Summary
This Workforce development framework for care co-ordinators has been developed to:
- set clear and consistent standards for care co-ordinators
- demonstrate the benefits of care co-ordinators working in health and care
- provide information about the training, support, supervision, and continuing professional development (CPD) needed to enable care co-ordinators to succeed
- support the development of a strong and capable workforce of care co-ordinators
- support improved quality and consistency of care co-ordination and reduce variation in outcomes and access standards.
The framework includes competencies for the role and links to resources to support employers to recruit and embed care co-ordinators in services. Organisations employing care co-ordinators, including primary care networks, can use this framework to support recruitment and retention. It will help them develop a greater understanding of the role, its scope of practice and the training and development care co-ordinators need to enable them to practice safely and effectively.
Care co-ordinators are personalised care roles. They focus on what matters to individuals and support people from diverse backgrounds, including those with a range of conditions and disabilities. They co-ordinate and navigate care across the health and care system, helping people make the right connections, with the right teams at the right time. They are skilled in personalised conversations, assessing people’s needs, facilitating joint working, ensuring the effective flow of information, monitoring needs and responding to change.
Care co-ordinators work in different settings across health and care, including but not limited to primary care, hospitals and secondary care services, end of life care, children and family services, community health services and care homes. They offer significant benefits to individuals they support and the health and care system, for example freeing up clinical capacity and reducing the likelihood of the need for acute or crisis care.
As with any role in a health and care setting, care co-ordinators need to be supported and enabled to succeed in their role. Before employing a care co-ordinator employers should be clear on the purpose of the role and how it can contribute to meeting people’s needs and neighbourhood/place/system priorities.
Before taking referrals, employers should ensure that care co-ordinators have the necessary skills and training. Care co-ordinators should complete a Personalised Care Institute accredited two-day care co-ordination course – this is the minimum required training standard. They should also complete free e-learning on personalised care and support planning and shared decision making. Employers are responsible for funding any necessary training for care co-ordinators they employ.
Good supervision arrangements for care co-ordinators are crucial to ensure they practice safely and effectively. Supervisors should have a good understanding of the role of a care co-ordinator and be trained in providing supervision. Care co-ordinators should be able to discuss patient related concerns, with a member of staff who can follow up on arising issues and be supported to follow appropriate safeguarding procedures.
Care co-ordinators manage a caseload of people, which should be determined locally, based on the complexity of cases and the support needs of people and their carers. The adaptable and transferable skills of care co-ordinators mean that they can work in a specialist role or with people with a range of conditions – the core skills and competencies of the role remain the same. As does the fundamental purpose of the role – focusing on delivering personalised care.
Employers should support care co-ordinators in their CPD by giving them dedicated time, and where necessary funding, for training and CPD. Regular supervision sessions, appraisals and personal development planning should all be used as opportunities to focus on specific needs to progress and/or meet the competencies for the role. Care co-ordinators themselves, their supervisors and employers have collective responsibility for CPD.
1. Introduction
This Workforce development framework for care co-ordinators has been developed to support care co-ordinators and their employers to understand the role and set them up to deliver personalised care safely and effectively in a range of health and care settings. The framework replaces previous guidance and resources issued by NHS England about the role of care co-ordinators.
The role of care co-ordinators is developing and maturing in the health and care system and this framework is a useful resource for those who want to embed care co-ordinators in a service. It will be of particular use to:
- care co-ordinators working in health and care settings
- primary care networks, and staff working in them, employing care co-ordinators through the Additional Roles Reimbursement Scheme
- organisations employing care co-ordinators including secondary care, voluntary, community and social enterprise sector
- colleagues involved in workforce planning and redesign.
The framework sets out the core functions, skills, competencies and training needs of care co-ordinators, regardless of the setting they work in. However, employers should recognise that care co-ordinators working in specific settings or with specific groups (for example, care homes, end of life care, perioperative services, anticipatory care) will need additional knowledge, skills and training.
The framework has been developed by NHS England, in collaboration with a range of stakeholders including Health Education England. It includes information on the professional support and development care co-ordinators need to work with people to optimise outcomes. Its purpose is to:
- set clear and consistent standards for care co-ordinators
- demonstrate the benefits of care co-ordinators working in the NHS
- provide information about the training, support, supervision, and continuous professional development needed to enable them to succeed
- support the development of a strong and capable workforce of care co-ordinators
- support improved quality and consistency of care co-ordination and reduce variation in outcomes and access standards.
2. Context
The NHS Long Term Plan set out the need to make personalised care business as usual across the health and care system, committing that “people will get more control over their own health and more personalised care when they need it”.
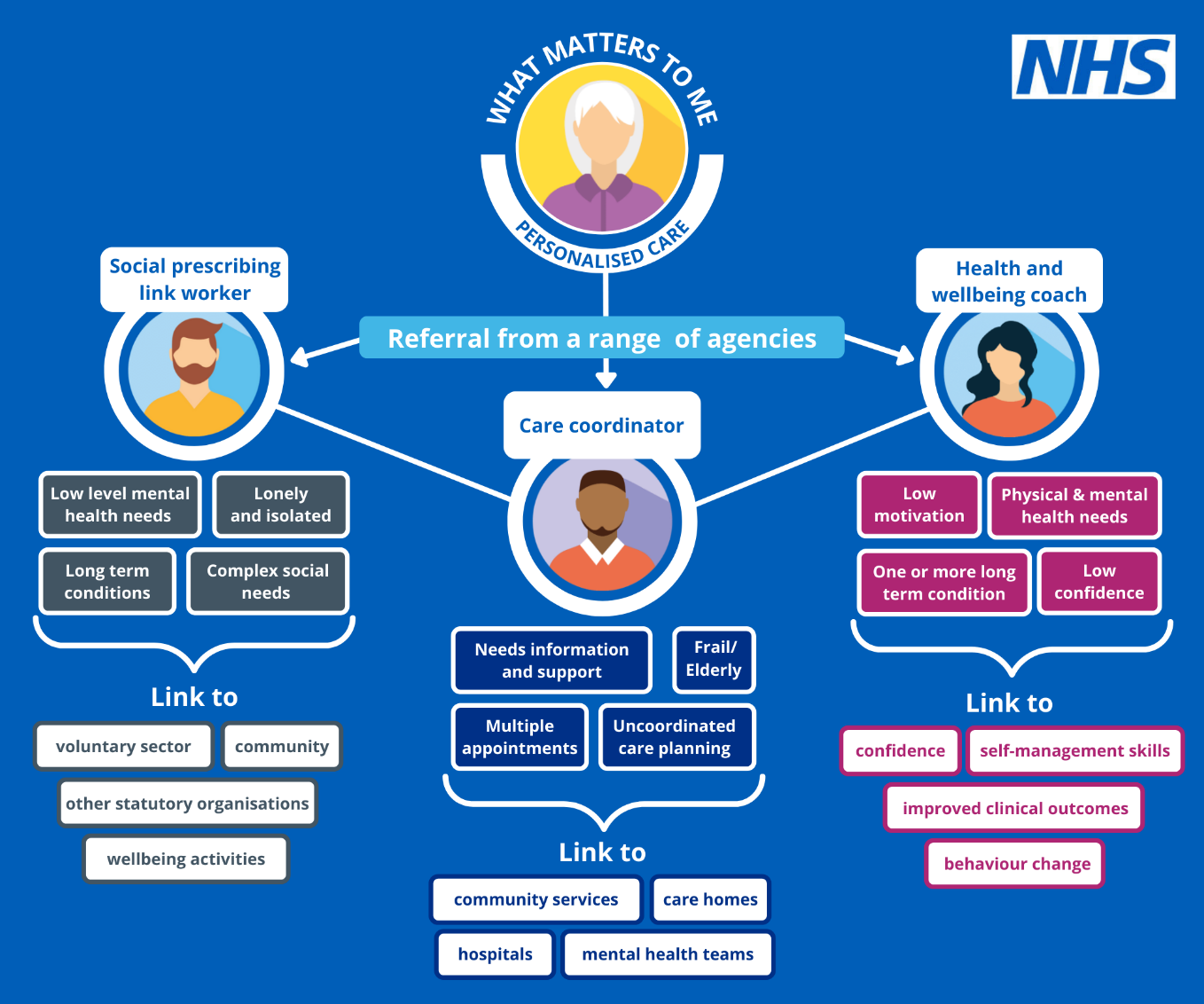
Additional complementary frameworks are available for two other personalised care roles – social prescribing link workers and health and wellbeing coaches.
3. What is a care co-ordinator?
Care co-ordinators work with people to build trusting relationships and listen to what matters to them. They work with a range of people, particularly those with long-term conditions, multiple long-term conditions, and people living with or at risk of frailty. They help people co-ordinate and navigate their care across the health and care system and can support people to become more active in their own health and care.
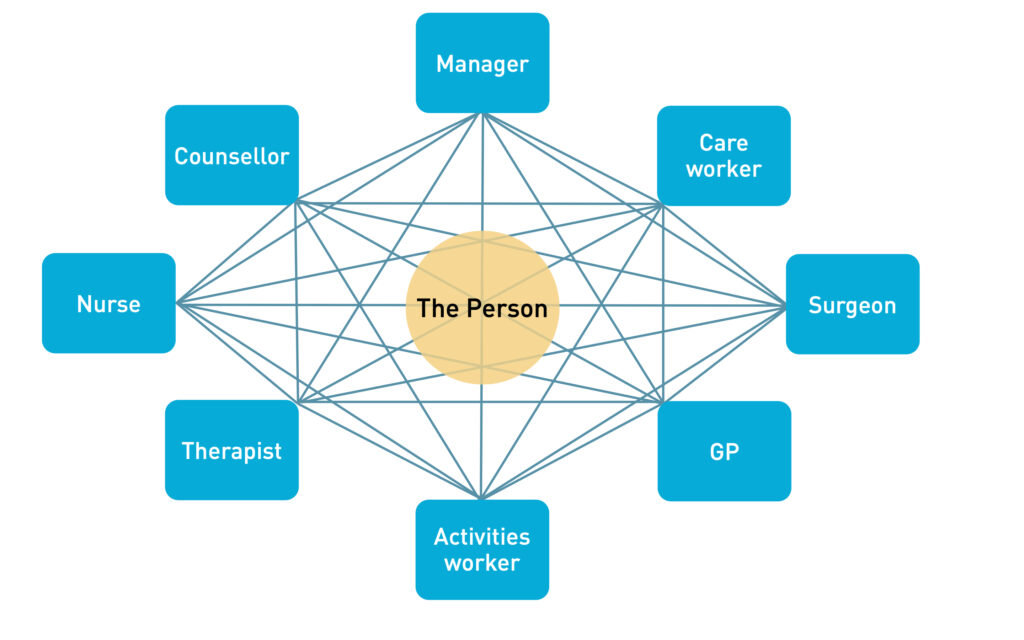
Diagram 1 (see below) highlights the complexity of navigating the health and care system. Some people may benefit from support to understand and make sense of this ‘web’ of interactions and which team/professional to get support from, including nurses, counsellors, therapist, activity workers, GPs, surgeons, care worker and managers. Care co-ordinators help people make the right connections, with the right teams at the right time.
Diagram 1: Making sense of coordinated care (Health Education England and Birmingham City University)
Care co-ordinators are at the centre of a person’s care. They walk alongside the person and are uniquely placed to see the bigger picture, from clinical care to how their social interactions support their wellbeing.
Care co-ordinators take a personalised approach and bring together all the information about a person’s care and support needs. They play a key role in personalised care and support planning and focus on the six components of personalised care. They take a holistic approach, looking at the person, rather than just the conditions they have.
They are skilled in personalised conversations, assessing people’s needs, facilitating joint working, ensuring the effective flow of information, monitoring needs and responding to change.
Care co-ordinators work in variety of settings across health and care, including but not limited to primary care, hospitals and secondary care services, end of life care, children and families services, community health services and care homes. They play a key role in multidisciplinary teams (MDTs) and wider multiagency teams, working in partnership to optimise outcomes for people and populations.
Care co-ordinators support a joined-up way of working. They can facilitate referrals and conversations to ensure timely care and access to specialists, GPs, community services etc. In many cases they play a role in the initial set up of an MDT and championing a proactive approach to people’s care. As care co-ordinators act as a single point of contact for people they are a crucial link for teams, including staff in care homes, primary care, community care and secondary care.
3. Benefits of a care co-ordinator
3.1 Benefits to people
The health and care system is complex and can be confusing and difficult to navigate, especially for those who are vulnerable, frail and/or face health inequalities. The benefits of having a care co-ordinator include:
- A named contact to go to with questions and requests for information who will check on people to see how they are doing.
- A contact who understands all of a person’s health and care needs and what is important to them.
- Support to understand the health and care system and get access to the right services and resources at the right time, for example personal health budgets.
- Reducing stress and anxiety for those who have difficulty understanding what is happening or accessing the services they need.
- Preparing people for upcoming appointments and conversations about their health and care, facilitating shared decision-making and choice.
- Advocating for people in multi-disciplinary team (MDT) meetings by highlighting what is important to them.
- Empowering and enabling people to self-manage their own care and support as much as they can (supported self-management).
3.2 Benefits to the health and care system
The skills and expertise of care co-ordinators support the health and care system by:
- Providing people with a first point of contact for in-depth conversations and follow up discussions, which can help to free up clinical staff time. For example, if their needs change or they are having issues accessing services.
- Supporting people with complex needs during consultations to assist them in articulating themselves and increase their understanding, reducing the need for follow-up clinical appointments.
- Tackling health inequalities through targeted work with specific groups identified through population health management. For example, people with long-term conditions or multiple long-term conditions.
- Providing time, capacity and expertise to support people to prepare for clinical conversations so that clinical time can be used effectively.
- Facilitating joint working and relationships across teams and organisations through MDT working.
- Reducing the likelihood of the need for acute or crisis care. For example, by supporting people who are receiving anticipatory care.
- Supporting integrated and efficient ways of working across the health and care system.
- Reducing the risk of deterioration/exacerbations with poor outcomes for people with long-term conditions through conducting long-term conditions care @home reviews, prioritising patients for follow up and providing remote structured supported self-management.
- Supporting people to wait for elective care appointments/operations and to become as well as possible leading up to any treatment or surgery, reducing the risk of treatments having to be cancelled due to health concerns.
4. Employing a care co-ordinator
As with any role in a health and care setting, care co-ordinators should be supported and enabled to thrive in their role. Employers should be clear on the purpose of the role and how it can contribute to meeting people’s needs and neighbourhood/place/system priorities, including objectives around population health management and health inequalities.
Making sense of coordinated care, produced by Health Education England and Birmingham City University, is a useful resource for organisations setting up a co-ordinated care service and includes a useful checklist for developing a co-ordinated care service.
Employers should be confident that they have the necessary resources and support to embed the care co-ordinator in the team. This includes having appropriate supervision arrangements in place, which is essential, and provision for training and ongoing continuing professional development (CPD).
A template recruitment pack has been developed and is a helpful resource for primary care networks (PCNs) and other employers that want to recruit a care co-ordinator (you will need to register for a FutureNHS account to access this template and some of the other resources referenced in this framework). It provides a job description and sets out the skills and responsibilities of the role. Appendix one includes a competency framework for care co-ordinators, which can be used to support recruitment, retention, supervision and ongoing CPD.
4.1 Training and requirements prior to taking referrals
Care co-ordinators come to the role with a wide variety of transferable skills and experiences. However, a basic level of training is needed before care co-ordinators should take referrals. This is important for all care co-ordinators to work safely and effectively, but particularly for those who have never worked in the NHS before.
Employers should ensure that care co-ordinators have the necessary skills and training before taking referrals. Training falls into two parts:
- personalised care and care co-ordination training
- induction and training specific to the setting the role is working in.
1. Personalised care and care co-ordination training
| Minimum training requirement for care co-ordinators | Source | Cost |
| Two-day accredited care co-ordinator training | Accredited training providers of this course can be found on the Personalised Care Institute website | Funded by employer – price varies depending on provider. |
|
Accredited personalised care and support plan e-learning | Personalised Care Institute website | Free |
| Accredited shared decision making e-learning | Free |
Care co-ordinators should complete Personalised Care Institute accredited training before taking referrals or at the start of their employment, if they have not done this already. Details of the minimum training requirements for care co-ordinators can be found on the Personalised Care Institute website. Two-day accredited care co-ordinator training is a minimum requirement. This course will ensure a developed understanding of the role of a care co-ordinator and where it adds value to people and the system.
In addition, care co-ordinators need to complete Personalised Care Institute accredited online learning courses. They may also find coaching skills and motivational interviewing skills training useful.
2. Induction and training specific to the setting
Care co-ordinators should complete an induction and training specific to the setting they are working in before taking referrals.
Examples of useful induction/training
- Mandatory training, including safeguarding and confidentiality.
- Training in relevant IT systems, templates and recording interventions.
- Learning about the service, or setting, to understand different roles in the multidisciplinary team, new ways of working, and how they link to the care co-ordinator.
- Information and introduction to the service, the team, partner organisations (for example, patient safety collaboratives) and the locality.
- Learning about specific patient groups or pathways, for example enhanced health in care homes (EHCH), anticipatory care, elective procedures.
- Learning about the long-term conditions care @home frameworks for cardiovascular disease prevention and respiratory, including the use of risk stratification tools.
- Priorities of the employing organisation, and how the role contributes to them.
- Policy context of the role, for example, supporting the Network Contract Directed Enhanced Service, anticipatory care, elective care, EHCH, proactive care @home etc.
- Expected outcomes and boundaries of the role.
Care co-ordinators who are new to working in health and care may also benefit from completing the Care Certificate as part of their induction to ensure they can provide a compassionate and caring service.
Care co-ordinators will need ongoing training and CPD as they continue to develop in the role. Further details on this can be found in section eight.
4.2 Supervision
4.2.1 What is supervision?
Supervision is a process whereby individual care co-ordinators are supported by someone else to meet their professional, organisational and personal objectives, which together promote best outcomes for the patient.
Supervision covers the various types of support a care co-ordinator will need to practise safely and effectively. It includes day-to-day management and clinical and professional expertise. Supervisors should have a good understanding of the level of skills and competencies a care co-ordinator has, where they are now, and what they need to do to progress. They are enablers that support good working relationships and help to address issues and celebrate achievements. They encourage reflection and ongoing development and improvement.
Health and care providers regulated by the Care Quality Commission are expected to offer staff regular supervision to ensure they are competent and confident to do their role. PCNs employing care co-ordinators through the Additional Roles Reimbursement Scheme have a contractual responsibility to provide supervision as set out in the Network Contract DES contract specification.
4.2.2 Supervision requirements
Good supervision arrangements for care co-ordinators are crucial. Supervision is key in terms of supporting care co-ordinators to excel in their role and in supporting their ongoing CPD, especially those new to the role who are less experienced.
NHS England carried out a survey of care co-ordinators working in primary care in autumn 2021 to understand their experiences. In the survey, lack of adequate supervision was cited as one of the main reasons for care co-ordinators leaving their role. Employers will have their own resources and arrangements for line management and supervision, including carrying out appraisals.
Organisations that employ care co-ordinators should have appropriate supervision arrangements in place, including a named first point of contact for general advice and support. Supervisors should be experienced members of staff with a good understanding of the role of a care co-ordinator and ideally an understanding of advanced communication skills. It is recommended that supervision should take place on a minimum of a monthly basis (for full time staff) and this could be provided by one or more named individuals. New, less experienced care co-ordinators may need more frequent supervision in the first six months as they learn about the role and the setting they are working in.
Where organisations commission care co-ordinators via a third party arrangement, for example, through a voluntary community and social enterprise sector or other partner, supervision arrangements should be agreed as part of the commissioning arrangement to ensure that appropriate supervision is in place.
Care co-ordinators should be able to discuss patient related concerns (for example, abuse, domestic violence and support with mental health) with a senior member of staff and be supported to follow appropriate safeguarding procedures. Regardless of the setting the care co-ordinator works in, it should be clear who they need to speak to in the first instance about any patient-related concerns.
PCNs employing care co-ordinators should refer to section B5.5 of the Network Contract DES contract specification for specific supervision requirements.
5. Ways of working – professional framework
5.1 Caseload
In primary care, care co-ordinators manage a caseload of people, working closely with a multidisciplinary team (MDT). There is no defined caseload expectation for the role. Caseloads should be determined locally, based on the complexity of cases and the support needs of people and their carers. Care co-ordinators should discuss caseload and any concerns around it with their supervisor(s).
Typically, a care co-ordinator’s time involves a mix of face-to-face sessions, telephone, and/or virtual sessions with people. Alongside these they will attend MDT meetings, connect with other teams and organisations and facilitate the sharing of information. Time for admin, supervision and continued professional development (CPD) should also be available.
In secondary care or other settings, the role of the care co-ordinator might work slightly differently. For example, a care co-ordinator working in a perioperative care co-ordination team might have a large number of patients in their caseload that they are in contact with every two to three months for a relatively short conversation, plus a smaller number of patients that they work more closely with.
The adaptable and transferable skills of care co-ordinators can be applied to a range of settings and people. For example. a care co-ordinator’s caseload could be made up of people living with cancer, people at risk of frailty, those with multiple long-term conditions and people with learning disabilities.
Sessions should be personalised and can vary in length and frequency. As a guide:
- they usually last around 45 minutes, often with a longer more in-depth initial session
- frequency and number of sessions is determined by the care co-ordinator and the individual – not a service specification. This does not need to be decided at first contact and can be adapted based on the ongoing needs of the person, including fluctuations in their condition, and the complexity of care co-ordination needed
- initial sessions should include developing a personalised care and support plan and setting review dates to check follow up has happened and whether needs have changed
- sessions should focus on the individual, exploring the management of their health and wellbeing in the context of their whole life and what is important to them.
It is important to encourage people to become active in their own health and care and to equip them with the knowledge, skills, and confidence to self-manage their condition, where appropriate. This will help to keep caseloads manageable and ensure capacity to accept new referrals.
5.2 Working with people
Care co-ordinators support people from diverse backgrounds, including those with a range of conditions and disabilities. They should be able to adapt their communication approach to individual needs, using plain language and culturally appropriate communication. Care co-ordinators should ensure the people they support are able to say:
- I am listened to and understood, and ‘what matters to me’ is central to all our work together.
- I am respected and treated with dignity as an individual.
- My human rights are protected, and I do not experience discrimination.
- I experience warm, compassionate, personalised care and support.
- If I raise a concern or make a complaint, it is acted on quickly.
Care co-ordinators should set clear expectations around their expertise and knowledge and how they can support the individual. This includes setting boundaries and being clear on issues around confidentiality and safeguarding. Further information related to this section can be found in the competency framework for care co-ordinators in appendix one.
5.3 Referrals to a care co-ordinator
Referrals to care co-ordinators can come from a variety of places, depending on how the service is set up. Referrals could come via clinical staff, administrative and managerial staff, voluntary community and social enterprise (VCSE) partners, or even self-referral.
Care co-ordinators can also work with colleagues to proactively target people who they feel could benefit most from their support. For example, using population health data and/or risk stratification tools to target people who are not engaged with services and/or their long-term condition is unmanaged.
5.4 Working as part of a multidisciplinary team
Multidisciplinary team (MDTs) are a group of professionals working together with a focus on the person receiving care. MDTs can be in place in primary, secondary and community settings. Working this way allows a wrap-around, holistic approach to supporting people, allowing professionals to work together to explore problems and reach shared solutions. MDTs enable a wide range of experts to work with a person, including those from health services, social care and the VCSE sector.
Care co-ordinators should be fully integrated within MDTs. They need access to other healthcare professionals, electronic ‘live’ and paper-based record systems, as well as administrative/office support and training and development.
Care co-ordinators have a unique overview of all the services and teams involved in someone’s health and care, plus the person/carer’s perspective. They can help MDTs build the right connections and understand what is important to the person receiving care. For example, bringing services together and co-ordinating them when someone is at end of life.
Care co-ordinators need to build good working relationships with colleagues in MDTs and understand each role in the team. MDT colleagues may also need an introduction to the role of the care co-ordinator. MDT working is key to enabling care co-ordinators to succeed and optimise patient outcomes.
Variability based on setting
In the case of perioperative care co-ordinators working in secondary care, they will be part of a team including consultant anaesthetists and perioperative care nurses. They will have an important role in undertaking an initial exercise to determine a person’s level of perioperative risk factors on information provided by the person and their GP. Once this assessment is completed by the perioperative care nurse, the perioperative care co-ordinator will contact all patients, arranging appointments for those assessed as being at medium or high perioperative risk.
5.5 Working with other personalised care roles
Care co-ordinators working in a primary care setting will often work closely with other personalised care roles. This includes social prescribing link workers and health and wellbeing coaches. Each role has its own unique, distinct skills and competencies that lead to improved outcomes for people.
Diagram 2 illustrates how the three roles complement each other in a primary care setting by providing a holistic personalised care approach. These roles can also be employed outside of primary care and still work in a complementary way. Information about the roles of health and wellbeing coaches and social prescribing link workers can be found on the NHS England website.
Diagram 2 – Personalised care roles in primary care
5.6 Boundaries of care co-ordinators
Care co-ordinators should focus on what is important to the patient and not be drawn into taking a prescriptive or directive approach. In primary care their role is non-clinical.
They need to be confident in their area of expertise and aware of the boundaries of their role. Boundaries are important in safely supporting people and managing the expectations of the individual and other teams involved in their care.
These issues are covered in Personalised Care Institute accredited care co-ordinator training and should be discussed during supervision and reflective practice. Supervision conversations are an ideal situation to set expectations of the role and where it starts and ends, this is especially important for care co-ordinators who are less experienced or who may not have worked in the NHS before.
Care co-ordinators will also need to be confident in spotting issues of concern, which should be discussed with a supervisor, or referred to another clinical colleague. For example, if someone is not clear about their medication or there is a safeguarding concern.
5.7 Care co-ordinators in specific settings/services
Care co-ordinators play a valuable role in a range of settings and services and can manage a varied caseload. However, in some cases care co-ordinators are employed in specific services to improve people’s outcomes and ensure they get the level of support and care they need.
Whether in a generalist or specialist role, the core skills and competencies of the role remain the same. As do the fundamental aspects of the role – focusing on personalised care and the six component parts of it:
- shared decision making
- personalised care and support planning
- enabling choice, including legal rights to choice
- social prescribing and community-based support
- supported self-management
- personal health budgets and integrated personal budgets.
However, care coordinators working in specific settings may need additional knowledge, skills, training, and specialised supervision to carry out their role effectively. As the role develops care co-ordinators are being embedded in MDTs in areas such as:
- cancer
- end of life
- learning disability
- anticipatory care
- elective care
- enhanced health in care homes
- long-term condition management
- perioperative care.
6. Values and behaviours of care co-ordinators
Care co-ordinators should believe in and be committed to the values set out in the NHS constitution, along with the principles of personalised care and focusing on what matters to the person.
There are six NHS values that all staff are expected to demonstrate:
- working together for patients
- respect and dignity
- commitment to quality of care
- compassion
- improving lives
- everyone counts
Care co-ordinators will also need to ensure their values and behaviours align with those of the organisation they are based in. It is the responsibility of the employer to communicate these with care co-ordinators through their recruitment and induction process.
7. Competency framework
A competency framework for care co-ordinators (appendix one) has been developed in collaboration with Health Education England, Birmingham City University, the Personalised Care Institute (PCI), and a range of stakeholders. It includes the core competencies needed to be a care co-ordinator and to practise safely and effectively. This framework should be used to ensure that people with the right skills and abilities are recruited to the role and as a tool to support ongoing continuing professional development (CPD).
The competency framework is aligned to the NHS England sample job description for care co-ordinators and the core curriculum for personalised care published by the PCI. It is broken down into four areas:
- personalised care
- relationships
- communication
- continuous learning
These core competencies are a foundation for all care co-ordinators from which specialist roles and competencies can be built on.
It is the employing organisation’s responsibility to ensure that it recruits people with the core competencies needed for this role and supports them to continue to develop these competencies. Employers should consider these competencies throughout the recruitment, induction and supervision process and support care co-ordinators to develop a portfolio of evidence linked to these competencies.
8. Ongoing training and continuing professional development
Continuing professional development (CPD) supports care co-ordinators to enhance and develop their personal and professional skills throughout their careers. CPD can be achieved in different ways including training, events, online learning, peer support, mentoring and action learning sets.
Employers should support care co-ordinators in their CPD and give them dedicated time, and where necessary funding, for training and CPD. Regular supervision sessions, appraisals and personal development planning should all be used as opportunities to focus on CPD and any specific needs to progress and/or meet the competencies for the role. Care co-ordinators themselves, their supervisors and employers have collective responsibility for CPD. Care co-ordinators are encouraged to develop a portfolio of evidence to share with their supervisors to help identify areas of strength and opportunities for development.
The following sections, and the competency framework in appendix one, set out training standards for care co-ordinators at various career stages. This training may be supplemented by local training offers, specific to employers, places and systems, such as training for staff working in primary care networks (PCNs) facilitated by training hubs.
If a care co-ordinator is carrying out more than one personalised care role they will need to be properly trained and supported in all functions. For example, if someone is doing both a care co-ordinator and health and wellbeing coach role, they will need to meet the competencies and training standards for both roles.
8.1 Training and continuing professional development six to12 months in post
Care co-ordinators who have been in post for several months will need ongoing support through training, along with appropriate supervision and opportunities for personal and professional development.
Training needs should be discussed in regular supervision sessions, appraisals and personal development plans, as part of ongoing CPD, and decided upon based on the individual needs of the care co-ordinator, their level of skills and experience, and the competencies set out in the competency framework in appendix one. The portfolio of evidence can be used to provide structure for conversations around CPD.
Training could include informal provision, such as attending webinars on subjects specific to the role, or formal offers via the Personalised Care Institute, training hubs, leadership for personalised care, a PCN, trust, or integrated care system. Care co-ordinators could benefit from a variety of training, including that specific to their role or the setting they are working in (for example, training on internal systems or working with local people). They may also benefit from local training provision on topics such as mental health, trauma informed care, and having difficult conversations.
Aside from training, care co-ordinators may also find peer support valuable for their personal development, for example taking part in action learning sets and/or regular peer support meetings. Job shadowing, reflective practice, group supervision, case discussions and independent reading and research are all forms of CPD too.
8.2 Specialist roles
It is important that where care co-ordinators specialise in working with a particular patient group, or condition, that they have the necessary training and are supported by an appropriate professional and service. For example, if working in cancer services a care co-ordinator may need specialist training around cancer care and will need to be part of the cancer multidisciplinary team (MDT) with access to support and appropriate guidance and supervision.
There is growing interest in the role of care co-ordinators in several specialist areas, as the value of their expertise is recognised. Key areas include:
- enhanced health in care home
- primary care networks
- elective care/My Planned Care
- Long-term conditions care @home
- perioperative care.
8.3 Supervision and evidencing capabilities
Supervisors should monitor how care co-ordinators are meeting their competencies at various stages of their career, alongside assessing CPD needs. Supervisors have oversight of the ongoing development and performance of a care co-ordinator. They assess and provide feedback on their portfolio of evidence on a regular basis. This helps keep the role on target, in line with priorities and ensures that there are no issues preventing the care co-ordinator from effectively doing their role.
8.3.1 Evidence
The care co-ordinator competency framework in appendix one sets out each competency and can be used as a tool to facilitate supervision conversations. Care co-ordinators should keep a portfolio of evidence relating to different competencies, this could include examples of work, feedback from people and colleagues and observed practice.
Employers may also set key quality indicators for their services which include care co-ordination or to measure the impact of interventions. NHS England has developed information on how to use measurement within supported self-management, based on evidence and good practice, which employers may find useful.
Care co-ordinators should be encouraged to record referrals and outcomes for people they see. In primary care activity linked to care coordination should be recorded using the following SNOMED code: 148481000000101 Seen by care coordinator (finding).
8.3.2 Portfolio of evidence
The portfolio of evidence will support care co-ordinators and their supervisors to evidence their knowledge, skills and behaviours. It is not a formal assessment tool, but a supportive toolkit for care co-ordinators to build their reflective practice.
It provides a range of tools to help:
- evidence and reflect on practice
- identify CPD needs and opportunities
- demonstrate the impact of care co-ordination
- demonstrate how care co-ordinators can work as part of the MDT
- support supervisors to understand the care co-ordinator role.
Care co-ordinators and employers are encouraged to use these tools in a way that works best for them, including agreeing frequency and use and format. Care co-ordinators will find protected time to use the tools and reflect on their practice useful.
9. Career pathway
9.1 Entry to the role
There is no set career route into becoming a care co-ordinator. People who choose to become a care co-ordinator could be from a health and care background or a different sector, where they have gained the transferable skills to meet the core competencies required for the role.
Care co-ordinators come from diverse backgrounds and bring with them skills in different areas, for example welfare, education and supporting vulnerable communities. Employers should have an awareness of their care co-ordinators’ previous experience and what additional training and support is needed, particularly for care co-ordinators who are new to the NHS.
In addition to entry routes based on prior professional experience, care co-ordination can offer a route into employment for those who may have few formal qualifications or who have lived experience. Similarly, those who take a route to employment through volunteering in community services may find that this experience offers a route into a care co-ordinator or similar role. In this way, the care co-ordinator role can be a powerful force in tackling inequity in employment opportunities as well as health inequalities.
A community health and wellbeing worker apprenticeship is one route into the role of care co-ordinator. The purpose of a community health and wellbeing worker is to work in partnership with individuals and their communities to identify and address health and wellbeing needs, improve health, prevent ill-health and reduce inequalities. After completing the apprenticeship people may choose a career in care co-ordination. However, they would still need to demonstrate the necessary competencies, be committed to personalised care and have the necessary care co-ordinator training set out in earlier sections.
9.2 Career development
The role of care co-ordinator is still relatively new in the NHS and is evolving and maturing. At this stage there is no set career pathway, but the role provides an excellent entry level career in the health and care sector.
Career development conversations should form part of ongoing supervision and tools, including the competency framework and portfolio of evidence, and can be used to identify skills and experience that could be transferred to other roles (see section eight on training and continuing professional development). Care co-ordinators working in primary care can also access career coaching support through the Looking after your career programme.
Websites such as NHS Jobs and NHS Careers are useful resources for care co-ordinators who are considering their next steps.
9.3 Management and leadership roles
Line management of care co-ordination teams may be a natural progression for experienced care co-ordinators. Management is needed to deliver high-quality care co-ordination services. Managers can also have a ‘service management’ role by working to ensure care co-ordination is understood across individual services and the health and care system. In this management role care co-ordinators are likely to have a role in building connections across teams and organisations and advising on how care co-ordinators can support targeted approaches across multidisciplinary teams, using techniques such as population health management.
10. Health and wellbeing support
Care co-ordinators, like clinical frontline staff, can face pressures due to juggling caseloads, managing patient needs, complex cases and personal commitments. Alongside professional development they may also benefit from personal development to build resilience and manage their wellbeing.
Care co-ordinators working in primary care can access individual coaching. Information about how to access a coach for wellbeing support is available on the Looking after you too section of the NHS England website. Team coaching is also available.
All NHS employees can access staff mental health and wellbeing hubs and local support may also be available in specific services and systems. Employers should ensure that care co-ordinators are aware of the health and wellbeing support available to them.
11. Useful resources
11.1 Resources about care co-ordination
- Making sense of co-ordinated care (Health Education England and Birmingham City University)
- Care co-ordinators recruitment pack
11.2 Training and continued professional development related resources
11.3 Personalised care focused resources
- Personalised care and support planning
- Shared decision making
- Social prescribing
- Care co-ordination
- Supported self-management summary guide
- Measuring supported self-management
11.4 Primary care specific resources
- Network Contract Directed Enhanced Service – contract specification
- Network Contract Directed Enhanced Service guidance
- Further Network Contract Directed Enhanced Service resources
11.5 Support for care co-ordinators working in the NHS
- Looking after you too – for staff working in primary care
- Looking after your career – for staff working in primary care
- Looking after your team – for staff working in primary care
- Supporting our NHS people
- Staff mental health and wellbeing hubs
12. Appendix 1 – Competency framework for care co-ordinators
Core competency: Personalised care
Personalised care
Personalised care is a way of thinking and doing things that sees the people using health and social services as equal partners in planning, developing and monitoring care to make sure it meets their needs and demands. This means putting people and their families at the centre of decisions and seeing them as experts, working alongside professionals to get the best outcomes. Personalised care is about considering what matters to people, their values, family situations, social circumstances and lifestyles; seeing the person as an individual and working together to develop appropriate solutions.
Key components
- Comprehend that effective personalised care and support planning requires several discussions.
- Take into account what matters to people as well as their expressed needs.
- Emotional support involving family and friends.
- Provide care that is timely, appropriate, and effective for treating health problems.
Assess needs
Determine the patient’s co-ordination needs, including working with the person’s key clinician around areas such physical, emotional, and psychological health; functional status; current health and health history; self-management knowledge and behaviours; current treatment recommendations, including prescribed medications; and need for support services.
Align resources with patient and population needs
Within the care setting, assess the needs of patients and populations and allocate health care resources according to those needs. At the population level, this includes developing system-level approaches to meet the needs of particular patient populations. At the patient level, it includes assessing the needs of individual patients to determine whether they might benefit from the system-level approach.
Core competency: Relationships
Establish accountability or negotiate responsibility
Make clear the responsibility of participants in a patient’s care for a particular aspect of that care.
The accountable entity (whether a health care professional, care team, or social care organisation) will be expected to answer for failures in the aspect(s) of care for which it is accountable.
Specify who is primarily responsible for key care and co-ordination activities, the extent of that responsibility, and when that responsibility will be transferred to other care participants.
Facilitate transitions
Facilitate specific transitions that occur when information about, or accountability for, some aspect of a patient’s care is transferred between two or more care entities or is maintained over time by one entity. Facilitation may be achieved through activities designed to ensure timely and complete transmission of information or accountability.
Create a proactive plan of care, a personalised care and support plan (PCSP)
Establish and maintain a plan of care, jointly created and managed by the patient/family and health care team, which outlines the things that matter to the patient, their current and longstanding needs and goals for care and/or identifies co-ordination gaps.
The plan is designed to fill gaps in co-ordination, establish patient goals that focus on what the patient wants to change or achieve in relation to their needs and, in some cases, set goals for the patient’s providers. Ideally, the care plan anticipates routine needs and tracks current progress toward patient goals.
Monitor, follow up, and respond to change
Jointly with the patient/family, assess progress toward care and co-ordination goals outlined in the PCSP. Monitor for successes and failures in care and co-ordination. Refine the PCSP as needed to accommodate new information or circumstances and to address any failures. Provide necessary follow-up care to patients.
Support self-management goals
Tailor education and support to align with patients’ capacity for and preferences about involvement in their own care. Education and support include information, training, or coaching provided to patients or their informal caregivers to promote patient understanding of and ability to carry out self-care tasks, including support for navigating their care transitions, self-efficacy, and behaviour change.
Building and sustaining professional relationships
Relationships underpin effective inter-boundary working and are skills people in co-ordination roles need to develop. The ability to engage and sustain key working relationships is fundamental to work with patients, their family and with multidisciplinary team members.
Core competency: Communications
Communications
Share knowledge among participants in a patient’s care. Communication may occur through a wide variety of channels.
Four overarching themes:
- Frequent communication: frequent communication helps to build relationships through the familiarity that grows from repeated interaction.
- Accurate communication: the effective co-ordination of work depends not only on frequent and timely communication, but also on accurate communication.
- Problem solving communication: task interdependencies often result in problems that require joint problem solving. Hence, effective co-ordination requires that participants engage in problem solving.
- Timely communication: Communication can be frequent and still be of poor quality. For one thing, it can lack timeliness. In co-ordinating highly interdependent work, timing can be critical.
Making sure communication takes place in a way that meets the patient’s information and decision making needs.
Interpersonal communication
The give-and-take of ideas, preferences, goals, and experiences through personal interactions. Examples include face-to-face interactions, telephone conversations, email, and letters.
Information transfer
The flow of information, such as medical history, medication lists, test results, and other data, from one participant in a patient’s care to another.
Link to community resources
Provide information on the availability of and, if necessary, co-ordinate services with additional resources available in the community that may help support patients’ health and wellness or meet their care goals. Community resources are any service or programme outside the health and care system that may support a patient’s health and wellness.
Enabling and signposting to digital health and wellbeing
Provide information on the availability of digital and online services that may help support a patients’ health and wellness or meet their care goals. Digital and online resources are any applications, digital services or programmes that may support a patient’s health and wellness.
Teamwork focused on co-ordination
Integration among separate health and care entities participating in a particular patient’s care (whether health care professionals, care teams, or other care organisations) into a cohesive and functioning whole capable of addressing patient needs.
Handling data and information
Accurate and accessible information and data underpins effective care navigation. Failures in communication between organisations, sectors and patients/carers can lead to disjointed and poor care. Individuals who work to provide effective care navigation need to be able to appropriately use relevant electronic records, databases to access, input, store and retrieve information. Data is also important for service evaluation improvement.
Core competency: Continuous learning
Continuous learning
The ability to demonstrate reflective practice, based on the best available evidence and to assess and continually improve the services delivered as an individual provider and as a member of an interprofessional team.
- Participate in practice-based learning and improvement activities that involve investigation and evaluation of patient experiences, evidence, and resources.
- Apply new technical and information/knowledge to practical use on the job.
- Regularly engage in interdisciplinary training for staff.
- Regularly engage in continued professional development.
- Implement and routinely monitor patient safety standards.
- Identify evidence to inform practice and integrated care.
People who are in care co-ordinator roles learn significantly through experience and working within local contexts – therefore reflection on practice, for the individual and as teams, is of core importance to personal as well as service development.
Professionalism
These are rooted in the ethical, moral and legal aspects of care and support, grounded in the principles of personalised care. Commitment to develop expertise, self-awareness, limitations of scope of practice and working with integrity are some important features.
Digital health IT-enabled co-ordination
Using tools, such as electronic medical records, patient portals, or databases, to communicate information about patients and their care between health care entities (health care professionals, care teams, or health care organisations) or to maintain information over time.
Publication reference: B1571

