1. Introduction and evidence summary
The NHS remains under enormous pressure.
Our healthcare service continues to recover from the COVID-19 pandemic as well as the industrial action that saw 1.3 million appointments postponed. Despite this, there has been solid progress across several areas.
In September 2024, 73.0% of patients waited under 4 hours in A&E departments, an improvement on the 70.3% who did in October 2023. Furthermore, the number of patients waiting for an elective procedure has fallen from 7.77 million in September 2023 to 7.57 million in September 2024.
Overall, the NHS is providing more care contacts in 2024 across secondary care services, mental health and community health services than in 2023.
Despite these improvements, Lord Darzi’s recent Independent Investigation of the National Health Service in England highlights that the NHS in England still has a lot further to go in addressing access issues, the mixed quality of care (in particular from maternity and mental health services), and the need to shift resource allocation from hospital to community. The impact of COVID-19 led to significant backlogs in operations, exacerbating pre-existing challenges the NHS was facing.
Workforce issues have posed long-term challenges for the NHS – too few staff have resulted in burnout and a demoralised workforce which further exasperate recruitment challenges.
We have taken action to recruit more staff. The NHS has increased the number of Agenda for Change (AfC) staff over the last few years by 22% (22,106 FTE), supported by successful international recruitment activity. This permanent recruitment has reduced reliance on temporary staffing. In addition, the NHS has benefitted from a post-COVID boosted interest in NHS careers and training opportunities, although we are now starting to see this effect begin to drop off.
The AfC leaver rate for most staff groups has steadily returned from its peak of 9.2% in April 2022 to pre-pandemic levels. By June 2024, the AfC vacancy rate was 7.1% (96,000 FTE staff), down 1.8 percentage points (19,000 FTE staff) from the previous year.
The 5 nursing and midwifery high-impact actions was influential in meeting the previous government’s target of 50,000 more nurses by March 2024. In addition, nursing leaver rates dropped to 5.5% in June 2024, below the pre-pandemic average of 6.8%.
In 2023/24, total expenditure on non-medical temporary staffing decreased by 0.94% (£63 million) compared to 2022/23, largely due to a reduction in spending on agency staff. Non-medical agency costs made up 3.1% of the total NHS pay bill in 2023/24, down from 4% in 2022/23, representing a cost reduction of approximately £438 million (19%). The 2024/25 priorities and operational planning guidance aims to reduce agency spending to 3.2% of the total pay bill in 2024/25.
Perceptions of health and wellbeing among staff have slightly improved, though burnout, stress and musculoskeletal (MSK) issues persist, especially among ambulance staff and nurses. Sickness absence was at 4.9% in June 2024, compared to 4.4% in June 2019, with mental health and MSK issues cited as major causes. COVID-19 highlighted an upward trend which has continued post pandemic.
We have worked to spread best practice on retention. In 2023/24 the People Promise Exemplars Programme was expanded to 116 more organisations, focusing on enhancing staff retention through improvement cycles and targeted equality, diversity and inclusion interventions.
Pay has been an historical issue. We were pleased to see the significant progress with the pay award for 2024/25 delivering a 5.5% uplift to all pay points for AfC staff on a consolidated basis and adding an intermediate pay point for Bands 8a–d and 9. Consultative ballots show that most unions endorsed the award, though not the Royal College of Nursing.
The results of the 2024 NHS Staff Survey are not yet available. We will share the analysis as early as we can following publication (anticipated March 2025). However, the 2023 NHS Staff Survey did show improved ‘recognised and rewarded’ scores across all AfC groups and average pay satisfaction at 31.2%, but still below the pre-pandemic score of 38.0% in 2019. Ambulance staff (23.6%) and healthcare assistants (19.9%) remained the least satisfied.
Going into next year, NHS funding will be extremely tight, and it will constitute a year of significant consolidation.
The NHS revenue settlement is likely to grow by 2% in real terms from which all pressures must be met including unavoidable elements like non-pay inflation, new medicines and treatments approved by the National Institute for Health and Care Excellence (NICE) and a series of other pressures, as well as pay settlements.
In that context, the NHS will not be able to make material investments in new services and meet all its pressures from the uplift available, including the usual growth in capacity that is necessary to meet demand growth. It is possible that some services will see real terms cuts in funding and activity after allowing for the pay settlement, depending on its scale.
NHS staff work incredibly hard. We want to see them fairly rewarded, in a way that strikes the right balance on resources so that they have the ability to deliver the care they want to for patients. Our view on affordability considers the likely NHS budget from discussions to date with DHSC and what was set out by HM Treasury in the Autumn Budget 2024. Based on this, we propose to set allocations for NHS planning on the basis of a 2.8% pay settlement. Every 0.5% increase above that costs around £700m; which is the equivalent to around 2% of elective activity (greater than 300k completed patient pathways).
We have already made significant prioritisation decisions. Pay awards above what has already been allocated will require further tough re-prioritisation of the decisions already made, significantly impacting patient care and in turn making the day-to-day job of NHS staff even harder.
2. NHS finances
2.1 Financial context
The indicative NHS England budget confirmed with the Department of Health and Social Care (DHSC) for 2024/25 is currently £186.6 billion, including education funding and the cost of the former NHS Digital. This budget also includes additional funding from the government to meet the unplanned costs of industrial action and some of the cost of the higher than planned pay award and pay reform deals, and for additional elective activity above the core funded level. The budget is likely to change as we confirm further transfers of funding within the DHSC group before the end of the financial year.
Plans to deliver within the available budget have required significant efficiency from local systems and providers, partly a deliberate decision to require higher efficiency post pandemic (SR21 set a target of at least 2.2%), and partly the result of higher than planned and funded inflation over the last few years and in 2024/25. The efficiency requirement identified in 2024/25 system plans is £9.3 billion (equivalent to 6.9% of their total allocation), which compares to £7.2 billion (5.4% of allocations) of efficiencies delivered in 2023/24. While systems are likely to deliver more efficiencies in 2024/25 compared to 2023/24, there is a risk they may not deliver these planned efficiencies. Several systems set financial plans based on a deficit, and this has required NHS England to identify cuts in frontline service investment to set a balanced overall plan.
We are confirming with Government how to implement the DHSC 2025/26 resource settlement as part of the planning process, at which point we will be able to confirm the NHS England allocation for the next financial year.
The NHS needs to plan for and manage the impact of Pay Review Body recommendations on headline pay increases. The Spending Review set out the government’s expectation that additional in-year resource will not be provided for pay awards in 2025/26. We have already made significant prioritisation decisions. Pay awards above what has already been allocated will require further tough re-prioritisation of the decisions already made.
2.2 Financial support for education and training
From the start of 2022/23, we have been sharing statements about the financial support we provide for education and training and the corresponding activity delivered by providers within each of the 42 integrated care system (ICSs) geographical footprints. Our aim has been to:
- increase the transparency of educational funding flows to enable ICS-level strategic discussions on our investment, including its alignment to ICS clinical strategy delivery and long-term service sustainability
- inform the development of an education and training plan for each ICS
Our NHS education funding guidance 2022/23 standardises and clarifies payment rates. We did not publish 2023/24 guidance, but we will do for 2024/25 and thereafter it will be an annual publication.
2.3 Affordability
Pay remains the largest component of NHS costs (around 65% of total operating costs), and therefore, pay inflation represents a material cost pressure that the NHS needs to plan for and manage. Our view on affordability considers the likely NHS budget from discussions to date with DHSC and what was set out by HM Treasury in the Autumn Budget 2024. Based on this, we propose to set allocations for NHS planning on the basis of a 2.8% pay settlement. Every 0.5% increase above that costs around £700m; which is the equivalent to around 2% of elective activity (greater than 300k completed patient pathways).
Some other elements of cost increase can also be anticipated and must be planned for (for example, non-pay inflation on goods and services, and statutory requirements on NICE-recommended drugs). Thus, the decision on headline pay awards is highly material to the affordable level of growth (or indeed reduction) in NHS staffing and capacity to deliver planned activity or service improvements.
3. Workforce planning
3.1 NHS Long Term Workforce Plan
The NHS Long Term Workforce Plan, published in June 2023, sets out NHS England’s long-term projections for workforce growth based on service and clinical strategy, and financial planning for the long term. We committed to updating the plan at least every 2 years.
Following consultation and engagement on the 10-Year Health Plan, we expect some of the priorities for the NHS workforce will change. It is, however, too early to confirm exactly how this might alter the projected workforce numbers given in the first iteration of the NHS Long Term Workforce Plan, which we reference in this submission.
3.2 Productivity
The size of the NHS workforce has grown significantly in recent years. The total number of full time equivalents (FTEs) employed in NHS trusts and other core organisations grew by 4.9% on average between 2022 and 2024 (2.5% between 2020 and 2022). Within that, numbers of nurses and health visitors grew by 5.9% (3.0% between 2020 and 2022) and of staff supporting clinical staff and infrastructure staff by 4.3% (2.3% between 2020 and 2022).
Staff FTEs are a key input in estimating productivity in the NHS, as a substantial proportion of the NHS budget is spent on pay. The Office for National Statistics (ONS) bases its estimates of NHS productivity on measures of how well the NHS turns a volume of inputs (including staff) into a volume of outputs (such as procedures, consultations and attendances). It does not, however, fully capture wider benefits, such as where patients receive the same or better care in less intensive healthcare settings.
The most recent ONS data shows that after a sharp fall in 2020/21, overall productivity recovered significantly in 2021/22, though it was still 6.6% below the pre-pandemic level. Our best estimate of productivity in 2024/25 from acute sector data is that it is still lower than pre-pandemic but is recovering by between 1.6% and 2.8% a year.
Government confirmed in the Autumn Budget 2024 that the NHS has a productivity target of 2% for 2025/26. NHS England will work with systems as part of annual planning on what will be required to deliver this, which will include action to improve workforce productivity through improved retention, job planning and reducing the use of temporary staffing.
3.3 Temporary workforce solutions
Influenced by seasonal factors and broader labour market fluctuations, NHS demand may lead providers to rely on temporary staff.
In 2016, measures were introduced to curb NHS agency spending, including price caps, mandatory use of approved procurement frameworks and annual expenditure ceilings for agency staff. These measures, regularly monitored for compliance and effectiveness, aim to reduce costs and give greater assurance of quality. Performance metrics on agency usage are included in the NHS Oversight Framework, reinforcing compliance rules for NHS trusts and foundation trusts.
The measures were relaxed during the pandemic but re-established in September 2022, to control agency expenditure, including a system agency expenditure limit. Further measures to drive down the reliance on agency staff are being consulted on during Q3 2024/25.
In 2023/24, total expenditure on non-medical temporary staffing decreased by 0.94% (£63 million) compared to 2022/23, largely due to a reduction in spending on agency staff.
Non-medical agency costs made up 3.1% of the total NHS pay bill in 2023/24, down from 4% in 2022/23, representing a cost reduction of approximately £438 million (19%).
The bank staffing expenditure increased by 8.6% (from £4.4 billion to £4.7 billion) in 2023/24, and the proportion of bank staff in the overall pay bill increased by 0.3 percentage points, from 7.5% to 7.8%.
The 2024/25 priorities and operational planning guidance states that systems should reduce agency spending across the NHS to 3.2% of the total pay bill in 2024/25. The NHS Long Term Workforce Plan aims to decrease reliance on temporary staffing from 9% in 2021/22 to around 5% in 2032/33.
DHSC and NHS England’s flexible staffing strategy supports NHS providers in reducing their agency staff bills and encouraging workers back into substantive and bank roles. Trusts are encouraged to develop and improve their strategy, procurement and commercial negotiation for temporary staffing.
NHS England’s NHS Interim Management and Support (IMAS) offers NHS organisations short or medium-term interim support. The service operates on the principle of ‘by the NHS, for the NHS’. NHS IMAS manages between 120 and 140 assignments at any time, supporting organisations with interim resourcing to senior roles. Any NHS organisation in England can access support from the NHS IMAS talent pools, with no additional commission or recruitment or search fees.
4. Recruitment
In June 2024, the vacancy rate for AfC staff stood at 7.1% [equivalent to 96,000 whole time equivalent (WTE)], representing a year-on-year decrease of 1.8 percentage points (-19,000).
- London continued to have the highest vacancy rate at 9.8%, and the North East and Yorkshire region had the lowest at 5.1%.
- There were 130,488 NHS new starters and 109,820 trust new starters in the rolling 12 months up to March 2024.
- 22,358 job adverts were placed in June 2024 (TRAC recruitment system).
- 22,511 job adverts were published on NHS Jobs in June 2024, with the total number decreasing by 10% month on month and 27% year on year.
- 5,387 (23.9%) of those adverts offered flexible working opportunities, with the total doing so increasing by 0.7 percentage points month on month and decreasing by 1.8 percentage points year on year.
4.1 International recruitment
Since publication of the NHS Long Term Workforce Plan, there has been growth in domestic training for nursing, midwifery and allied health professions (AHPs) (excluding operating department practitioners, orthoptists, physiotherapists, podiatrists and speech and language therapists).
International recruitment was always intended to mitigate any potential deficit between demand and the number of domestic clinicians graduating each year, and we have significantly reduced investment in international recruitment in 2024/25 following successful growth over the last 2 to 3 years in substantive staffing.
The NHS Staff Survey 2023 shows that international staff are:
- more satisfied with opportunities to develop their careers (68.25%) than they were in 2022 (66.13%) and have higher satisfaction than staff born in this country (54.89%)
- more satisfied with opportunities for flexible working (sub-score of 6.5) than they were in 2022 (6.2) and have higher satisfaction than domestically trained staff (6.34)
- more satisfied with pay (22.81%) than they were in 2022 (16.66%) but are still less satisfied with pay than staff born in this country (31.8%)
4.2 Newly qualified registrants
There has been a noticeable decline in the number of newly qualified workers (nursing, midwifery and AHPs) entering the NHS workforce. However, tracking this accurately is challenging due to the absence of a unique identifier linking students to workforce members, meaning reliance on assumptions based on course starters, completions and new workforce joiners. Further work to improve tracking is needed.
Reducing pre-registration nursing attrition remains an important focus, and NHS England is developing a long-term strategy to increase applications.
5. Retention
The leaver rate for most AfC staff groups has decreased month on month since its peak of 9.2% in April 2022, with rates now stabilising at pre-pandemic levels. The rate in June 2024 was 7.1%, representing a fall equivalent to 19,302 fewer FTE staff leaving in the year to June 2024 compared to the year to April 2022.
5.1 People Promise Exemplars Programme
In 2021, we established the People Promise Exemplars Programme, working with 23 trusts (cohort 1) across all regions in England to support system leaders with their simultaneous implementation of a bundle of high impact actions to improve staff experience and retention. The evaluation of cohort 1 identified that, based on a difference-in-differences analysis*, 22 of the 23 exemplar trusts showed a significant decrease in their all-staff monthly leaver rate, collectively reducing this by 11.8% more than non-exemplar trusts.
In the last quarter of 2023/24, building on the outcomes from cohort 1, the People Promise Exemplar Programme included a further 116 organisations across all sectors, including primary care and ambulance services. Informed by the encouraging evidence from cohorts 1 and 2, we are exploring the development of a People Promise Accreditation Scheme to help spread best practice. This work is still in the very early stages.
*A difference-in-differences method is a quasi-experimental approach that compares the changes in outcomes over time between a group enrolled in a programme (the treatment group) and a group that is not (the comparison group).
5.2 Flexible working
In 2023, the NHS Staff Survey flexibility scores showed an overall annual improvement of 6.28 compared to 6.06 in 2021. 70.67% (66.97% in 2021) of staff felt that they could approach their line manager about flexible working.
Since 2021, the lowest-scoring question in the survey has been that relating to the organisation’s commitment to flexible working. A new national flexible working people policy framework was launched in March 2024 to help employers better support staff work/life balance. Focusing on leadership and developing a culture of flexibility will be key to driving further improvement in this area.
Also of note, Pulse Survey data shows:
- appointment of board-level flexible working champions increased from 51% to 55% between Q1 2023/24 and Q1 2024/25
- organisations with flexible working action plans increased from 28% in Q4 2023/24 to 31% in Q1 2024/25
- 63% (Q1 2024/25) of respondents reported that their health and wellbeing conversations covered flexible working (this was the first-time sufficient numbers had responded to report on this metric)
- 60.7% of respondents to the Pulse Survey in August 2024 knew where to access flexible working information (no comparator data exists)
However, the most recent Pulse Survey in August 2024 also shows some metrics declining:
- 65.2% of staff felt able to approach managers about flexible working, down from 71.2% in January 2024
- 42.8% believed their organisation champions flexible working, compared to 50.6% in January 2024
In response, we aim to target improvements in flexible working for those groups where it appears to be less embedded – doctors, ambulance, primary care and maternity service staff, ensuring alignment with Reforming Medical Education and Improving the working lives of doctors in training.
6. NHS workforce
6.1 Nursing
Nurses are the NHS’s largest staff group. Data shows the substantive nursing workforce increased by 65,339 FTE (+22.4%) between September 2019 and June 2024, the largest ever sustained growth in the NHS nursing workforce and particularly helped the acute hospital sector. This has been achieved through domestic and international recruitment. The latest Nursing & Midwifery Council (NMC) data indicates that as of March 2024 there are 132,000 registered nurses who trained outside the UK, over 90,000 of whom joined between March 2019 and March 2024. During this period, the previous government set an ambition to increase the nursing workforce by 50,000 and provided dedicated yearly funding to support this, including directly funding the international recruitment of nurses.
Over the same period, the monthly use of temporary nursing workforce increased by around 3,800 FTE (+10.8%), which is attributed to an increase in monthly bank nurse use (+c6,800 FTE).
The UCAS deadline for applications was in June 2024. As of Day 28 after A-level results day, 18,420 applicants had been accepted on nursing courses with providers in England. While this number is 2.4% down on that in 2023 (-450), 14.3% down on 2022 (-3,070) and 21.6% down on 2021 (-5,070), it is 2.6% up on that in 2019 (+470). This downturn will impact not just the NHS but all sectors that require a nursing workforce.
The reported number of advanced nursing practitioner (ANP) roles continues to increase, reflecting robust workforce expansion and demand for these roles. Currently 8,046 FTE ANPs work in the NHS, which is 1,463 FTE more than last year.
The number of substantive nursing vacancies decreased by 11,057 FTE between September 2019 and June 2024, to 31,049 FTE, and as a result, the nursing vacancy rate has decreased from 12.5% to 7.9%. However, there is variation in the vacancy rate between the nursing branches: for example, mental health nursing has the highest vacancy rate at 16.1% and acute nursing has the lowest at 6.2%.
Training and education
Nursing associates
NHS England is expanding access to the nursing profession through the nursing associates apprenticeship programme. As of March 2024, NMC data shows that the number of registered nursing associates is 10,816, representing a 16.5% rise from the previous year. About 6,000 of them are employed by the NHS.
Graduate nursing
UCAS data for 2024 shows 33,560 applications to nursing courses with providers in England. While this is 6% up on 2019, it is an 8% decrease from 2023, and there has been a gradual decline since the peak in 2021.
As mentioned above, the number of students accepting offers onto undergraduate nursing courses has also reduced this year: 18,420 in 2024 compared to 18,870 at the same point in 2023 and 23,490 at the peak in 2021.
The continued decline of applications and acceptances onto nursing programmes risks workforce supply challenges, including greater reliance on the temporary workforce and international recruitment.
6.2 Midwifery
The 2024/25 priorities and operational planning guidance set the objective to increase fill rates against funded establishment for maternity staff, and trusts are responding.
As of June 2024, the total number of midwives in substantive employment is 23,562 FTE, a record number for this point in the year. Investment at national and trust level has facilitated growth in the establishments of midwives, maternity support workers and obstetricians. Trusts have funded 1,500 FTE midwifery posts that are additional to the 1,200 FTE funded by NHS England in 2021.
Since 2021, NHS England has invested an additional £185 million of recurrent funding in maternity and neonatal care, mostly on workforce.
There are currently (June 2024) a reported 1,842 FTE midwifery vacancies, a decrease of 1,407 FTE from the peak of 3,432 FTE in August 2022. This decrease has largely been driven by recent investments to increase midwifery posts following the Ockenden review recommendations. Between June 2023 and June 2024, the substantive midwifery employed workforce increased by 1,414 FTE (+6.4%).
Leaver rates (midwives leaving the profession) have reduced to 4.6% as of June 2024, from their peak of 7.3% in August 2022. This improved position has been supported with a range of national programmes and interventions, including investment for trusts to employ retention leads in each maternity unit.
Training and education
Recent and ongoing inquiries into maternity services appear to have damaged perceptions of the service, reducing its attractiveness to potential new joiners. In 2024, UCAS reported receiving 7,290 applications to midwifery undergraduate courses in England, a number that continues the decline since the peak in 2021 of 10,170. The number of students accepting offers onto undergraduate midwifery courses has also reduced this year, with 3,290 now confirmed compared to 3,360 at the same point in 2023 and 3,670 at the peak in 2021.
The continued decline of applications and acceptances onto midwifery programmes risks workforce supply challenges, including greater reliance on the temporary workforce and international recruitment.
6.3 Allied health professions
Several interventions have been designed to attract and keep the AHP workforce the NHS needs, including those outlined in:
Addressing the NHS AHP workforce supply gap is challenging because of the compound impact of the reduction in people applying for and qualifying from AHP courses, student attrition and poor translation of those qualifying and registering with the Health and Care Professions Council (HCPS) AHPs into NHS jobs (as opposed to private practice). Half or more of the profession for podiatry, physiotherapy, occupational therapy and prosthetists and orthotists is now outside the NHS.
Vacancy rates for many AHPs remain high in the NHS, particularly at early-stage career. Across the professions, the FTE vacancy rate for AHPs was 8.9% in June 2024, compared to 11.2% in June 2023, but with rates fluctuating rather than steadily declining over the year (ranging between 8.8% and 11.2%).
The wider ambulance workforce has grown steadily, increasing from 38,033 FTE staff in April 2019 to 46,991 FTE staff in June 2024 – a 23.7% rise. From June 2023 to June 2024, qualified ambulance staff numbers grew by 7.5%, from 18,734 to 20,141, and support staff by 4.9%, from 25,587 to 26,850, an overall workforce expansion of 6%.
From June 2023 to June 2024, the paramedic workforce vacancy rate decreased from 6.8% to 5.7%, and FTE vacancies reduced from 1,407 to 1,288.
Training and education
Overall, university applications to AHP courses have declined 4.4% from 2022 to 2024, with the greatest falls for paramedic (26%), prosthetics and orthotics (25%) and osteopathy (19%) courses and the largest increases for diagnostic radiography (20%) and therapeutic radiography (43%) courses. University AHP course acceptances have increased 13% between 2022 and 2024, but with reductions for operating department practice (-15%), osteopathy (12%) and podiatry (-11%) courses. AHP student attrition remained high at 11.5% in 2023/24 but was down from 14.7% in 2022/23.
To support ongoing education and training reforms for the ambulance sector, NHS England aims to enhance experiences in academic and clinical training, expand placement capacity and reduce training attrition. Funding will be provided for 2-year MSc paramedic programmes, allowing students to become registered clinicians faster.
6.4 Healthcare scientists
Healthcare scientists are highly skilled professionals capable of bridging workforce demand gaps when supported by structured training, education and clear career pathways. This potential is evident in consultant clinical scientist roles, particularly in shortage areas such as histopathology, microbiology and neurophysiology; though pay parity remains an issue.
They perform crucial, high-risk interventions adhering to stringent standards to prevent patient harm. Over 55,000 healthcare scientists work in the NHS across 50 plus specialisms, representing around 3.5% of the NHS workforce. Most are in lower bands, with 73% at Band 6 or below, and 93% are employed in acute and specialist trusts.
Healthcare scientists are employed by a range of agencies, industries and academic institutions, necessitating competitive offers from the NHS to attract and retain talent.
29% of healthcare scientists are Health and Care Professions Council (HCPC) regulated, though only clinical scientists and biomedical scientists can register with this body. Graduates can voluntarily register with the Academy of Healthcare Scientists (AHCS) or the Register of Clinical Technologists, but both have low uptake among some groups.
Training and education
The healthcare science professions have several entry levels, including healthcare science assistant and associate roles. These roles support diagnostic work and enhance skill mix to allow healthcare scientists to work at the top of their scope of practice.
The educational routes to become a healthcare scientist are the undergraduate healthcare science practitioner (PTP) degree initiated in 2011 and degree apprenticeships, started in 2019. Postgraduate options include the Scientist Training Programme (STP) initiated in 2011, with 1,024 starting PTP/STP in 2023/2024, and the Echocardiography Training Programme, begun in 2020, with 140 trainees in 2024.
The professional doctorate Higher Specialist Scientist Training Programme (HSST), begun in 2014, has 420 trainees in 2024, and leads to AHCS registration at the consultant scientist grade. PTP, STP, and HSST cover fields like audiology, cardiac science, medical physics, and genomics, created from the Modernising Scientific Careers review. There is a need for pre-undergraduate entry pathways for flexible profession access.
Following recommendations from the Richards report – Diagnostics: recovery and renewal, healthcare science assistant and associate roles have grown through apprenticeships, with degree apprenticeships increasing from 44 in 2017/2018 to 185 in 2022/2023 (National School of Healthcare Science). Recruitment into PTP degrees can be increased by providing equal access to learning support funds for healthcare science undergraduates.
Healthcare science students face disadvantages compared to other professions. Biomedical science students do not currently attract employer placement tariffs, and some healthcare scientists are ineligible for international recruitment visas, despite NHS demand.
6.5 Medical associate professions
Medical associate professions (MAPs) include physician associates (PAs) and anaesthesia associates (AAs). These roles increase team capacity and reduce the overall workload pressure on doctors. From December 2024, the General Medical Council (GMC) will begin to regulate PAs and AAs.
PAs work as part of a multidisciplinary team and perform clinical duties, such as medical history taking, examinations and managing illnesses, under the supervision of a named senior doctor. AAs work in hospitals as part of the anaesthesia team, delivering pre and post-operative care and providing anaesthesia during surgery under the direction and supervision of a consultant anaesthetist.
Currently, over 3,500 PAs and 150 AAs work in the NHS, providing care to patients in GP practices, hospitals and the community. The NHS Long Term Workforce Plan aims to expand these numbers, aiming to train10,000 PAs and 2,000 AAs by 2036/37.
The British Medical Association and the medical Royal Colleges have expressed concerns about the PA and AA roles, including their potential impact on training opportunities for doctors, care quality and patient safety. These have resulted in calls for a pause in recruitment, phasing out the PA role in general practice and limiting PAs and AAs scope of practice. As a result, there have been impacts on the recruitment and retention of PAs and AAs, including some education providers experiencing a lower uptake of students onto pre-registration training programmes.
On 20 November 2024, the Governance announced an independent review of physician and anaesthesia associate professions.
Education and training
PA and AA roles require a 2-year postgraduate degree following a relevant undergraduate degree. NHS England commissions PA and AA education and training based on a national funding model, including preceptorship allowances paid to employers to support the supervision and educational needs of qualified PAs in primary care. Through our national MAPs programme, NHS England works with its partners to develop and shape the post-registration education, training and careers for the MAP roles.
6.6 Pharmacy technicians
NHS England launched a community expansion programme in 2024, aiming to deliver an additional 530 training places per year in community pharmacy settings. This is in addition to the annual training programme commission, which offered around 826 training places in 2024/25. Pharmacy technicians can now supply medicines and services through patient group directions, supported by legislative changes to optimise skills and technology use across NHS teams.
Education and training
The NHS Long Term Workforce Plan aims to increase pharmacist training places (‘MPharm’ undergraduate degree Year 1 starters) by nearly 50% to around 5,000 by 2031/32, starting with a 15% expansion in 2026/27 and a 29% expansion to achieve 4,300 additional places by 2028/29. Reforms to pharmacist and technician education focus on creating a skilled workforce to ease pressures and improve patient care.
Pharmacist initial education and training (IET) includes a 4-year masters-level undergraduate degree, followed by a 1-year foundation training programme. Reforms will introduce independent prescriber training and multi-sector rotations. By 2026/27, all newly qualified pharmacists will be independent prescribers, enhancing clinical services across sectors. In primary care networks, pharmacists and technicians will work with GPs and multidisciplinary teams to provide enhanced services.
A Newly Qualified Pharmacist pathway will prepare pharmacists for cross-sector roles, supported by advanced practice development. In October 2024, NHS England launched a community apprenticeship programme for pre-registration trainee pharmacy technicians to complete their full 24-month apprenticeship training within a community pharmacy setting.
For the existing pharmacist workforce, 3,000 independent prescriber training places will be commissioned annually from 2025, enhancing services in community pharmacy, primary care, and secondary care. In hospital pharmacies, specialist clinical and technical roles will focus on high-quality medicines optimisation.
As set out in the NHS People Plan, 50 training places per year are being offered to community-based specialist mental health pharmacists – initially to pharmacists in community mental health services. Future cohorts may include other pharmacy staff.
6.7 Estates and facilities
The NHS estates and facilities workforce accounts for over 6% of the total NHS workforce, with around 94,000 directly employed staff. Around 65% (about 61,500) are employed at pay Bands 1 and 2. The workforce includes hard facilities management (15%), soft facilities management (77%) and leadership and support roles (7%).
The Estates and Facilities Workforce Action Plan highlights the significant challenges facing the NHS from an ageing workforce and limited recruitment of younger employees. Currently, 42% of staff are 55 or older, compared to 21% in the wider NHS workforce. Only 4% are under 25, compared to 6% across the NHS.
Vacancy rates vary from 3% to 22%, depending on role. Despite improvements in the Estates Returns Information Collection, the accuracy of vacancy data is variable. NHS Jobs data shows recruitment difficulties, with a re-advertisement rate of 57.6% for estates and facilities management roles, compared to a national average of 34%. Recruitment and attraction challenges are most acute at Bands 2 to 4, which represent 81% of estates and facilities roles, compared to 33% for other staff groups.
Private sector salaries for technical roles are between 35% and 53% higher than in the NHS. This differential exacerbates the challenges the NHS faces in ensuring it has the staff it needs to run the NHS estate and tackle crumbling infrastructure. Numbers in FTE skilled crafts and engineering roles are falling, and the maintenance backlog is growing; as cited in Lord Darzi’s review, this impacts safety.
Numbers of building crafts people decreased by 12% (321 to 283 FTE) and electricians by 16% (505 to 423 FTE) between April 2019 and June 2024. Chef numbers are similarly affected; private sector salaries are 14.2% higher than those for equivalent roles in the NHS, and the leaver rates for chefs is 8.7% above the national NHS average.
The first Skills England report from the Department for Education, Driving growth and widening opportunities, indicates there will be significant growth in engineering by 2035, intensifying the competition the NHS faces in attracting these skills. The Joint Industry Board identifies that a qualified electrician earns 33.5% more (£19.41 an hour) than an NHS electrician at Band 5 trained to the same industry standard.
Some organisations use local Recruitment and Retention Premia (RRP) to attract and retain technically skilled staff, but this solution remains localised.
6.8 Digital, data and technology (DDaT)
Technology, automation and artificial intelligence (AI) are integral to NHS processes, necessitating a robust digital and data workforce. The NHS has to compete with almost every other sector for these much needed skills. The 2024 Digital Maturity Assessment (DMA) survey found that over 70% of providers struggle to recruit for many digital and data profession roles.
The AnalystX Observatory State of the Nation Workforce survey key findings, published in October 2022, found that NHS data professionals typically stay in post for 2 to 4 years. Over half of data and analytics teams had vacancies, particularly at Bands 6 and 7, with most Band 7 gaps in national organisations. Recruitment challenges affected both rural and urban settings.
Government aims to boost productivity in the NHS by leveraging technology. Research indicates that 70% of complex, large-scale change programmes and digital transformations fall short of stated goals. 63% of the reason digital initiatives fail is due to cultural and skills deficit issues.
The 2024 DMA identified that the most difficult roles to recruit and retain are technical/ architecture (79% for ICSs and 68% for NHS providers), cybersecurity (78% and 67%), and data and analytics (73% and 78%). The current vacancy rate for digital and data posts is 7% or 2,721 positions, with 42% of these vacant for over 6 months.
7. Workforce education and training
7.1 National education and training (NETS) survey
The National Education and Training Survey (NETS) survey provides a unique, multiprofessional insight into the experience of the current and future workforce training and working in health and care services across the country. In 2023, nearly 40,000 health and care trainees, students and doctors and dentists in training responded to the survey.
NETS data from 2021 to 2023 shows a positive upward trend in the quality of learning experience in many key indicators, including:
- overall educational experience 85.30% (84.19% in 2021)
- overall quality of supervision 88.13% (87.48% in 2021)
- inductions 85.15% (83.12% in 2021)
- range of learning opportunities 85.78% (83.88% in 2021)
- ability to learn from other professions 87.83% (86.70% in 2021)
- access to health and wellbeing resources 75.23% (72.11% in 2022)
However, they also describe our learners experiencing high levels of stress, burnout and feeling overwhelmed. Furthermore, in 2023 and for the second year in a row, a third of learners had considered leaving their training programme, citing stress, workload and being overwhelmed. We continue to work in partnership with education and training providers to improve the learner experience.
Considerable improvement is also seen in learners reporting the balance between the workload and their learning is about right – 57.33% in 2023 compared to 53.26% in 2022 and 53.65% in 2021, while 42.67% stated their workload is either too busy or too quiet for them to get the learning opportunities they need.
We have seen considerable improvement in learners reporting they are aware of who their local Freedom to Speak Up Guardian is – 70.07% in 2023 compared to 65.02% in 2022 and 50.39% in 2021. 94.51% of learners also report knowing how to raise concerns, and 81.83% feel comfortable doing so.
75% of learners in 2023 would recommend their placement area to friends and colleagues as a place to work or train, a level that surpasses that pre-pandemic (74% in 2019), and 77% would recommend it to family and friends for care or treatment.
7.2 Apprenticeships
Apprenticeship data shows that the NHS continues to be the largest public sector employer of apprentices, though starts were fewer in 2023/24 compared to 2022/23, in line with decreases across most of the public sector.
Since implementation of the apprenticeship reforms and inception of the levy in 2016, there over 131,000 people have started apprenticeships in the NHS. The most popular are nursing associate, registered nurse degree and senior healthcare support worker.
Higher and degree-level apprenticeships for staff continue to increase, with 66% of apprenticeships in the 2022/23 academic year at level 4 or above compared to 27% in 2017/18. This supports the effort to widen participation by giving more colleagues access to degree-level education.
Nearly a quarter of all degree apprenticeship starts in 2022/23 in England were clinical degree apprenticeships. Growth in clinical apprenticeships at level 5 and above is a key part of the clinical expansion trajectories in the NHS Long Term Workforce Plan – 16% of registered clinical staff training on apprenticeships and 20% of registered nurses qualifying on the Registered Nurse Degree Apprenticeship by 2028/29.
Evidence is emerging from the early adopters of degree apprenticeships, such as Mid and South Essex NHS Foundation Trust and University Hospital Southampton NHS Foundation Trust, that on-programme attrition is very low. It is 4% compared to almost 100% for those taking a postgraduate route into employment, and retention (post-qualifying) is high through the apprenticeship route, as evidenced in this nurse degree case study.
8. Motivation
8.1 NHS Staff Survey
The NHS Staff Survey is one of the world’s largest staff surveys with 707,460 responses in 2023, around 87% of which are from AfC staff. The closing date for the 2024 NHS Staff Survey is 29 November 2024. We will share the analysis as early as we can following publication of the 2024 NHS Staff Survey (anticipated March 2025).
Changes to the 2023 questionnaire were minimal, which means most of the 2023 results can be compared to previous years. The new questions in the 2023 survey covered:
- unwanted behaviour of a sexual nature in the workplace
- accessibility to food while working
- home working
NHS Staff Survey data can be interrogated in detail against the demographics using the new interactive dashboard. NHS Staff Survey Promise element/theme scores by benchmarking group can be found in the data pack.
Trends in engagement
The staff engagement metric in the survey correlates strongly with wider patient and organisational outcomes such as patient satisfaction and productivity. Between 2019 and 2023, the staff engagement scores and related metrics have fluctuated:
- the engagement score was 7.04 in 2019, 7.02 in 2020, 6.84 in 2021, 6.79 in 2022 and 6.89 in 2023
- the motivation sub-score was 7.31 in 2019, 6.96 in 2021 and 7.02 in 2023
- the involvement sub-score was 6.81 in 2019, 6.74 in 2021 and 6.85 in 2023, which is above the pre-pandemic level
- the advocacy sub-score – the pride our NHS people have for their organisation and service provision – was 7.02 in 2019, 7.16 in 2020, 6.66 in 2022 and 6.81 in 2023
In the 2023 results, 5 of the 7 People Promise elements showed notable improvements and 2 remained similar to 2022 levels. The 2 themes (engagement and morale) at a national average level remained consistent. 46 of 209 trusts improved (by at least 0.10) in all 7 People Promise elements and the staff engagement and morale themes. Additionally, 128 trusts improved across all elements and themes. No NHS trust experienced a decline in all 9 themes between 2022 and 2023, and none saw a decline in the ‘We are safe and healthy’ score.
Ambulance trusts and acute and community trusts continue to score below the NHS average.
Trends in satisfaction with pay
Nationally, the People Promise element ‘We are recognised and rewarded’ score increased from 5.89 in 2022 to 6.02 in 2023. This was driven by the 5.6 percentage points rise in the percentage of staff satisfied with their level of pay to 31.2%, but this percentage remains below that pre-pandemic (36.73% in 2019).
Similarly, the percentage of staff feeling that their work is recognised, valued and appreciated improved from 52.85% in 2022 to 55.14% in 2023. All AfC occupation groups saw an increase in pay satisfaction in 2023, but the percentage of staff who are “very satisfied” or “satisfied” with their pay remains lower than that recorded in 2019/20 and nursing and healthcare assistants and ambulance staff remain the least satisfied. The percentages by staff group* who are “very satisfied” or “satisfied” with their pay are:
- allied health professionals/healthcare scientists/scientific and technical (32.96%)
- admin and clerical (28.91%)
- registered nurse and midwife (27.67%)
- ambulance (operational) (23.62%)
- nursing and healthcare assistants (19.93%)
* For other groups see NHS Staff Survey results for 2023
8.2 National Quarterly Pulse Survey
The National Quarterly Pulse Survey (NQPS) also offers a consistent and standardised approach to understanding staff experience and engagement but more frequently than the annual NHS Staff Survey. Rolled out from July 2021, the NQPS replaced the Staff Friends and Family Test and became mandatory for all NHS trusts to complete in April 2022, supporting the national employee listening strategy.
The dataset includes medical and non-medical staff, and these cannot be segregated.
Since Q4 2021/22, the NQPS has gathered over 110,000 responses in each of Q1, Q2 and Q4 (there is no NQPS in Q3 because that is when the NHS Staff Survey runs), with a peak of 128,638 responses (10% of the NHS workforce) in Q2 2024/25. This response rate helps ensure high data reliability and validity.
After declining in Q4 2023/24 (6.63) and Q1 2024/25 (6.56), the national average staff engagement theme score increased to 6.64 in Q2 2024/25, matching the Q1 2023/24 score, but still below the Q2 2023/24 peak of 6.67.
The national average staff engagement sub-scores, while previously relatively stable, have shown substantial movement in the most recent quarters. All sub-scores in Q1 2024/25 were lower than in Q4 2024/25, with the involvement and advocacy sub-scores declining most drastically. However, the reverse was true in Q2 2024/25, with all sub-scores higher than in the previous quarter, with involvement and advocacy sub-scores increasing most drastically.
NHS England research suggests that among the sub-themes, involvement is most strongly linked to staff retention, and research by Ipsos Karian and Box (unpublished) indicates that the advocacy sub-theme has the greatest impact on patient experience. The NHS trusts with higher advocacy scores showed improved patient ratings in areas such as bed waiting times, knowing whom to contact and access to hospital food.
8.3 Staff experience
The national listening tools provide a consistent and standardised way to understand, measure and improve staff experience in the NHS in line with the People Promise, as well as staff engagement and morale.
Freedom to Speak Up
In 2023/24, the national Freedom to Speak Up (FTSU) team supported 440 people to speak up about the organisations they worked or trained in, doubling the number they supported over the previous year, and 27 people received support from the National Speak Up Support Scheme. The FTSU team continues to work with and contribute to NHS England’s NHS Patient Safety Strategy.
Results of the 2023 NHS Staff Survey show that:
- Nationally, feeling safe about speaking up in organisations remained the same as in the previous 3 years – around 62%. However, there were some slight improvements across acute, acute and community, mental health and learning disabilities, mental health and learning disabilities and community sectors, with the biggest improvement observed in ambulance services (+3 percentage points).
- Confidence that organisations would take action to address any concerns, should they be raised, rose by 1.51% to 50.72% across all organisation types on average; with the most notable increase among ambulance trusts (+3.72%).
- The percentage of colleagues who feel secure raising concerns about unsafe clinical practice declined to 71.62% from 72.15% in 2022, with the percentage only increasing in ambulance trusts.
- Confidence that organisations would take action to address concerns about unsafe clinical practice remained relatively static at national level (57.62%). There was improvement among ambulance trusts from 48.37% in 2022 to 50.10% in 2023.
- The percentage of colleagues who believe their organisation treats staff who are involved in incidents fairly rose by around 1% across all organisation types apart from acute specialist trusts.
Health and wellbeing
The 2023 NHS Staff Survey identifies that perceptions around health and wellbeing are more positive.
- The overall ‘We are safe and healthy’ score increased by 0.2 between 2022 and 2023, but this is likely due to moving out of the pandemic.
- Perceived presenteeism (55.6%), experiences of burnout (30.38%), stress (41.71%) and musculoskeletal (MSK) issues (28.69%) remained high but did decline slightly.
- These health and wellbeing indicators vary between professional groups, with ambulance and registered nurses continuing to report the highest perceived levels of stress.
The spring months of 2024 showed a slight increase in sickness absence rates compared to the previous year – before falling to 4.9% in June 2024, but this is still higher than the rate before the pandemic (4.4% in June 2019). Outside seasonal variations, mental health (27.2%) and MSK issues (13.3%) continue to be prominent reasons for sickness.
The Growing occupational health and wellbeing together strategy continues to drive our national strategic direction for action. Key achievements over the past year can be found in the annual look back, look forward report.
Work continues to support local implementation of health and health and wellbeing guardians, champions and conversations; leaders to create needs-driven strategy using the NHS health and wellbeing framework; and managers and their teams to create local health and wellbeing cultures.
However, NHS staff access to health and wellbeing support continues to be inconsistent, as identified in recent work by NHS England as part of the internally commissioned Staff Treatment Access Review (2024). Inconsistent and unsustainable funding was identified as the main reason for this, with much of the available support relying on non-recurring programme or charitable funds. Smaller healthcare organisations, including general practices, are least likely to have any provision beyond statutory minimum requirements to fulfil Health and Safety requirements due to their size.
Menopause Improvement Programme
NHS England established the National Menopause Improvement Programme to ensure employees receive the necessary support at work. To help NHS organisations retain their dedicated staff experiencing symptoms of perimenopause or menopause, a comprehensive workforce support model has been developed and includes a range of interventions. It is underpinned by the Wellbeing of Women Menopause Workplace Pledge, which NHS England has signed.
Violence prevention and reduction
The 2023 NHS Staff Survey results identified that:
- 73% of staff experienced physical violence from patients or the public in the last 12 months
- 44% faced harassment, bullying or abuse from patients, service users or their relatives
- 41% of pharmacists experienced verbal abuse and 7% faced physical abuse (Pharmacist Support and Royal Pharmaceutical Society, 2023)
Work-related violence includes abuse, threats and physical attacks (Health and Safety Executive). The International Labour Organisation’s Violence and Harassment Convention mandates a violence-free work environment. The economic costs of workplace violence include lost earnings, mental distress and healthcare expenditure, with significant long-term impacts, particularly on female victims.
The NHS Violence Reduction Programme and the NHS Violence Prevention and Reduction Standard support NHS organisations in risk assessment, prevention and response to workplace violence.
NHS England’s Violence Prevention and Reduction (VPR) programme for 2024/25 has 4 key deliverables (not yet published):
- updated Violence Prevention and Reduction Standard
- cost of violence calculator and report
- evaluation of body-worn cameras pilot
Culture transformation
Developing high-quality care depends on creating positive, inclusive work environments where people want to come to work. Within NHS England, the national Civility and Respect Programme supports and promotes cultures of civility and respect in the NHS, creating positive working environments that are kind, compassionate and inclusive for all.
The Culture and Leadership Programme has 6 key lines of enquiry that analyse culture in the context of the strong evidence for the need to improve organisational culture in the NHS.
The 2023 NHS Staff Survey results for staff experience are encouraging:
- the ‘compassionate culture’ sub-score improved to 7.11 in 2023, following a decline to 6.99 in 2022 from 7.12 in 2021
- the ‘compassionate leadership’ sub-score improved between 2022 and 2023, a trend seen across all trust types, but notably in ambulance trusts – up from 6.17 in 2021 to 6.57
Leadership
There are several training programmes for improving leadership skills: Edward Jenner, Mary Seacole, Rosalind Franklin, Elizabeth Garrett Anderson and the Healthcare Leadership Model 360 Degree Feedback Tool.
From February 2025, NHS England in collaboration with Henley Business School will launch the first Future Leadership Apprenticeship Diploma in Equality, Diversity and Inclusion. Informed by the Kark and Messenger reviews, NHS England’s ambition is to include manager standards across the entire employee lifecycle for managers and leaders in the NHS, including those who are on AfC. We will collaborate with the NHS Staff Council to identify how best to achieve this.
8.4 Equality, diversity and inclusion improvement plan
The NHS equality, diversity and inclusion improvement plan (EDI IP), published June 2023, aims to attract new talent, enhance staff experience and retain staff to help deliver the NHS Long Term Workforce Plan, the People Promise and the People Plan.
NHS England has worked with ambulance trusts to implement a bespoke EDI plan following a culture review of ambulance trusts (February 2024). We have undertaken similar work for primary care, and supported Skills for Care with its wider EDI and social care Workforce Race Equality Standard (WRES) programme.
We established a national collaborative of integrated care boards (ICBs) and a regional EDI leads forum to support NHS organisations implementing the high impact actions, and a national EDI repository to share good practice and promote an improvement approach.
Delivery of the EDI IP and its 6 high impact actions has been mandated in England through the NHS Standard Contract. The NHS WRES for 2023 showed that:
- Bullying and harassment: Black and minority ethnic (BME) staff are more likely to have experienced harassment, bullying or abuse from staff in the last 12 months, or to have entered a formal disciplinary process, compared to white staff. The gap between BME staff and white staff is only narrowing marginally.
- Career progression:7% of BME staff believed their trust provides equal opportunities for career progression or promotion across all grades, compared to 59.4% of white staff. This is a smaller percentage of BME staff than in 2022, and the gap between BME staff and white staff is not narrowing. However, BME representation in AfC pay Bands 8C to very senior manager (VSM) has seen improvement, from 8.8% in March 2020 to 13.0% in March 2024.
Over the last 5 years, the UK gender pay gap has narrowed by a fifth, from 17.8% in 2018 to 14.3% in 2023, and this narrowing is seen across all health and social care roles. A King’s Fund report highlights the progress made in closing the gender pay gap. In 2023, male workers were paid 10.2% more than their female counterparts across all healthcare professions.
Both race and disability pay gap reporting lack sufficient robust data, which we will be addressing with urgency in light of proposed future legislative changes.
9. Agenda for Change contract and pension reform
The 2023 AfC pay deal includes 10 non-pay commitments overseen by a programme board co-chaired by DHSC and the NHS Staff Council. The last AfC update was published in November 2024.
9.1 Job evaluation
NHS England is working closely with NHS Employers to identify how we best support leaders to ensure they understand the importance of implementing job evaluation correctly, as well as the staff engagement and financial risks of flawed implementation.
In September 2024, NHS Employers published further job evaluation guidance, including training opportunities. Further detail about work to support the NHS to implement local job evaluation processes can be found in the written evidence from NHS Employers.
9.2 NHS Pension Scheme reform
The new flexible retirement options were introduced to encourage staff to prolong their working lives. For example, retire and re-join (effective from 1 April 2023) is particularly attractive to staff with the special right to take their pension unreduced from age 55 (nurses, midwives, physiotherapists and health visitors); and partial retirement (effective from 1 October 2023) allows staff to take up to 100% of their pension and carry on working, without taking a break in their employment. At the time of writing, the NHS Business Services Authority report that since 1 October 2023 18,881 NHS staff have taken partial retirement.
More than £13 billion of employer and employee contributions is invested in the scheme every year, but widespread ignorance and misunderstanding about its value remain. The scheme is an important lever for attracting, retaining and encouraging staff to return to the NHS.
NHS England’s Pension Response Project, developed in 2021, supports leaders to influence behaviour change. By demonstrating the financial benefits of the scheme to staff and their loved ones, it seeks to persuade staff who would otherwise retire earlier than planned or who plan to retire when they reach their normal pension age (60, 65 or older) to work longer or return to the NHS after retiring.
Since 2021, working with our pension partners, we have led virtual staff pension seminars and master classes for line managers to explain the pension basics, flexible retirement opportunities and implications for those still affected by pensions tax. We have reached over 27,800 staff. Though this is a modest number, qualitative data (staff feedback following virtual pension seminars) suggests staff appreciate and value the opportunity to ask questions and clarify their understanding.
At the March 2023 Budget, the previous government reduced the tax disincentive for 10s of 1000s of NHS staff by increasing the annual allowance from £40,000 to £60,000 and abolishing the lifetime allowance.
However, although far fewer NHS staff are affected by pension tax, for some, opting out of the NHS Pension Scheme because of the continuing impact of pensions tax may be a sound financial decision. In March 2023, NHS Employers published pension tax guidance to support trusts to explore options for retaining staff still affected by pensions tax.
In August 2023, NHS England wrote to trusts about the flexibility they have to develop local NHS Pension Scheme employer contributions recycling schemes; some have already introduced such schemes. The decision to offer recycling schemes is for trusts to make and should focus on securing best value for money and delivering the best possible outcomes for patients.
We will continue to work closely with NHS Employers and DHSC over the remainder of 2024/25 to identify and agree interventions that highlight the value of flexible retirement and other pension-related options for staff in late-stage career. We want to retain the experienced and skilled staff the NHS needs to support recovery and their less experienced colleagues.
10. Annex
10.1 Determining leavers from NHS secondary care
Leaver rate methodologies comparison
Summary
This document details the methodology behind the NHS England/Long-Term Workforce Plan (LTWP) leaver rate definitions and how they compare against other leaver rates already in the public domain.
Data source
The Electronic Staff Record (ESR) is a HR and payroll system in place in all NHS secondary care providers in England, as well as some other healthcare organisations. Data from ESR is used to support the delivery of national workforce policy and strategy, including monitoring of staff retention. Primary and social care organisations do not always use a unified payroll system such as ESR, so we are not currently able to derive information in the same way, although there is a dedicated data collection for the GP workforce.
Information is inputted at source by employees, managers, HR departments, etc. in organisations registered on ESR. This information is pulled monthly from ESR records to the ESR data warehouse owned by the NHS Business Services Authority (BSA). Data services teams at NHS England pull the data from the ESR data warehouse into NHS England internal data servers. Identifiable record-level information is pseudonymised which is then loaded into NHS England data warehouse where it can be directly queried by those with access rights. Leaver data is extracted from NHS England data warehouses using SQL scripts.
Identifying leavers
To identify who has left the secondary care workforce over a period of time, a snapshot of staff in post active on ESR is taken at timepoint 1 and compared to a snapshot of staff in post at timepoint 2 (see Figure 1). If an individual is active on ESR at timepoint 1 but does not appear at timepoint 2, they are assumed to have left the NHS secondary care workforce and their full time equivalent (FTE) is counted toward the overall leaver FTE for that period. We use annual leaver FTE, therefore timepoint 2 is one year after timepoint 1.
This method has limitations, for example if someone leaves and returns again between timepoint 1 and 2, they are not captured. Furthermore, if someone moves to primary or social care but does not leave the NHS, they may be counted as a leaver if they no longer have an active ESR record.
Figure 1. Examples of how individual staff movements would be classed when determining annual leavers using LTWP method.

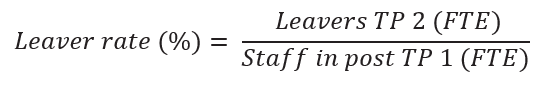
Leaver rate
Leaver FTE at timepoint 2 is identified using the method described above and illustrated in Figure 1. Leaver rate is calculated by dividing leavers at the end of the time period (TP2) by the staff in post at the start of the time period (TP1).
Differences between NHS England/LTWP methods and published Official Statistics.
There are other published official statistics about the NHS workforce derived from ESR which include information about leavers, joiners and movers in the NHS. These employ different methods to the NHS England/LTWP-aligned figures. Differences in methods include the calculation itself, as well as inclusion and exclusion criteria regarding which types of staff should be factored in those calculations. Table 1 outlines difference between the two methods.
Table 1. Comparison of criteria in NHS England/LTWP and Official Statistics leaver methodology.
| Criteria | NHS England/LTWP Methodology | Official Statistics Methodology |
| Contract Type | Includes staff with permanent, fixed term and locum contract types only (bank and agency staff are excluded). | Includes staff with permanent and fixed term contract types only (bank and agency staff are excluded). |
| Contracted FTE | No criteria applied based on contracted hours. However, staff without any contracted hours would not be included in FTE figures. | Staff with zero contracted hours excluded. |
| Organisation Type | Records from all organisations on ESR are included. Thisincludes small numbers of staff in non-NHS organisations (e.g. independent healthcare providers). | Only includes NHS Organisations, termed Core (e.g. Trusts) and Wider (e.g. Arms Length Bodies). |
| Multiple Assignments | Where someone has multiple roles within the NHS at the same time, total FTE is summed across records. | Same methodology employed. |
| Inactive status (including staff on maternity leave) | Movement from a substantive role to inactive status (including maternity leave, career breaks and secondments) is not counted as a leaver. | Movement from a substantive role to inactive status is counted as a leaver. Employee is deemed not part of the ‘active’ workforce. |
| Payment received in period | Individuals are counted in staff in post and leaver FTE whether they have received any payment or not. | Staff must have recorded earnings on ESR in month to be included in all official statistics publications. |
| Change in hours | If an individual decreases their FTE, this is not counted towards leavers. | Where FTE is used as the measure, this is counted towards leavers. |
| Leaver rate calculation | Leavers TP2 (FTP) Staff in post TP1 (FTP) TP = timepoint | Leavers TP2 (FTP) (Staff in post TP1 + TP2) / 2 FTE Note the use of a different denominator between calculations |
| Unit of measurement | FTE only – the number of hours worked, indicative of capacity | Headcount (individual members of staff) and FTE |
| Backdating/retrospective revisions | ESR records relating to specific time periods can be updated/revised at a later point. This method takes snapshots of ESR records at the point of receiving the data from the data warehouse. We do not back-date any records, therefore such historical revisions would not be reflected in the data. | Same method employed – no retrospective revisions. |
The differences between methodologies means the derived leaver rate differs between the two datasets. Official statistics tend to state the national all staff leaver rate as 3 to 3.5 percentage points higher at any one time, as there are more cases in which someone is considered a leaver. However, trends in rates between the two datasets are the same.
Reasons for differences
The official statistics and NHS England/LTWP leaver figures have different purposes. The NHS England/LTWP leaver rate is used for workforce planning, therefore it considers all staff who are available to work, not just those in active service (as in the Official Statistics method). Staff on career breaks, or maternity leave, cannot be legally replaced on a permanent basis therefore they must be included when making planning decisions or judgements. Therefore, only counting active service staff (those in receipt of pay) risks underestimating the workforce capacity.
Publication reference: PRN01676