1. Evidence summary
The NHS remains under enormous pressure.
Our healthcare service continues to recover from the COVID-19 pandemic as well as the industrial action that saw 1.3 million appointments postponed. Despite this, there has been solid progress across several areas.
In September 2024, 73.0% of patients waited under 4 hours in A&E departments, an improvement on the 70.3% who did in October 2023. Furthermore, the number of patients waiting for an elective procedure has fallen from 7.77 million in September 2023 to 7.57 million in September 2024.
Public sentiment has also improved. 73.9% of patients reported a good or very good experience of their GP practice compared to 71.3% in 2023.
Overall, the NHS is providing more care contacts in 2024 across secondary care services, mental health and community health services than in 2023.
Despite these improvements, Lord Darzi’s recent Independent Investigation of the National Health Service in England highlights that the NHS in England still has a lot further to go in addressing access issues, the mixed quality of care (in particular from maternity and mental health services), and the need to shift resource allocation from hospital to community. The impact of COVID-19 led to significant backlogs in operations, exacerbating pre-existing challenges the NHS was facing.
Workforce issues have posed long-term challenges for the NHS – too few staff have resulted in burnout and a demoralised workforce which further exasperate recruitment challenges.
Perceptions of health and wellbeing among staff have slightly improved, though burnout, stress and musculoskeletal (MSK) issues persist. Sickness absence for hospital and community health service doctors continues to rise and is now higher than before the pandemic (1.8% in May 2024 and 1.3% in 2019). In June 2024, the most common reason for sickness absence among doctors was a common mental health condition (including anxiety, stress and depression). Staff survey and sickness absence data is not available for GPs, but other surveys show their morale is lower and workplace experiences poorer than other doctors.
We have worked to spread best practice on retention. In 2023/24 the People Promise Exemplar Programme was expanded to 116 more organisations, focusing on enhancing staff retention through improvement cycles and targeted equality, diversity and inclusion interventions.
We have recruited more staff. The NHS has increased the number of hospital and community health service medical staff by 25.8% (28,886 FTE) over the last 5 years, with successful international recruitment playing a significant role. The NHS Long Term Workforce Plan seeks to put the workforce on a more sustainable footing by reducing reliance on the overseas workforce from 25% now, to 9% to 10.5% over the next 15 years.
The most recent NHS Staff Survey satisfaction score for ‘We are recognised and rewarded’ (in 2023) reflects the period of industrial action during which the survey was conducted. Following the resolution of recent pay disputes affecting hospital and community health service doctors and dentists, as well as ongoing non-pay initiatives with the British Medical Association (BMA), we hope to see improvements in the 2024 NHS Staff Survey results. There is a continuing contractual dispute affecting the GP workforce.
Control measures to curb NHS agency spending continue to support the reduction of agency costs, which made up 5.5% of the medical pay bill in 2023/24, down from 6.2% in 2022/23.
Going into next year, NHS funding will be extremely tight, and it will constitute a year of significant consolidation.
The NHS revenue settlement is likely to grow by 2% in real terms from which all pressures must be met including unavoidable elements like non-pay inflation, new medicines and treatments approved by the National Institute for Health and Care Excellence (NICE) and a series of other pressures, as well as pay settlements.
In that context, the NHS will not be able to make material investments in new services and meet all its pressures from the uplift available, including the usual growth in capacity that is necessary to meet demand growth. It is possible that some services will see real terms cuts in funding and activity after allowing for the pay settlement, depending on its scale.
NHS staff work incredibly hard. We want to see them fairly rewarded, in a way that strikes the right balance on resources so that they have the ability to deliver the care they want to for patients. Our view on affordability considers the likely NHS budget from discussions to date with the Department of Health and Social Care (DHSC) and what was set out by HM Treasury in the Autumn Budget 2024. Based on this, we propose to set allocations for NHS planning on the basis of a 2.8% pay settlement. Every 0.5% increase above that costs around £700 million; which is the equivalent to around 2% of elective activity (greater than 300,000 completed patient pathways).
We have already made significant prioritisation decisions. Pay awards above what has already been allocated will require further tough re-prioritisation of the decisions already made, significantly impacting patient care and in turn making the day-to-day job of NHS staff even harder.
2. NHS finances
2.1 Financial context
The indicative NHS England budget confirmed with DHSC for 2024/25 is currently £186.6 billion, including education funding and the cost of the former NHS Digital. This budget also includes additional funding from the government to meet the unplanned costs of industrial action and some of the cost of the higher than planned pay award and pay reform deals, and for additional elective activity above the core funded level. The budget is likely to change as we confirm further transfers of funding within the DHSC group before the end of the financial year.
Plans to deliver within the available budget have required significant efficiency from local systems and providers, partly a deliberate decision to require higher efficiency post pandemic (SR21 set a target of at least 2.2%), and partly the result of higher than planned and funded inflation over the last few years and in 2024/25. The efficiency requirement identified in 2024/25 system plans is £9.3 billion (equivalent to 6.9% of their total allocation), which compares to £7.2 billion (5.4% of allocations) of efficiencies delivered in 2023/24. While systems are likely to deliver more efficiencies in 2024/25 compared to 2023/24, there is a risk they may not deliver these planned efficiencies. Several systems set financial plans based on a deficit, and this has required NHS England to identify cuts in frontline service investment to set a balanced overall plan.
We are confirming with Government how to implement the DHSC 2025/26 resource settlement as part of the planning process, at which point we will be able to confirm the NHSE allocation for the next financial year.
The NHS needs to plan for and manage the impact of Pay Review Body recommendations on headline pay increases. The Spending Review set out the government’s expectation that additional in-year resource will not be provided for pay awards in 2025/26. We have already made significant prioritisation decisions. Pay awards above what has already been allocated will require further tough re-prioritisation of the decisions already made.
2.2 Financial support for education and training
The Education and training tariff guidance 2024 to 2025 confirms uplifts to tariff prices and postgraduate medical salary support arrangements for 2024/25. The revised prices are inclusive of the approved 2024/25 pay awards and apply to all activity undertaken from 1 April 2024. The uplifts include an increase to the study leave funding available for postgraduate doctors in training, as that is top sliced from the postgraduate medical tariff. There are no significant policy changes to tariff arrangements being introduced in 2024/25.
2.3 Affordability
Pay remains the largest component of NHS costs (around 65% of total operating costs), and therefore, pay inflation represents a material cost pressure that the NHS needs to plan for and manage. Our view on affordability considers the likely NHS budget from discussions to date with DHSC and what was set out by HM Treasury in the Autumn Budget 2024. Based on this, we propose to set allocations for NHS planning on the basis of a 2.8% pay settlement. Every 0.5% increase above that costs around £700 million; which is the equivalent to around 2% of elective activity (greater than 300,000 completed patient pathways).
Some other elements of cost increase can also be anticipated and must be planned for (for example, non-pay inflation on goods and services, and statutory requirements on NICE-recommended drugs). Thus, the decision on headline pay awards is highly material to the affordable level of growth (or indeed reduction) in NHS staffing and capacity to deliver planned activity or service improvements.
3. Workforce planning
3.1 NHS Long Term Workforce Plan
The NHS Long Term Workforce Plan, published in June 2023, sets out NHS England’s long-term projections for workforce growth based on service and clinical strategy, and financial planning for the long term. We committed to updating the plan at least every 2 years.
Following consultation and engagement on the 10-Year Health Plan, we expect some of the priorities for the NHS workforce will change. It is, however, too early to confirm exactly how this might alter the projected workforce numbers given in the first iteration of the NHS Long Term Workforce Plan, which we reference in this submission. We will update the Review Body on Doctors’ and Dentists’ Remuneration (DDRB) as soon as we can.
3.2 Productivity
The size of the NHS workforce has grown significantly in recent years. The total number of full time equivalents (FTEs) employed in NHS trusts and other core organisations grew by 4.9% on average between 2022 and 2024 (2.5% between 2020 and 2022). The number of doctors grew by 5.1% (2.8%).
Staff FTEs are a key input in estimating productivity in the NHS, as a substantial proportion of the NHS budget is spent on pay. The Office for National Statistics (ONS) bases its estimates of NHS productivity on measures of how well the NHS turns a volume of inputs (including staff) into a volume of outputs (such as procedures, consultations and attendances). It does not, however, fully capture wider benefits, such as where patients receive the same or better care in less intensive healthcare settings.
The most recent ONS data shows that after a sharp fall in 2020/21, overall productivity recovered significantly in 2021/22, though it was still 6.6% below the pre-pandemic level. Our best estimate of productivity in 2024/25 from acute sector data is that it is still lower than pre-pandemic but is recovering by between 1.6% and 2.8% a year.
Government confirmed in the Autumn Budget 2024 that the NHS has a productivity target of 2% for 2025/26. NHS England will work with systems as part of annual planning on what will be required to deliver this, which will include action to improve workforce productivity through improved retention, job planning and reducing the use of temporary staffing.
3.3 NHS equality, diversity and inclusion improvement plan
The NHS equality, diversity and inclusion improvement plan (EDI IP), published June 2023, aims to attract new talent, enhance staff experience and retain staff to help deliver the NHS Long Term Workforce Plan, the People Promise and the People Plan.
NHS England is currently engaging with clinical and non-clinical staff across the 4 sectors of primary care (general practice, dentistry, pharmacy and optometry) on an EDI Improvement Plan for primary care.
We established a national collaborative of integrated care boards (ICBs) and a regional EDI leads forum to support NHS organisations implementing the high impact actions, and a national EDI repository to share good practice and promote an improvement approach.
Delivery of the EDI IP and its 6 high impact actions has been mandated in England through the NHS Standard Contract. The NHS Workforce Race Equality Standard (WRES) for 2023 showed that:
- Bullying and harassment: Black and minority ethnic (BME) staff are more likely to have experienced harassment, bullying or abuse from staff in the last 12 months, or to have entered a formal disciplinary process, compared to white staff. The gap between BME staff and white staff is only narrowing marginally.
- Career progression: 46.7% of BME staff believed their trust provides equal opportunities for career progression or promotion across all grades, compared to 59.4% of white staff. This is a smaller percentage of BME staff than in 2022, and the gap between BME staff and white staff is not narrowing. However, BME representation in Agenda for Change (AfC) pay Bands 8C to very senior manager (VSM) has seen improvement, from 8.8% in March 2020 to 13.0% in March 2024.
Over the last 5 years, the UK gender pay gap has narrowed by a fifth, from 17.8% in 2018 to 14.3% in 2023, and this narrowing is seen across all health and social care roles. Doctors’ pay has shown the greatest shift: from 20.9% in 2018 to 5.5% in 2023.
Both race and disability pay gap reporting lack sufficient robust data, which we will be addressing with urgency in light of proposed future legislative changes.
DHSC published the Independent Review into Gender Pay Gaps in Medicine in England in December 2020. NHS England is a named delivery partner for 9 of its recommendations. A key area of activity is promoting opportunities to work more flexibly and encouraging take up of these opportunities by both men and women.
NHS England plans to build on its commitment to address the gender pay gap by asking all lead employers of postgraduate doctors in training to report annually on ethnicity and gender pay gaps.
In support of the Messenger Review, NHS England has:
- been working with Henley Business School to launch the first Future Leadership Apprenticeship Diploma in EDI in February 2025
- worked with NHS boards to use the EDI dashboard on the Model Health System to support their strategic decision making and EDI improvements
- continued to work with healthcare training and education providers using the quality framework to ensure parity of access to learning opportunities for all learners
- updated the Educator Workforce Strategy to ensure that those educating our future workforce understand how EDI issues can impact the learning experience
4. International recruitment
The State of Medical Education and Practice in the UK Workforce Report (2023) says that doctors from overseas will continue to make up a large proportion of those joining the medical register, with over half (52%) of new additions in 2022 being international medical graduates (IMGs). The General Medical Council (GMC) forecasts that, while the supply of UK graduates will increase over the next decade, IMGs will still account for a substantial proportion (32%) of the workforce in 2036. It is therefore essential that the NHS can recruit, integrate, and retain doctors from a range of backgrounds.
The path for IMGs to obtain medical employment in this country can be difficult, and they often report a poorer workplace experience than those with a UK primary medical qualification (PMQ). We continue to work to improve the induction and onboarding of IMGs and to improve their experiences at work.
The NHS is enormously grateful for the contribution of its internationally trained staff. However, it is not sustainable to continue recruiting staff from overseas at the level the NHS has been in recent years. Global workforce supply can be fragile. Pandemics, armed conflict, and climate change all pose risks to staff supply, and the international labour market is likely to become increasingly competitive as healthcare systems around the world face increasing demand.
Consultants
We currently rely on IMGs to fill the shortfall in domestic supply, using both the postgraduate training and specialty and specialist (SAS) doctor routes. While UK medical student places are growing, it will take at least 10 years for this to translate into more senior doctors. Recent data from the GMC shows a 2% increase in UK-trained medical graduates joining the workforce since 2017, compared to a 121% rise in IMGs.
SAS and LEDs
An increasing number of IMGs are joining the workforce as SAS and locally employed doctors (LEDs). The majority join without any speciality qualifications being recognised on entry. GMC data indicates that 71% of LEDs are trained internationally and that the retention of IMGs in LED roles is improving. The proportion of this group who were no longer licensed after 4 years fell from 37% of the 2014 cohort to 20% of the 2018 cohort. The proportion entering postgraduate training within 4 years of being licensed almost doubled between 2014 and 2018. 22% of the 2014 cohort were in postgraduate training 3 years after joining, compared to 41% of the 2018 cohort.
GPs
The proportion of doctors joining the GP register in England who are European Economic Area (EEA) graduates more than doubled (+121%) between 2013 and 2024. The larger IMG component almost tripled (+162%) between 2013 to 2024, while doctors with a UK PMQ increased slightly (+15%) over the same period.
The number of entrants to the GP register has grown from 2,230 in 2013 to 3,434 in 2024. This growth is mainly due to doctors with a non-UK PMQ: from 620 in 2013 to 1,589 in 2024. The current number of GP registrants with a non-UK PMQ is 46% in 2024 and is expected to exceed 50% of new supply within the next 2 years. Our analysis indicates regional variations in the number of entrants to the GMC register, with the Midlands recording around two thirds of new GP supply with a non-UK PMQ in 2024, compared to only 14% in London.
While the GP International Induction Programme continues to offer a supported pathway for overseas qualified GPs to be inducted safely into general practice, GP headcount growth is largely due to IMGs completing their GP speciality training (GPST) in the UK, rather than joining from abroad with recognised GP qualifications.
In their 2024 report, the DDRB requested information on retention rates for international GP recruits, both qualified GPs joining from overseas and IMGs joining GP training. GP register data shows that around 90% of GPs have a licence to practise 10 years after initial registration. British nationals with a UK PMQ have the highest retention rates among nationality and ‘routes to register’ groups. The rate of GP registrant retention is lower among non-UK PMQs than UK PMQs (81% 11 years after registration, compared to 91% for UK PMQs). Among non-UK PMQs, initial registrant attrition is highest in the early years post GP registration. Those with EU/EEA PMQs have the highest level of register attrition. Of doctors on the GP register or specialist register who are over 50, smaller proportions of IMGs left for retirement compared with their UK graduate peers, although it is not possible to fully understand the scale of the problem due to data challenges.
GP and specialty training
In the recruitment round for the 2022/23 academic year, 42% of all doctors at core training/specialty training 1 (CT/ST1), 60% of GPs, and 51% of core psychiatry doctors in postgraduate training had a non-UK PMQ. This includes a small but growing number who were UK citizens undertaking medical degrees abroad.
IMGs make up an increasing proportion of the future GP workforce due to ongoing expansion to GPST. As the number and proportion of IMGs in GPST continues to grow, the number of extensions required will increase if we do not provide additional support. The number of UK PMQ graduates choosing GPST as their first or subsequent preference has remained largely unchanged.
NHS England has allocated additional resources to support IMGs to complete their GP and specialty training on time and to a high standard. Regions are providing IMG GP doctors in postgraduate training with a range of support, including enhanced induction, social integration, language skills and exam preparation. IMGs due to complete GPST are supported in finding practices with visa sponsorship licences, enabling them to continue to live and work in England when they qualify as a GP.
5. Temporary workforce solutions
Influenced by seasonal factors and broader labour market fluctuations, NHS demand may lead providers to rely on temporary staff.
In 2016, measures were introduced to curb NHS agency spending, including price caps, mandatory use of approved procurement frameworks and annual expenditure ceilings for agency staff. These measures, regularly monitored for compliance and effectiveness, aim to reduce costs and give greater assurance of quality. Performance metrics on agency usage are included in the NHS Oversight Framework, reinforcing compliance rules for NHS trusts and foundation trusts.
The measures were relaxed during the pandemic but re-established in September 2022, to control agency expenditure, including a system agency expenditure limit. Further measures to drive down the reliance on agency staff are being consulted on during Q3 2024/25.
In 2023/24, total expenditure on medical temporary staffing increased by 18% (£470 million) compared to 2022/23, largely due to an increase in spending on bank staff.
Bank staffing costs increased by 34% (from £1.4 billion to £1.9 billion) in 2023/24, and bank staff as a proportion of the overall medical pay bill increased by 1.5 percentage points, from 7.8% to 9.3%.
Agency costs made up 5.5% of the medical NHS pay bill in 2023/24, down from 6.2% in 2022/23, representing a cost reduction of approximately £12 million (1.1%).
While the BMA withdrew its rate card guidance as part of the recent medical pay deals, the NHS is left grappling with bank and agency locum rates that are significantly out of line with substantive pay rates.
DHSC and NHS England’s flexible staffing strategy supports NHS providers in reducing their agency staff bills and encouraging workers back into substantive and bank roles. Trusts are encouraged to develop and improve their strategy, procurement and commercial negotiation for temporary staffing.
6. Motivation and morale
6.1 National listening tools
The national listening tools provide a consistent and standardised way to understand, measure and improve staff experience in the NHS in line with the People Promise, as well as staff engagement and morale. These tools do not currently extend to primary care.
6.2 Staff survey
The NHS Staff Survey is one of the world’s largest staff surveys with 707,460 responses in 2023, and 45,502 of these were from the medical and dental occupational group. The breakdown of responses for this group was:
- Medical or dental – consultant: 27,311 responses
- Medical or dental – in postgraduate training: 8,237 responses
- Medical or dental – SAS doctors: 5,030 responses
- Medical or dental – other: 4,450 responses
- Medical or dental – salaried primary care dentists: 474 responses
The closing date for the 2024 NHS Staff Survey is 29 November 2024. We will share the analysis as early as we can following publication of the 2024 NHS Staff Survey (anticipated March 2025).
Changes to the 2023 questionnaire were minimal, which means most of the 2023 results can be compared to previous years. The new questions in the 2023 survey covered:
- unwanted behaviour of a sexual nature in the workplace
- accessibility to food while working
- home working
- NHS Staff Survey data can be interrogated in detail against the demographics using the new interactive dashboard. NHS Staff Survey Promise element/theme scores by benchmarking group can be found in the data pack.
Trends in engagement
The staff engagement metric in the survey correlates strongly with wider patient and organisational outcomes such as patient satisfaction and productivity. Between 2019 and 2023, the staff engagement scores and related metrics have fluctuated:
- the engagement score was 7.04 in 2019, 7.02 in 2020, 6.84 in 2021, 6.79 in 2022 and 6.89 in 2023
- the motivation sub-score was 7.31 in 2019, 6.96 in 2021 and 7.02 in 2023
- the involvement sub-score was 6.81 in 2019, 6.74 in 2021 and 6.85 in 2023, which is above the pre-pandemic level
- the advocacy sub-score – the pride our NHS people have for their organisation and service provision – was 7.02 in 2019, 7.16 in 2020, 6.66 in 2022 and 6.81 in 2023
For the medical and dental occupation group, the overall staff engagement theme score increased from 2022 to 2023 (+0.06). All sub-theme scores for this occupation group also increased.
In the 2023 results, 5 of the 7 People Promise elements showed notable improvements and 2 remained similar to 2022 levels. The 2 themes (engagement and morale) at a national average level remained consistent. 46 of 209 trusts improved (by at least 0.10) in all 7 People Promise elements and the staff engagement and morale themes. Additionally, 128 trusts improved across all elements and themes. No NHS trust experienced a decline in all 9 themes between 2022 and 2023, and none saw a decline in the ‘We are safe and healthy’ score.
For the medical and dental occupation group, there was no decline for 5 of the People Promise elements: ‘We are compassionate and inclusive’ (+0.03), ‘We are safe and healthy’ (+0.14), ‘We are always learning’ (+0.15), ‘We work flexibly’ (+0.13), ‘We are recognised and rewarded’ (0.00) and ‘We are a team’ (+0.15). The ‘We each have a voice that counts’ element declined marginally from 2022 (-0.02). This decline appears to be driven by a steady decline against the ‘Raising concerns’ element.
Ambulance trusts, acute and acute and community trusts continue to score below the NHS average.
Trends in satisfaction with pay
Nationally, the People Promise element ‘We are recognised and rewarded’ score increased from 5.89 in 2022 to 6.02 in 2023. This was driven by the 5.6 percentage points rise in the percentage of staff satisfied with their level of pay to 31.2%, but this percentage remains below that pre-pandemic (36.73% in 2019). The percentage of staff feeling that their work is recognised, valued and appreciated improved from 52.85% in 2022 to 55.14% in 2023.
There has been no change for the medical and dental occupation group against the ‘We are recognised and rewarded’ element since 2022 and satisfaction with pay has decreased to 32.05% from 36.6% in 2022. The decline in satisfaction with pay is unique to the medical and dental occupation group and was not seen amongst other occupation groups.
6.3 General Practice Staff Survey
In 2023, the NHS Staff Survey was extended to general practice on a voluntary basis. The General Practice Staff Survey (GPSS) supports a ‘one workforce’ approach and aims to give a voice to staff working in general practice organisations. For the first time, it will provide standardised, comparable and actionable data on staff experience, benefiting individual practices, primary care networks (PCNs), and integrated care systems (ICSs). This data will help guide efforts to enhance recruitment and retention and mitigate the prevalence of burnout.
The introduction of the GPSS is a critical step toward implementing the WRES and the Workforce Disability Equality Standard (WDES) in primary care settings. National, ICB and PCN footprint reports include results against the survey questions, benchmarked against averages, as well as 4 of the 9 WRES and 5 of the 9 WDES indicators.
In 2023, 21 ICBs participated in the 1st year of the GPSS, and 45% of practices in those systems shared staff lists. This created a survey sample of more than 1,500 organisations and 45,000 individuals, 40% of whom responded to the request to share their views. We expect the sample size and response rate to grow. 34 ICBs have committed to supporting the survey in 2024.
Results for the GPSS are not publicly available. However, the move to a nationally provided survey for general practice is a positive shift. We know that listening to employee voices is a key enabler of employee engagement (MacLeod and Clarke, 2009).
6.4 National Quarterly Pulse Survey
The National Quarterly Pulse Survey (NQPS) also offers a consistent and standardised approach to understanding staff experience and engagement but more frequently than the annual NHS Staff Survey. Rolled out from July 2021, the NQPS replaced the Staff Friends and Family Test and became mandatory for all NHS trusts to complete in April 2022, supporting the national employee listening strategy.
The dataset includes medical and non-medical staff, and these cannot be segregated.
Since Q4 2021/22, the NQPS has gathered over 110,000 responses in each of Q1, Q2 and Q4 (there is no NQPS in Q3 because that is when the NHS Staff Survey runs), with a peak of 128,638 responses (10% of the NHS workforce) in Q2 2024/25. This response rate helps ensure high data reliability and validity.
After declining in Q4 2023/24 (6.63) and Q1 2024/25 (6.56), the national average staff engagement theme score increased to 6.64 in Q2 2024/25, matching the Q1 2023/24 score, but still below the Q2 2023/24 peak of 6.67.
The national average staff engagement sub-scores, while previously relatively stable, have shown substantial movement in the most recent quarters. All sub-scores in Q1 2024/25 were lower than in Q4 2024/25, with the involvement and advocacy sub-scores declining most drastically. However, the reverse was true in Q2 2024/25, with all sub-scores higher than in the previous quarter, with involvement and advocacy sub-scores increasing most drastically.
NHS England research suggests that among the sub-themes, involvement is most strongly linked to staff retention, and research by Ipsos Karian and Box (unpublished) indicates that the advocacy sub-theme has the greatest impact on patient experience. The NHS trusts with higher advocacy scores showed improved patient ratings in areas such as bed waiting times, knowing whom to contact and access to hospital food.
7. Staff experience
Freedom to Speak Up
In 2023/24, the national Freedom to Speak Up (FTSU) team supported 440 people to speak up about the organisations they worked or trained in, doubling the number they supported over the previous year, and 27 people received support from the National Speak Up Support Scheme. The FTSU team continues to work with and contribute to NHS England’s NHS Patient Safety Strategy.
Results of the 2023 NHS Staff Survey show that:
- Nationally, feeling safe about speaking up in organisations remained the same as in the previous 3 years – around 62%. However, there were some slight improvements across acute, acute and community, mental health and learning disabilities, mental health and learning disabilities and community sectors, with the biggest improvement observed in ambulance services (+3 percentage points).
- Confidence that organisations would take action to address any concerns, should they be raised, rose by 1.51% to 50.72% across all organisation types on average; with the most notable increase among ambulance trusts (+3.72%).
- The percentage of colleagues who feel secure raising concerns about unsafe clinical practice declined to 71.62% from 72.15% in 2022, with the percentage only increasing in ambulance trusts.
- Confidence that organisations would take action to address concerns about unsafe clinical practice remained relatively static at national level (57.62%). There was improvement among ambulance trusts from 48.37% in 2022 to 50.10% in 2023.
- The percentage of colleagues who believe their organisation treats staff who are involved in incidents fairly rose by around 1% across all organisation types apart from acute specialist trusts.
Health and wellbeing
The 2023 NHS Staff Survey reported greater positivity among staff in NHS trusts about health and wellbeing.
The overall ‘We are safe and healthy’ score increased by 0.14 between 2022 and 2023. A range of measures reflecting staff-reported issues with staff wellbeing and health remained high but declined slightly over the period:
- perceived presenteeism: 43.7%
- experiences of burnout: 32.4%
- stress: 43.5%
- MSK issues: 33.0%
Variation exists between professional groups. NHS Staff Survey results indicate that 44.7% of consultants (a decline of 0.5 percentage points compared to 2022) and 38.7% of doctors in postgraduate training (a decline of 1 percentage point compared to 2022) agreed that their organisation takes positive action on health and wellbeing. Consultants in the ambulance sector and doctors in postgraduate training in the acute sector reported the highest perceived levels of stress compared to their peers.
Sickness absence datasets for hospital and community health service doctors identify that sickness continues to rise and is higher now (1.8% May 2024) than before the pandemic (1.3% May 2019). The most common reason for sickness absence for doctors in June 2024 was a common mental health condition (including anxiety, stress, depression and other psychiatric illnesses).
Staff survey and sickness absence data is not available for GPs, but separate surveys show low morale and poor workplace experiences compared to other doctors. The GMC’s annual State of Medical Education and Practice in the UK report has found that GPs consistently have worse experiences than other groups of doctors. The most recent report found that in 2023, GPs were the register type with the highest proportion of doctors who were struggling (48% compared with 33% of all doctors) and, overall, only 14% of all GPs were ‘doing well’ compared with 27% of all doctors. Only 42% of GPs were satisfied in their work, compared with 53% of all doctors. Similarly, the Royal College of General Practitioners’ GP Voice Survey 2024 found that 60% of GPs surveyed reported their mental health had declined while working as a GP over the past 12 months, and over 40% of GPs felt so stressed they couldn’t cope at least once a week.
The Growing occupational health and wellbeing together strategy continues to drive our national strategic direction for action. Key achievements over the past year can be found in the annual look back, look forward report.
In line with the NHS England Operating Framework, the national Health and Wellbeing Programme is moving from delivering direct support nationally to equipping ICSs and employing organisations to better support staff through a preventative and responsive approach. However, support for doctors, dentists, and anyone who cannot access confidential care locally, continues nationally through the NHS Practitioner Health Service. As of September 2024, GPs make up 41% of the caseload, other doctor groups represent 52%, and other workforce groups represent 7%. Common mental health conditions are the dominant reason for practitioners accessing the service (84% of current caseload). Anxiety continues to be the thing that troubles practitioners the most, followed by work pressures and then low mood or depression.
Work continues to support local implementation of health and health and wellbeing guardians, champions and conversations; leaders to create needs-driven strategy using the NHS health and wellbeing framework; and managers and their teams to create local health and wellbeing cultures.
However, NHS staff access to health and wellbeing support continues to be inconsistent, as identified in recent work by NHS England as part of the internally commissioned Staff Treatment Access Review (2024). Inconsistent and unsustainable funding was identified as the main reason for this, with much of the available support relying on non-recurring programme or charitable funds. Smaller healthcare organisations, including general practices, are least likely to have any provision beyond statutory minimum requirements to fulfil Health and Safety requirements due to their size.
Menopause Improvement Programme
NHS England established the National Menopause Improvement Programme to ensure employees receive the necessary support at work. To help NHS organisations retain their dedicated staff experiencing symptoms of perimenopause or menopause, a comprehensive workforce support model has been developed and includes a range of interventions. It is underpinned by the Wellbeing of Women Menopause Workplace Pledge, which NHS England has signed.
Violence prevention and reduction
The 2023 NHS Staff Survey identified that:
- 11.6% of medical staff experienced physical violence from patients or the public in the last 12 months
- 33.0% faced harassment, bullying or abuse from patients, service users or their relatives in the last 12 months
- acute and acute and community trusts scored below average on the ‘We are safe and healthy’ metric
Work-related violence includes abuse, threats and physical attacks (Health and Safety Executive). The International Labour Organisation’s Violence and Harassment Convention mandates a violence-free work environment. The economic costs of workplace violence include lost earnings, mental distress and healthcare expenditure, with significant long-term impacts, particularly on female victims.
The NHS Violence Reduction Programme and the NHS Violence Prevention and Reduction Standard support NHS organisations in risk assessment, prevention and response to workplace violence.
NHS England’s Violence Prevention and Reduction (VPR) programme for 2024/25 has 4 key deliverables (not yet published), including:
- updated Violence Prevention and Reduction Standard
- cost of violence calculator and report
- evaluation of body-worn cameras pilot
Culture transformation
Developing high-quality care depends on creating positive, inclusive work environments where people want to come to work. Within NHS England, the national Civility and Respect Programme supports and promotes cultures of civility and respect in the NHS, creating positive working environments that are kind, compassionate and inclusive for all.
The Culture and Leadership Programme has 6 key lines of enquiry that analyse culture in the context of the strong evidence for the need to improve organisational culture in the NHS.
The 2023 NHS Staff Survey results for staff experience are encouraging:
- the ‘compassionate culture’ sub-score improved to 7.11 in 2023, following a decline to 6.99 in 2022 from 7.12 in 2021
- the ‘compassionate leadership’ sub-score improved between 2022 and 2023, a trend seen across all trust types, but notably in ambulance trusts – up from 6.17 in 2021 to 6.57
Flexible working
Flexible working gives individuals greater choice of when, where, and how they work and can support a better work-life balance. This includes flexibility in working patterns, hours, location and job design.
Flexible working is integral to the NHS’s role as an anchor institution, allowing the NHS to support individuals with caring and broader social responsibilities and to offer employment opportunities to a wider section of the community. Improving opportunities for staff to work more flexibly supports recruitment and retention and is a key factor in improving staff experience.
NHS England’s flexible working programme focuses on education and the promotion of best practice and supports staff employed under both Agenda for Change and medical and dental contracts.
Specific initiatives to improve flexible working for doctors include work undertaken as part of NHS England’s Postgraduate Medical Education Reform and Improving Working Lives programmes to improve flexibility in training pathways and rota management and increase the use of self-rostering. (This is discussed further in the doctors in postgraduate training section of our evidence).
8. Retention
The leaver rate for medical and dental staff has been declining, dropping from a peak of 10.7% in August 2022 to 10% in June 2024. The consultant leaver rate fell from 4.0% in April 2019 to 3.5% in June 2024, with a peak of 4.5% in April 2022. Similarly, the leaver rate for fully qualified GPs decreased from a peak of 8.9% in June 2022 to 6.6% in June 2024.
8.1 People Promise Exemplar Programme
In 2021, we established the People Promise Exemplar Programme, working with 23 trusts (cohort 1) across all regions in England to support system leaders with their simultaneous implementation of a bundle of high impact actions to improve staff experience and retention. The evaluation of cohort 1 identified that, based on a difference-in-differences analysis*, 22 of the 23 exemplar trusts showed a significant decrease in their all-staff monthly leaver rate, collectively reducing this by 11.8% more than non-exemplar trusts.
* A difference-in-differences method is a quasi-experimental approach that compares the changes in outcomes over time between a group enrolled in a programme (the treatment group) and a group that is not (the comparison group).
In the last quarter of 2023/24, building on the outcomes from cohort 1, the People Promise Exemplar Programme included a further 116 organisations across all sectors, including primary care and ambulance services. Informed by the encouraging evidence from cohorts 1 and 2, we are exploring the development of a People Promise Accreditation Scheme to help spread best practice. This work is still in the very early stages.
8.2 GP retention
In addition to cohort 2 of the People Promise Exemplar Programme, which includes 11 primary care sites, ICBs can use primary care transformation funding to support recruitment and retention of GPs and other general practice staff.
9. Doctors in postgraduate training
Data from June 2024 shows the NHS employs approximately 1.4 million FTE staff, with approximately 141,000 FTE qualified doctors. As a group, doctors in postgraduate training range from newly qualified foundation doctors to clinicians with over a decade of experience. There are currently around 70,000 doctors in postgraduate training, accounting for approximately 50% of the medical workforce.
Doctors in postgraduate training are increasingly likely to practise medicine abroad, delay entry to specialist training, or leave the profession altogether. There is also a well known imbalance in medical distribution in the UK, with many rural and underdeveloped areas struggling to recruit and retain doctors. The desire to work more flexibly is an increasing aspiration of newer generations of trainees, and policymakers and workforce and service planners must look to develop strategies to accommodate these preferences.
9.1 National Education and Training Survey
The National Education and Training Survey (NETS) provides a unique, multiprofessional perspective on the experiences of the current and future workforce as they train and work within health and care services. Since its launch in 2019, it has offered a longitudinal view across professions, complementing the GMC’s National Training Survey.
Overall satisfaction levels for doctors in postgraduate training remain below 2019 pre-pandemic levels (workload, dissatisfaction with reward and recognition, and rota gaps may be influencing these findings), although the scores for several indicators have increased over the last 2 years:
- 72% would recommend their training environment to friends and colleagues as a place to work or train, an increase from 70% in 2022 and 69% in 2021.
- 89% reported a positive experience of supervision in training, an improvement from 85% in 2022 and 88% in 2021.
- 16% reported experiencing bullying and harassment in their training post, compared with 17% in 2022 and 15% in 2021.
- 74% confirmed they would know how to access support from their local FTSU Guardian.
In the 2023 NETS, postgraduate dentists in training have the highest scores for overall satisfaction:
- 82% would recommend their training environment to friends and colleagues as a place to work or train, compared to 79% in 2022 and 77% in 2021.
- 90% reported a positive experience of supervision in training, an improvement compared with 88% in 2022 and 2021.
- 8% reported experiencing bullying and harassment in their training post, compared with 10% in 2022 and 12% in 2021.
- 46% confirmed they would know how to access support from their local FTSU Guardian.
The NETS is a key tool to measure and understand the landscape of healthcare education and training. It is fundamental to supporting our quality management processes, helping to create a culture that is fair, promotes equality and values and facilitates learning opportunities for all.
9.2 Training experience and quality assurance
The NHS England Education Quality Strategy outlines our approach to managing and improving the quality of education and training in healthcare services across England. It is underpinned by the multi-professional Education Quality Framework, which defines the standards for delivering high-quality education and training in a safe, supportive and inclusive learning environment.
Doctors in postgraduate training rotate between different placements. Their feedback on educational experience and the nature of each workplace in terms of patient safety, interpersonal or interprofessional behaviours and culture is often an early warning sign of potential quality or safety concerns. NHS England has a pathway for learners and educators to raise and, where appropriate, escalate concerns regarding the learning environment, complemented by the NETS. We continue to work with ICSs to support quality improvement programmes, including by sharing best practice aligned to national, regional and local priorities.
9.3 The Postgraduate Medical Education Reform Programme
The Postgraduate Medical Education Reform Programme continues to work with partners to reform the medical training system to better align the medical workforce with patient and service needs, and to support the aspirations of doctors in postgraduate training. The programme covers a range of aligned initiatives, including:
- enhanced generalist skills
- providing wider flexible medical careers (further information is included in the SAS and LED sections of our evidence)
- improving the wellbeing and experience of doctors in postgraduate training through flexible training opportunities, reviewing rotations, portfolio careers, the People Promise Exemplar Programme and implementation of the NHS Staff and Learners’ Mental Wellbeing Commission (further information is included in the retention section of our evidence).
- Enhanced generalist skills
9.4 Enhanced generalist skills
The Future Doctor Report highlighted the need for more doctors and other healthcare professionals to have generalist skills. This was reinforced by what we learned from the COVID-19 pandemic. Enhancing and maintaining generalist skills will enable clinicians to be more adaptable, better able to meet patient needs, and address health inequity across populations.
The Enhancing Generalist Skills Syllabus covers 6 healthcare domains: person-centred practice, complex multi-morbidity, system working, population health, social justice and health equity, and environmental sustainability. These are supported by 4 cross-cutting themes: wellbeing, leadership, digital, and transformative reflection. A large number of healthcare workers across a broad spectrum of professions have participated in an enhance programme delivered through 7 regional trailblazers. The programme is offered to all foundation doctors in England. It helps early-stage clinicians to understand the clinical, societal and system-wide complexities of health and care services, equipping them to navigate these challenges and deliver integrated, person-centred care for everyone.
We are also expanding partnerships with ICSs to create more opportunities for all health and care staff to develop generalist skills. So far, this includes 7 ICSs. We aim to embed the programme in the wider NHS to maximise benefits for patients, teams and systems.
9.5 Flexible training opportunities
NHS England is committed to improving flexibility across training pathways, with several initiatives developed to permit a more individualised approach to training. NHS England has improved access to less than full-time training (LTFT) and other flexible approaches, including opportunities to take time out of training, flexible portfolio training, and fellowship offers.
9.6 Out of programme pause
Out of programme pause (OOPP) initiative allows doctors in postgraduate training to step away from formal training to take up an NHS or other UK-based patient-facing non-training role.
Unlike other ‘out of programme’ options, OOPP allows skills and capabilities developed by doctors during their time away to be assessed when they return to training. These may contribute to their Certificate of Completion of Training (CCT) if faculty and Annual Review of Competence (ARCP) panels agree that capabilities are demonstrated on return.
This initiative provides a flexible training option, which can support wellbeing, and it acknowledges that capabilities and experience can be gained outside of training. The GMC and the devolved nations have endorsed the integration of OOPP as a standard option for doctors in postgraduate training.
NHS England has responded to recommendations from stakeholders by removing some limitations from OOPP, including the length of time a doctor can take out of training, and these changes have been jointly approved across the devolved nations and by the GMC.
9.7 Less than full-time training
The option to train LTFT has now been fully integrated, with no specific categories for eligibility, only an indicative list. This means that all doctors in postgraduate training can apply to work LTFT. To ensure we continue to comply with the Equality Act, we still give priority to those who have a protected characteristic.
This is a major change. LTFT training was previously only available to those with caring or health needs (LTFT category 1) or those with unique opportunities for personal development (LTFT category 2). Responding to trainee perspectives, Health Education England introduced a new flexibility initiative in 2017: LTFT category 3. This allowed doctors to opt to train on a LTFT basis for an individual, professional or lifestyle need, only constrained by local service pressures.
LTFT category 3 has had an overwhelmingly positive impact on work-life balance and on the likelihood of doctors completing their training.
9.8 Flexible portfolio training
Flexible portfolio training (FPT) provides a tailored, flexible opportunity for postgraduate medical specialty trainees to dedicate 1 day per week (or 20% FTE) to professional development activities, aligned to local educational, academic and service goals.
Initially, FPT offered 4 distinct pathways, each designed to connect trainees with diverse individuals, teams and networks that might not be part of their regular clinical work. The available pathways included:
- clinical informatics
- medical education
- clinical service or quality improvement
- research
Launched as a pilot in collaboration with the Royal College of Physicians, the programme showed positive results and was expanded. As of August 2023, it is now available across all medical specialties in England.
9.9 Addressing health inequalities – distribution of training places
This programme seeks to address health inequalities by helping remote, rural and smaller health systems attract, recruit and retain trainees, consultants and GPs. It has implemented and trialled a range of methods to change the distribution of training places to meet future needs. The NHS England model prioritises 3 high-fill specialties (haematology, cardiology, and obstetrics and gynaecology) to better align with patient need. The first tranche of training posts in these 3 specialties started their first-year post movement in August 2022. 16 additional specialties started the first phase of the programme in 2023.
Any change in the distribution of specialty training posts under this programme will be implemented gradually over up to 10 years to ensure continuity of care and uphold quality and patient safety. Additional phases will be developed in parallel with future specialty training expansion.
9.10 Priority allocation in the foundation programme
In response to feedback, a new allocation model for medical graduates was introduced. This gives applicants a computer-generated ranking based on their geographic preference, removing the need to sit a situational judgment test.
The aim was to give more graduates, including overseas applicants, their first-preference location and the new allocation model has placed more applicants in their first-choice locations.
The higher proportion of first-preference placements and the more even distribution of overseas applicants has resulted in a more consistent withdrawal rate across the country and reduced vacancy hotspots in less popular regions or trusts. NHS England will continue to review and improve the allocation methodology based on the data for 2024 and 2025.
9.11 Foundation priority programmes
NHS England has maintained support for a range of foundation priority programmes in areas of England that find it difficult to attract and retain trainees through the foundation and specialty recruitment processes. To date, the following local financial incentives have been introduced and evaluated.
- The Northern Foundation School offers 85 priority programmes with a £7,500 per training year taxable incentive. These programmes also give additional educational support for all foundation year 1 and 2 doctors through the F-Docs online education package.
- To support recruitment to pathology specialties, applicants allocated to foundation programmes with a pathology specialty are invited to apply for a fellowship with the Royal College of Pathology.
9.12 Recruitment incentives – paediatric and perinatal pathology
All trainees accepting a paediatric and perinatal pathology training post in England from 2023 are eligible for a £20,000 recruitment incentive. This recognises the need to improve recruitment into the specialty and expand the paediatric and perinatal pathology workforce. To date, this incentive has not resulted in increased applications to ST3 paediatric and perinatal pathology. The reasons for this are multifaceted. They include, but are not limited to, the capacity of placements to provide training. NHS England is working with The Royal College of Pathologists to develop other initiatives to increase the attractiveness of and recruitment to the speciality.
9.13 Recruitment incentives – general practice specialty training
The General Practice Targeted Enhanced Recruitment Scheme (TERS) provided financial incentives for trainees who committed to working in parts of the UK with a history of under-recruitment or in under-doctored or deprived areas. Successful applicants who committed to training for 3 years in TERS areas were offered a one-off £20,000 salary supplement funded by NHS England. The scheme was designed to test whether additional financial incentives could improve workforce supply in areas facing the severest recruitment pressures.
TERS had some success in attracting GP trainees, but it is not clear whether it made GP training more attractive to prospective trainees or helped NHS England fill all advertised GP specialty training places. Longitudinal tracking is needed to determine whether trainees stay in areas after qualification.
9.14 General practice specialty training reform
One of the biggest challenges in meeting expansion targets is the capacity of training placements, including the limitations imposed by estates.
We need more placements to deliver the GPST reform agenda and meet current and future training targets. NHS England aims to support this by using blended learning and other reform and capacity building initiatives. These learning placements are needed to expand GPST training placements, but also to equip doctors in postgraduate training with generalist, high-quality clinical skills, along with digital, leadership and quality improvement capabilities.
A 4-month blended learning ‘proof of concept’ ran between April and August 2023 for 18 trainees in the West Midlands. This was followed by 4 pilots across different regions to evaluate effectiveness and potential benefits for learners, educators and the wider NHS. While it is too early to assess the outcomes of the pilots, initial feedback is that the blended learning placements had some positive impacts and will continue delivering benefits in the future.
9.15 Improving the working lives of doctors in postgraduate training
In April 2024, NHS England issued a letter to trusts stressing the importance of addressing issues that negatively impact the working lives of doctors in postgraduate training.
The letter was informed by extensive stakeholder engagement and research from organisations, including the Academy of Royal Medical Colleges and the BMA. In August 2024, a follow-up questionnaire was sent to all chief people officers and chief medical officers, asking for updates on key actions outlined in the letter. 95 trusts responded.
Key actions are:
Board ownership of issues: This includes having a named lead reporting to trust boards on improving working lives of doctors in postgraduate training. In the follow-up questionnaire, 93 of the 95 trusts that responded had appointed a lead. Virtually all of these were either chief people or chief medical officers. 90 trusts said they intended to have a board-level discussion about this year’s GMC/NETS survey results. Many also provided examples of the additional work they had done locally on these issues, suggesting a genuine focus on improvement.
Working with partners to improve the experience of rotations: Feedback from doctors in postgraduate training indicates the most significant issue they face is the current system of rotations, which can see them move 8 or 9 times on average during their training. This work aims to ensure that doctors receive the required training while minimising the administrative and bureaucratic hurdles involved in rotating. This includes addressing relocation, logistics, travel and accommodation issues. A key goal is to reduce disruption to personal and family life and ensure more consistent support systems across rotations and geographies. This is a major piece of work and will involve a comprehensive review of how doctors in postgraduate training are trained and employed.
Exploring expansion of the lead employer model (LEM): This work aims to assess the feasibility and cost of expanding LEM arrangements to all doctors in postgraduate training, so they are employed by a single employer throughout their training. Feedback from doctors indicates that the continued need to change employers is bureaucratic, time-consuming and doesn’t add value. Many employment frustrations described by doctors in postgraduate training would be resolved, or at least minimised, with the expansion of LEMs.
Compliance with the rota code of practice: This includes 3 elements: organisations receiving trainee grid information at 12 weeks, organisations providing work schedules at least 8 weeks in advance, and the finalisation of duty rosters 6 weeks in advance. The performance metric for the 12-week notification was 91% in July. Responses to the questionnaire sent to trusts in August indicated that 82% of trusts had provided 80% or more of their doctors in postgraduate training with work schedules within 8 weeks and 81% or more with a rota within 6 weeks of starting. Work is underway to establish formal monitoring of rota code compliance, aiming for implementation by the February 2025 rotations.
Reducing payroll errors: Payroll errors disproportionately affect doctors in postgraduate training. NHS England is providing targeted support to providers with the greatest need and has shared best practice guidance with all organisations. Intensive support will be provided to 35 organisations across all 7 regions.
Payment of course fees: Reforms to course fee payments will shift to a system where trusts pay upfront for mandatory courses, replacing the current reimbursement process for doctors.
Changes to statutory and mandatory training: This programme will standardise core training elements and, subject to risk assessment, assess opportunities to reduce the time burden on staff, including looking at renewal frequency and whether any staff groups can be excluded. This will have a disproportionately positive impact on doctors in postgraduate training, who often need to repeat statutory and mandatory training as they rotate between organisations.
10. Consultants
Consultants deliver expert care, improve patient outcomes and play a vital role in teaching and mentoring doctors and dentists in postgraduate training. They work in the largest numbers in acute hospitals, and their leadership of multidisciplinary teams is vital to the efficient and effective delivery of healthcare services.
The number of consultants has increased by 18.5% over the last 5 years. The Institute of Fiscal Studies has reported that, with more consultants across all age groups wanting to work LTFT, greater numbers are needed to achieve the required FTE level.
Medical student places are growing and NHS workforce statistics show that the overall number of doctors in the NHS is growing faster than any other staff group since 2010.
Research by the Institute of Fiscal Studies shows that while there is variation across age and gender, with female consultants under 60 being 4 times more likely to work LTFT than their male counterparts, on average a LTFT consultant will work between 6 and 7 programmed activities (PAs) per week. Data is not currently available on how consultants’ work time is balanced between PAs and supporting professional activities (SPAs), as this is agreed at an individual level, but the BMA advice recommends 2.5 SPAs in a standard 10 PA contract.
Workforce data indicates that around 1,000 consultants retire from the NHS each year, at an average age of 60, 6 years before the current state pension age. This average age has been relatively static for at least 5 years.
The NHS Emeritus pilot scheme was launched in January 2024 with the aim of connecting retired or semi-retired consultants to secondary care providers requiring specific support through a digital platform. If successful, the 12-month pilot will be expanded to include other work areas. In the first 4 months of the scheme, more than 200 consultants registered to join and were linked to 40 providers.
11. Speciality and specialist (SAS) doctors
SAS doctors include specialty doctors, associate specialists and specialist doctors. They form an important and growing part of the medical workforce. The latest GMC State of Medical Education and Practice Workforce Report says all groups on the medical register have increased since 2017, but data for England shows that growth is especially pronounced in the SAS and LED groups. If this trend continues, SAS and LEDs will form the largest part of the medical workforce by 2030.
11.1 Numbers and average working hours of SAS doctors
Data from NHS workforce statistics showed that there were 12,156 FTE (11,938 headcount) SAS doctors in June 2024.
As of August 2024, the number of specialty doctors on closed contracts versus the 2021 contracts was as follows:
- closed contracts: 3,643 FTE (4,273 headcount)
- 2021 contract: 5,847 FTE (6,326 headcount)
The total headcount of specialists has grown from 933 in August 2023 to 1,367 (1,239 FTE) by the end of August 2024.
The SAS workforce currently makes up 30% of all licensed doctors.
GMC data from 2022 showed that:
- 61% of SAS doctors worked on a permanent, full-time basis, compared with 52% of all doctors
- 15% of SAS doctors worked on a permanent, part-time basis, compared with 19% of all doctors
- 15% of SAS doctors worked on a fixed-term or temporary full-time contract, compared with 17% of all doctors
- Characteristics of SAS doctors
SAS doctors work in a variety of settings, including hospitals, community settings, and primary care. The 2022 census of physicians reported that more than two-thirds (66%) of SAS doctors are women, compared with 41% of consultants. The percentage working LTFT or flexibly is also higher: 50% for SAS doctors, compared with 28% for consultants. This could be linked to people choosing a SAS career to improve work-life balance or to accommodate caring responsibilities. In addition, 64% of SAS doctors had taken their full annual leave entitlement compared with 58% of consultants. Where SAS doctors had not used all their annual leave, they said they were either too busy or unable to find cover.
SAS doctors make a significant service contribution and enable workforce flexibility. A large proportion are doctors who trained outside the UK. According to GMC data, there are a higher proportion of IMGs working as SAS and LEDs compared to those on the specialist or GP register (54% compared to 25%). The UK’s healthcare systems benefit considerably from the experience and flexibility of both SAS and LEDs. It is therefore vital that a variety of fulfilling career paths are available to them. The GMC Workforce Report demonstrates that the increasing proportions of IMG joiners moving into postgraduate training or SAS roles has been accompanied by an improved retention rate.
11.2 SAS workplace experience
The NHS Long Term Workforce Plan commits to working with DHSC, legislators and employers to improve SAS doctors professional experiences by ensuring equitable promotion and options for career diversification.
Some SAS doctors report concerns about lack of support in the workplace. NHS England continues to explore and implement initiatives to improve their overall experience, wellbeing, access to education, training and assessment, and opportunities for career development and progression through:
- enhanced inductions, especially for IMGs, to support their integration into the NHS
- improved opportunities to work flexibility
- new professional development offers to support learning and collaboration across professions
- development of clinical leadership and educator roles to support career development through implementation of the educator supervision strategy
- exploration of new assessment routes to facilitate career progression and CCT attainment for those who wish to work at consultant level
In response to specific actions related to SAS doctors in the NHS Long Term Workforce Plan, NHS England is working with partners to deliver the SAS Excellence in Development Recognition Award. This will formally recognise trusts that are meeting specific outcomes in promoting an inclusive culture and supporting the development and retention of their SAS workforce. Due to launch in Spring 2025, this recognition award will be a valuable recruitment and retention tool for this part of the medical workforce.
The GMC SAS and LED Survey found that 22% of SAS doctors felt they were not provided with personal and professional development opportunities to advance their careers. Local employers can advertise for specialist posts via competitive entry through recruitment processes, so there is no automatic progression to specialist posts for current specialty doctors.
In collaboration with NHS Employers, NHS England and the Academy of Medical Royal Colleges, the BMA published the SAS Charter for England in 2014. The BMA have since adapted the SAS Charter for all other UK nations. The charter aims to help SAS doctors with their development by setting out the support and opportunities employers are expected to provide.
12. Locally employed doctors (LEDs)
According to GMC data, LEDs are the fastest growing part of the UK medical workforce and, in 2023, the number of LEDs was growing much faster than the number of SAS doctors.
LEDs are employed by a range of different organisation types, often on fixed-term contracts with local terms and conditions. LEDs often undertake more supportive roles, requiring direct or indirect supervision. They also have a wide range of job titles, including trust grade, foundation year 3 (F3), clinical fellow, teaching fellow or locally employed doctor. This lack of consistent naming of LEDs and the way they are coded on the electronic staff record (ESR) creates challenges locally and nationally when looking at data.
While the NHS Long Term Workforce Plan recognises the instrumental role LEDs play in delivering healthcare within the NHS, the plan also highlights the lack of data on the experience, skills, ethnic diversity and geographic distribution of LEDs. These challenges with access to data need to be addressed to better understand this diverse group’s needs, career choices and aspirations.
12.1 The shape of the LED workforce
Increasing numbers of doctors take a break from training for personal and professional reasons. Uncertainty about their training paths or a wish to gain specialty experience (the F3 phenomenon) can contribute. This affects how training is delivered and how doctors are supported and has important implications for future workforce supply. The productivity of the medical workforce depends on supporting the learning of doctors who take a break from training, allowing them to gain experience so they can provide more complex care. LEDs play an important role in service delivery and are also a potential future supply of consultants and SAS doctors, provided that appropriate support and career structures are put in place.
GMC data indicates that a significant proportion of LEDs are from BME backgrounds, the majority are aged 30-49, and over half are men, but the number of women is increasing.
12.2 NHS England LED Blueprint for Change
The NHS England LED Blueprint for Change was co-produced with LEDs and senior leaders and aligns with the pillars of the NHS Long Term Workforce Plan: train, retain and reform.
The ‘train’ pillar sets out targeted high-impact actions to address the challenges facing LEDs, including enhancing existing medical training and career pathways, so there is a wider range of more flexible opportunities available to the medical workforce from early in their careers. NHS England and our partners will ensure the LED role is supported, developed, and enabled as a viable medical career pathway.
The GMC’s Workplace Experiences Report (2024) highlights that LEDs are the group of doctors most likely to have taken concrete steps toward leaving their roles and, in comparison with other groups, fewer LEDs felt part of a supportive team. In response, the ‘retain’ pillar of the LED Blueprint for Change contains actions trusts can take to improve the experience of LEDs by improving opportunities for progression, skills development, induction and access to educational opportunities, while creating a culture that fosters inclusion and belonging.
12.3 Opportunities for the LED workforce
The LED workforce must be a key consideration in integrated workforce planning. Ensuring an adequate and balanced distribution of doctors across different specialties and regions is a significant challenge. Retention can be improved by better supporting LEDs through their careers. As many LEDs are uncertain about their career path, they require greater career-specific support. It is important to help LEDs advance in their careers by opening routes into SAS roles and into training pathways. To build and retain a highly engaged workforce, it is essential to understand what providers require from LEDs, what LEDs need from providers, and how to deliver the care patients need.
12.4 Impact of Review Body on Doctors’ and Dentists’ Remuneration recommendations
Since 2022, LEDs have been included in the DDRB’s remit, and the expectation was that employers would increase their pay in line with DDRB recommendations. In July 2024, the written ministerial statement on public sector pay did not respond to the DDRB’s recommendation on LEDs.
Where LEDs are paid according to national pay scales, they will have received an uplift alongside their counterparts on the same pay scale. However, NHS England does not have information on the consequences of the DDRB’s recommendation. Systems were funded in allocations to implement the impact of pay awards to LEDs through the cost uplift factor. FTE data published by NHS England maps LEDs to their respective pay scales (doctors in postgraduate training and SAS doctors), depending on pay reported in ESR.
13. General medical practitioners (GPs)
Government asked the DDRB to include recommendations on the minimum and maximum pay range for salaried GPs and earnings and expenses uplifts for GP partners. The pay recommendations for salaried GPs are usually also applied to all practice staff, and it is recommended that this continues. Recommendations will need to be informed by affordability and the contract resources available to practices. This information will also inform GP practice decisions about the pay of their salaried GPs and other practice staff.
Most GPs work under general medical services (GMS) contracts as independent contractors. They are self-employed or members of partnerships running their own practices as small businesses. As of 31 March 2023, there were 1,615 personal medical services (PMS) arrangements (24.2% of all contracts). Any uplifts in investment for PMS contracts are a matter for local commissioners to consider. In addition, a small number of GPs work, or hold contracts, under a locally contracted alternative provider medical services arrangement across 235 practices (NHS Payments to General Practice – NHS England Digital).
13.1 Numbers and average working hours of GPs
NHS England publishes monthly data on the size and composition of the general practice and PCN workforce, and information is therefore not replicated in this evidence.
The DDRB have said they would like a better understanding of GPs’ decisions around working hours and how this relates to pay. NHS England is not aware of any evidence on the relationship between actual working hours decisions and pay for GPs. Research (GMC’s State of Medical Education and Practice, 2024; The King’s Fund GP trainees’ survey, 2022) shows that reduced working hours is most often related to high workload, stress and low satisfaction. However, the link to renumeration is not clear.
13.2 Access to general practice services
General practice began collective action on 1 August 2024. If this action intensifies, the potential impact on the wider NHS remains uncertain. If there is no resolution to the dispute, it is still possible that collective action could escalate to industrial action in the near future, which would have larger consequences.
GP teams are delivering more appointments to patients than ever before: 30 million per month in September 2024, up 13% compared with the same period before the pandemic. Although patients still express frustration about accessing general practice services, the GP Patient Survey published in July 2024 found 89.9% of patients said their needs were met at their last appointment and 73.9% of patients had a good overall experience of their GP practice.
Work is continuing through the commitments included in the Primary Care Access Recovery Plan, particularly the implementation of the modern general practice model, to improve access to general practice. For example, most practices now have cloud-based telephony systems to improve access and patient experience and to reduce the 8am rush. Practices also have a range of online consultation, messaging and appointment booking tools available. NHS England supports practices to spread uptake and integrate these tools effectively into their workflows and processes. The modern general practice model includes gathering information from patients and improving care navigation and triage processes. This enables practices to allocate care to patients more effectively and efficiently.
There is growing evidence that new GPs are not as inclined to become partners, resulting in a drop in the number of partners annually. Latest General Practice Workforce data shows the number of partner GPs (headcount) has fallen by over 10% in the last 5 years (10.8% since September 2019), 2.3% in the last year – equating to 13.9% and 2.7% FTEs respectively. The BMA’s GP Committee England reports that this is due to a lack of funding and unsustainable working hours. Other factors include the reduction in salaried GPs appetite for:
- raising the finance required to join practice partnerships (adding to their outstanding student loans)
- managing the business activities and premises of a practice
- Morale and motivation
Information on morale of GPs is included in the motivation, morale and staff experience section of the evidence.
13.3 Recruitment and retention
General practices, as independent contractors, are responsible for recruitment decisions. However, there have been reports from the GP profession of changes to the employment market for GPs, with fewer salaried jobs and locum sessions being advertised and greater competition for those jobs.
To help resolve the immediate issue of under-employment among recently qualified GPs, additional funding of £82 million was announced to support the inclusion of recently qualified GPs in the Additional Roles Reimbursement Scheme from October 2024. Data on numbers of GPs employed by PCNs will be reported in the same way as other staff employed by practices and PCNs and included in the regular PCN workforce statistics.
To increase the supply of qualified GPs, NHS England continues to fund the GP Return to Practice Programme, which provides a route for qualified GPs to return to NHS general practice in England, and the GP International Induction Programme, which offers a supported pathway for overseas qualified GPs to be inducted safely into NHS general practice.
Information on the national retention offer is covered in the retention section of our evidence.
13.4 Joiners, leavers, turnover, and vacancies
NHS England is continually working to ensure our publications are useful and relevant. This includes work to improve the data available on the movement of GPs between roles and locations. Published data now includes:
- GP joiners and leavers – Every quarter we publish data on GP joiners, leavers and ‘movers’ alongside the usual monthly general practice workforce statistics. This includes annual counts of joiners to and leavers from the qualified GP workforce (excluding GPs in training) and qualified permanent GP workforce (excluding GPs in training and GP locums) in FTE and headcount. It also includes files presenting annual FTE and headcount joiner and leaver figures for the same 2 groups of GPs at regional and ICB level, which includes GPs moving between regions and ICBs.
- Reasons for leaving – We have published information on the reasons reported for leaving general practice roles, as well as the average age of leavers for each reason within each staff group. Caution is required in interpreting these results, as it is not mandatory for practices to record a reason for leaving.
- Previous and next roles of partner and salaried GPs – Every quarter, we publish analyses of the path GPs take into and out of partner and salaried roles. This includes the number of salaried GPs who are new to general practice compared to those who previously worked in general practice in a different role (for example, partner or locum).
- Tracking GPs in training into fully qualified general practice roles – We publish quarterly analysis on GPs in ST3 training placements recorded in the Training Information System (TIS) who can be tracked into the fully qualified GP workforce as recorded in the National Workforce Reporting Service (NWRS), by gender and country of PMQ
While practices do not have fixed establishment positions against which they report vacancies, NHS England is working with the NHS Business Services Authority (NHSBSA) to release data on job adverts placed on NHS Jobs by practices. While this will not provide a comprehensive view of vacancies, as practices can use other advertising media, it will improve understanding of recruitment in general practice.
13.5 GP educators
A shortage of educators and supervisors is hindering efforts to expand GP numbers. The Royal College of General Practitioners’ survey report Fit for the future: Reshaping general practice infrastructure in England (May 2023) explained why practices find it difficult to take on more GP trainees or other learners. 47% of respondents reported a shortage of educators or supervisors, and 84% reported a lack of physical space.
The GMC’s The State of Medical Education and Practice in the UK: Workplace Experiences report found that GPs with training responsibilities were under more pressure than their non-trainer colleagues, and the National Training Survey (2024) found that 50% of trainers were at high or moderate risk of burnout. 64% of GP trainers said they always or often felt worn out at the end of a working day.
The expansion of roles across primary care and the increase of GPST places have increased the role of GP trainers and their workload. Feedback from all regions consistently highlights the imbalance between workload and remuneration as the main reason practices and doctors decide not to join the training community.
13.6 Earnings and expenses
Trends in pay and earnings for contractor GPs
The average income before tax for contractor GPs in England working in either a GMS or PMS practice in 2022/23 was £140,200, compared to £153,400 in 2021/22, an 8.6% reduction following the cumulative 25.9% increase over the previous 2 years. There has been a net cumulative 15.1% increase since 2019/20.
The reduction between 2021/22 and 2022/23 is mainly due to the reduction in additional funding provided for the delivery of the COVID-19 Vaccination Programme.
The GP Earnings and Expenses Estimates (2022/23) (the latest available) shows trends in average PMS contractor net earnings, including cumulative cash and real terms growth. Table ‘1b. GPMS contractor real terms’ shows trends in average gross earnings, expenses and net earnings for PMS contractor GPs in England and the ratio of their expenses to gross earnings between 2013/14 and 2022/23.
Contractor GP earnings increased by 37.6% in cash terms and 11.4% in real terms over the same period. Expenses rose from 65.0% of gross earnings to 71.7% (see data pack [link to be inserted once published] for further information).
Trends in the earnings and expenses of salaried GPs
The average income before tax for salaried GPs in England working in either a GMS or PMS practice in 2022/23 was £69,200, compared to £68,000 in 2021/22, a statistically significant increase of 1.8%. This is 2.7% below the DDRB recommended uplift for 2022/23 of 4.5% and is only partially offset by the additional 1.8% uplift above the 3.0% DDRB recommendation for 2021/22 to give the 4.8% actual uplift.
Table ‘7a. salaried GP earnings by country’ and table ‘7b. salaried GP GPMS real terms earnings’ set out trends in average gross earnings, expenses and net earnings for salaried GPs in England and the ratio of their expenses to gross earnings between 2013/14 and 2022/23.
Salaried GP earnings increased by 26.1% in cash terms and 2.1% in real terms over that period. Expenses fell from 14.4% of gross earnings to 13.2%.
Table ‘12. salaried distribution’ shows that the number of GPMS salaried GPs in England in the £100,000+ income before tax band rose 18% from 1,610 in 2021/22 to 1,900 in 2022/23.
Gender and ethnicity pay gaps
The Independent Review into Gender Pay Gaps in Medicine identified a wider gap for salaried GPs compared to hospital and community health service doctors, clinical academics and contractor GPs. Table ‘14. GPMS combined GP earnings by age and gender’ provides the most recent available data, comparing pay per head for men and women salaried GPs and contractor GPs in the same age bracket. However, this data has accuracy and quality limitations and accurate conclusions can’t be drawn from it. Comparing pay per FTE would give a better picture of the gender pay gap for salaried GPs, given the difference in average working hours between male and female salaried GPs.
No data is available on GP pay by ethnicity. However, since May 2023, NHS England has published quarterly data on ethnicity of GPs by job role.
GP appraiser fee
GPs, like other doctors, are subject to revalidation and must engage in annual appraisal. NHS England provides an appraisal programme for all GPs included on the England medical performers list (about 59,000) and recruits, trains and contracts with appraisers. The appraisers do not need to be GPs themselves.
The objectives and delivery of the appraisal programme are currently the subject of an NHS England review. There is a set fee for each appraisal (currently £584, in line with the DDRB recommendations for 2022/23) and an annual total cost of about £28 million plus pension contributions.
The time spent preparing for, carrying out and writing up an appraisal can vary greatly. However, in most cases, the time required is less than the equivalent of a half-day session. It is of concern, therefore, that time spent on appraisals is being remunerated at the equivalent of an annual salary of about £250,000 per annum, considerably more than would be earned delivering clinical work. NHS England submits that the GP appraiser fee is a fee for a service and should be subject to periodic value for money review, particularly in light of changed appraisal requirements. It should not remain within the DDRB’s remit for further increases alongside salaries.
14. The dental workforce
14.1 Dentists in training
The government caps undergraduate dentistry intake numbers for home and international students (defined as those from countries outside the EEA). More than 800 places are available each year in England. The number of unique applicants to dentistry in 2023 was at an all-time high, with 4,415 applicants and 830 acceptances. This equates to a 19% success rate for applicants.
Dental foundation training
In 2023/24, 97% of postgraduates satisfactorily completed dental foundation training (DFT). 2% required an extension and 1% exited training.
A loss of training sites within DFT is a growing risk that impacts the placement of UK graduates. The decline is driven by factors including the workload on training practices and educational supervisors, as well as static payments for the service component of training, which have not increased since 2013 despite rising inflationary costs. The payment issue is a disincentive for practices and requires urgent review from relevant government bodies. Foundation training plays a significant role in introducing graduate dentists to NHS general dental practice, and DFT is also the main route for UK dental graduates to be accepted onto the NHS performer list.
Dental core training
Dental core training (DCT) recruitment for 2024 received an overall above-average rate of applications for posts across the UK. The application numbers were particularly high from overseas dentists, with an increase of over 1,000 additional applications for DCT1 posts. As of September 2024, England-only data shows a strong fill rate for DCT, with Year 1 filling 87.6% of positions, Year 2 filling 74.9%, and Year 3 achieving 94.7%.
98% of postgraduates satisfactorily completed DCT. The option for trainees to extend DCT was introduced in 2022. 1% of postgraduates completing DCT in 2024 required an extension to their training, and 1% resigned from post during training.
Despite high fill rates in DCT, more can be done to improve trainee satisfaction. A review of DCT posts found a variety of reasons for trainee dissatisfaction. Location, out-of-hours duties, specialty rotations and run through programmes all contributed. However, the relevance of each factor varied across regions.
All regions are now rolling out versions of early- and middle-years programmes (see below) to incorporate run through 2-year versions of DFT and DCT training. Work has been undertaken with the General Dental Council (GDC) on the initial application and supervision requirements for temporary registrants performing local service duties in place of DCT posts. Standardisation and improved processing of applications has enabled overseas dentists to start in posts much earlier than in previous years.
Dental specialty training
As of September 2024, England-only data shows that most specialties had full recruitment. Oral surgery (ST1), orthodontics (ST1), paediatric dentistry, public health dental, and restorative dentistry all filled 100% of their posts. However, oral medicine (ST1) had a lower fill rate of 66.7% and special care dentistry (ST1) and orthodontics (ST4) had notable gaps, filling only 53.3% and 52%, respectively.
The under recruitment in special care dentistry is particularly concerning given the ageing population. There is also a shortage of consultant-level orthodontists. Many trusts have vacancies. The Post-Certificate of Completion of Specialist Training (CCST) in orthodontics plays a crucial role in training primary care orthodontic specialists to become consultants and to deliver more complex care.
Dental Education Reform Programme
The Dental Education Reform Programme (DERP) includes work to develop more flexible training experiences in varied settings, build better training pathways for dentists and dental care practitioners (DCPs) and support more multidisciplinary working. Evidence suggests that dentists could be released for more complex work if other members of the dental team were working to their full scope of practice.
The DERP dental training distribution workstream has sought to address patients’ lack of access to specialist dental services by funding additional training posts in oral surgery, special care and paediatric dentistry.
Delivery to date includes:
- the Early Years Postgraduate Dental Training Programme is introducing a new curriculum, with early adopter regions in England implementing this in 2024
- the Middle Years Postgraduate Dental Training Programme has completed scoping work across all regions and has highlighted that there are run-throughs for DCT1-2 and DCT2-3 in some regions. A curriculum for the Middle Years Programme is in development to support a 2-year training programme spanning DCT years 2 and 3, providing rotational posts across the different dental specialties and better support to trainees to gain enhanced skills in their career progression to dental specialty training
- a Return to Dental Therapy (RtDT) task and finish group established in 2023 developed a set of recommendations for a RtDT approach across England
14.2 General dental practitioners
Access to NHS dental services remains challenging despite NHS England’s 2022 reforms. Stabilisation of the workforce is critical to delivering further improvements for patients, and we have taken steps to address this through the Dental Recovery Plan. However, dentists are rarely employed on a salaried basis within NHS primary dental services. A high proportion of dentists delivering NHS dental care work as associates on a self-employed basis. They negotiate their own terms of engagement with the NHS contract holder, with limited requirements on either side regarding pay and conditions apart from those referenced in the Statement of Financial Entitlements (SFE).
Available data sources to understand general dental practitioner recruitment, retention and morale
The evidence presented below draws upon several data sources to describe our understanding of NHS dental services and the recruitment, retention and morale of both NHS dental contract holders and associates:
- NHSBSA activity data
- Dental statistics – England (2023/24)
- Dentists’ working patterns, motivation and morale (2022/23)
- Dental earnings and expenses (2022/23)
- NASDAL and Morris and Co. expenditure data (provided by NASDAL, data not published)
- NHS England dental workforce collection (data due to be published)
Delivery of NHS dental contracts
NHS England regularly monitors contract delivery. This is measured using data taken from FP17 forms transmitted to the NHSBSA. This analysis demonstrates that the number of units of dental activity (UDAs) being delivered as a proportion of UDAs commissioned has continued to improve since the end of the pandemic.
Numbers of dentists providing NHS care
The Dental statistics for England (2023/24) suggest that the number of dentists delivering NHS care (based on the number of unique individuals submitting an FP17 form) has stabilised. This data does not capture dentists who undertake NHS work that does not require an FP17 form transmission (for example, some working in community dental services (CDS)). It is therefore an underestimate of the total number of dentists providing NHS care.
While the number of dentists delivering services has not fallen, data from Dentists’ Working Patterns, Motivation and Morale (2022/23) may indicate that some dentists have reduced the time they spend on NHS-funded care. Data from 2022/23 shows the proportion of dentist time spent on NHS work was 70%, a slight decrease on the previous data point of 73% in 2019/20. However, reported time commitments have varied over the last decade from 70% to 74%. The data collection was paused during the pandemic, so we are unable to comment on the proportion of time spent on NHS care during those years and how the latest data relates to it.
Overall, the data indicates that, since the pandemic ended and contracting arrangements returned to normal, the number of dentists providing NHS care has begun to stabilise, and contract delivery has continued to improve.
Morale and motivation
Data from Dentists’ Working Patterns, Motivation and Morale (2022/23) indicates a decrease in the proportion of both provider-performer dentists (contract holders) and associates reporting ‘very high’ or ‘high’ morale. This represents a continuation of a downward trend for both groups. Still, levels remain comparable with dentists in other countries of the UK, suggesting the factors behind the trend are more nuanced than simple dissatisfaction with the contract in England.
Potential drivers of low morale also vary by type of dentist. The single largest reported driver of low morale in provider-performers was expenses versus income. While this was true for all countries in the UK, it was endorsed marginally less frequently by dentists in England compared to the other home nations. Provider-performer dentists also identified concerns about recruitment and retention as having a major effect on morale.
Associate dentists were more likely to identify concerns about litigation risks and indemnity fees as causes of low morale. This data suggests there is anxiety within the profession that the complexity and therefore cost of providing dental care to some patients is higher than the financial return.
To help address these concerns and make NHS dentistry a more attractive and sustainable area, NHS England have raised the minimum indicative UDA value from £23 to £28. In addition, NHS England has also introduced a new patient premium (NPP) to run to 31 March 2025 as part of the Dental Recovery Plan. The NPP is a payment to dental practices for each eligible new patient they treat. The amount paid depends on the type of care required and is in addition to the funding accrued to the course of treatment:
- Band 1 care: £15 per patient
- Band 2 or 3 care: £50 per patient
There is no legal requirement for contract holders to pass DDRB uplifts, payments for NPP credits or the minimum UDA value uplift on to performers and NHS England remains concerned about the impact this may have on morale.
Earning and expenses
NHS dentistry remains profitable for both contractors and associates, although profits for 2022/23 decreased slightly compared to 2021/22. Data from the Dental Earnings and Expenses (2022/23) report showed a non-significant decrease of 0.90% in pre-tax income for associate dentists from £64,900 to £64,300 across all contract types. A non-significant decrease was also reported for contract holders of 4.6% from £135,000 to £128,800. These figures are slightly lower than those presented by NASDAL in their NASDAL benchmarking report for 2022/23, which reports NHS practice profits of ~£157,000 per provider. NHS England is unable to obtain the full NASDAL report but understands that DDRB has access to this.
Data from NASDAL and Morris and Co. provides the percentage of gross income spent on certain categories of expenditure for NHS and private practices, and, since 2020/21, is inclusive of practices delivering a mix of both NHS and private care within England. The data indicates that the percentage of gross income spent on laboratory, material, and other non-staffing costs has increased for NHS practices since services returned to normal contractual arrangements. However, the overall trend is that the percentage of gross income spent on these costs has remained relatively stable and, for some cost lines, has decreased for NHS practices over the last 10 years. The main area where this doesn’t apply is the percentage of gross income spent on non-clinical staff wages, which remains higher for NHS practices in 2022/23 (21.2%) compared to private (18.3%) and mixed practices (20.2%).
Recruitment
Data from NHS practices that completed the NHS England dental workforce collection (due to be published in December 2024) indicates that the vacancy rate for NHS general dentists in England is 17%. There is some variation between regions, with London reporting the lowest vacancy rate (15%) and the Southwest region reporting the highest (22%).
To help support recruitment in areas with poorer access for patients, NHS England have introduced an incentivised recruitment (‘golden hello’) scheme, providing funding of £20,000 to each dentist. NHS England will evaluate the scheme’s impact once it is fully implemented.
Community dental services
NHS England has 68 contracts that provide CDS across 296 geographical locations. Most of these are held with foundation, community and mental health trusts and the remainder with community interest companies (CICs). Those employed by NHS trusts are remunerated based on nationally agreed pay rates, determined by DHSC. Those employed in CICs may be subject to different rates of pay and wider terms and conditions. CICs tend to reference the NHS bands for salaried dentists when setting their pay scales, and they need to comply with the employment protections and payments laid out in the SFE. However, their pay scales will also reflect the individual contract value.
Data from the NHS England dental workforce collection provided by 54 CDS providers, indicated that the vacancy rate for general dentists working in CDS was 13.4%, which is lower than the national average within high street practices.
14.3 Dental reform
In the joint DHSC/NHS England Dental Recovery Plan, we committed to developing further recommendations for dental contract reform to properly reflect the care needed by different patients, more fairly remunerate practices, and make NHS dental care an attractive career choice where all professionals can work to their full scope of practice.
The SFE was amended in December 2022, allowing commissioners to agree overperformance of UDAs and units of orthodontic activity (UOAs) up to 110%. Unpublished data provided by NHSBSA showed that in 2023/24 more than 15% of contracts received a payment equating to about £22 million for overperformance. Throughout 2024/24, NHS England will collaborate with ICBs to identify opportunities to support contractors in delivering additional capacity beyond their current contractual obligations (up to 110%).
We have made it easier for ICBs to free up funding for practices that can deliver more by addressing persistent contract under-performance. The SFE was amended in April 2024 to allow commissioners to permanently and unilaterally amend NHS dental contracts that fail to deliver their contracted amount of dental activity over 3 consecutive non-COVID-19 years. While the default expectation is that commissioners should try to reach an agreed reduction with the contractor, the SFE allows a unilateral rebase where agreement cannot be reached.
Skill mix guidance was published to highlight the opportunities for practices to reduce pressure on dentists. Since 2022, we have seen an increase in hygienists and therapists undertaking Band 2 treatments. In June 2024, amendments to the Human Medicines Regulations 2012 (HMR 2012) enabled suitably trained and supported dental hygienists and dental therapists to supply and administer specified medicines (for example, certain local anaesthetics and fluoride varnish) without requiring a Patient Group Direction or a Patient Specific Direction from a dentist. We continue to work with the GDC and others to promote good practice in skill mix utilisation and address any concerns and questions from contract holders.
15. Reform
15.1 Employment contract reform
We are pleased that the trade unions and government have resolved the pay disputes involving consultants, SAS doctors and doctors in postgraduate training.
NHS England is working with DHSC, NHS Employers and the medical trade unions to support the implementation of the various components of the pay and contract reform deals.
The DHSC’s evidence provides detailed information about the recent deals; we are offering information on the elements that NHS England is playing a leading role in implementing — and providing some general commentary which will be of interest to the DDRB.
The additional investment in the doctors’ pay deals seeks to increase productivity and efficiency, support effective performance management, and reduce inequalities across the workforce. But it will take time to assess what benefit is delivered.
15.2 Consultants
Key features of the consultants’ deal included reducing the time it takes for consultants to reach the top of the pay scale and an amendment to the Terms and Conditions of Service (Consultants) 2003 to introduce provisions for shared parental leave. Both should help to reduce the gender pay gap in medicine. (More information on NHS England’s work to reduce the gender pay gap in medicine is referenced under the NHS Equality Diversity and Inclusion Plan section of this evidence.)
The introduction of shared parental leave also brings the terms and conditions for the consultant workforce in line with those for other medical and non-medical staff groups, improving equity across the workforce and ensuring the NHS offers a modern and consistent ‘employee value proposition’ to all staff.
To support implementation of the new pay progression process for consultants, NHS England have worked in partnership with NHS Employers, DHSC, and the medical trade unions to develop joint guidance for employer organisations. This is hosted on NHS Employers’ website.
To complement this guidance, NHS England has recently developed an Improvement Guide: Medical Consultant Job Planning for the consultant and SAS workforce, sharing learning from across organisations and offering a range of practical ideas to improve job planning. It supports implementation of the consultant and SAS deals, both of which place a greater emphasis on the need for doctors and employers to work together to carry out effective job planning.
15.3 Clinical excellence awards
NHS England lack an evidence base to evaluate the effectiveness of the National Clinical Impact Awards (NCIA) scheme in supporting recruitment and retention of medical staff or its impact on patient care and productivity. This will be covered in the DHSC’s evidence. As referenced in the retention section of this submission, the reasons why staff leave are multifaceted. It is therefore hard to determine the impact of the NCIA scheme in isolation on retention of the consultant workforce. We suspect that NCIAs probably do very little in terms of recruitment because there is no guarantee of winning an award. However, NCIAs are an attractive part of the wider total reward offer for the consultant workforce.
The recent reform of NCIAs, previously known as National Clinical Excellence Awards (NCEAs), sought to make the application process fairer and more inclusive and ensure the scheme rewarded and incentivised excellence across a broader range of activity and behaviours. NHS England supports this. However, we again lack an evidence base to assess the scheme’s effectiveness in promoting equity. This will be covered in DHSC’s evidence.
We believe the removal of the contractual entitlement to new Local Clinical Excellence Awards (LCEAs) as part of the government pay deal with consultants was the right decision. Consolidated LCEAs awarded before 2018 will be retained and will remain consolidated and pensionable (up to the value of £36,000). These may aid retention to some extent, although they may also mean that some individuals are in a financial position to think about retirement earlier.
LCEAs have always been a divisive area given competition for awards and varying perceptions about the fairness of outcomes. Typically, they have required significant amounts of additional resource (for example, the sourcing and training of award panel members and administrative and IT infrastructure). Given that in recent years the default position of employers has been to equally distribute funds to those that meet the basic criteria, this raises questions about whether LCEAs were actually rewarding excellence.
LCEAs have contributed to the gender pay gap in medicine. We believe removing them and using the LCEA funding released to support reforms to the pay scale will go some way to addressing that gap.
15.4 SAS
The new SAS contracts were introduced from 1 April 2021, following agreement by all parties. The new grades were linked to a 3-year deal including annual pay increases, which ended on 31 March 2024. NHS England supported the introduction of these new contracts. They provide modernised national contracts that are attractive to doctors who do not wish to pursue a career as a consultant or who want to step out of training to focus on providing NHS services. With flexibility in mind, the grades were designed to closely align with pay points in other medical grades.
In previous years, differing pay awards – between those who stayed on the old contracts and those under the three-year pay deal for the new contract – created a disincentive for some SAS doctors to transition to the new contract. This has made it harder to realise the full benefits of the new contract. NHS England is keen for any pay award for 2025/26 to support the transition to the 2021 SAS contract for those on the old contracts. This will help us get the most from the approach to SAS contract modernisation agreed with trade unions.
Following months of negotiation, SAS doctors accepted a revised pay offer in June 2024 that includes a pay uplift of between 6.1% and 9.22% for those on 2021 contracts and a consolidated pay uplift of £1,400 for those on non-2021 contracts.
The offer was designed to address the imbalance between old and new contracts, speed up the delivery of some of the key objectives of the 2021 deal, and encourage more existing SAS doctors to take up the new contracts.
Between the withdrawal of the national specialist grade in 2008 and the introduction of the specialist grade in 2021, there was no national grade between specialty doctor and consultant. The introduction of the specialist grade gives flexibility to both employers and senior doctors: employers can create specialist roles that best provide the skill mix they require, and doctors have an alternative senior grade to consultant if they meet the entry requirements. The reformed SAS grades are aligned to the commitments in the NHS Long Term Workforce Plan and have an important medium- to long-term role in providing attractive and flexible career routes as the aspirations of doctors in postgraduate training change.
To support implementation of the SAS deal, NHS England has worked with DHSC, NHS Employers and the BMA to develop guidance on establishing the specialist role in England. The guidance, which has been published on NHS Employers’ website, helps providers to identify the circumstances in which a specialist role can be established within a medical and/or dental workforce structure. This aligns with our commitment in the NHS Long Term Workforce Plan to work with stakeholders to enhance the professional experience of SAS doctors by developing equitable opportunities for promotion and career diversification.
As part of implementation of the SAS deal, NHS England is also:
- exploring what national levers are available to encourage, establish, and embed specialist roles, including finalising the SAS Excellence in Development Recognition Award, due to launch in Spring 2025 (mentioned above)
- working with partners to collaborate on a shared objective of helping SAS doctors to progress through the portfolio pathway
- undertaking a joint piece of work with partners to understand how LEDs can be better supported to progress in their careers, building on NHS England’s LED Blueprint for Change (mentioned above)
15.5 Doctors in postgraduate training
In September 2024, the dispute between the BMA resident doctor committee and the government was resolved following months of protracted negotiations. The offer is designed to reform pay and includes measures to improve the experience of resident doctors in England.
At the time of writing, an implementation group had recently been established, with NHS England participation, to discuss the detail of the deal, including flexible pay premium uplifts and changes to the exception reporting process. A separate workstream outside of the implementation group is reviewing the training model (specifically, the number and frequency of rotations). This separate workstream is part of the Improving Working Lives of Doctors in Postgraduate Training Programme referred to in a previous section of this submission.
15.6 Rate cards
We are pleased that the BMA have withdrawn the rate cards for extracontractual activity for consultants, SAS, and doctors in postgraduate training following acceptance of the deals. The BMA’s suggested minimum rates were more than triple the estimated basic hourly rate for a consultant and more than what employers typically pay for additional activity.
15.7 NHS Pension Scheme reform
The new flexible retirement options were introduced to encourage staff to prolong their working lives. For example, retire and re-join (effective from 1 April 2023) is particularly attractive to staff with the special right to take their pension unreduced from age 55 (nurses, midwives, physiotherapists and health visitors); and partial retirement (effective from 1 October 2023) allows staff to take up to 100% of their pension and carry on working, without taking a break in their employment. At the time of writing, the NHS Business Services Authority report that since 1 October 2023 18,881 NHS staff have taken partial retirement.
More than £13 billion of employer and employee contributions is invested in the scheme every year, but widespread ignorance and misunderstanding about its value remain. The scheme is an important lever for attracting, retaining and encouraging staff to return to the NHS.
NHS England’s Pension Response Project, developed in 2021, supports leaders to influence behaviour change. By demonstrating the financial benefits of the scheme to staff and their loved ones, it seeks to persuade staff who would otherwise retire earlier than planned or who plan to retire when they reach their normal pension age (60, 65 or older) to work longer or return to the NHS after retiring.
Since 2021, working with our pension partners, we have led virtual staff pension seminars and master classes for line managers to explain the pension basics, flexible retirement opportunities and implications for those still affected by pensions tax. We have reached over 27,800 staff. Though this is a modest number, qualitative data (staff feedback following virtual pension seminars) suggests staff appreciate and value the opportunity to ask questions and clarify their understanding.
At the March 2023 Budget, the previous government reduced the tax disincentive for 10s of 1000s of NHS staff by increasing the annual allowance from £40,000 to £60,000 and abolishing the lifetime allowance.
However, although far fewer NHS staff are affected by pension tax, for some, opting out of the NHS Pension Scheme because of the continuing impact of pensions tax may be a sound financial decision. In March 2023, NHS Employers published pension tax guidance to support trusts to explore options for retaining staff still affected by pensions tax.
In August 2023, NHS England wrote to trusts about the flexibility they have to develop local NHS Pension Scheme employer contributions recycling schemes; some have already introduced such schemes. The decision to offer recycling schemes is for trusts to make and should focus on securing best value for money and delivering the best possible outcomes for patients.
We will continue to work closely with NHS Employers and DHSC over the remainder of 2024/25 to identify and agree interventions that highlight the value of flexible retirement and other pension-related options for staff in late-stage career. We want to retain the experienced and skilled staff the NHS needs to support recovery and their less experienced colleagues.
16. Annex
Determining leavers from NHS secondary care
Leaver rate methodologies comparison
Summary
This document details the methodology behind the NHS England/NHS Long Term Workforce Plan leaver rate definitions and how they compare against other leaver rates already in the public domain.
Data source
ESR is a HR and payroll system in place in all NHS secondary care providers in England, as well as some other healthcare organisations. Data from ESR is used to support the delivery of national workforce policy and strategy, including monitoring of staff retention (Electronic Staff Record (ESR) Workforce Services | NHSBSA). Primary and social care organisations do not always use a unified payroll system such as ESR, so we are not currently able to derive information in the same way, although there is a dedicated data collection for the GP workforce.
Information is inputted at source by employees, managers and HR departments in organisations registered on ESR. This information is pulled monthly from ESR records to the ESR data warehouse owned by the NHSBSA. Data services teams at NHS England pull the data from the ESR data warehouse into NHS England internal data servers. Identifiable record-level information is pseudonymised which is then loaded into NHS England data warehouse where it can be directly queried by those with access rights. Leaver data is extracted from NHS England data warehouses using SQL scripts.
Identifying leavers
To identify who has left the secondary care workforce over a period of time, a snapshot of staff in post active on ESR is taken at timepoint 1 and compared to a snapshot of staff in post at timepoint 2 (see Figure 1). If an individual is active on ESR at timepoint 1 but does not appear at timepoint 2, they are assumed to have left the NHS secondary care workforce and their FTE is counted toward the overall leaver FTE for that period. We use annual leaver FTE, therefore timepoint 2 is one year after timepoint 1.
This method has limitations, for example if someone leaves and returns between timepoint 1 and 2, they are not captured. Furthermore, if someone moves to primary or social care but does not leave the NHS, they may be counted as a leaver if they no longer have an active ESR record.
Figure 1. Examples of how individual staff movements would be classed when determining annual leavers using NHS Long Term Workforce Plan method.

Leaver rate
Leaver FTE at timepoint 2 is identified using the method described above and illustrated in Figure 1. Leaver rate is calculated by dividing leavers at the end of the time period (TP2) by the staff in post at the start of the time period (TP1).
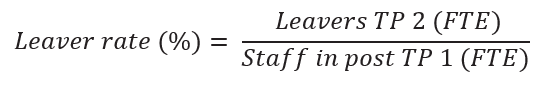
Differences between NHS England/NHS Long Term Workforce Plan methods and published official statistics.
There are other published official statistics about the NHS workforce derived from ESR which include information about leavers, joiners and movers in the NHS (NHS workforce statistics – NHS Digital). These employ different methods to the NHS England/NHS Long Term Workforce Plan-aligned figures. Differences in methods include the calculation itself, as well as inclusion and exclusion criteria regarding which types of staff should be factored in those calculations. Table 1 outlines difference between the two methods.
Table 1. Comparison of criteria in NHS England/ NHS Long Term Workforce Plan and official statistics leaver methodology.
| Criteria | NHS England/NHS Long Term Workforce Plan methodology | Official Statistics Methodology |
| Contract type | Includes staff with permanent, fixed term and locum contract types only (bank and agency staff are excluded). | Includes staff with permanent and fixed term contract types only (bank and agency staff are excluded). |
| Contracted FTE | No criteria applied based on contracted hours. However, staff without any contracted hours would not be included in FTE figures. | Staff with zero contracted hours excluded. |
| Organisation type | Records from all organisations on ESR are included. Thisincludes small numbers of staff in non-NHS organisations (for example, independent healthcare providers). | Only includes NHS Organisations, termed Core (e.g. Trusts) and Wider (for example, arms length bodies). |
| Multiple assignments | Where someone has multiple roles within the NHS at the same time, total FTE is summed across records. | Same methodology employed. |
| Inactive status (including staff on maternity leave) | Movement from a substantive role to inactive status (including maternity leave, career breaks and secondments) is not counted as a leaver. | Movement from a substantive role to inactive status is counted as a leaver. Employee is deemed not part of the ‘active’ workforce. |
| Payment received in period | Individuals are counted in staff in post and leaver FTE whether they have received any payment or not. | Staff must have recorded earnings on ESR in month to be included in all official statistics publications. |
| Change in hours | If an individual decreases their FTE, this is not counted towards leavers. | Where FTE is used as the measure, this is counted towards leavers. |
| Leaver rate calculation | Leavers TP2 (FTP) Staff in post TP1 (FTP) TP = timepoint | Leavers TP2 (FTP) (Staff in post TP1 + TP2) / 2 FTE Note the use of a different denominator between calculations |
| Unit of measurement | FTE only – the number of hours worked, indicative of capacity | Headcount (individual members of staff) and FTE |
| Backdating / retrospective revisions | ESR records relating to specific time periods can be updated/revised at a later point. This method takes snapshots of ESR records at the point of receiving the data from the data warehouse. We do not back-date any records, therefore such historical revisions would not be reflected in the data. | Same method employed – no retrospective revisions. |
The differences between methodologies means the derived leaver rate differs between the two datasets. Official statistics tend to state the national all staff leaver rate as 3 to 3.5 percentage points higher at any one time, as there are more cases in which someone is considered a leaver. However, trends in rates between the two datasets are the same.
Reasons for differences
The Official statistics and NHS England/NHS Long Term Workforce Plan leaver figures have different purposes. The NHS England/ NHS Long Term Workforce Plan leaver rate is used for workforce planning; therefore, it considers all staff who are available to work, not just those in active service (as in the official statistics method). Staff on career breaks, or maternity leave, cannot be legally replaced on a permanent basis therefore they must be included when making planning decisions or judgements. Therefore, only counting active service staff (those in receipt of pay) risks underestimating the workforce capacity.
Publication reference: PRN01677

