Summary
This Workforce development framework for health and wellbeing coaches:
- sets clear and consistent standards for health and wellbeing coaches
- demonstrates the benefits of health and wellbeing coaches working in the NHS
- provides information about the training, support, supervision, and continuing professional development (CPD) needed to enable them to succeed
- supports the development of a strong and capable workforce of health and wellbeing coaches
- supports improved quality and consistency of health coaching and reduces variation in outcomes and access standards.
The framework includes competencies for the role and links to resources to support employers to recruit and embed health and wellbeing coaches in services. Organisations employing health and wellbeing coaches, including primary care networks, can use this framework to support recruitment and retention. It will help them develop a greater understanding of the role, its scope of practice and the training and development health and wellbeing coaches need to enable them to practise safely and effectively.
Health and wellbeing coaches are non-clinical, personalised care roles. They work with people with physical and/or mental health conditions, people with long-term conditions and those at risk of developing them. They focus on improving health related outcomes by working with people to set personalised goals. Health and wellbeing coaches offer people support to increase their self-efficacy, motivation and commitment to make changes to their lifestyle and improve their health. Health coaches are experts in behaviour change, working in a person-centred way – they are not directive or prescriptive and they do not give advice. Evaluations show that health coaching can produce positive effects on adoption of healthy behaviours, improving physical activity, weight management, body mass index (BMI), blood glucose levels (HBA1c) and dietary fat, along with improving patient satisfaction and quality of life (see appendix one: evidence).
They work in different settings across health and care, including but not limited to primary care, hospitals and secondary care services. They offer significant benefits to the individuals they support and the health and care system, for example freeing up clinical capacity and improving patient outcomes. Health and wellbeing coaches can also support people to stay well while they wait for clinical interventions.
Health and wellbeing coaches need to be supported and enabled to succeed in their role. Before employing health and wellbeing coaches, employers should be clear on the purpose of the role and how it can contribute to meeting people’s needs and neighbourhood/place/system priorities.
Before taking referrals, employers should ensure that health and wellbeing coaches have the necessary skills and training. Health and wellbeing coaches should complete a Personalised Care Institute accredited four-day health coaching training course. This is the minimum required training standard. Employers are responsible for funding any necessary training.
Good supervision arrangements for health and wellbeing coaches are crucial to ensure they practice safely and effectively. There are three types of supervision that health and wellbeing coaches should receive:
- line management support and supervision
- access to supervision from a clinician
- health coaching supervision and CPD.
Health and wellbeing coaches manage a caseload of patients, often working closely with colleagues in a multidisciplinary team (MDT). Caseloads should be determined based on the complexity of cases, the support needs of the individual and the capacity and experience of the health and wellbeing coach.
Employers should support health and wellbeing coaches in their CPD by giving them dedicated time, and where necessary, funding for training and CPD. Regular supervision sessions, appraisals and personal development planning should all be used as opportunities to focus on specific needs to progress and/or meet the competencies for the role. Health and wellbeing coaches themselves, their supervisors and employers have collective responsibility for CPD.
1. Introduction
This framework supports health and wellbeing coaches, and their employers, to understand the role and set them up to deliver personalised care safely and effectively in a range of health and care settings. The framework replaces previous guidance and resources issued by NHS England about the role of health and wellbeing coaches.
The role of health and wellbeing coaches is developing and maturing in the health and care system and this framework is a useful resource for those who want to embed health and wellbeing coaches in a service. It will be of particular use to:
- health and wellbeing coaches working in NHS settings
- primary care networks (PCN), and staff working in them, employing health and wellbeing coaches through the Additional Roles Reimbursement Scheme
- organisations employing health and wellbeing coaches including secondary care, voluntary, community and social enterprise sector
- colleagues involved in workforce planning and redesign.
The framework sets out the fundamental competencies and training needs of health and wellbeing coaches, regardless of the setting they work in. While the core competencies remain the same, employers should recognise that health and wellbeing coaches working in specific settings or with specific groups will need additional knowledge, skills and training.
This framework has been developed by NHS England, in collaboration with a range of stakeholders including Health Education England. It includes information on the professional support and development health and wellbeing coaches need to work with people to optimise outcomes. Its purpose is to:
- set clear and consistent standards for health and wellbeing coaches
- demonstrate the benefits of health and wellbeing coaches working in the NHS
- provide information about the training, support, supervision, and continuous professional development needed to enable them to succeed
- support the development of a strong and capable workforce of health and wellbeing coaches
- support improved quality and consistency of health coaching and reduce variation in outcomes and access standards.
It also provides clear and consistent guidelines for training providers developing and delivering four-day Personalised Care Institute accredited health coaching courses.
2. Context
The NHS Long Term Plan set out the need to make personalised care business as usual across the health and care system, committing that “people will get more control over their own health and more personalised care when they need it.”
Additional complementary frameworks have been developed for two other personalised care roles – social prescribing link workers and care co-ordinators.
3. What is a health and wellbeing coach?
Health and wellbeing coaches work with people with physical and/or mental health conditions, people with long-term conditions and those at risk of developing them. They focus on improving health related outcomes where lifestyle modification and self-management have a significant impact on outcomes and prognosis, by working with the person to set personalised goals.
They support people with their physical and mental health and wellbeing. They use coaching skills, models of behaviour change and positive psychology to guide people on how to meet their personal health and wellbeing goals. Coaches support people to think through their own challenges and goals, increasing their self-efficacy, motivation and commitment to move forwards to make changes to their lifestyle and improve their health.
For some patients the earliest stages of health coaching involve generating enough psychological safety to start to engage with support. Many people need this initial confidence building support before they can develop their own health and wellbeing goals.
Health and wellbeing coaches are an effective intervention for improving self-management, by developing people’s motivation, knowledge, skills and confidence around a variety of issues/conditions, including:
- weight
- diet
- activity levels
- stress, mood, low level mental health issues
- diabetes
- cardiovascular disease
- stroke
- hypertension
- end of life care
- persistent pain.
Health and wellbeing coaches can also support groups of people through group coaching sessions and structured self-management education. This can support the development and capability of peer support groups.
There are four tiers of practice/expertise for health and wellbeing coaches. More information about these tiers of practice can be found in the competency framework.
Health and wellbeing coaches can work in a variety of settings across health and care, including but not limited to primary care, secondary care, community services, acute services, and children and family services. They play a key role in multidisciplinary teams (MDTs) and work in partnership with colleagues to optimise outcomes for people and populations.
3.1 Benefits of a health and wellbeing coach
There is significant evidence into the effectiveness of health coaching (see appendix one and NHS England Health Coaching Guide). Internationally it is a profession with standards, accreditation and a strong research base.
Evaluations show that health coaching can produce positive effects on:
- adoption of healthy behaviours, improving physical activity, weight management, body mass index (BMI), blood glucose levels (HBA1c) and dietary fat
- people’s motivation to self-manage, patient activation and self-efficacy
- patient satisfaction and quality of life (What is the evidence?).
3.2 Benefits to people
Health and wellbeing coaches support people by:
- focusing on their clinical and non-clinical needs and factors that may be impacting on their health and wellbeing
- working in partnership with them to guide and support them to meet their self-identified short and long-term goals
- empowering them to understand their own strengths and unlock their potential to self-manage their condition/situation
- supporting them to strengthen life skills, such as emotional regulation and executive function
- enabling them to sustain healthier lifestyle choices and improve health and wellbeing outcomes, sometimes while they wait to access other services
- helping them take steps to prevent long-term illness and prevent conditions from escalating.
3.3 Benefits to the health and care system
The skills and expertise of health and wellbeing coaches support the health and care system in a variety of ways. These can include:
- supporting people to develop their own knowledge, skills and confidence to self-manage their conditions, which can help to free up the time of clinical staff
- improving patient outcomes through sustained behaviour change, leading to improved blood sugar control, weight reduction, reduced blood pressure. In turn this can reduce the need for further clinical interventions, or ensure people have better outcomes from future interventions, for example surgery
- supporting people on NHS waiting lists to help them stay well, or prepare for upcoming clinical interventions
- tackling health inequalities through targeted work with specific groups identified through population health management data, for example, people with long-term conditions
- providing dedicated time, capacity and expertise to support people with behaviour change, helping to free up clinical time
- enhancing the quality of interactions between people and the health and social care system, improving satisfaction for both staff and service users.
4. Employing a health and wellbeing coach
As with any role in a health and care setting, health and wellbeing coaches should be supported and enabled to succeed in their role. Before employing a health and wellbeing coach employers should be clear on the purpose of the role and how it can contribute to meeting people’s needs and neighbourhood/place/system priorities, including objectives around population health management and health inequalities.
Employers should be confident that they have the necessary resources and support in place to embed the health and wellbeing coach into their team, so that the role can have the maximum impact – this role should be an integral part of multidisciplinary teams (MDTs). This includes having appropriate supervision arrangements in place for the role, which is essential, and provision for training and ongoing continuing professional development (CPD). Supervision and CPD should be more specialised where coaches are employed to work with a specific group or pathway, for example working with children and young people.
A template recruitment pack has been developed and is a helpful resource for primary care networks (PCNs) and other employers that want to recruit a health and wellbeing coach (you will need to register for a FutureNHS account to access this template and some of the other resources referenced in this framework). This sets out a job description, along with the skills and responsibilities of the role. Appendix two of this document includes a competency framework for health and wellbeing coaches, which should be used to support recruitment, retention, supervision and CPD.
4.1 Training and requirements prior to taking referrals
Health and wellbeing coaches come to the role with a wide variety of transferable skills and experiences, for example they could come from a health and care background, the private or voluntary sector. However, when working in the NHS, a basic level of training is needed before health and wellbeing coaches should take referrals. This is important for all health and wellbeing coaches to work safely and effectively, but particularly for those who have never worked in the NHS before.
Before taking referrals, employers should ensure that health and wellbeing coaches have the necessary skills and training. Training falls into two parts:
- personalised care and health and wellbeing coaching
- induction and training specific to the setting the role is based in.
It is the responsibility of the employer to ensure that health and wellbeing coaches have the appropriate level of training, and/or to support their training needs by funding and allowing time to attend training. This ensures a high standard of care and that the health and wellbeing coach has the maximum impact.
Tier 1 practitioners, in their first six to 12 months of practice, may be new to health and wellbeing coaching, and potentially the health and care system. Employers should recognise that this is the foundation stage for health and wellbeing coaches and they will be developing their skills and competencies.
1. Personalised care and health and wellbeing coach training
Minimum training requirement for health and wellbeing coaches: Four-day PCI accredited health coaching training
Source: Accredited training providers of this course can be found on the PCI website.
Cost: Funded by employer price varies depending on provider.
Health and wellbeing coaches working in health and care settings should complete Personalised Care Institute (PCI) accredited training before taking referrals, or at the start of their employment if they have not already done this. Details of the minimum training requirements, and recommended additional training for health and wellbeing coaches can be found on the PCI website.
New coaches may also benefit from:
- shadowing other coaches, especially around complex cases
- practising running sessions (face to face, online, by telephone) before seeing clients to provide opportunities for feedback and self-reflection
- spending time with team members they will receive referrals from or will work with
- building a set of resources which can help with sessions, for example, models and information for clients, such as apps, worksheets, podcasts etc.
2. Induction and training specific to the setting
Health and wellbeing coaches should complete an induction and training specific to the setting they are working in before taking referrals.
Examples of useful induction/training
- Mandatory training, including safeguarding and confidentiality
- Training in relevant IT systems, templates, and recording interventions
- Learning about the service, or setting, to understand different roles in the MDT, new ways of working, and how they link to the health and wellbeing coach
- Information and introduction to the service, the team, partner organisations and the locality
- Learning about specific patient groups or pathways, for example people with long term conditions
- Priorities of the employing organisation, and how the role contributes to them
- Policy context of the role. Eg supporting the Network Contract DES, elective care, etc
- Expected outcomes and boundaries of the role
4.2 Supervision
4.2.1 What is supervision?
Supervision is a process whereby individual health and wellbeing coaches are supported by others to meet their professional, organisational and personal objectives, which together promote best outcomes for the patient. There are three types of supervision for health and wellbeing coaches should receive:
- line management support and supervision
- access to supervision from a clinician
- health coaching supervision and CPD.
Supervision covers the various types of support a health and wellbeing coach will need to practise safely and effectively. It covers day-to-day management and professional expertise. Supervisors should have a good understanding of the level of skills and competencies a health and wellbeing coach has, where they are now and what they need to do to progress. They are enablers that support good working relationships and help to address issues and celebrate achievements. They encourage reflection and ongoing development and improvement.
Health and care providers regulated by the Care Quality Commission are expected to offer staff regular supervision to ensure staff are competent and confident to do their role. Primary care networks (PCNs) employing health and wellbeing coaches through the Additional Roles Reimbursement Scheme have a contractual responsibility to provide supervision as set out in the Directed Enhanced Service (DES).
4.2.2 Supervision requirements
Good supervision arrangements for health and wellbeing coaches are crucial and tier 1 practitioners may need more frequent supervision in the first six months as they learn about the role and the setting they are working in. Supervision is key in terms of supporting health and wellbeing coaches to excel in their role and in supporting their ongoing training and CPD. NHS England carried out a survey of health and wellbeing coaches working in primary care in autumn 2021 to understand their experiences. In the survey, lack of adequate supervision was cited as one of the main reasons for health and wellbeing coaches leaving their role. Employers will have their own resources and arrangements for line management and supervision, including carrying out appraisals.
There are three types of supervision that health and wellbeing coaches should receive.
1. Line management support and supervision
Recommended frequency: monthly with provision for ad hoc support
- general day-to-day management of the role. Provides support by giving advice, helping to manage caseloads
- first point of contact for health and wellbeing coaches
- line management responsibility for the health and wellbeing coach and lead on regular reviews, appraisals, training being met and personal development plans
- separate from the other supervision
- has an overview of all the supervision arrangements in place.
2. Access to supervision from a clinician
Recommended frequency: need to have a mechanism in place for any urgent queries which may arise.
Every two to three months for full time coaches (or pro-rata).
- named point of contact for support with clinical expertise and specific clinical concerns, for example, queries around medication, or a condition worsening which come up in a coaching conversation. This could be a GP, senior clinician or advanced practitioner, whose has the skills, knowledge and experience to offer appropriate clinical support
- pastoral and professional support
- supports experiential learning and reflective practice – case studies, significant events.
3. Health coaching supervision and continuing professional development
Recommended frequency: Individual health coaching supervision – one to two hours per month.
Group health coaching supervision also recommended as a supplementary development opportunity.
- provided by person experienced in health coaching (minimum tier 3 practitioner)
- support ongoing personal and professional development
- focus on developing the skills, competencies and confidence of the health and wellbeing coach in health coaching approaches and practice, and working through dynamics and issues with individual clients.
Where organisations commission health and wellbeing coaches via a third party arrangement, for example, through a voluntary sector or other partner, supervision arrangements should be agreed as part of the commissioning arrangement to ensure that appropriate supervision is in place.
Health and wellbeing coaches should be able to discuss patient related concerns and be supported to follow appropriate safeguarding procedures (for example, abuse, domestic violence and support with mental health) with a senior member of staff. Regardless of the setting the health and wellbeing coaches works in, it should be clear who they need to speak to in the first instance about any patient-related concerns.
PCNs should refer to section B4.5 of the Network Contract DES contract specification for requirements specific to that setting.
4.2.3 Who should provide health coaching supervision?
Health coaching supervision, to support the ongoing development of health coaching skills and expertise, should be provided by someone with adequate health coaching experience – a tier 3 practitioner would be the minimum expected experience. This could be a health and wellbeing coach or a clinical professional with relevant health coaching experience. The minimum standards for health coaching supervisors are outlined in the competency framework for health and wellbeing coaches.
Some accredited courses will offer a training package that provides an element of health coaching supervision, ongoing learning support and assessment of health coaching practice.
NHS England is currently looking at ways to develop increased health coaching supervision capacity and capability in the system. This will include exploring competencies and training for coaching supervisors. This framework will be updated in the future to reflect the outcomes of this work.
5. Ways of working – professional framework
5.1 Caseload
Health and wellbeing coaches are expected to manage a caseload of patients, working closely with colleagues in multidisciplinary teams (MDTs). They often support people with complex and multiple long-term conditions. Therefore, caseloads should be determined based on the complexity of cases, the support needs of the individual and the capacity and experience of the health and wellbeing coach. Health and wellbeing coaches should discuss caseloads and any concerns around it with their supervisor(s). When determining caseloads employers should be mindful of the level of training/experience the coach has – new coaches may need more support/time to manage caseloads.
Coaching sessions should be tailored around individual needs and can vary in length and frequency. As a guide:
- sessions usually last an average of 45-50 minutes, often with a longer more in-depth initial session
- frequency is determined by the coach and the individual
- the number of sessions needed is decided between the coach and the individual and not a service specification
- regular reviews should take place – every six sessions or as decided by the coach and client.
Health and wellbeing coaches use sessions to explore a range of topics with the client, this could include but is not limited to:
- exploring outcomes and goals
- increasing autonomy and motivation
- providing supportive challenge
- exploring someone’s current situation and options of change, including risks and benefits
- emotion regulation, emotion literacy and executive function
- supporting self-reflection to understand the relationships and connections between emotions, feelings, and behaviours
- exploring and challenging health beliefs, where appropriate
- increasing motivation, knowledge, skills and confidence to enable people to move on and self-manage, where appropriate. This will help to keep caseloads manageable and ensure capacity to accept new referrals.
It is unlikely that a health and wellbeing coach would hold more than four to five sessions per day. This allows time for updating notes, follow up tasks, conversations with colleagues in the MDT, decompressing between sessions and ad hoc follow up support.
5.2 Working with people (clients)
Health and wellbeing coaches support a variety of people from diverse backgrounds, including people with a range of conditions and disabilities. They should be able to adapt their communication approach to individual needs, including using plain language and culturally appropriate communication. Health and wellbeing coaches should ensure the people they support are able to say:
- I am listened to and understood, and ‘what matters to me’ is central to all our work together.
- I am respected and treated with dignity as an individual.
- My human rights are protected, and I do not experience discrimination.
- I experience warm, compassionate, personalised care and support.
- If I raise a concern or make a complaint, it is acted on quickly.
Coaches should set clear expectations around their expertise and knowledge and how they can support the individual. This includes setting boundaries and being clear on issues around confidentiality and safeguarding. Further information related to this section can be found in the competency framework for health and wellbeing coaches in appendix two.
5.3 Referrals to health and wellbeing coaches
Referrals to health and wellbeing coaches can come from a variety of places, depending on how the service is set up. Referrals could come via clinical staff, administrative and managerial staff, voluntary community and social enterprise (VCSE) partners, or even self-referral.
Health and wellbeing coaches can also work with MDT colleagues to proactively target patients who they feel could benefit most from their support. For example, using population health data and/or risk stratification tools to target people who need support to manage their health and wellbeing or who may be at risk of developing specific health problems.
5.4 Working as part of a multidisciplinary team
MDTs are groups of professionals working together with a focus on the person receiving care. MDTs can be in place in primary, secondary and community settings. Working this way allows a wrap-around, holistic approach to supporting people, allowing professionals to work together to explore problems and reach shared solutions. MDTs enable a wide range of experts to work with a person, including those from health services, social care and the VCSE sector.
Health and wellbeing coaches should be fully integrated within MDTs. They need access to other healthcare professionals, electronic ‘live’ and paper-based record systems, as well as administration/office support and training and development. Health and wellbeing coaches should attend MDT meetings to offer expertise on where health coaching, supported self-management and/or peer support could be beneficial to someone.
By including health and wellbeing coaches in MDTs people can be supported with their behavioural, social, emotional and practical needs. The unique contribution of a health and wellbeing coach is that they understand the person and their motivations, developing their capability to make and sustain healthy lifestyle choices. These changes could result in clinical outcomes, for example improvement in hypertension, but the MDT should be aware of the boundaries (see section 5.6) of this non-clinical role.
Health and wellbeing coaches need to build good working relationships with colleagues in the MDT and understand each role in the team. MDT colleagues may also need an introduction to the role of the health and wellbeing coach. This helps to build shared understanding of the value of the role and its utilisation in the MDT.
At tier 2 and above, the health and wellbeing coach also has a role in gathering feedback about their personal practice and service as a whole, for ongoing continuous quality improvement, and to share this with the wider MDT.
5.5 Working with other personalised care roles
Health and wellbeing coaches working in a primary care setting will often work closely with other personalised care roles. This includes social prescribing link workers and care co-ordinators. Each role has its own unique, distinct skills and competencies that lead to improved outcomes for people.
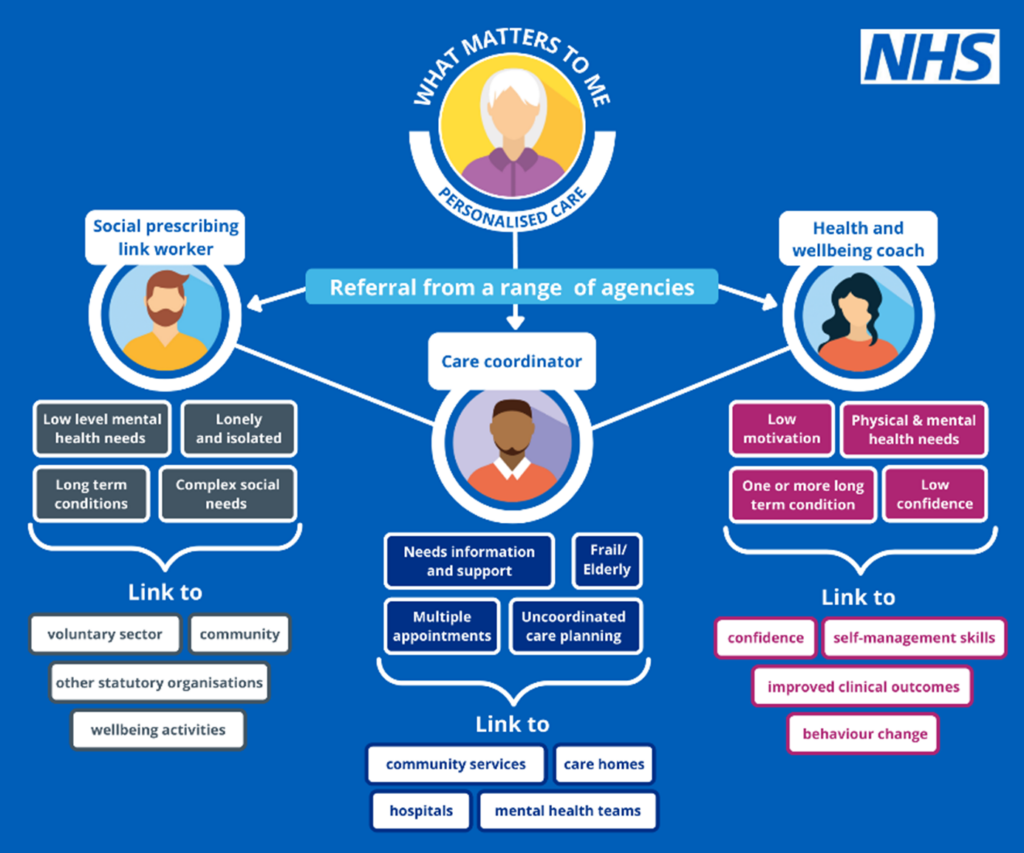
Diagram 1 illustrates how the three roles complement each other in a primary care setting by providing a holistic personalised care approach. These roles can also be employed outside of primary care and still work in a complementary way. Information about the roles of care co-ordinators and social prescribing link workers can be found on the NHS England website.
Diagram 1 – Personalised care roles in primary care
5.6 Boundaries of health and wellbeing coaches
Health and wellbeing coaches need to be aware that their role is non-clinical, keeping the focus on what is important to the person and not being drawn into taking a prescriptive or directive approach. For example, if supporting someone around weight management it is not the role of a health and wellbeing coach to diagnose and prescribe specific diets.
They need to be confident in their area of expertise and aware of the boundaries of their role. Boundaries are important in safely supporting people and in ‘contracting’ with them. This includes explicit contracting (such as communicating with the client what the service is and what a health and wellbeing coach can do) and implicit contracting (the way they will behave with the person, for example, balance between being friendly and supportive without stepping beyond role of a professional). These issues are covered in health and wellbeing coach training and can be discussed during coaching supervision and reflective practice. Supervision conversations are an ideal situation to set expectations of the role and where it starts and ends, this is especially important for health and wellbeing coaches who are less experienced or who may not have worked in the health and care sector before.
Health and wellbeing coaches will also need to be confident in spotting issues of concern, which should be discussed with a supervisor, or referred to another clinical colleague, for example, if a client is not clear about their medication, or what exercise they can safely do. Health and wellbeing coaches should also undergo safeguarding training and will need to know who their safeguarding lead is and who and when to ask for help.
6. Values and behaviours of health and wellbeing coaches
Health and wellbeing coaches should believe in and be committed to the values set out in the NHS constitution, along with the principles of personalised care and focusing on what matters to the person.
There are six NHS values that all staff are expected to demonstrate:
- Working together for patients
- Respect and dignity
- Commitment to quality of care
- Compassion
- Improving lives
- Everyone counts
They will also need to ensure their values and behaviours align with those of the organisation they are based in. It is the responsibility of the employer to communicate these with health and wellbeing coaches through their internal recruitment and induction process.
7. Competency framework
A competency framework for health and wellbeing coaches (appendix two) has been developed in collaboration with a range of stakeholders. It sets out the key competencies and capabilities needed to be a health and wellbeing coach. This framework should be used to ensure that people with the right skills and abilities are recruited to the role and as a tool to support ongoing continuing professional development (CPD).
The competency framework is aligned to the NHS England sample job description for health and wellbeing coaches and the Core Curriculum for Personalised Care published by the Personalised Care Institute. It is broken down into four areas:
- Professional competencies for health and wellbeing coaches.
- Skills for communication and enabling in a health coaching context.
- Knowledge of models and frameworks.
- Group work skills to support self-management and group approaches.
These core competencies are a foundation for health and wellbeing coaches from which specialist roles and competencies can be built on.
It is the employing organisation’s responsibility to ensure that it recruits people with the core competencies needed for this role and supports them to continue to develop these competencies. Employers should consider these competencies throughout the recruitment, induction and supervision process and support health and wellbeing coaches to develop a portfolio of evidence linked to these competencies.
8. Continuing professional development and training
8.1 Continuing professional development
Continuing professional development (CPD) supports health and wellbeing coaches to enhance and develop their personal and professional skills throughout their careers. CPD can be achieved in different ways including training, events, online learning, peer support, mentoring and action learning sets. It is important at all levels of practice.
CPD should cover the breadth of a health and wellbeing coach’s work, addressing both ongoing health coaching learning (for example, coaching styles/behavioural change models/reflective practice) and learning related to the clinical system in which they work (for example, diabetes or weight management).
Health and wellbeing coaches should be supported by their employer in their CPD and be given dedicated time, and where necessary funding, for training and CPD. Regular supervision sessions, appraisals and personal development planning (PDP) should be used to focus on CPD and any specific needs for career progression and/or meet the competencies for the role. CPD can be assessed as part of an annual appraisal or on a more frequent basis. Health and wellbeing coaches themselves, their supervisors and employers have collective responsibility for CPD.
To support their quality of practice and CPD, all health and wellbeing coaches should receive supervision from a person experienced in health coaching. Peer learning and networks, reflective practice, action learning sets and experiential learning are effective CPD approaches for health and wellbeing coaches.
8.2 Training
The following sections, and the competency framework, set out expected personalised care training standards for health and wellbeing coaches at four different career stages. This training may be supplemented by local training offers, specific to employers, places and systems, including training for staff working in primary care networks (PCNs) facilitated by training hubs.
There are four tiers of practice/expertise for health and wellbeing coaches:
Tier 1: People working at Tier 1 require a comprehensive, factual, and theoretical knowledge within their field of work and an awareness of the boundaries of that knowledge.
- Four-day health coaching training.
- 50 hours supervised coaching experience in the NHS.
Tier 2: People working at Tier 2 require a critical understanding of detailed theoretical and practical knowledge. They can demonstrate initiative and are creative in finding solutions to problems.
- 200 hours coaching experience in the NHS and evidence of level of competency.
Tier 3: People working at Tier 3 require a critical awareness of knowledge issues in the field and at the interface between different fields. They are innovative and have a responsibility for developing and changing practice and/or services in a complex and unpredictable environment.
- 500 hours coaching experience in the NHS and evidence of level of competency for that level agreed with supervisor.
Tier 4: People working at Tier 4 require highly in-depth knowledge, some of which is at the forefront of knowledge in their scope of practice, which they use as the basis for original thinking and/or research. They are leaders with considerable responsibility.
- 1000 hours coaching experience in the NHS and evidence of level of competency for that level agreed with supervisor.
8.2.1 Tier 1
Tier 1 practitioners will be new to working in the NHS, and could be new to coaching, they will need training before taking referrals. Section four of this framework sets this out in more detail.
Progression from Tier 1 to Tier 2 should be approved by a supervisor who is independent from the coach’s own organisation.
8.2.2 Tier 2
Training needs should be discussed in regular supervision sessions, appraisals and PDPs, as part of ongoing CPD, and decided upon based on the individual needs of the health and wellbeing coach and the competencies set out in the competency framework.
Health and wellbeing coaches at this stage in their career, should be encouraged and supported to develop their reflective practice (use and knowledge of models of reflection) to identity areas for improvement and development. They should also know how to select and apply relevant evidence-based themes and models to explore and develop their practice.
Training could include informal provisions such as attending webinars on subjects specific to the role, or formal offers via the Personalised Care Institute (PCI), training hubs, a PCN, trust, or integrated care system (ICS). Health and wellbeing coaches could benefit from a variety of training, including that specific to their role (for example, PCI training) or the setting they are working in (for example, training on internal systems or working with local people). They may also benefit from local training provision on topics such as mental health, trauma informed care, working with children and young people.
Tier 2 health and wellbeing coaches should be encouraged to engage with peer support networks, ‘buddy’ coaches and action learning sets. All of which are effective ways of building confidence and a sense of identity, as well as sharing experience. They help to develop self-reflection and improved ways of working.
Tier 2 health and wellbeing coaches may also benefit from training and development focused on management and evaluation of local services, to support ongoing continuous quality improvement of services. If they have the necessary experience, Tier 2 health and wellbeing coaches could also begin exploring becoming a coaching supervisor in the future.
8.2.3 Tier 3
At this stage in their career health and wellbeing coaches will need CPD to continue to reflect and build on their practice and keep up to date with the latest tools, models and techniques.
Tier 3 practitioners can undertake additional training to become coaching supervisors, enabling them to provide supervision for other coaches. Supporting CPD can enable the system to develop a pool of new coaching supervisors, laying the foundations for quality supervisors and managers. Coaches with this level of experience may also be interested in developing their knowledge and experience of system services and may benefit from additional training to become more involved in the management and evaluation of services.
8.2.4 Tier 4
Tier 4 practitioners will have the experience to be senior supervisors and are likely to have extensive experience of working in the health and care system, including service management and skills development. CPD is still important and topics could include advanced health coaching training and developing an understanding of managing services at a regional or national level.
8.2.5 Health and wellbeing coach specialisms
Some health and wellbeing coaches specialise in working with specific groups/conditions, for example, weight management, diabetes, learning disability, mental illness, cancer, children and young people and perioperative.
The fundamental principles of health and wellbeing coaching remain the same regardless of the setting and specialism, as do the competencies. Where health and wellbeing coaches specialise in working with a particular client group, or condition, they should have the necessary training and be supported by an appropriate professional and service. For example, if working with children and young people, health and wellbeing coaches would need specific training on working with this group and to sit in or be closely linked to a dedicated children and young people’s service. This would give the coach the necessary expertise and supervision to ensure they can meet the specific needs of children and young people.
Health and wellbeing coaches may want to develop their role to focus on a particular patient group, condition or clinical pathway. Or there may be a need to develop specialisms to meet people’s needs or neighbourhood/place/system priorities. Discussion around whether health and wellbeing coaches want to specialise, and the training and support they will need to do this, should be held in supervision sessions, appraisals and PDPs.
9. Supervision and evidencing capabilities
Supervisors play an essential role in supporting health and wellbeing coaches ongoing development. They should work alongside health and wellbeing coaches to set and measure goals and examine how they are improving outcomes for patients. They should also monitor how health and wellbeing coaches are meeting their competencies at various stages of their career, alongside assessing training and continuing professional development (CPD) needs.
The line management supervisor will play a key role in this process through regular meetings, appraisals and personal development plans (PDPs), and having an overview of all supervision arrangements that are in place. However, the health coaching supervisor (experienced health coach) would be an essential part of the process in ongoing assessment of a health and wellbeing coach’s coaching competencies and fitness to practise.
Health coaching and line management supervisors have a collective responsibility to assess the ongoing development and performance of a health and wellbeing coach, by assessing and providing feedback on their portfolio of evidence on a regular basis. This helps keep the role on target and in line with the priorities of the employer and ensures that there are no issues preventing the health and wellbeing coach from effectively doing their role. The health and wellbeing coach competency framework sets out how to evidence each competency and can be used as a tool to facilitate supervision conversations.
9.1 Evidence
Health and wellbeing coaches should develop a portfolio of evidence to share in supervision discussions this could include observation, client feedback and a journal of reflective practice. They should have protected time to develop their portfolio as part of their CPD.
Employers may also want to set key quality indicators for their services which include health coaching or to measure the impact of interventions. NHS England has developed information on how to use measurement within supported self-management, based on evidence and good practice, which employers may find useful.
Health and wellbeing coaches should be encouraged to record referrals and outcomes for people they see. In primary care activity linked to health and wellbeing coaching should be recorded using SNOMED code: 148471000000103 seen by health and wellbeing coach (finding).
9.2 Portfolio of evidence
The portfolio of evidence will support health and wellbeing coaches and their supervisors to evidence their knowledge, skills and behaviours. It is not a formal assessment tool, but a supportive toolkit for health and wellbeing coaches to build their reflective practice.
It provides a range of tools to help:
- evidence and reflective practice
- identify CPD needs and opportunities
- demonstrate the impact of health coaching
- demonstrate how health and wellbeing coaches can work as part of the multidisciplinary team
- support supervisors to understand health coaching.
Health and wellbeing coaches and employers are encouraged to use these tools in a way that works best for them, including agreeing frequency and use and format. Health and wellbeing coaches will find protected time to use the tools and reflect on their practice useful.
10. Career pathway
10.1 Entry to the role
There is no set career route into becoming a health and wellbeing coach. People who choose to become a health and wellbeing coach could be from a health and care background or a different sector, where they have gained the transferable skills to meet the core competencies required for the role. They may already be an experienced coach or have little coaching experience.
Health and wellbeing coaches come from diverse backgrounds and bring with them skills in many different areas, including welfare, education and supporting vulnerable communities. Employers should have an awareness of their previous experience and any additional training and support needed on employment, particularly for health and wellbeing coaches who are new to the health and care system or are less experienced.
In addition to entry routes based on prior professional experience, health and wellbeing coaching can offer a route into employment for those who may have few formal qualifications or who have lived experience. Similarly, those who take a route to employment through volunteering in community services may find that this experience offers a route into health and wellbeing coaching or similar roles. In this way, the health and wellbeing coach roles can be a powerful force in tackling inequity in employment opportunities as well as health inequalities.
A community health and wellbeing worker apprenticeship is one route into the role of health and wellbeing coaching. The purpose of a community health and wellbeing worker is to work in partnership with individuals and their communities to identify and address health and wellbeing needs, improve health, prevent ill-health and reduce inequalities. After completing the apprenticeship people may choose a career in health coaching. However, they would still need to demonstrate the necessary competencies, be committed to personalised care and have the necessary Personalised Care Institute (PCI) accredited health coaching training set out in earlier sections.
10.2 Transfer of prior experience
People may come into NHS health and wellbeing coach roles with previous experience and training. This may include counselling, wellness coaching, life coaching, sport, and executive coaching.
It should be recognised that NHS referrals and practice often involve a very different client group to that seen in private practice and some other areas of coaching. NHS referrals are often characterised by low motivation, complex health and social care needs and issues, and poor experiences of health care services. Coaches with prior coaching experience should still attend the four day PCI accredited training on joining the NHS. They will also need orientation, especially around concepts such as health literacy, self management and COM-B in relation to health conditions.
10.3 Career development
The role of health and wellbeing coach is still relatively new in the NHS and is evolving and maturing. At this stage there is no set career pathway, but the role provides an excellent entry level career in the health and care sector.
Career development conversations should form part of ongoing supervision. Tools including the competency framework and portfolio of evidence can be used to identify skills and experience that could be transferred to other roles. Health and wellbeing coaches working in primary care can also access career coaching support through the Looking after your career programme.
Websites such as NHS jobs and NHS careers are useful resources for health and wellbeing coaches who are considering their next steps.
10.4 Management and leadership roles
Line management of health and wellbeing coach teams may be a natural progression for experienced health and wellbeing coaches. Management is needed to deliver high-quality services. Managers can also have a ‘service management’ role by working to ensure health coaching is understood across individual services and the health and care system. In this management role, health and wellbeing coaches are likely to have a part in building connections across teams and organisations and advising on how the role can support targeted approaches across MDTs, using techniques such as population health management.
11. Health and wellbeing support
Health and wellbeing coaches, like clinical frontline staff, can face pressures due to juggling caseloads, managing patient needs, complex cases and personal commitments. Alongside professional development they may also benefit from personal development to build resilience and manage their wellbeing.
Health and wellbeing coaches working in primary care can access individual coaching to address issues affecting their wellbeing. Information about how to access a coach for wellbeing support is available on the Looking after you too section of the NHS England website.
All NHS employees can access staff mental health and wellbeing hubs and local support may also be available in specific services and systems. Employers should ensure that health and wellbeing coaches are aware of the health and wellbeing support available to them.
12. Useful resources
12.1 Resources about health and wellbeing coaching
- Health and wellbeing coach recruitment pack
- Health coaching guide
- ‘Better Conversation’ resources for clinicians and health and care leaders, including video, infographics and a resource guide which contains case studies, evidence and tips on how to introduce a health coaching approach to improve the quality of conversation and help patients change behaviour.
12.2 Training and CPD related resources
- Personalised Care Institute website
- Training hubs – Health Education England
- Looking after you too – NHS England
12.3 Personalised care focused resources
- Personalised care and support planning
- Shared decision making
- Social prescribing
- Care co-ordination
- Supported self-management summary guide
- Measuring supported self-management
- Personalised care, including the comprehensive model of personalised care and universal personalised care
12.4 Primary care specific resources
- Directed Enhanced Service specification
- Directed Enhanced Service guidance
- Further Directed Enhanced Service links
12.5 Professional bodies
- UK Health Coaches Association
- Association of Coaching
- European Mentoring Coaching Council
- International Coach Federation
12.6 Support for health and wellbeing coaches working in the NHS
- Looking after you too – for staff working in primary care
- Looking after your career – for staff working in primary care
- Looking after your team – for staff working in primary care
- Supporting our NHS people
- Staff mental health and wellbeing hubs
13. Appendices
13.1 Appendix 1: Evidence
Much of the existing evidence on the effectiveness of health coaching comes from studies undertaken overseas. There is compelling meta-analytic evidence which demonstrates that health coaching services have a positive impact on the outcomes for patients with chronic diseases such as diabetes, hypertension, obesity and heart disease[1]. As well as having a positive effect on patient health and wellbeing, health coaching has also been found to reduce the demand on healthcare services. For example, a large-scale randomised controlled trial conducted in Sweden demonstrated that the implementation of health coaching reduced hospitalisation rates by 12%[2].
While much of the research has been conducted overseas, the UK evidence base on the effectiveness of health coaching has been growing. Although they have typically been on a smaller scale, the UK studies provide a foundation of evidence to support the adoption of the innovation. To date, there have been three previous outcome evaluations of health coaching in the UK. The first found improvements in patient self – efficacy in a small-scale pilot in Suffolk[3]. The second explored organisational case studies as part of a large-scale pilot across the East of England region. It found that clinicians were still using the approach up to a year after their training and that they perceived reduced demands and patients responding well to the approach[4]. The third was an outcome evaluation of a small-scale application on a rehabilitation ward in Hampshire; an accompanying economic evaluation estimated an indicative cost saving of £3 million[5]. A rapid review commissioned by Health Education East of England[6] led to health coaching being selected as one of five national priorities in NHS England’s ‘Realising the Value’ programme to deliver on the Five Year Forward View.
Health coaching is associated with high practitioner and patient satisfaction, increased patient motivation to self-manage and adopt healthy behaviours, reduction of waste, improved outcomes and positive impact on the culture of services and health inequalities.
Recorded outcomes include:
- increases patient motivation to self-manage and adopt healthy behaviours
- increases adherence to medication
- improves self-efficacy and patient activation
- works best for those most in need
- can impact on outcomes such as HbA1c
- can reduce waste, for example, a reduction of 20% to 40% in readmissions, the need for residential home placements after rehab and physio follow-up appointments.
These outcomes are achieved through health coaching because informed, empowered patients have the knowledge, skills and confidence to manage their own health. They make healthier lifestyle choices and personally relevant decisions, adhere to treatment regimens, and experience fewer adverse events. Patients who possess the skills, confidence and knowledge to manage their own health use services more effectively, resulting in cost savings of 8% to 21%[7].
Health coaching skills training provides clinicians and non-clinicians an opportunity to acquire the necessary interpersonal skills to share responsibility with patients or service users and empower them to self-care and change behaviours[8].
What ‘good’ health coaching looks like may be described differently depending on your perspective and which type of health coaching is being referred to. People working within the system tend to think of health coaching as involving a similar skill set, whoever is leading the coaching conversation. However, from the perspective of the person being coached, there is an expectation that in a specialist health coaching service context there would be a higher standard of training and expertise in health coaching and supporting behaviour change. They would not expect the same level of expertise from someone trained in using health coaching as part of their usual role.
Good evidence-based health coaching can be recognised within a health and care system when there is:
- A clear articulation and evidence of the role of health coaching in the system.
- Health coaching linked to the vision, values and strategy of the organisations and system.
- A commitment by all parties to promote health coaching.
- Evaluation, data collection and measured outcomes, including those relating to wider determinants of health, for example, housing, employment.
- Adequate resources, infrastructure, time and space allocated to the delivery process and practitioners delivering health coaching.
- A system that includes health coaching in its variety of forms, for example, as an approach and a service.
- Activity linked to a bigger national picture and the comprehensive model for personalised care.
- Practitioner and leader support, and sufficient time given to specifically develop, undertake or evaluate health coaching and develop new roles.
- Consideration given by system leaders to the comprehensive model for personalised care, including how health coaching and behaviour change in supported self-management can augment other components.
13.2 Appendix 2 Health and wellbeing coach competency framework
Introduction
This competency framework has been designed to outline capabilities that health and wellbeing coaches working in primary care networks (PCNs) and other areas of the NHS require in order to provide an effective, evidence based service.
This framework is also aligned to the Core Curriculum for Personalised Care published by the Personalised Care Institute (PCI), which acts as the foundation framework for both personalised care and specific personalised care roles in primary care. The framework is divided into four competency areas:
- Professional competencies for health and wellbeing coaches.
- Skills for communication and enabling in a health coaching context.
- Knowledge of models and frameworks.
- Group work skills to support self-management and group approaches.
The competencies apply to health and wellbeing coaches at different levels of experience. There are four tiers of practice/expertise for health and wellbeing coaches:
Tier 1: Four-day PCI accredited health coaching training. Plus 50 hours coaching experience in the NHS.
Tier 2: 200 hours coaching experience in the NHS.
Tier 3: 500 hours coaching experience in the NHS.
Tier 4: 1000 hours coaching experience in the NHS.
This competency framework will assist those who employ or direct the activities of health and wellbeing coaches working in the NHS to understand the competencies they require to practise safely and effectively in their role, and how these competencies can be achieved.
This framework is aimed at health and wellbeing coaches working with adults. It focuses on the fundamental competencies of health and wellbeing coaches, regardless of the setting they work in. While the core competencies remain the same, employers should recognise that health and wellbeing coaches working in specific settings or with specific groups will need additional knowledge, skills and training. For example, those in specialist roles or working with specific groups such as young people.
1. Professional competencies for health and wellbeing coaches
The following sets out the key professional capabilities which underpin health and wellbeing coach practice. It is a useful tool to use during supervision sessions.
Competency: Contracting – understanding the importance of contracting, procedural and psychological, managing the ‘contract’, setting expectations, checking-in and spot contracting with the client and understanding the interrelationship of contracting with the client and contracting between the coach and service sponsor.
Gained through: Training – e-learning or face to face.
Evidenced by: Review of session notes by health coaching supervisor. Observation of practice.
Competency: Works within the boundaries of the health coach remit in particular where the coach may have additional specialist knowledge and expertise and awareness of when to explore referring on.
Gained through: Exploration of topic in training and supervision.
Evidenced by: Observation and line management and health coaching supervision.
Competency: Has a high level of awareness of how the beliefs of the coach may unconsciously/consciously influence the client’s goals and what is important to the client and be committed to managing potential conflicts through supervision.
Gained through: Exploration through discussion in training, peer groups and supervision.
Evidenced by: Health coaching supervision and reflective journal.
Competency: Is a reflective practitioner. Demonstrates commitment to personal and professional development through reflective practice. Understands the importance of regularly reflecting in/on/after action. Pre, during, and post client session as well as preparation for supervision, in peer learning. Use and knowledge of models of reflection.
Gained through: First six months of practice.
Evidenced by: Reflective journal, line management and health coaching supervision, facilitated peer groups.
Competency: Participates in regular supervision to develop their coaching practice.
Gained through: Ongoing.
Evidenced by: Health coaching supervision log.
Competency: Can select and apply relevant evidence-based themes and models to explore and develop their practice.
Gained through: Developed and demonstrated in first six months of practice.
Evidenced by: Health coaching supervision.
Competency: Participates in peer learning networks and is willing to demonstrate skills and receive feedback from peers.
Gained through: Ongoing.
Evidenced by: Attendance log and facilitator feedback.
Competency: Keeps up to date with and evaluates research and thinking on coaching.
Gained through: Attendance at local and national events, desk top research.
Evidenced by: Portfolio.
Competency: Ensures that the focus and purpose of the coaching relationship is to:
– Raise the awareness of the client regarding their health and wellbeing and individual responsibility and choice – pre-contemplation to contemplation of change.
– Promote client autonomy and empowerment.
Gained through: Training and first month of practice.
Evidenced by: Observation of practice and health coaching supervision. Client feedback and evaluation.
Competency: Where issues are raised that require specialist input (psychological support, specific support on diet, exercise, clinical treatment, or diagnosis) the coach promptly explores referral options and ensures timely and appropriate handover to the appropriate professional whist supporting client autonomy.
Gained through: Explored in training.
Evidenced by: All forms of supervision.
Observation does not have to be in person – a recording of a session (audio or film) can be used as evidence where a client gives permission for the session to be recorded.
The following are general capabilities and will generally be defined by an employer or legislation. They can be acquired through mandatory training for employees and recorded in the health and wellbeing coach’s portfolio.
- safeguarding for children and adults
- confidentiality and information governance
- lone working
- equality and diversity awareness
- health and safety awareness
- awareness of roles and responsibilities
- values in personalised care (as defined in universal model)
- accurate record keeping
- handling data and information
- duty of care and negligence
- domestic abuse awareness
- promote the holistic wellbeing, rights, and interests, of individuals and carers
- Mental Capacity Act awareness
- emotional resilience awareness
- promote the independence of people who use services while protecting them
- basic first aid.
2. Skills for communication and enabling in a health coaching model
Competency: Demonstrates the use of communication and enabling skills to facilitate a coaching conversation that takes into account the persons level of capability to change.
Gained through: Face-to-face training, online ‘live’ training, in practice.
Evidenced by: Practice sessions in training followed up by observed practice.
Competency: Uses active and empathic listening to develop a trusting and supportive environment and help raise individual awareness and clarity of purpose.
Gained through: Face-to-face training, online ‘live training, in practice.
Evidenced by: Practice sessions in training followed up by observed practice.
Competency: Uses effective questioning – use of open and closed questions to explore the client’s current situation and options of change.
Gained through: Face-to-face training, online ‘live training, in practice.
Evidenced by: Practice sessions in training followed up by observed practice.
Competency: Collaborative exploration of outcomes and goals, to promote change based on what is important to the client and support the client to gain insight of how health outcomes may relate to these.
Gained through: Face-to-face training, online ‘live training, in practice.
Evidenced by: Practice sessions in training followed up by observed practice.
Competency: Able to provide information where appropriate in the context of client centred generated goals/outcomes (what matters to me) – a way that promotes autotomy, increases knowledge, skills, and confidence.
Gained through: Face-to-face training, online ‘live training, in practice.
Evidenced by: Practice sessions in training followed up by observed practice.
Competency: Identifies cues of non-verbal/body language and uses the information to support the coaching relationship.
Gained through: Face-to-face training, e-learning.
Evidenced by: Evidence of training recorded in portfolio.
Competency: Follow up goals and outcomes in a way that supports increasing autonomy, motivation and change.
Gained through: Face to face training, online ‘live training, in practice.
Evidenced by: Practice sessions in training followed up by observed practice.
Competency: Builds trust and rapport.
Gained through: Face to face training, online ‘live’ training, in practice.
Evidenced by: Practice sessions in training followed up by observed practice.
Competency: Provides supportive challenge to help raise awareness of client’s current reality and explore areas of dissonance.
Gained through: Face-to-face training, online ‘live training, in practice.
Evidenced by: Practice sessions in training followed up by observed practice.
Competency: Has an awareness and understanding of how different locations, mediums (telephone, ZOOM/Teams) may impact adversely or positively on an interaction.
Gained through: e-learning, face-to-face, online ‘live’ training, self-directed learning.
Evidenced by: Evidence of work done recorded in portfolio
In practice – client hours during first 12 months under supervision.
3. Skills around models and frameworks
This section focuses on the skills that hold the process for coaches and help provide structure – coaches should be able to demonstrate the theoretical and evidence base of their approach to working.
Competency: Able to set out the boundaries and structure of the coaching conversation.
Gained through: Face-to-face training, e-learning, and self-directed learning.
Evidenced by: Practice sessions in training followed up by observed practice.
Competency: Able to find out the client’s priorities and what outcomes are important to them.
Gained through: Face-to-face training, e-learning, and self-directed learning.
Evidenced by: Observed practice and assessment in health coaching supervision, evidence of e-learning and self-directed learning via portfolio.
Competency: Can gather information that is meaningful for the client (the client’s story) (for example, use of appreciative enquiry).
Gained through: Face-to-face training, e-learning, and self-directed learning.
Evidenced by: Observed practice and assessment in health coaching supervision, evidence of e-learning and self-directed learning via portfolio.
Competency: Supports people to integrate their ideas, opinions, and perspectives into the session. Able to use appropriate frameworks to support the client to gain insight (for example, Karpman’s drama triangle, transactional analysis).
Gained through: Face-to-face training, e-learning, and self-directed learning.
Evidenced by: Observed practice and assessment in health coaching supervision, evidence of e-learning and self-directed learning via portfolio.
Competency: Increases the client’s awareness of their current situation and how they may wish their situation to be (understanding of positive psychology in health coaching).
Gained through: Face-to-face training, e-learning, and self-directed learning.
Evidenced by: Observed practice and assessment in health coaching supervision, evidence of e-learning and self-directed learning via portfolio.
Competency: Uses action planning and goal/outcome setting models – including breaking goals into achievable chunks and identifying opportunities for follow up.
Gained through: Face-to-face training, e-learning, and self-directed learning.
Evidenced by: Observed practice and assessment in health coaching supervision, evidence of e-learning and self-directed learning via portfolio.
Competency: Explores the risks, benefits, and consequences of different courses of action with the client. Discusses what these mean to the person in the context of their life and goals, supporting them to be able make a decision and/or agree the way forward together (for example, in context of COM-B model etc).
Gained through: Face-to-face training, e-learning, and self-directed learning.
Evidenced by: Observed practice and assessment in health coaching supervision, evidence of e-learning and self-directed learning via portfolio.
Competency: Supports people to self-reflect and understand the relationships and connections between their emotions, feelings, and behaviours (for example, CBT).
Gained through: Face-to-face training, e-learning, and self-directed learning.
Evidenced by: Observed practice and assessment in health coaching supervision, evidence of e-learning and self-directed learning via portfolio.
Competency: Use theoretical models to assess people’s current levels of knowledge, skills and confidence. Modifies conversations accordingly and supports people in a way that develops these factors, for example, models of health literacy, activation, self-efficacy theory.
Gained through: Face-to-face training, e-learning, and self-directed learning.
Evidenced by: Observed practice and assessment in health coaching supervision, evidence of e-learning and self-directed learning via portfolio.
Competency: Identifies an individual’s propensity to change on a particular habit – (e.g. transtheoretical theory of change or similar models).
Gained through: Face to face training, eLearning, and self-directed learning.
Evidenced by: Observed practice and assessment in health coaching supervision, evidence of eLearning and self-directed learning via portfolio.
Competency: Understands how a client’s past experiences may impact on their motivation to change (e.g. awareness of impact of unresolved trauma in relation to health major acute episodes such as cardiac failure, stroke).
Gained through: Face to face training, eLearning, and self-directed learning.
Evidenced by: Observed practice and assessment in health coaching supervision, evidence of eLearning and self-directed learning via portfolio.
Competency: Universal model of personalised care.
Gained through: PCI eLearning.
Evidenced by: Completion certificate.
4. Group work skills to support self-management and group approaches: Tier 2 and above
Competency: Understands and applies key theoretical frameworks such as social learning theory, self-efficacy theory to the group process.
Gained through: Face to face training, eLearning, and self-directed learning, in practice.
Evidenced by: Observed practice. Portfolio.
Competency: Understands group dynamics and how to manage them.
Gained through: Face to face training, eLearning, and self-directed learning, in practice.
Evidenced by: Observed practice. Client feedback and evaluation.
Competency: Understands role modelling and its use.
Gained through: Face to face training, eLearning, and self-directed learning, in practice.
Evidenced by: Practice sessions in training followed up by observed practice.
Competency: Manages conflict.
Gained through: In practice.
Evidenced by: Observed practice.
Competency: Facilitates group-based approaches to problem solving.
Gained through: In practice.
Evidenced by: Observed practice. Client feedback and evaluation.
Competency: Facilitates group-based approaches to action planning, goal setting and goal follow up.
Gained through: Face to face training, eLearning, and self-directed learning, in practice.
Evidenced by: Observed practice. Client feedback and evaluation.
5. Additional models and approaches: Tier 2 and above
The following sets out some of the key models, approaches, and frameworks that a coach should have knowledge of and use when working in the NHS. Gained through eLearning and other mediums and evidenced in their portfolio. This list may be partly determined by employers, and the particular client group or locality the coach works in. These sit in the desirable rather than essential.
- Local structures of health and social care services including an awareness of how primary care, community services, mental health services and secondary providers work in their locality, as well as how they are grouped (primary care networks, integrated care systems, social care and local authority) and voluntary sector.
- Social determinants of health.
- Health literacy.
- Cultural awareness.
- Social welfare awareness.
- Awareness of supporting bereaved individuals.
- Asset-based approaches.
- Awareness of long-term conditions, learning disability and autism, drug, and substance misuse.
- Social determinants of health assessment.
- Carer awareness.
- Prevention (primary, secondary, and tertiary).
- Multi-disciplinary team (MDT) working awareness.
- Working with community groups awareness.
- Patient activation.
- Coproduction.
- Making Every Contact Count (MECC).
- Person-centred measurement and outcomes.
- Asset based community development.
- Nutrition and weight management, health eating and physical activity awareness.
- Working with volunteers.
- Accessible Information Standard.
- Working with veterans awareness.
- Core models of behaviour change most commonly used in the NHS (COM-B, Trans theoretical model of change).
- Statutory and mandatory regulation and governance.
- Personalised care in the remote and virtual environment.
- Technology to support health and wellbeing.
- Range of consultation models used by health care professionals.
- Strategic co-production patient and public involvement.
6. Supervision
Health coaching supervision
This framework supports the development of minimum standards for health and wellbeing coach supervision.
Health coaching supervision is required for all health and wellbeing coaches. Services funded though reimbursement schemes such as the DES may have additional requirements such as a named GP. These are in addition to that set out below.
Full time health and wellbeing coaches should have supervision at least every month and access to peer learning networks.
Health coaching supervision statement: Health coaching supervisors must be able to demonstrate significant experience in application of health coaching skills within the NHS.
Minimum standard: Tier 3 practitioner.
Health coaching supervision statement: Health coaching supervisors must be able to demonstrate they recently have carried a client/patient caseload.
Minimum standard: Minimum 50 hours per year in current previous 12 months.
Health coaching supervision statement: Health coaching supervisors must be able to demonstrate experience of providing health coaching or similar (e.g. clinical) supervision in a variety of formats (e.g., face to face, 1:1 and group formats) in a variety of settings (including face to face and online environments).
Minimum standard: Provide examples of health coaching supervision undertaken either as part of a contract or part of a supervision training apprenticeship.
Health coaching supervision statement: Health coaching supervisors must be able to demonstrate that they receive regular supervision from an experienced supervisor as part of their practice and ongoing professional development.
Minimum standard: Provide records and name of health coaching supervisor. Statement from their health coaching supervisor, signed off by their health coaching supervisor. Their health coaching supervisor should have a higher level of experience.
Health coaching supervision statement: Health coaching supervisors must be able to demonstrate a capacity for self-regulation and to practise safely and effectively.
Minimum standard: Statement from their health coaching supervisor, signed off by their supervisor.
Health coaching supervision statement: Health coaching supervisors must be able to demonstrate that they are experienced in the application of relevant health coaching supervision models/theoretical frameworks and how to adapt approaches depending on the work, needs and developmental stage of the supervisee.
Minimum standard: Statement of professional practice incorporating explanation of the models they use and how they adapt to circumstances.
Health coaching supervision statement: Health coaching supervisors must be able to demonstrate an awareness of the values, beliefs and assumptions which underpin their work.
Statement of professional values, including alignment with NHS values.
Health coaching supervision statement: Health coaching supervisors must be able to show evidence of health coaching supervision training or equivalent experience.
Minimum standard: Evidence of training or statement of equivalent experience
Footnotes
[1] Sforzo, G., Kaye, M., Todorova, I., et al., 2017. Compendium of the health and wellness coaching literature. American Journal of Lifestyle Medicine, 12(6), pp.436-447.
[2] Edgren, G., Anderson, J., Dolk, A., et al., 2016. A case management intervention targeted to reduce healthcare consumption for frequent Emergency Department visitors. European Journal of Emergency Medicine, 23(5), pp.344-350.
[3] Thomas, W., 2011. Primary care health coaching evaluation report: executive summary. University College Suffolk.
[4] Carter, A., Tamkin, P. and Wilson, S., 2015. The Case for Health Coaching. Lessons learned from implementing a training and development intervention for clinicians across the East of England. Brighton: Institute for Employment Studies.orzo, G., et al., 2013. A systematic review of the literature on health and wellness coaching: defining a key behavioral intervention in healthcare. Global Advances in Health and Medicine, 2(4), pp.38-57.
[5] Kibble, S., Gray, D., Prat-Sala, M., et al., 2014. Recovery coaching in an acute older people rehabilitation ward. BMJ Quality Improvement Reports, 3(1), pp.u205646.w2316.
[6] Newman, P. and McDowell, A., 2016. Health changing conversations: clinicians ’ experience of health coaching in the East of England. Future Hospital Journal, 3(2), pp.147-151. 18
[7] Hibbard, J. and Gilburt, H., 2014. Supporting people to manage their health: an introduction to patient activation. London: The King’s Fund. http://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/supporting-peoplemanage-health-patient-activation-may14.pdf
[8] Wolever, R., Simmons, L., Sforzo, G., et al., 2013. A systematic review of the literature on health and wellness coaching: defining a key behavioral intervention in healthcare. Global Advances in Health and Medicine, 2(4), pp.38-57.
Publication reference: B1570

