How to make shared decision making happen
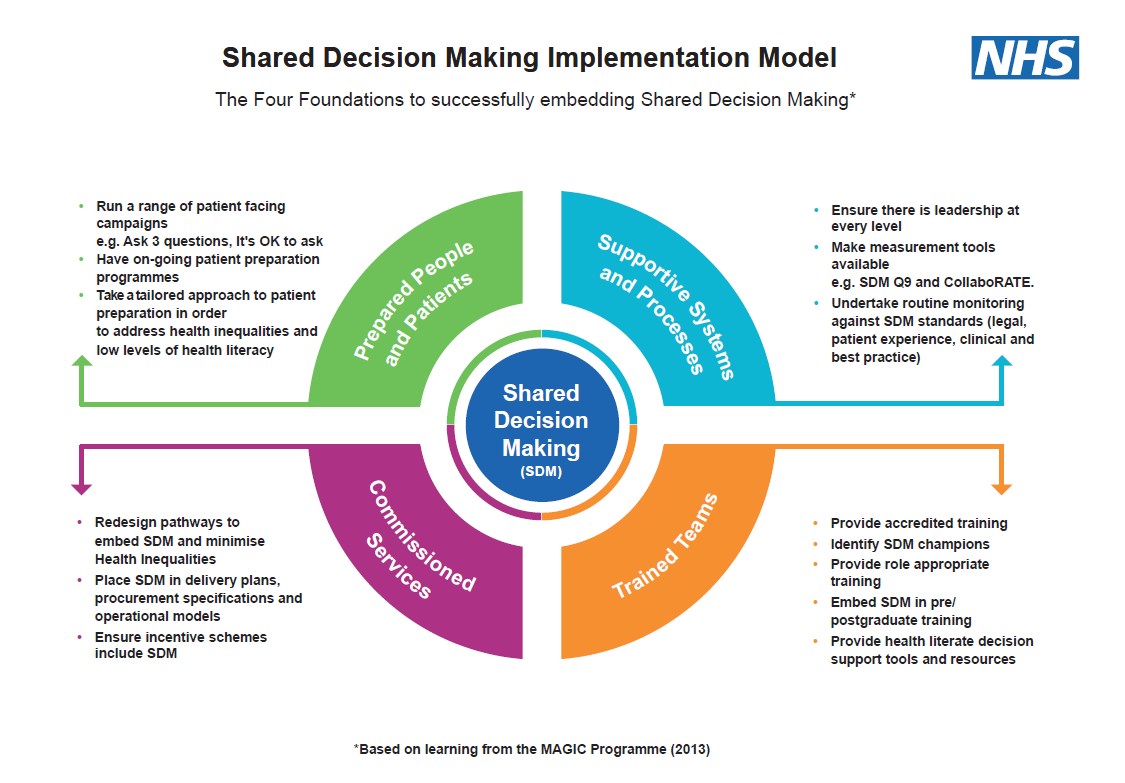
Shared decision making requires:
- shifts in culture and systems
- strong executive and clinical leadership
- appropriate training programmes with clinicians demonstrating they are putting learning into practice
- prepared and supported individuals
- commissioners understanding what shared decision making is and demonstrating how it is included in local incentives, delivery and improvement plans, pathway redesign and assurance.
In order to support the implementation of shared decision making, NHS England has developed a CQUIN scheme for 2022/23 (page 30). This covers all of the specialised services commissioned by NHS England.
Shared decision making – common challenges
There are so many reasons in favour of shared decision making, with policies and national publications supporting it, so why is it still not happening consistently across the health and care system? A number of challenges still exist about shared decision making.
Challenge 1: It takes too much time
A Cochrane review of patient decision aids suggested that using these to facilitate shared decision making increased the consultation time by 7.5%. However, optimal shared decision making improved communication, information sharing and risk assessment, thereby helping patients feel more satisfied with their choices, knowledge base, and decisions. Optimal shared decision making also helps to reduce repeat appointments, therefore, saving time in the long run.
Challenge 2: We don’t have the right tools
There are numerous tools available including:
- Personalised Care Institute:
- introductory shared decision making module
- health literacy techniques i.e. Teachback
- NHS England:
- Winton Centre
- risk communication training
- health coaching/motivational interviewing
- The National Institute for Health and Care Excellence
Challenge 3: Patients don’t want it
Patients have long been saying that they want to be more involved than they currently are in making decisions about their own health and health care (Care Quality Commission Inpatient Survey 2020; GP Patient Survey 2022; Community Mental Health Survey 2021).
Shared decision making in surgery: A scoping review of the literature (July 2020) concludes that “Shared decision making in surgery decreases decisional conflict, anxiety and surgical intervention rates, while increasing knowledge retained decisional satisfaction, quality and physician trust. Surgical patients also appear to prefer shared decision making paradigms. Shared decision making appears beneficial in surgery and therefore worth promoting and expanding in use.”
Challenge 4: We can’t measure it
- Patient reported experience measures such as CollaoRATE, SURE and SDM-Q-9.
- 5 clinical codes (SNOMED CT) that exist for shared decision making that all primary care clinicians can use.
- Objective observer-based outcome measures such as Observer OPTION 5 used by a third observer to capture the decision making process between a patient and a healthcare professional.
Challenge 5: We do it already
The Montgomery judgement states that clinicians now have to take “reasonable care to ensure that the patient is aware of any material risks involved in any recommended treatment and of any reasonable alternative or variant treatments”. The definition of what constitutes material risk has changed from the Bolam test of “responsible body of medical men” to “a reasonable person in the patient’s position”. Material risk is subjective so clinicians cannot determine it alone but must assess each case on an individual not generalised basis.