Personal health budgets for mental health
The NHS long term plan made a clear commitment to expand personalised care and personal health budgets, with a specific expectation that personal health budgets will be offered within mental health services as part of plans for up to 200,000 people to benefit by 2023/24.
Personal health budgets for mental health are flexible. They can be used to meet a variety of needs:
- for ongoing care and support to meet people’s assessed health and wellbeing needs, eg aftercare services under section 117 of the Mental Health Act (1983)
- for one-off budgets to support people to achieve specific goals or outcomes enabling supported self-management e.g. hospital discharge, mental health recovery
And they can be:
- pooled, to support several individuals to achieve a common health and wellbeing goal
- integrated with social care and/or education personal budgets
- used to target and address wider system priorities such as identified health inequalities.
Personal health budgets can only be accessed following a personalised care and support planning conversation that identifies the care, support and services it will be spent on.
The extension of the legal right to a personal health budget for those eligible for aftercare services under section 117 of the Mental Health Act (1983) was, in part, a result of a national personal health budget evaluation (2014). The evaluation found that personal health budgets had positive impacts for those with mental health conditions, resulting in significant improvement to people’s quality of life and wellbeing and were cost effective.
Further guidance is available for health and social care professionals on implementing the legal rights to personal health budgets, including section 117 after-care.
Personal health budgets and the recovery model
Personal health budgets are closely aligned to one of the central strands of service transformation in mental health: recovery. As a highly personal journey, recovery depends on services being able to develop individually tailored approaches.
Personal health budgets for mental health in action
Personal health budgets for mental health can include a range of things to give people access to care, support and services that are holistic, innovative and build on their strengths. Examples include:
- Physical activities and equipment to help people manage voices, distract from paranoid thoughts, help with self-regulation and manage angry outbursts whilst also helping to develop friendships, build confidence and concentration.
- Technology that helps people develop self-management skills in a variety of settings, builds confidence and supports independence, such as sensory needs equipment.
- Digital equipment to sustain contact with friends/family, access relevant health management apps, online support and appropriate help. Digital equipment can also aid emotional regulation, self-management, the development of social interactions and prevent escalation into crisis services.
- Music/art sessions that support expression and creativity, provide distraction from symptoms, help engagement with new environments and building of relationships.
- Support with access to training and education opportunities, including essential equipment needed to support these opportunities, to build self-confidence, learn to manage anxiety and identify further education or employment opportunities.
Carers and family members have also reported that the ‘personalised support they have received had a positive impact on their life, mental health and wellbeing. They highly valued the ways the support they received was tailored to their interests and needs, with the offer of choice and flexibility in how they were supported.’ Making a Difference to Young People’s Lives Through Personalised care, National Children’s Bureau, 2021.
Positive impact of personal health budgets
 “Never underestimate the power of truly engaging with your patients and service users in deciding how and what they want their recovery journey to look like. I was moments away from a secure unit, now I’m living my dream in my own flat, having adventures, every day is a day further away from my past and a day spent realising new possibilities, opportunities. All it took was somebody to walk into my life for an hour and essentially ask me “Martha, what matters to you?”
“Never underestimate the power of truly engaging with your patients and service users in deciding how and what they want their recovery journey to look like. I was moments away from a secure unit, now I’m living my dream in my own flat, having adventures, every day is a day further away from my past and a day spent realising new possibilities, opportunities. All it took was somebody to walk into my life for an hour and essentially ask me “Martha, what matters to you?”
Read Martha’s story about how a personal health budget for s117 aftercare changed her life by logging onto the personal health pages of the Personalised Care Collaborative Platform.
A qualitative evaluation of personal health budgets for mental health by the National Development Team for Inclusion, 2020 found that personal health budgets positively impacted both the people receiving a personal health budget and the sites delivering them.
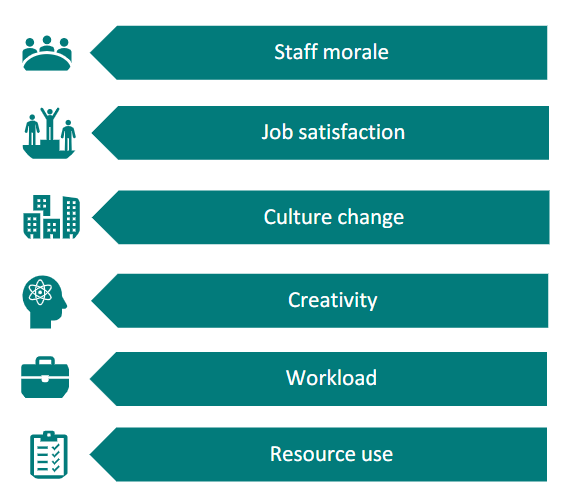
Impact on sites
“That’s the beauty of PHBs…an opportunity for people to overcome practical hurdles so they can focus on their recovery…”
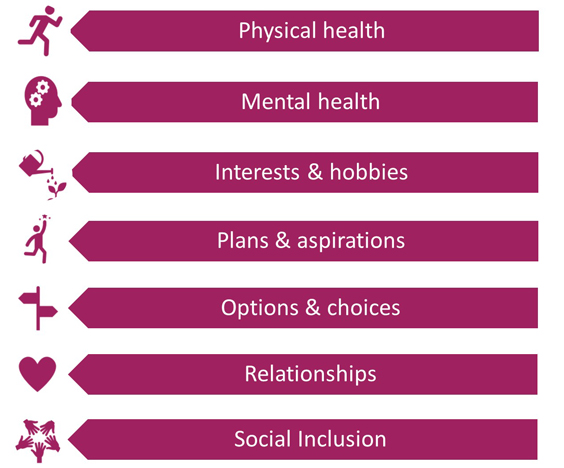
Impact on the person
“I feel positive…I have something to get up for now…it feels good.”
“Before this budget, I might not see or speak to anybody for 2 or 3 days, now there are people in and out. They treat me with respect, not like I have mental health problems. It’s a two way thing.”
Implementing personal health budgets for mental health and need more information?
If you work within the NHS, a local authority or a voluntary sector partner, you can sign up to the Personalised Care Collaborative Network to access a range of resources, share learning and discuss issues with colleagues across the country. To discuss access please email england.pccn@nhs.net.
Alternatively, for more information please see the overview of the support available for professionals, or contact the national Personal Health Budgets team by emailing england.personalhealthbudgets@nhs.net.