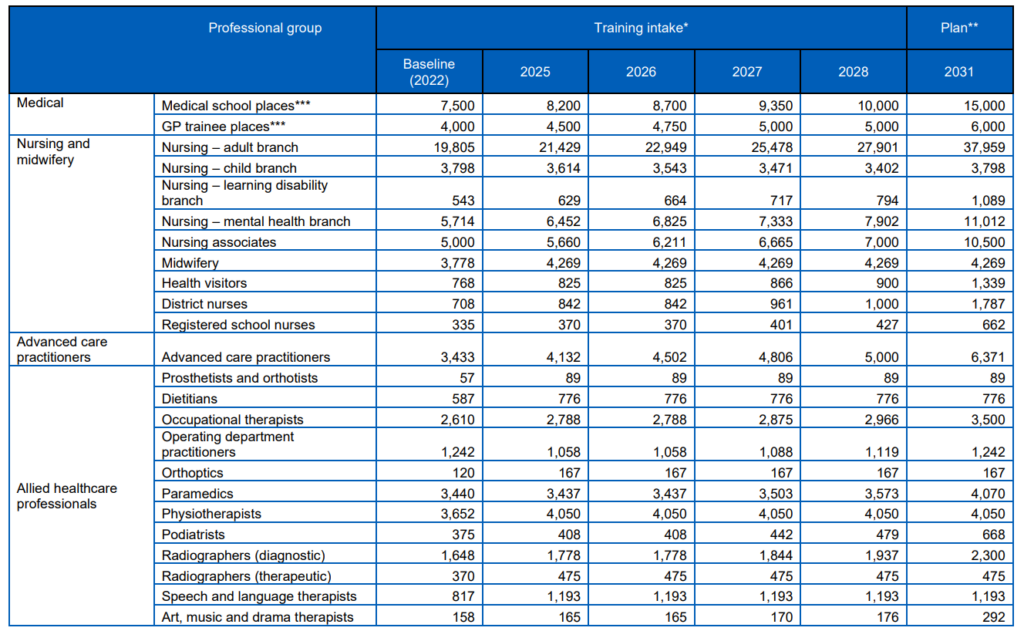
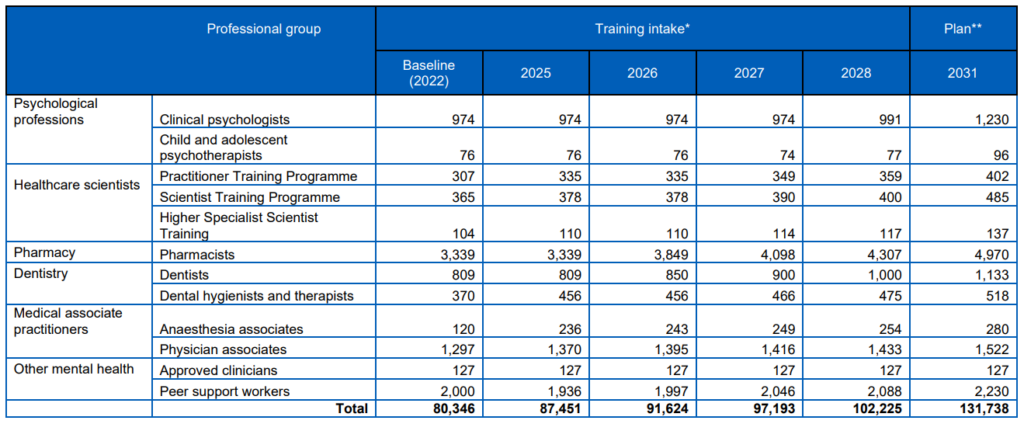
Table 1 data is repeated below in web format
| Professional group | Training intake* | Plan** | |||||
| Baseline (2022) | 2025 | 2026 | 2027 | 2028 | 2031 | ||
| Medical | Medical school places*** | 7,500 | 8,200 | 8,700 | 9,350 | 10,000 | 15,000 |
| GP trainee places*** | 4,000 | 4,500 | 4,750 | 5,000 | 5,000 | 6,000 | |
| Nursing and midwifery | Nursing – adult branch | 19,805 | 21,429 | 22,949 | 25,478 | 27,901 | 37,959 |
| Nursing – child branch | 3,798 | 3,614 | 3,543 | 3,471 | 3,402 | 3,798 | |
| Nursing – learning disability branch | 543 | 629 | 664 | 717 | 794 | 1,089 | |
|
Nursing – mental health branch |
5,714 |
6,452 |
6,825 |
7,333 |
7,902 |
11,012 | |
| Nursing associates | 5,000 | 5,660 | 6,211 | 6,665 | 7,000 | 10,500 | |
| Midwifery | 3,778 | 4,269 | 4,269 | 4,269 | 4,269 | 4,269 | |
| Health visitors | 768 | 825 | 825 | 866 | 900 | 1,339 | |
| District nurses | 708 | 842 | 842 | 961 | 1,000 | 1,787 | |
| Registered school nurses | 335 | 370 | 370 | 401 | 427 | 662 | |
| Advanced care practitioners | Advanced care practitioners | 3,433 | 4,132 | 4,502 | 4,806 | 5,000 | 6,371 |
|
Allied healthcare professionals | Prosthetists and orthotists | 57 | 89 | 89 | 89 | 89 | 89 |
| Dietitians | 587 | 776 | 776 | 776 | 776 | 776 | |
| Occupational therapists |
2,610 | 2,788 | 2,788 | 2,875 | 2,966 | 3,500 | |
| Operating department practitioners | 1,242 | 1,058 | 1,058 | 1,088 | 1,119 | 1,242 | |
| Orthoptics | 120 | 167 | 167 | 167 | 167 | 167 | |
| Paramedics | 3,440 | 3,437 | 3,437 | 3,503 | 3,573 | 4,070 | |
| Physiotherapists | 3,652 | 4,050 | 4,050 | 4,050 | 4,050 | 4,050 | |
| Podiatrists | 375 | 408 | 408 | 442 | 479 | 668 | |
| Radiographers (diagnostic) | 1,648 | 1,778 | 1,778 | 1,844 | 1,937 | 2,300 | |
| Radiographers (therapeutic) | 370 | 475 | 475 | 475 | 475 | 475 | |
| Speech and language therapists | 817 | 1,193 | 1,193 | 1,193 | 1,193 | 1,193 | |
| Art, music and drama therapists | 158 | 165 | 165 | 170 | 176 | 292 | |
| Professional group | Training intake* | Plan** | |||||
| Baseline (2022) | 2025 | 2026 | 2027 | 2028 | 2031 | ||
| Psychological professions | Clinical psychologists | 974 | 974 | 974 | 974 | 991 | 1,230 |
| Child and adolescent psychotherapists | 76 | 76 | 76 | 74 | 77 | 96 | |
| Healthcare scientists | Practitioner Training Programme | 307 | 335 | 335 | 349 | 359 | 402 |
| Scientist Training Programme | 365 | 378 | 378 | 390 | 400 | 485 | |
| Higher Specialist Scientist Training | 104 | 110 | 110 | 114 | 117 | 137 | |
| Pharmacy | Pharmacists | 3,339 | 3,339 | 3,849 | 4,098 | 4,307 | 4,970 |
|
Dentistry | Dentists | 809 | 809 | 850 | 900 | 1,000 | 1,133 |
| Dental hygienists and therapists | 370 | 456 | 456 | 466 | 475 | 518 | |
| Medical associate practitioners | Anaesthesia associates | 120 | 236 | 243 | 249 | 254 | 280 |
| Physician associates | 1,297 | 1,370 | 1,395 | 1,416 | 1,433 | 1,522 | |
| Other mental health | Approved clinicians | 127 | 127 | 127 | 127 | 127 | 127 |
| Peer support workers | 2,000 | 1,936 | 1,997 | 2,046 | 2,088 | 2,230 | |
|
| Total | 80,346 | 87,451 | 91,624 | 97,193 | 102,225 | 131,738 |
* Current intake is based on the Student Data Collection which includes undergraduate, postgraduate and apprentices.
** The planned level of increase sits within a modelled range, where the level required is dependent on productivity and retention levels alongside other factors.
***Assumes proportional increase in postgraduate training (foundation training) and specialty training including the potential to further increase GP trainee places.
Considerations for the wider health and care sector
- Current clinical education pipelines do not exclusively support the NHS; they also provide trained staff to social care, charitable, special education and private and independent healthcare organisations. While the Plan only considers the workforce demand from NHS services, it is assumed that the expansion set out across domestic education and training would result in increases across the entire health and care pipeline. Specifically, it is assumed that the proportion of newly trained staff who move into non-NHS health and care settings would remain in line with current trends.
Priorities for working differently and education and training reform
- The assessed level of education and training expansion will need to be accompanied by wider education and training reforms. This will include measures to increase capacity in the education sector alongside designing education capacity into services across ICSs, which would be considered and implemented in partnership with key stakeholders. These actions include:
- education reforms to support bringing people into the workforce more efficiently and easily and more consistent recognition of previous learning
- expansion of education capacity, both educators and infrastructure
- clinical placement capacity expansion, multiprofessional ICS/pan-ICS co- ordination and management, which could improve both workforce supply and retention
- reform to adopt innovative and accessible modes of tuition and supervision
- more visible NHS career routes from T-levels through to enhanced careers
- financial architecture that supports efficient expansion, incentivising growth in the right professions and geographies
- apprentice routes for employers
- expansion of 18-month MSc postgraduate routes with funding
- support worker routes for part-time learners and those looking to access education through experience.
- Other factors to consider include:
- how the expansion of training places will address health inequalities and ensure all prospective students have equitable access to new courses
- more equitable spread of training opportunities across geographies
- more diverse and integrated clinical
Implementation
- The Plan sets out next steps for engagement and implementation. For education and training it will be essential for partners and stakeholders across the NHS and education sector to work together to support delivery of the proposed actions. Each stakeholder’s unique role and leverage to deliver the Plan will be acknowledged to achieve this.
- ICSs will be responsible for addressing current and future predicted workforce supply requirements in response to local needs. This includes piloting existing programmes to help learners and trainees develop generalist and core skills. They will continue to develop important relationships with education and training providers to secure domestic education capacity and efficiency. This will include attracting local people into health and care careers, through work with schools, colleges, local enterprise partnerships and local communities. This will ensure education and training planning is an integral part of both operational and strategic service, financial and workforce plans.
- The supply of core clinical professions, doctors, nurses, midwives and allied health professionals into the NHS relies on undergraduate degree programmes that are led and delivered by the university sector. To enable expansion in the right geographies and professions, consideration will also need to be given to how the NHS can direct the level, geography and mix of courses provided. To effectively plan and manage education capacity, NHS England will need to clearly communicate its strategic intent to the education sector and work in partnership with higher education institutions (HEIs) and professional regulators, both nationally and locally to deliver a workforce that meets the NHS’s needs.
- Continued engagement with regulators, royal colleges, the HEI sector and government will be key to ensuring support for and the ability to deliver education reforms.
Annex D: Abbreviations
| AA | Anaesthesia associate |
| ACCEND | Aspirant Cancer Career and Education Development |
| AHP | Allied health professions |
| AI | Artificial intelligence |
| APEL | Accrediting prior experiential learning |
| ARRS | Additional Roles Reimbursement Scheme |
| CEGPR | Certificate of Eligibility for GP Registration |
| CESR | Certificate of Eligibility for Specialist Registration |
| CIPD | Chartered Institute of Professional Development |
| CPD | Continuing professional development |
| CVD | Cardiovascular disease |
| DASV | Domestic abuse and sexual violence |
| DHSC | Department of Health and Social Care |
| ESFA | Education and Skills Funding Agency |
| ESR | Electronic staff record |
| EVP | Employee value proposition |
| FDP | Federated Data Platform |
| FTE | Full-time equivalent |
| GP | General practitioner |
| GMC | General Medical Council |
| HEI | Higher education institute |
| HLE | Healthy life expectancy |
| ICB | Integrated care board |
| JFPs | Joint forward plans |
| LED | Locally employed doctor |
| MECC | Making Every Contact Count |
| MHP | Mental health practitioner |
| NA | Nursing associate |
| NIHR | National Institute for Health and Care Research |
| NMC | Nursing and Midwifery Council |
| ODP | Operating department practitioner |
| OECD | Organisation for Economic Co-operation and Development |
| OHWB | Occupational health and wellbeing |
| OOPP pilot | Out of Programme Pause pilot |
| PA | Physician associate |
| PTP | Practitioner Training Programme |
| RPA | Robotic process automation |
| SAS doctor | Specialty and associate specialist doctor |
| SDEC | Same day emergency care |
| STP | Scientist Training Programme |
| WDES | Workforce Disability Equality Standard |
| WRES | Workforce Race Equality Standard |
References
1 NHS England (July 2020). We are the NHS: People Plan for 2020/21 – action for us all. https://www.england.nhs.uk/publication/we-are-the-nhs-people-plan-for-2020-21-action-for-us-all/
2 NHS England (July 2021). Our NHS People Promise. https://www.england.nhs.uk/publication/our-nhs-people-promise/
3 Department of Health and Social Care (June 2022). Leadership for a collaborative and inclusive future. https://www.gov.uk/government/publications/health-and-social-care-review-leadership-for-a-collaborative-and- inclusive-future/leadership-for-a-collaborative-and-inclusive-future
4 NHS England (May 2023). NHS workforce statistics – February 2023 (Including selected provisional statistics for March 2023.
5 NHS Digital (June 2023). General Practice Workforce, 31 May 2023. https://digital.nhs.uk/data-and-information/publications/statistical/general-and-personal-medical-services/31- may-2023
6 NHS England (June 2023). General Practice Workforce, 31 May 2023. https://digital.nhs.uk/data-and-information/publications/statistical/general-and-personal-medical-services/31- may-2023
7 Department of Health and Social Care (July 2021). Chief Medical Officer’s annual report 2021: health in coastal communities.
8 NHS England (May 2023). NHS workforce statistics – February 2023 (Including selected provisional statistics for March 2023.
9 The Health Foundation (November 2019). Falling short: The NHS workforce challenge. https://www.health.org.uk/publications/reports/falling-short-the-nhs-workforce-challenge
10 General Medical Council (October 2021). The state of medical education and practice in the UK: The workforce report 2022.
11 Nursing and Midwifery Council. Registration data reports.
12 NHS England (May 2023). NHS Vacancy Statistics England, April 2015–March 2023, Experimental Statistics. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-vacancies-survey/april-2015—march- 2023-experimental-statistics
13 NHS (January 2019). The NHS Long Term Plan. https://www.longtermplan.nhs.uk/
14 NHS England (February 2023). NHS Workforce Race Equality Standard (WRES) 2022 data analysis report for NHS trusts.
15 Health Education England (February 2019). The Topol Review: Preparing the healthcare workforce to deliver the digital future.
16 NHS England (May 2023). Primary Care Workforce Quarterly Update, 31 March 2023, Experimental Statistics. https://digital.nhs.uk/data-and-information/publications/statistical/primary-care-workforce-quarterly-update/31- march-2023
17 NHS England (May 2023). NHS workforce statistics – February 2023 (Including selected provisional statistics for March 2023.
18 NHS England (June 2023). General Practice Workforce, 31 May 2023. https://digital.nhs.uk/data-and-information/publications/statistical/general-and-personal-medical-services/31- may-2023
19 HM Treasury (March 2023). Spring Budget 2023. https://www.gov.uk/government/publications/spring-budget-2023
20 HM Treasury (March 2023). Spring Budget 2023. https://www.gov.uk/government/publications/spring-budget-2023
21 NHS (June 2021). Integrated Care Systems: design framework (2021). https://www.england.nhs.uk/publication/integrated-care-systems-guidance/#ics-design-framework
22 NHS England (August 2021). Building strong integrated care systems everywhere: guidance on the integrated care system people function.
23 Health Education England (October 2021). Working differently together: Progressing a one workforce approach. https://www.hee.nhs.uk/sites/default/files/documents/HEE_MDT_Toolkit_V1.1.pdf
24 NHS England (November 2021). The future of NHS human resources and organisational development report.
25 NHS Confederation (July 2022). System on a cliff edge: addressing challenges in social care capacity. https://www.nhsconfed.org/publications/system-cliff-edge-addressing-challenges-social-care-capacity
26 Department of Health and Social Care (December 2021). People at the Heart of Care: adult social care reform white paper. https://www.gov.uk/government/publications/people-at-the-heart-of-care-adult-social-care-reform-white-paper
27 Department of Health and Social Care (April 2023). Next steps to put People at the Heart of Care. https://www.gov.uk/government/publications/adult-social-care-system-reform-next-steps-to-put-people-at-the- heart-of-care/next-steps-to-put-people-at-the-heart-of-care
28 NHS England (October 2022). NHS England operating framework. https://www.england.nhs.uk/publication/operating-framework/
29 Office for National Statistics (January 2022). National population projections: 2020-based interim. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/bulletin s/nationalpopulationprojections/2020basedinterim
30 British Geriatrics Society (June 2014). Introduction to Frailty, Fit for Frailty Part 1. https://www.bgs.org.uk/resources/introduction-to- frailty#:~:text=What%20is%20frailty%3F%20Frailty%20is%20a%20distinctive%20health,and%20a%20half%2 0of%20those%20aged%20over%2085
31 Institute for Fiscal Studies (May 2017). UK health spending. https://ifs.org.uk/publications/uk-health-spending
32 NHS Digital (September 2022). Hospital Admitted Patient Care Activity, 2021–22. https://digital.nhs.uk/data-and-information/publications/statistical/hospital-admitted-patient-care-activity
33 Office for National Statistics. Population estimates. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates
34 Office for National Statistics (April 2022). Health state life expectancies by national deprivation deciles, England: 2018 to 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthinequalities/bulletins/health statelifeexpectanciesbyindexofmultipledeprivationimd/2018to2020
35 British Medical Journal (January 2020). Rising to the challenge of multimorbidity. https://www.bmj.com/content/368/bmj.l6964
36 Office for National Statistics (July 2020). Living longer: trends in subnational ageing across the UK. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/ageing/articles/livinglongert rendsinsubnationalageingacrosstheuk/2020-07-20
37 Office for National Statistics (August 2018). Living longer: how our population is changing and why it matters. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/ageing/articles/livinglonger howourpopulationischangingandwhyitmatters/2018-08-13
38 British Medical Journal (January 2020). Rising to the challenge of multimorbidity. https://www.bmj.com/content/368/bmj.l6964
39 NHS England (May 2023). NHS Workforce Statistics – February 2023 (Including selected provisional statistics for March 2023). https://digital.nhs.uk/data-and-information/publications/statistical/nhs-workforce-statistics/february-2023
40 NHS Digital (June 2023). General Practice Workforce, 31 May 2023. https://digital.nhs.uk/data-and-information/publications/statistical/general-and-personal-medical-services/31- may-2023
41 NHS England. Internal management information. Various sources.
42 NHS England (May 2023). NHS Workforce Statistics – February 2023 (Including selected provisional statistics for March 2023). https://digital.nhs.uk/data-and-information/publications/statistical/nhs-workforce-statistics/february-2023
43 NHS Digital (June 2023). General Practice Workforce, 31 May 2023. https://digital.nhs.uk/data-and-information/publications/statistical/general-and-personal-medical-services/31- may-2023
44 NHS England (March 2023). NHS Staff Survey national results 2022. https://www.nhsstaffsurveys.com/results/
45 OECD iLibrary. Health resources – doctors. https://www.oecd-ilibrary.org/social-issues-migration-health/doctors/indicator/english_4355e1ec- en?parentId=http%3A%2F%2Finstance.metastore.ingenta.com%2Fcontent%2Fthematicgrouping%2F777a95 75-en
46 OECD.Stat (March 2023). Health Care Resources: Number of GPs per 1000 population. https://stats.oecd.org/Index.aspx?QueryId=106894
47 OECD iLibrary. Health resources – nurses. https://www.oecd-ilibrary.org/social-issues-migration-health/nurses/indicator/english_283e64de- en?parentId=http%3A%2F%2Finstance.metastore.ingenta.com%2Fcontent%2Fthematicgrouping%2F777a95 75-en
48 OECD iLibrary Health resources. https://doi.org/10.1787/777a9575-en
49 OECD iLibrary. Health resources – doctors. https://www.oecd-ilibrary.org/social-issues-migration-health/doctors/indicator/english_4355e1ec- en?parentId=http%3A%2F%2Finstance.metastore.ingenta.com%2Fcontent%2Fthematicgrouping%2F777a95 75-en
50 OECD iLibrary. Health resources – nurses. https://www.oecd-ilibrary.org/social-issues-migration-health/nurses/indicator/english_283e64de- en?parentId=http%3A%2F%2Finstance.metastore.ingenta.com%2Fcontent%2Fthematicgrouping%2F777a95 75-en
51 OECD iLibrary. Health resources – medical graduates. https://www.oecd-ilibrary.org/social-issues-migration-health/medical-graduates/indicator/english_ac5bd5d3- en?parentId=http%3A%2F%2Finstance.metastore.ingenta.com%2Fcontent%2Fthematicgrouping%2F777a95 75-en
52 OECD Data: Health resources – nursing graduates. https://www.oecd-ilibrary.org/social-issues-migration-health/nursing-graduates/indicator/english_c54611e3- en?parentId=http%3A%2F%2Finstance.metastore.ingenta.com%2Fcontent%2Fthematicgrouping%2F777a95 75-en
53 NHS England. NHS providers: trust accounts consolidation (TAC) data publications. https://www.england.nhs.uk/financial-accounting-and-reporting/nhs-providers-tac-data-publications/
54 Journal of Nursing Scholarship, Dall’Ora et al (December 2019). Temporary Staffing and Patient Death in Acute Care Hospitals: A Retrospective Longitudinal Study. https://sigmapubs.onlinelibrary.wiley.com/doi/full/10.1111/jnu.12537
55 The Health Foundation (November 2019). Falling short: The NHS workforce challenge. https://www.health.org.uk/publications/reports/falling-short-the-nhs-workforce-challenge
56 NHS England (April 2023). NHS workforce statistics – December 2022 (Including selected provisional statistics for January 2023). https://digital.nhs.uk/data-and-information/publications/statistical/nhs-workforce-statistics/december- 2022https://digital.nhs.uk/data-and-information/publications/statistical/nhs-workforce-statistics/february-2023
57 General Medical Council (October 2021). The state of medical education and practice in the UK: The workforce report 2022. https://www.gmc-uk.org/-/media/documents/workforce-report-2022—full-report_pdf-94540077.pdf
58 World Health Organization (October 2022). Ageing and health. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health
59 Nuffield Trust (October 2021). Recruitment of nurses from overseas: Exploring the factors affecting levels of international recruitment. https://www.nuffieldtrust.org.uk/files/2021-11/recruitment-of-nurses-drivers-web2.pdf
60 Office for National Statistics (January 2022). Population projections. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/#datas ets
61 NHS (January 2019). The NHS Long Term Plan. https://www.longtermplan.nhs.uk/
62 OECD (2022). OECD Health Statistics 2022. https://www.oecd.org/health/health-data.htm
63 NHS England (May 2023). NHS workforce statistics – February 2023 (Including selected provisional statistics for March 2023. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-workforce-statistics/february-2023
64 OECD iLibrary (November 2021). Health at a Glance OECD indicators. https://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-2021_ae3016b9-en https://www.england.nhs.uk/statistics/statistical-work-areas/rtt-waiting-times/rtt-data-2022-23/
65 Office for National Statistics (June 2020). Coronavirus and depression in adults, Great Britain: June 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/articles/coronavirusanddepressioninadultsg reatbritain/june2020
66 NHS England (May 2023). NHS mental health dashboard. https://www.england.nhs.uk/publication/nhs-mental-health-dashboard/
67 Skills for Care (October 2022). The state of the adult social care sector and workforce in England. https://www.skillsforcare.org.uk/Adult-Social-Care-Workforce-Data/Workforce- intelligence/publications/national-information/The-state-of-the-adult-social-care-sector-and-workforce-in- England.aspx
68 Community Integrated Care (July 2021). Unfair to Care: Understanding the social care pay gap and how to close it. https://www.unfairtocare.co.uk/wp-content/uploads/2021/07/Unfair-To-Care-Full-Report-Single-Pages.pdf
69 Skills for Care (October 2022). The state of the adult social care sector and workforce in England. https://www.skillsforcare.org.uk/Adult-Social-Care-Workforce-Data/Workforce- intelligence/publications/national-information/The-state-of-the-adult-social-care-sector-and-workforce-in- England.aspx
70 Skills for Care (October 2022). The state of the adult social care sector and workforce in England. https://www.skillsforcare.org.uk/Adult-Social-Care-Workforce-Data/Workforce- intelligence/publications/national-information/The-state-of-the-adult-social-care-sector-and-workforce-in- England.aspx
71 World Health Organization (June 2021). Ethics and governance of artificial intelligence for health. https://www.who.int/publications/i/item/9789240029200
72 National Human Genome Research Institute (January 2022). Artificial Intelligence, Machine Learning and Genomics. https://www.genome.gov/about-genomics/educational-resources/fact-sheets/artificial-intelligence-machine- learning-and-genomics
73 Health Education England (February 2019). The Topol Review: Preparing the healthcare workforce to deliver the digital future. https://topol.hee.nhs.uk/
74 NHS England (March 2023). NHS Staff Survey national results 2022. https://www.nhsstaffsurveys.com/results/
75 NHS England (July 2021). Our NHS People Promise. https://www.england.nhs.uk/publication/our-nhs-people-promise/
76 NHS England (February 2023). NHS Workforce Race Equality Standard (WRES) 2022 data analysis report for NHS trusts.
77 NHS England (March 2023). NHS Staff Survey national results 2022. https://www.nhsstaffsurveys.com/results/
78 NHS England (February 2023). NHS Workforce Race Equality Standard (WRES) 2022 data analysis report for NHS trusts.
79 NHS England (March 2023). NHS Staff Survey national results 2022.
80 NHS England (June 2023). General Practice Workforce, 31 May 2023. https://digital.nhs.uk/data-and-information/publications/statistical/general-and-personal-medical-services/31- may-2023
81 NHS England (April 2022). Ockenden review of maternity services. https://www.england.nhs.uk/publication/ockenden-review-of-maternity-services/
82 Health Education England. Student Data Collection. https://www.hee.nhs.uk/our-work/hee-national-data-function/ecollection/student-data-collection
83 Health Education England. Medical Doctor Degree Apprenticeship. https://www.hee.nhs.uk/our-work/talent-care-widening-participation/apprenticeships/medical-doctor-degree- apprenticeship
84 NHS England (April 2022). Ockenden review of maternity services. https://www.england.nhs.uk/publication/ockenden-review-of-maternity-services/
85 Office for National Statistics (January 2022). Principal projection – England summary: 2020-based interim edition of this dataset. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/dataset s/tablea14principalprojectionenglandsummary
86 Office for National Statistics (August 2022). Births in England and Wales: 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/bulletins/birthsum marytablesenglandandwales/2021
87 NMPA Project Team (June 2022). National Maternity and Perinatal Audit: Clinical Report 2022. Based on births in NHS maternity services in England and Wales between 1 April 2018 and 31 March 2019. https://maternityaudit.org.uk/FilesUploaded/Ref%20336%20NMPA%20Clinical%20Report_2022.pdf
88 NHS England (March 2023). Three year delivery plan for maternity and neonatal services. https://www.england.nhs.uk/long-read/three-year-delivery-plan-for-maternity-and-neonatal-services/
89 World Health Organization (May 2010). WHO Global Code of Practice on the International Recruitment of Health Personnel https://www.who.int/publications/i/item/wha68.32
90 Department for Education (December 2022). National statistics: Apprenticeships and traineeships. https://explore-education-statistics.service.gov.uk/find-statistics/apprenticeships-and-traineeships/2021-22
91 NHS England. Internal management information. Various sources.
92 Health Education England. Student Data Collection. https://www.hee.nhs.uk/our-work/hee-national-data-function/ecollection/student-data-collection
93 NHS Employers (December 2020). Retaining 100% of nurse degree apprentices. https://www.nhsemployers.org/articles/retaining-100-cent-nurse-degree-apprentices
94 NHS England (August 2021). Building strong integrated care systems everywhere: guidance on the integrated care system people function. https://www.england.nhs.uk/wp-content/uploads/2021/06/B0662_Building-strong-integrated-care-systems- everywhere-guidance-on-the-ICS-people-function-August-2021.pdf)
95 The Health Foundation (August 2019). Building healthier communities: the role of the NHS as an anchor institution. https://www.health.org.uk/publications/reports/building-healthier-communities-role-of-nhs-as-anchor-institution
96 Inspire, attract and recruit toolkit: Resources and guidance to support your workforce supply. https://www.nhsemployers.org/toolkits/inspire-attract-and-recruit-toolkit
97 Health Anchors Learning Network. https://haln.org.uk/
98 NHS England (June 2022). NHS estates and facilities workforce action plan. https://www.england.nhs.uk/publication/nhs-estates-and-facilities-workforce-action-plan/
99 Helpforce. Case studies. https://helpforce.community/iandi/projects
100 The King’s Fund (March 2013). Volunteering in health and care. https://www.kingsfund.org.uk/publications/volunteering-health-and-care
101 The King’s Fund (November 2013). Volunteering in acute trusts. https://www.kingsfund.org.uk/publications/volunteering-acute-trusts-england
102 The King’s Fund (December 2018). The role of volunteers in the NHS: views from the front line. https://www.kingsfund.org.uk/publications/role-volunteers-nhs-views-front-line
103 NHS England (June 2023). NHS Volunteering Taskforce – report and recommendations https://www.england.nhs.uk/long-read/nhs-volunteering-taskforce-report-and-recommendations/
104 NHS England. NHS and Care Volunteer Responders. https://nhscarevolunteerresponders.org/
105 St John Ambulance. NHS Cadets https://nhscadets.sja.org.uk/
106 Helpforce. Volunteer to Career. https://helpforce.community/back-to-health/volunteer-to-career-programme
107 NHS England (May 2023). Workforce Statistics – February 2023 (Including selected provisional statistics for March 2023) https://digital.nhs.uk/data-and-information/publications/statistical/nhs-workforce-statistics/february-2023
108 The Institute for Fiscal Studies (August 2022). Factors associated with staff retention in the NHS acute sector.
https://ifs.org.uk/sites/default/files/2022-08/IFS-R216-Factors-associated-with-staff-retention-in-the-NHS- acute-sector_0.pdf
109 NHS England (July 2021). Our NHS People Promise. https://www.england.nhs.uk/publication/our-nhs-people-promise/
110 NHS England (July 2020). We are the NHS: People Plan for 2020/21 – action for us all. https://www.england.nhs.uk/publication/we-are-the-nhs-people-plan-for-2020-21-action-for-us-all/
111 NHS England. Looking After Our People – Retention hub. https://www.england.nhs.uk/looking-after-our-people/
112 NHS England. National People Promise Exemplar Sites. https://www.england.nhs.uk/looking-after-our-people/our-pathfinders/
113 Academy of Medical Royal Colleges (January 2022). Workforce: recruitment, training and retention in health and social care Inquiry. https://www.aomrc.org.uk/wp-content/uploads/2022/01/ATDG_HSC_inquiry_response_0122.pdf
114 Royal College of Nursing (March 2022). Parliamentary submission: Workforce: Recruitment, Training and Retention in Health and Social Care. https://www.rcn.org.uk/About-us/Our-Influencing-work/Policy-briefings/conr-15721
115 Daniels, J., Robinson, E., Jenkinson, E & Carlton, E. (2023) Psychologically Informed Practice and Policy (PiPP) Project: Study Recommendations. Royal College of Emergency Medicine, accessed from
https://rcem.ac.uk/psychologically-informed-practice-and-policy-pipp/
116 NHS England. Our Leadership Way. https://www.leadershipacademy.nhs.uk/organisational-resources/our-leadership-way/
117 Department of Health and Social Care (February 2019). Kark review of the fit and proper person test. https://www.gov.uk/government/publications/kark-review-of-the-fit-and-proper-persons-test
118 Department of Health and Social Care (June 2022). Leadership for a collaborative and inclusive future. https://www.gov.uk/government/publications/health-and-social-care-review-leadership-for-a-collaborative-and- inclusive-future/leadership-for-a-collaborative-and-inclusive-future
119 NHS England (November 2021). The future of NHS human resources and organisational development report. https://www.england.nhs.uk/publication/the-future-of-nhs-human-resources-and-organisational-development- report/
120 The King’s Fund (2012). Employee engagement and NHS performance. https://assets.kingsfund.org.uk/f/256914/x/f7572997c3/employee_engagement_nhs_performance_west_dawson_leadership_review2012_paper.pdf
121 General Medical Council (November 2019). Caring for doctors, Caring for patients. https://www.gmc-uk.org/-/media/documents/caring-for-doctors-caring-for-patients_pdf-80706341.pdf
122 The King’s Fund (September 2020). The courage of compassion: Supporting nurses and midwives to deliver high-quality care. https://www.kingsfund.org.uk/publications/courage-compassion-supporting-nurses-midwives
123 NHS England (October 2022). NHS England operating framework. https://www.england.nhs.uk/publication/operating-framework/
124 NHS England (August 2021). Building strong integrated care systems everywhere: guidance on the integrated care system people function.
125 NHS England (May 2022). Next steps for integrating primary care: Fuller Stocktake report. https://www.england.nhs.uk/publication/next-steps-for-integrating-primary-care-fuller-stocktake-report/
126 NHS England (February 2023). NHS Workforce Race Equality Standard (WRES) 2022 data analysis report for NHS trusts.
127 NHS England (February 2023). NHS Workforce Race Equality Standard (WRES) 2022 data analysis report for NHS trusts.
128 NHS England (May 2022). Workforce Disability Equality Standard: 2021 data analysis report for NHS trusts and foundation trusts.
129 NHS England (March 2023). NHS Staff Survey national results 2022.
130 The King’s Fund (February 2020). What are health inequalities?
131 BMC Public Health, Fernandez Turienzo, C., Newburn, M., Agyepong, A. et al. January 2021). Addressing inequities in maternal health among women living in communities of social disadvantage and ethnic diversity. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-021-10182-4
132 NHS England (June 2023). NHS equality, diversity, and inclusion improvement plan. https://www.england.nhs.uk/long-read/nhs-equality-diversity-and-inclusion-improvement-plan/#conclusion
133 NHS England (November 2022). Combatting racial discrimation against minority ethnic nurses, midwives and nursing associates.
https://www.england.nhs.uk/long-read/combatting-racial-discrimination-against-minority-ethnic-nurses- midwives-and-nursing-associates/
134 NHS England. The Culture and Leadership programme. https://www.england.nhs.uk/culture/culture-leadership-programme/
135 HM Treasury (March 2023). Spring Budget 2023. https://www.gov.uk/government/publications/spring-budget-2023
136 NHS England (July 2021). Our NHS People Promise. https://www.england.nhs.uk/publication/our-nhs-people-promise/
137 NHS England (May 2022). Next steps for integrating primary care: Fuller Stocktake report. https://www.england.nhs.uk/publication/next-steps-for-integrating-primary-care-fuller-stocktake-report/
138 NHS England (February 2023). Listening well guidance – A blueprint for organisations to develop a local listening strategy.
139 NHS England (June 2022). Freedom to Speak Up policy for NHS.
https://www.england.nhs.uk/wp-content/uploads/2022/06/PAR1245i-NHS-freedom-to-speak-up-national- Policy-eBook.pdf
140 NHS England. NHS Staff Survey. https://www.nhsstaffsurveys.com/
141 NHS England. The National Quarterly Pulse Survey. https://www.england.nhs.uk/fft/nqps/
142 NHS England, NHS People Pulse. https://www.england.nhs.uk/nhs-people-pulse/
143 NHS England (March 2023). NHS Staff Survey national results 2022. https://www.nhsstaffsurveys.com/results/
144 NHS England (May 2023). NHS Sickness Absence Rates, January 2023. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-sickness-absence-rates/december-2022
145 NHS England (July 2022). NHS Sickness Absence Rates, January 2022 to March 2022, and Annual Summary 2009 to 2022, Provisional Statistics. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-sickness-absence-rates/nhs-sickness-absence-rates-january-2022-to-march-2022-and-annual-summary-2009-to-2020
146 NHS England (May 2023). NHS Sickness Absence Rates, January 2023. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-sickness-absence-rates/december-2022
147 PLOS ONE, Louise H. Hall, Judith Johnson, Ian Watt, Anastasia Tsipa, Daryl B. O’Connor (July 2016). Healthcare Staff Wellbeing, Burnout, and Patient Safety: A Systematic Review. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0159015
148 The Chartered Institute of Personnel and Development (April 2022). Health and wellbeing at work. https://www.cipd.co.uk/knowledge/culture/well-being/health-well-being-work
149 The King’s Fund (2012). Employee engagement and NHS performance. https://archive.kingsfund.org.uk/concern/published_works/000104276
150 NHS England. Professional nurse advocate. https://www.england.nhs.uk/nursingmidwifery/delivering-the-nhs-ltp/professional-nurse-advocate/
151 NHS England (January 2023) Growing occupational health and wellbeing together (OHWB) strategy. https://www.england.nhs.uk/publication/growing-occupational-health-and-wellbeing-together-strategy/
152 University of East Anglia (June 2020). Business cost effectiveness calculator. https://evolveworkplacewellbeing.org/business-calculator/
153 NHS England (May 2022). Next steps for integrating primary care: Fuller Stocktake report. https://www.england.nhs.uk/publication/next-steps-for-integrating-primary-care-fuller-stocktake-report/
154 NHS England. Wellbeing Guardians. https://www.england.nhs.uk/supporting-our-nhs-people/health-and-wellbeing-programmes/wellbeing- guardians/
155 NHS England (January 2023) Growing occupational health and wellbeing together (OHWB) strategy. https://www.england.nhs.uk/publication/growing-occupational-health-and-wellbeing-together-strategy/
156 NHS England. NHS health and wellbeing framework. https://www.england.nhs.uk/supporting-our-nhs-people/health-and-wellbeing-programmes/nhs-health-and- wellbeing-framework/
157 NHS England (March 2023). NHS Staff Survey national results 2022. https://www.nhsstaffsurveys.com/results/
158 NHS England. The Model Health System. https://www.england.nhs.uk/applications/model-hospital/
159 NHS England. NHS health and wellbeing framework. https://www.england.nhs.uk/supporting-our-nhs-people/health-and-wellbeing-programmes/nhs-health-and- wellbeing-framework/
160 NHS England. NHS health and wellbeing framework. https://www.england.nhs.uk/supporting-our-nhs-people/health-and-wellbeing-programmes/nhs-health-and- wellbeing-framework/
161 NHS England (November 2022). National standards for healthcare food and drink. https://www.england.nhs.uk/wp-content/uploads/2022/11/B0508-i-National-standards-for-healthcare-food-and- drink-Nove-2022.pdf
162 Office for National Statistics (November 2022). Domestic abuse in England and Wales overview: November 2022. https://www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/bulletins/domesticabuseinenglandand walesoverview/november2022
163 Cavell Nurses’ Trust (November 2017). Skint, shaken yet still caring: but who is caring for our nurses? https://cavell.org.uk/wp-content/uploads/2019/06/Skint-shaken-yet-still-caring-Key-Findings-Cavell-Nurses-Trust-Final.pdf
164 Department of Health and Social Care (July 2022). Women’s Health Strategy for England. https://www.gov.uk/government/publications/womens-health-strategy-for-england
165 HM Treasury (September 2019). Career boost for almost half a million frontline NHS staff. https://www.gov.uk/government/news/career-boost-for-almost-half-a-million-frontline-nhs-staff
166 Health Education England. Aspirant Cancer Career and Education Development programme. https://www.hee.nhs.uk/our-work/cancer-diagnostics/aspirant-cancer-career-education-development- programme
167 Department of Health and Social Care (Mar 2023). Commercial clinical trials in the UK: the Lord O’Shaughnessy review. https://www.gov.uk/government/publications/commercial-clinical-trials-in-the-uk-the-lord-oshaughnessy-review
168 Health Education England (June 2021). The National Education and Training Survey (NETS). https://www.hee.nhs.uk/our-work/quality/national-education-training-survey-nets
169 NHE Employers (February 2023) NHS Terms and Conditions of Service Handbook. https://www.nhsemployers.org/publications/tchandbook
170 NHS England (January 2022). Flexible working: Raising the standards for the NHS. https://www.england.nhs.uk/wp-content/uploads/2022/02/B0395-flexible-working-raising-the-standards-for-the- NHS.pdf
171 NHS Flex for The Future Programme – in conjunction with timewise. https://timewise.co.uk/nhs-flex-for-the-future-programme-resource-library/
172 NHS England. NHS Reservists. https://www.healthcareers.nhs.uk/we-are-nhs/nhs-reservists
173 NHS England (June 2023). Retired specialists set to help with tackling Covid backlog https://www.england.nhs.uk/2023/06/retired-specialists-set-to-help-with-tackling-covid-backlog/
174 The Chartered Institute of Personnel and Development (February 2017) Developing managers to manage sustainable employee engagement, health and wellbeing. https://www.cipd.co.uk/knowledge/culture/well-being/developing-managers-report
175 NHS Employers (March 2021) Do OD TEAM toolkit. https://www.nhsemployers.org/publications/do-od-team-toolkit
176 Department of Health and Social Care (June 2022). Leadership for a collaborative and inclusive future. https://www.gov.uk/government/publications/health-and-social-care-review-leadership-for-a-collaborative-and- inclusive-future/leadership-for-a-collaborative-and-inclusive-future
177 Health Education England (February 2019). The Topol Review: Preparing the healthcare workforce to deliver the digital future. https://topol.hee.nhs.uk/
178 Department of Health and Social Care (June 2022). Data saves lives: reshaping health and social care with data. https://www.gov.uk/government/publications/data-saves-lives-reshaping-health-and-social-care-with- data/data-saves-lives-reshaping-health-and-social-care-with-data
179 Department of Health and Social Care (June 2022). A plan for digital health and social care. https://www.gov.uk/government/publications/a-plan-for-digital-health-and-social-care/a-plan-for-digital-health- and-social-care#section-2-our-vision-for-a-digital-future
180 NHS England. The NHS AI Lab. https://transform.england.nhs.uk/ai-lab/
181 Willis M, Duckworth P, Coulter A, Meyer ET, Osborne M. Qualitative and quantitative approach to assess the potential for automating administrative tasks in general practice. BMJ Open. 2020; 10:e032412. https://bmjopen.bmj.com/content/10/6/e032412
182 The Health Foundation (June 2021). Switched on. How do we get the best out of automation and AI in health care? https://www.health.org.uk/publications/reports/switched-on
183 Health Education England (February 2019). The Topol Review: Preparing the healthcare workforce to deliver the digital future. https://topol.hee.nhs.uk/
184 Health Education England (February 2019). The Topol Review: Preparing the healthcare workforce to deliver the digital future. https://topol.hee.nhs.uk/
185 NHS England. AI Deployment Platform. https://transform.england.nhs.uk/ai-lab/ai-lab-programmes/ai-in-imaging/ai-deployment-platform/
186 Department of Health and Social Care (February 2023). Medical technology strategy. https://www.gov.uk/government/publications/medical-technology-strategy
187 Health Education England (February 2022). Health Education England publishes roadmap into use of AI in the NHS. https://www.hee.nhs.uk/news-blogs-events/news/health-education-england-publishes-roadmap-use-ai-nhs
188 Health Education England. Delivering education and training. https://digital-transformation.hee.nhs.uk/building-a-digital-workforce/dart-ed/delivering-education-and-training
189 Health Education England (May 2022). Understanding healthcare workers’ confidence in AI. https://digital-transformation.hee.nhs.uk/binaries/content/assets/digital-transformation/dart- ed/understandingconfidenceinai-may22.pdf
190 Health Education England (October 2022). Developing healthcare workers’ confidence in AI. https://digital-transformation.hee.nhs.uk/binaries/content/assets/digital-transformation/dart- ed/developingconfidenceinai-oct2022.pdf
191 Health Education England. Artificial Intelligence (AI) and Digital Healthcare Technologies Capability framework. https://digital-transformation.hee.nhs.uk/building-a-digital-workforce/dart-ed/horizon-scanning/ai-and-digital- healthcare-technologies
192 NHS England (May 2022). RPA in the NHS: Guidance for designing, delivering and sustaining RPA within the NHS. https://transform.england.nhs.uk/media/documents/RPA-Guidance-May-22.pdf
193 NHS England (May 2022). RPA in the NHS: Guidance for designing, delivering and sustaining RPA within the NHS. https://transform.england.nhs.uk/media/documents/RPA-Guidance-May-22.pdf
194 Health Tech Newspaper (January 2021). Feature: the rise of remote monitoring – what’s next? https://htn.co.uk/2021/01/07/feature-the-rise-of-remote-monitoring-whats-next/
195 NHS England. Supporting care with remote monitoring. https://transform.england.nhs.uk/covid-19-response/technology-nhs/supporting-the-innovation-collaboratives- to-expand-their-remote-monitoring-plans/
196 Department of Health and Social Care (June 2022). Data saves lives: reshaping health and social care with data. https://www.gov.uk/government/publications/data-saves-lives-reshaping-health-and-social-care-with- data/data-saves-lives-reshaping-health-and-social-care-with-data
197 NHS England (May 2022). Next steps for integrating primary care: Fuller stocktake report. https://www.england.nhs.uk/publication/next-steps-for-integrating-primary-care-fuller-stocktake- report/https://www.england.nhs.uk/publication/next-steps-for-integrating-primary-care-fuller-stocktake-report/
198 British Medical Journal – Rees MR, Bracewell M (June 2019). Academic factors in medical recruitment: evidence to support improvements in medical recruitment and retention by improving the academic content in medical posts. https://academic.oup.com/pmj/article/95/1124/323/6983980
199 Department of Health and Social Care (March 2022. 50,000 Nurses Programme: delivery update. https://www.gov.uk/government/publications/50000-nurses-programme-delivery-update/50000-nurses- programme-delivery-update
200 NHS England (October 2022). National preceptorship framework for nursing. https://www.england.nhs.uk/long-read/national-preceptorship-framework-for-nursing/
201 NHS learning hub. https://learninghub.nhs.uk/
202 NHS England. Core20PLUS5 (adults) – an approach to reducing healthcare inequalities. https://www.england.nhs.uk/about/equality/equality-hub/national-healthcare-inequalities-improvement- programme/core20plus5/
203 Southend-on Sea City Council, Halo Southend. https://www.halosouthend.co.uk/
204 South Essex College. Supported Internships. https://www.southessex.ac.uk/supported-internships
205 Medical Schools Council (December 2021). Active inclusion: Challenging exclusions in medical education. https://www.medschools.ac.uk/media/2918/active-inclusion-challenging-exclusions-in-medical-education.pdf
206 Health Education England. Enhance programme. https://www.hee.nhs.uk/our-work/enhancing-generalist-skills
161 General Medical Council (October 2021). The state of medical education and practice in the UK: The workforce report 2022. https://www.gmc-uk.org/-/media/documents/workforce-report-2022—full-report_pdf-94540077.pdf
208 General Medical Council. Certificate of Eligibility for Specialist Registration or Certificate of Eligibility for GP Registration application. https://www.gmc-uk.org/registration-and-licensing/join-the-register/registration-applications/specialist-application-guides/specialist-registration-portfolio
209 Health Education England. Doctors in training. https://www.hee.nhs.uk/our-work/doctors-training
210 Health Education England. XR Health UK. The Growing Value of XR in Healthcare. https://www.xrhealthuk.org/the-growing-value-of-xr-in-healthcare
211 Health Education England. Virtual and Hybrid Learning Faculty. https://www.hee.nhs.uk/our-work/technology-enhanced-learning/regional-resources
212 Health Education England (March 2023). Educator Workforce Strategy. https://www.hee.nhs.uk/our-work/educator-workforce-strategy
213 Nursing and Midwifery Council (March 2022). The NMC Register, England: 1 April 2021 – 31 March 2022. https://www.nmc.org.uk/globalassets/sitedocuments/data-reports/march-2022/nmc-register-data-march-2022- england.pdf
214 Health Education England (March 2015). Raising the Bar – Shape of Caring: A Review of the Future Education and Training of Registered Nurses and Care Assistants. https://www.hee.nhs.uk/our-work/shape-caring-review
215 King’s College London (November 2021). The Development of the Nursing Associate Role: The Postholder Perspective. https://kclpure.kcl.ac.uk/portal/en/publications/the-development-of-the-nursing-associate-role-the-postholder- perspective(87dfefa3-dbc0-4b76-99de-49f737d1d1ad).html
216 Health Education England. Anaesthesia Associates. https://www.hee.nhs.uk/our-work/anaesthesia-associates
217 General Medical Council (July 2022). Bringing physician associates and anaesthesia associates into regulation. https://www.gmc-uk.org/pa-and-aa-regulation-hub
218 Association of Anaesthesia Associates. FAQs. https://anaesthesiaassociates.org/general-info/faqs/
219 Intensive Care Society (December 2022). Critical care Outreach Practitioner Framework. https://ics.ac.uk/resource/ccopf.html
220 British Dietetic Association. Case Study – Primary Care Network Dietitians in Birmingham Community Health care NHS FT. https://www.bda.uk.com/resource/case-study-primary-care-network-dietitians-in-birmingham-community- healthcare-nhs-ft.html
221 Health Education England (December 2021). Multi-professional consultant-level practice capability and impact framework. https://www.hee.nhs.uk/sites/default/files/documents/Sept%202020%20HEE%20Consultant%20Practice%20Capability%20and%20Impact%20Framework.pdf
222 Health Education England (December 2021). Multi-professional consultant-level practice capability and impact framework. https://www.hee.nhs.uk/sites/default/files/documents/Sept%202020%20HEE%20Consultant%20Practice%20 Capability%20and%20Impact%20Framework.pdf
223 NHS England (May 2023). Primary Care Workforce Quarterly Update, 31 March 2023, Experimental Statistics. https://digital.nhs.uk/data-and-information/publications/statistical/primary-care-workforce-quarterly-update/31- march-2023
224 NHS England (January 2023). Building dental teams: Supporting the use of skill mix in NHS general dental practice – short guidance. https://www.england.nhs.uk/long-read/building-dental-teams-supporting-the-use-of-skill-mix-in-nhs-general- dental-practice-short-guidance/
225 Health Education England (September 2021). Advancing Dental Care Review: Final Report. https://www.hee.nhs.uk/our-work/advancing-dental-care
226 Health Education England (February 2019). Maternity Support Worker Competency, Education and Career Development Framework. https://www.hee.nhs.uk/our-work/maternity/maternity-support-workers
227 Health Education England (October 2021). AHP Support Worker Competency, Education and Career Development Framework. https://www.hee.nhs.uk/our-work/allied-health-professions/enable-workforce/developing-role-ahp-support- workers/ahp-support-worker-competency-education-career-development
228 NHS England. Healthcare support worker programme. https://www.england.nhs.uk/nursingmidwifery/healthcare-support-worker-programme/
229 Health Education England. Aspirant Cancer Career and Education Development programme. https://www.hee.nhs.uk/our-work/cancer-diagnostics/aspirant-cancer-career-education-development- programme
230 Skills for Care. Case study: The Doctors’ Assistant Role. https://www.skillsforhealth.org.uk/wp-content/uploads/2022/06/ID7-Doctors-Assistant.pdf
231 Skills for Care. Case study: The Doctors’ Assistant Role. https://www.skillsforhealth.org.uk/wp-content/uploads/2022/06/ID7-Doctors-Assistant.pdf
237 NHS England (2019). Induction guide for social prescribing link workers in primary care networks. https://www.england.nhs.uk/wp-content/uploads/2022/12/social-prescribing-link-worker-welcome-pack-web-2.pdf
233 NHS England (July 2019). NHS Mental Health Implementation Plan 2019/20 – 2023/24. https://www.longtermplan.nhs.uk/publication/nhs-mental-health-implementation-plan-2019-20-2023-24/
234 NHS England (April 2022). Diagnostic imaging network workforce guidance. https://www.england.nhs.uk/publication/diagnostic-imaging-network-workforce-guidance/
235 Health Education England. NHS Digital Academy. https://digital-transformation.hee.nhs.uk/digital-academy
236 Health Education England. Digital Skills Assessment Tool. https://digital-transformation.hee.nhs.uk/digital-academy/programmes/digital-skills-assessment-tool
237 Health Education England. Digital Learning Solutions. https://www.dls.nhs.uk/v2/Home/Welcome
238 Health Education England. Digital Health Leadership Programme. https://digital-transformation.hee.nhs.uk/digital-academy/programmes/digital-health-leadership-programme
239 Health Education England. Topol Digital Fellowships. https://topol.hee.nhs.uk/digital-fellowships/
240 Health Education England. Health Innovation Placement (HIP) programme. https://digital-transformation.hee.nhs.uk/digital-academy/programmes/health-innovation-placement-hip- pilot/health-innovation-placement-hip-programme
241 Health Education England. Informatics Skills Development Networks. https://www.hee.nhs.uk/our-work/supporting-our-digital-experts/regional-informatics-skills-development- networks-isdns
242 NHS Providers. Digital Boards development programme. https://nhsproviders.org/development-offer/digital-boards
243 Health education England. Fast Futures programme. https://digital-transformation.hee.nhs.uk/building-a-digital-workforce/fastfutures
244 NHS England (October 2022). Accelerating genomic medicine in the NHS. https://www.england.nhs.uk/publication/accelerating-genomic-medicine-in-the-nhs/
245 Personalised Care Institute. https://www.personalisedcareinstitute.org.uk/
246 Health Education England. Population Health Fellowship. https://www.hee.nhs.uk/our-work/population-health/population-health-fellowship-0
247 National Association of Primary Care (December 2021). The CARE programme. https://napc.co.uk/our-programmes/care/
248 Public Health England (October 2020). ASSIST-Lite screening tool: how to use. https://www.gov.uk/government/publications/assist-lite-screening-tool-how-to-use
249 Office for Health Improvement & Disparities (January 2023). Adult substance misuse treatment statistics 2021 to 2022: report. https://www.gov.uk/government/statistics/substance-misuse-treatment-for-adults-statistics-2021-to-2022/adult- substance-misuse-treatment-statistics-2021-to-2022-report
250 Health Education England (June 2020). Behaviour Change Development Framework and Toolkit. https://behaviourchange.hee.nhs.uk/
251 Health Education England (August 2022). Making Every Contact Count. https://www.hee.nhs.uk/our-work/population-health/making-every-contact-count-mecc
252 Health Education England. E-learning for healthcare. All Our Health. https://www.e-lfh.org.uk/programmes/all-our-health/
253 Health Education England. E-learning for healthcare (October 2022). All Our Health: Health disparities and health inequalities. https://portal.e-lfh.org.uk/Component/Details/778744
254 NHS England (November 2021). Making research matter: Chief Nursing Officer for England’s strategic plan for research. https://www.england.nhs.uk/publication/making-research-matter-chief-nursing-officer-for-englands-strategic- plan-for-research/
255 NHS England (May 2023). Chief Midwifery Officer for England’s strategic plan for research. https://www.england.nhs.uk/long-read/chief-midwifery-officer-for-englands-strategic-plan-for-research/
256 Postgraduate Medical Journal (June 2019). Academic factors in medical recruitment: evidence to support improvements in medical recruitment and retention by improving the academic content in medical posts. https://academic.oup.com/pmj/article/95/1124/323/6983980
257 Health Education England. Enhance programme. https://www.hee.nhs.uk/our-work/enhancing-generalist-skills
258 Health Education England. E-learning for healthcare. https://www.e-lfh.org.uk/
259 Health Education England (November 2019). Framework for the spread and adoption of workforce innovation. https://www.hee.nhs.uk/sites/default/files/documents/HEE%20-%20Model%20for%20spread%20and%20adoption%20worforce%20UPDATED%202022v1%20accesssible.pdf
260 Health Education England. HEE Star: Accelerating workforce design. https://www.hee.nhs.uk/our-work/hee-star
261 Skills for Health. Six steps methodology to integrated workforce planning. https://www.skillsforhealth.org.uk/info-hub/six-steps-methodology-to-integrated-workforce-planning/
262 Department of Health and Social Care (June 2022). The Future of UK Clinical Research Delivery: 2022 to 2025 implementation plan. https://www.gov.uk/government/publications/the-future-of-uk-clinical-research-delivery-2022-to-2025- implementation-plan
263 The Learning Healthcare Project (2015). Learning Healthcare System. https://learninghealthcareproject.org/background/learning-healthcare-system/
264 NHS England (August 2021). Building strong integrated care systems everywhere: guidance on the ICS people function.
265 Skills for Health (2008). Six steps methodology to integrated workforce planning. https://www.skillsforhealth.org.uk/info-hub/six-steps-methodology-to-integrated-workforce-planning/
266 NHS England (October 2022). NHS England operating framework. https://www.england.nhs.uk/publication/operating-framework/
267 Department of Health and Social Care (March 2022. 50,000 Nurses Programme: delivery update. https://www.gov.uk/government/publications/50000-nurses-programme-delivery-update/50000-nurses- programme-delivery-update
268 NHS England. Internal management information. Various sources.
269 Department of Health and Social Care (March 2022. 50,000 Nurses Programme: delivery update. https://www.gov.uk/government/publications/50000-nurses-programme-delivery-update/50000-nurses- programme-delivery-update
270 Office for National Statistics (January 2022). Population projections. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/#datas ets

