NRLS to LFPSE Transition Report (January 2021 to December 2024)
1 National Patient Safety Data Context
1.1 Transition of recording systems
NHS England previously published official statistics, using patient safety incident data from the National Reporting Learning Service (NRLS), in the National Patient Safety Incident Reports (NaPSIR) and Organisation Patient Safety Incident Reports (OPSIR). Additionally, we published monthly summary data which complemented those publications. The last official statistics using NRLS data were published in October 2022.
The Learn from Patient Safety Events (LFPSE) service, which has been operating since July 2021, has fully replaced NRLS, which was decommissioned on 30th June 2024 due to its ageing infrastructure. You can read more about LFPSE here. During the transition, we paused the production of official statistics.
Transition of all NHS secondary care providers from NRLS to LFPSE was completed in 2024. We resumed publishing data on patient safety events in April 2025 as official statistics in development using LFPSE data.
Although connection to the LFPSE service is now a contractual obligation, LFPSE operates as NRLS did in terms of being a largely voluntary recording system. Decisions on which events to record are not mandatory, except where recording a death or instance of severe harm fulfils mandatory notification requirements. Providers are encouraged to record as much useful information as possible for national learning.
This publication presents data on patient safety incidents recorded by healthcare organisations in England from January 2021 to December 2024. The data presented in this report was extracted on 28 January 2026.
1.2 Differences between NRLS and LFPSE recording systems
NRLS submissions required manual extract and upload, whereas LFPSE submissions occur in real time, including any updates made to records after their initial submission as the provider works towards a full and accurate picture of the event over time.
NRLS used older definitions and was primarily used by secondary care providers, due to its reliance on secondary-use data inputted to Local Risk Management System (LRMS) software, which varies from provider to provider. LFPSE offers an interface for providers without LRMS software to use the same tools, making it more accessible to primary care and other settings. Anyone can record a patient safety event on the service: they may be healthcare staff from any NHS or private provider, patients, or members of the public.
LFPSE captures patient safety event types beyond incidents: outcomes of concern, risks to patient safety, and instances of good care. Throughout this report, however, we will be using patient safety incidents only, which constitute the vast majority of patient safety events recorded to LFPSE, given that additional event types could not be explicitly recorded in NRLS.
Manual upload of incidents to NRLS implied that incidents occurred in the organisation that was recording to the platform. In contrast, LFPSE makes a distinction between the organisation providing the care where an incident takes place and the organisation that records the incident. As such, there are instances where a healthcare organisation records an incident that did not occur under their care, or where they record an incident on behalf of another organisation. Throughout this report, we specify whether figures are calculated based on recorder or occurring organisation.
LFPSE still uses the same levels of harm as in NRLS (with the exception of deaths now being called fatal), although the definitions have been clarified particularly to distinguish between low and moderate, and moderate and severe harm. However, we acknowledge that there will always be some level of subjective interpretation of harm when recorders are assessing an incident.
The NRLS and LFPSE datasets are different by design, and we expect to see differences in recording patterns and usage through the transition period and beyond. This is also true for LFPSE taxonomies (question set and answer options), as the taxonomies used within LFPSE will be updated to capture further details of how things go wrong, to enable development of targeted interventions to improve safety where they are likely to be most effective.
2 Data quality information
2.1 Interpreting the data
National data collected by both NRLS and LFPSE recording systems comes mainly as a secondary use from what is recorded by staff into local risk management systems (LRMSs). Currently, most records we hold have been submitted by NHS acute providers. This means that the recording systems do not, and cannot, provide the definitive number of patient safety events occurring in the NHS. Instead, the systems measure the number of safety events recorded. The number of recorded safety events has increased year on year, which likely reflects improved recording culture and accessibility, and must not be interpreted as the NHS becoming less safe. Data principles setting out how LFPSE data can and cannot be used are available here.
2.2 Anonymisation
LFPSE records that have been submitted with person identifiable information and are yet to be anonymised will not appear in this data. Records that have been submitted, and subsequently updated, that contain person identifiable information, and are yet to be re-anonymised, will be displayed as their previous version in this data until anonymised.
2.3 Incidents occurring in England
NRLS received submissions from Welsh organisations until April 2022 and we have observed sporadic Welsh records in LFPSE as well. Welsh incidents represented 1.2% of all incidents submitted to NRLS from January 2021 to December 2024 (i.e., 92,666 incidents). These incidents were submitted mostly by local health boards and the Welsh ambulance service. The equivalent figure for LFPSE was 948 incidents, distributed across pharmacies, local health boards, and a social care provider. Incidents from the Welsh head-quartered, social care provider might have occurred in England, but their incidents remain matched to Wales until we complete verification work. We have excluded all possible Welsh records, so this report presents trends that occurred in England only.
Additionally, we have removed incidents where the country of occurrence was unclear, either because no organisation code was attached to the incident, or because the code and name assigned did not allow inference of the country accurately. In NRLS, there were 2,109 incidents missing an organisation code, whereas in LFPSE there were 86,017 incidents missing both an occurring and a recording organisation code; this is a known data quality issue that we are working on resolving. Furthermore, 38 LFPSE incidents were excluded because it was not possible to determine in which country the incident occurred based on the code and name associated with the record. These exclusions comprised 1.2% of all NRLS and 2.7% of all LFPSE data recorded between January 2021 to December 2024.
2.4 Missing values
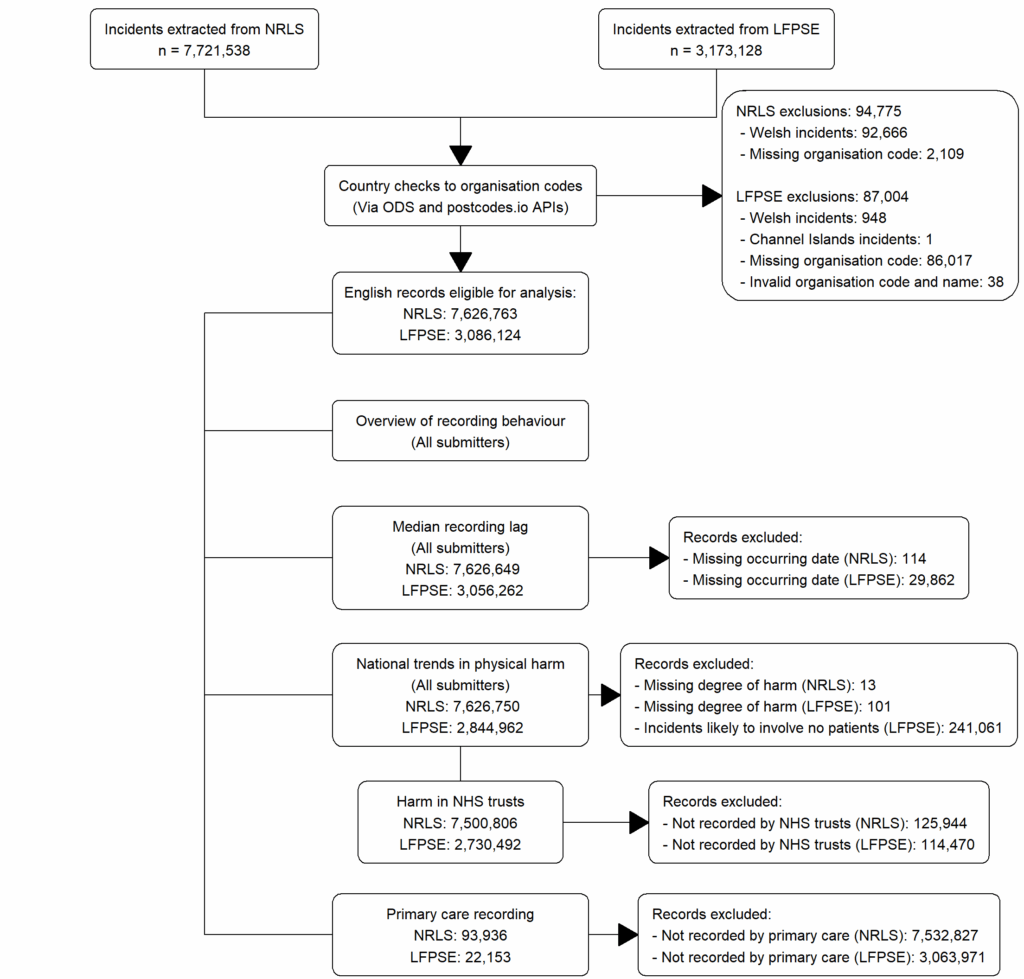
In addition to the exclusion based on country, other missing values have been handled and removed from tables and plots, so total counts will vary across sections of the report. The figure below presents a summary of the data extraction procedure and analysis undertaken for this report.
Figure 1: Transition report data pipeline
Based on incidents occurring in England and recorded between January 2021 to December 2024.
3 Overview of recording behaviour
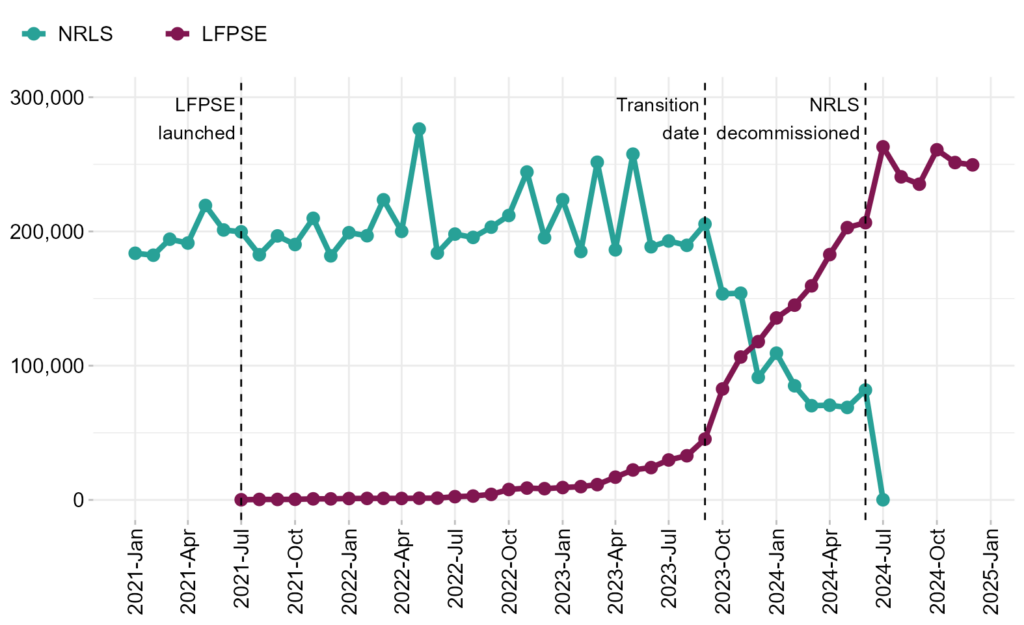
Submission of safety incidents to LFPSE began in July 2021, as early adopters of LFPSE and organisations using e-Forms in NRLS began using the new system. Nonetheless, NRLS held the majority of all incidents submitted to NHS England until September 2023, ranging from 81.9% to 100% of all incidents recorded. Thereafter we observed a consistent increase in LFPSE records and a subsequent decline in NRLS submissions, as organisations transitioned to LFPSE. Incidents recorded to LFPSE overtook those reported to NRLS by December 2023, and transition of all NHS trusts to LFPSE was completed in July 2024.
Figure 2: Total patient safety incidents recorded per month in NRLS and LFPSE
This plot illustrates the transition of patient safety incident recording from NRLS to LFPSE. Based on incidents occurring in England and recorded between January 2021 to December 2024.
Table 1: Total patient safety incidents recorded per month in NRLS and LFPSE
This table presents the number of patient safety incidents recorded to NRLS and LFPSE per month. Based on incidents occurring in England and recorded between January 2021 to December 2024.
| Month of Reporting | Count of NRLS Incidents | Count of LFPSE Incidents |
|---|---|---|
| 2021-Jan | 183,756 | – |
| 2021-Feb | 182,312 | – |
| 2021-Mar | 194,215 | – |
| 2021-Apr | 191,355 | – |
| 2021-May | 219,370 | – |
| 2021-Jun | 201,101 | – |
| 2021-Jul | 199,725 | 116 |
| 2021-Aug | 182,680 | 367 |
| 2021-Sep | 196,676 | 366 |
| 2021-Oct | 190,257 | 446 |
| 2021-Nov | 209,807 | 792 |
| 2021-Dec | 181,820 | 778 |
| 2022-Jan | 199,084 | 1,036 |
| 2022-Feb | 196,825 | 1,122 |
| 2022-Mar | 223,588 | 1,171 |
| 2022-Apr | 200,064 | 1,081 |
| 2022-May | 276,300 | 1,265 |
| 2022-Jun | 183,903 | 1,326 |
| 2022-Jul | 198,032 | 2,425 |
| 2022-Aug | 195,557 | 2,873 |
| 2022-Sep | 203,216 | 4,119 |
| 2022-Oct | 211,897 | 7,754 |
| 2022-Nov | 244,274 | 8,822 |
| 2022-Dec | 195,360 | 8,376 |
| 2023-Jan | 223,640 | 9,208 |
| 2023-Feb | 185,053 | 9,895 |
| 2023-Mar | 251,566 | 11,391 |
| 2023-Apr | 186,301 | 16,948 |
| 2023-May | 257,594 | 22,311 |
| 2023-Jun | 188,598 | 24,080 |
| 2023-Jul | 192,892 | 29,764 |
| 2023-Aug | 189,666 | 32,898 |
| 2023-Sep | 205,523 | 45,323 |
| 2023-Oct | 153,529 | 82,670 |
| 2023-Nov | 153,983 | 106,451 |
| 2023-Dec | 91,312 | 117,909 |
| 2024-Jan | 109,311 | 135,561 |
| 2024-Feb | 85,024 | 145,098 |
| 2024-Mar | 70,199 | 159,471 |
| 2024-Apr | 70,541 | 182,771 |
| 2024-May | 68,889 | 202,855 |
| 2024-Jun | 81,858 | 206,547 |
| 2024-Jul | 110 | 263,055 |
| 2024-Aug | – | 240,693 |
| 2024-Sep | – | 235,220 |
| 2024-Oct | – | 260,839 |
| 2024-Nov | – | 251,330 |
| 2024-Dec | – | 249,601 |
Preliminary analysis suggests that most organisations transitioning to LFPSE continued to submit to NRLS after their transition date. Further analysis will be needed to examine the extent to which this was dual reporting of the same incidents, versus overlapping reporting of different incidents. Note that the datasets are primarily textual, and there is no direct linkage between the two.
4 Recording lag
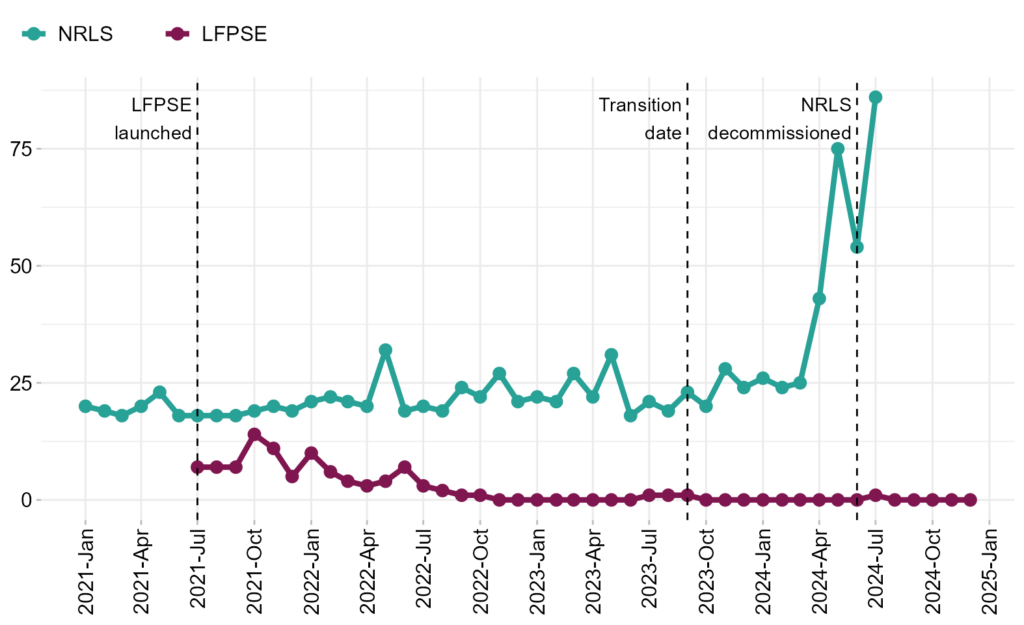
Recording lag for patient safety incidents is measured as the difference in the number of days between the date the incident occurred and the date that it was recorded to the national system. The median lag is then taken to minimise the effect of any outliers (such as events which only become apparent many years after occurring).
From January 2021 to April 2024, the national median lag for recording into NRLS ranged between 18 to 32 days. From May 2024, median lag increased noticeably, as the NRLS share of all incidents recorded dropped from 25.4% to 0. Inversely, the national median lag in LFPSE ranged between 1 to 14 days until October 2022, when LFPSE share of all incidents recorded ranged between 0.4% to 3.5%. From November 2022, the national recording lag in LFPSE consistently remained at 0 days. This reduction is due to the live nature of LFPSE, replacing the requirement for providers to manually extract and upload data as was the case for NRLS.
Between January 2021 to December 2024, there were 114 NRLS incidents without an occurring date and for which median lag could not be calculated. The equivalent figure for LFPSE was 29,862 incidents, of which 28,803 had an estimated occurring date. There is currently low confidence in the data quality of estimated occurring dates, and as such, they were not used in median lag calculations.
Figure 3: Monthly median recording lag, in days, for incidents submitted to NRLS and LFPSE
Based on patient safety incidents occurring in England and recorded between January 2021 to December 2024.
The aggregate data displayed below can be downloaded from this file:
5 Recording patterns of physical harm
LFPSE has a new variable for grading of the psychological harm associated with patient safety incidents. This is an experimental field which seeks to explore if responses to safety incidents need to be different if psychological harm is considered separately from physical harm, rather than rolling them together into one measure, as was done in NRLS. Currently, there is low confidence in the grading of psychological harm, as users familiarise themselves with its use, and as such, it is excluded from this report.
Grading the degree of physical harm to a patient resulting from a patient safety incident can be a challenge for recorders, but by grading patient safety incidents, healthcare providers can ensure consistency and comparability of data. This field is also used in the triage of records for national clinical review, ensuring the most severe harms are prioritised.
Sometimes a problem in care can affect more than one patient, or none at all. To capture this, as a new feature of LFPSE, recorders can submit information for multiple patients per incident, meaning there can be multiple degrees of harm per incident. We have aggregated LFPSE figures based on the highest physical harm level recorded per incident.
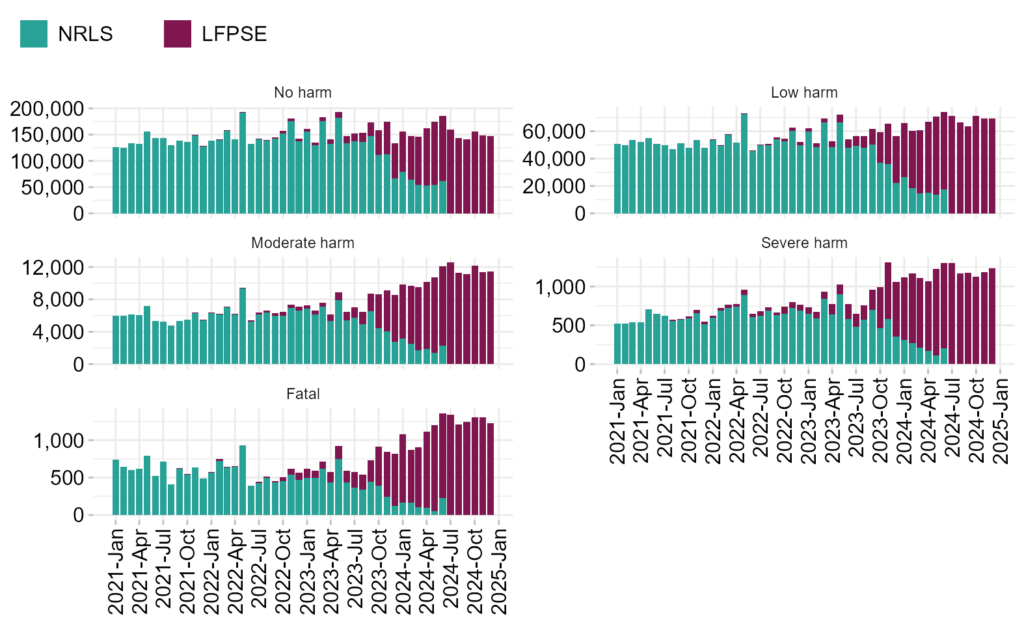
As expected with the overall increase in incident recording observed during the operational life of NRLS, we observed increased recording of incidents, for all degrees of physical harm, following transition to LFPSE. NRLS held most incidents submitted to NHS England from January 2021 until September 2023 (table 1). The monthly average of incidents recorded spanning that period of NRLS data is presented in table 2. The LFPSE figures shown for comparison are based on data from July 2024 until December 2024 (i.e., after withdrawal of NRLS and transition of all NHS trusts to LFPSE). Data recorded between October 2023 to June 2024 was not included in table 2 because incident recording was effectively split between systems, as submitters were transitioning from NRLS to LFPSE (figure 2).
Table 2: Monthly average number of incidents recorded to NRLS and LFPSE, by degree of harm, during periods of recording system dominance
Based on patient safety incidents occurring in England and recorded between January 2021 to September 2023 (for NRLS) and between July 2024 to December 2024 (for LFPSE).
| Degree of physical harm | NRLS monthly average | As percentage (NRLS) | LFPSE monthly average | As percentage (LFPSE) | Percent change |
|---|---|---|---|---|---|
| No harm | 144,163 | 70.6% | 149,026 | 64.3% | 3.4% |
| Low harm | 52,780 | 25.8% | 68,544 | 29.6% | 29.9% |
| Moderate harm | 6,160 | 3.0% | 11,660 | 5.0% | 89.3% |
| Severe harm | 642 | 0.3% | 1,199 | 0.5% | 86.9% |
| Fatal | 558 | 0.3% | 1,273 | 0.5% | 128.0% |
| Note: Averages are based on periods of system dominance. Data recorded between October 2023 to June 2024 was not included |
The increase in incident recording was not seen proportionally across all physical harm levels. The most noticeable increases in monthly incident recording, following full transition to LFPSE, were observed in moderate harm, severe harm, and fatal incidents (table 2). Given the fact that the data is mostly voluntary, and degree of harm can be subjective, it is unlikely that this represents a real increase in harm occurring during patient safety incidents. There are many possible alternative explanations for this, including but not limited to:
- NRLS was subject to harm corroboration prior to data being available due to its manual upload procedure, as opposed to the current LFPSE live system (although submitters can still revise their records).
- Generally less accurate coding of patient safety incidents in LFPSE compared to NRLS, which may be due to users being unfamiliar with the new system, or staff who are new to using LFPSE.
- De-prioritisation of recording no and low harm incidents in LFPSE compared to NRLS, which may or may not be impacted by the Patient Safety Incident Response Framework (PSIRF).
- Change in the makeup of organisation types submitting to LFPSE compared to NRLS, and the experience of the staff using LFPSE.
Despite the observed increases, the majority of incidents submitted to NHS England continued to record minor physical harm. Between January 2021 to December 2024, most incidents submitted to NRLS and LFPSE recorded low or no physical harm to patients (96.5% in NRLS vs. 93.7 % in LFPSE). We excluded 13 NRLS incidents and 241,162 LFPSE incidents from these calculations as there was no degree of harm recorded against the incident. In the excluded LFPSE group, we identified 241,061 incidents where the number of patients affected was unknown. Preliminary analysis suggests that these records likely represent incidents with no patients involved. We will continue further data quality checks to validate these figures.
Figure 4: Patient safety incidents by degree of physical harm across NRLS and LFPSE
Based on patient safety incidents occurring in England and recorded between January 2021 to December 2024.
The aggregate data displayed below can be downloaded from this file:
5.1 Physical harm in NHS trusts
The CSV file below contains the number of patient safety incidents recorded by NHS trusts in NRLS and LFPSE, broken down by degree of physical harm and month of recording, to retrospectively complete the gap in publications during the transition period. We are publishing data recorded by these organisations as they comprise the majority of incidents recorded between January 2021 to December 2024. These data have not been adjusted to reflect organisational changes (e.g., mergers and acquisitions). Quoting any figures from this file should consider and state this caveat. We aim to publish a revised version of this report to address this, and we will consider adding rates of recording to account for provider activity.
The NHS trusts aggregate data can be downloaded from this file:
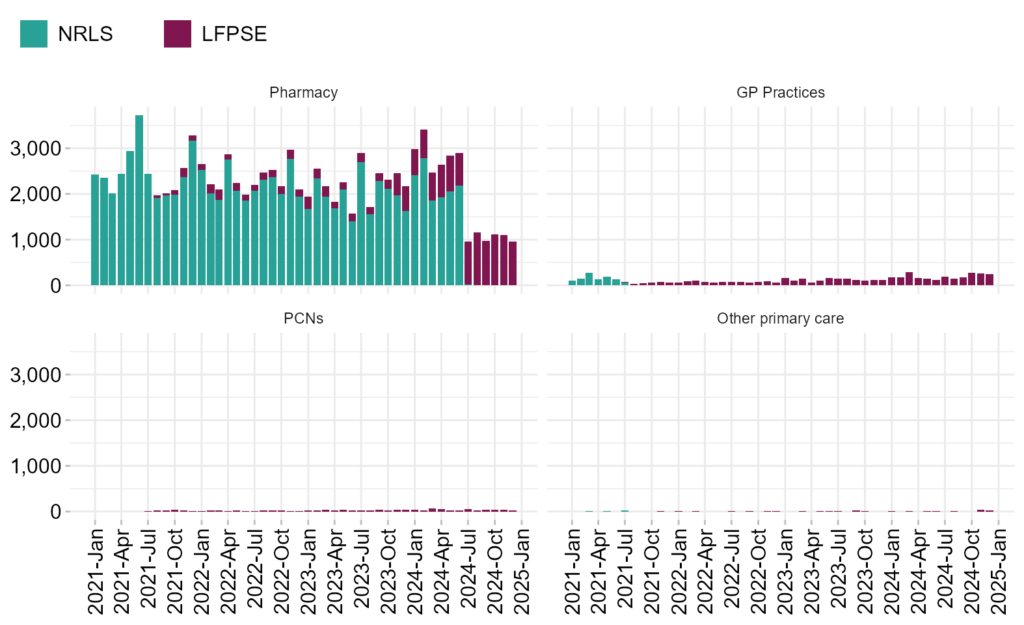
6 Primary care recording
As a proportion of all recording into both NRLS and LFPSE, incidents from primary care represented a small volume of all incidents recorded between January 2021 to December 2024. In LFPSE, there were 22,153 primary care incidents, which accounted for 0.7% of all LFPSE incident recording. The equivalent for NRLS was 93,936 primary care incidents, which represented 1.2% of all NRLS incident recording.
Most primary care incidents submitted to either system were recorded by pharmacies. There were 92,865 pharmacy incidents recorded in NRLS, which comprised most NRLS primary care recording (98.9%). Albeit smaller, the recording of incidents by primary care organisations in LFPSE showed a greater variety of submitters. Incidents recorded by pharmacies (i.e., 15,739) accounted for 71.0% of all LFPSE primary care recording, which was followed by incidents recorded by general practitioner (GP) practices (22.6%), primary care networks (PCNs, 5.3%), and other primary care providers (1.1%).
Table 3: Primary care recording in NRLS and LFPSE by organisation type
Based on patient safety incidents recorded between January 2021 to December 2024 and recorded by English healthcare organisations.
| Organisation type | NRLS incidents | As percentage (NRLS) | LFPSE incidents | As percentage (LFPSE) |
|---|---|---|---|---|
| Pharmacy | 92,865 | 98.9% | 15,739 | 71.0% |
| GP Practices | 1,029 | 1.1% | 4,999 | 22.6% |
| Other primary care | 42 | 0.0% | 239 | 1.1% |
| PCNs | – | – | 1,176 | 5.3% |
| Total | 93,936 | 100% | 22,153 | 100% |
Note: ‘Other primary care’ is a category assigned to an organisation by LFPSE and its broad nature requires further validation. We will likely break this category down in the future, after checking organisation codes in this group using NHS England’s Organisation Data Service (ODS), as we have done for pharmacies, GP practices, and PCNs.
Connection to LFPSE is a contractual obligation for both pharmacies and GP practices. However, recording is not mandatory except for severe harm and fatal incidents. Out of the 10,434 open pharmacies in England, 3,930 had an account in LFPSE as of December 2024, and we received at least one incident from 64.5% of them (i.e., 2,535 registered pharmacies). Out of the 6,267 GP practices in the country, there were 2,192 registered in LFPSE and we received incidents from 44.8% of registered practices (i.e., 982). Lastly, from the 1,299 PCNs in England, 584 had registered with LFPSE by December 2024 and we received incidents from 44.2% of them (i.e., 258 registered PCNs). We are currently working on releasing the detailed list of primary care organisations registered in LFPSE as part of our quarterly patient safety event reports.
The introduction of LFPSE has brought patient safety incident recording from new organisation types which did not record, or recorded low volumes, to NRLS. However, we have also observed a decrease in volumes of records received from pharmacies. Although the LFPSE online form was available to pharmacies from July 2021, the majority of pharmacies were using Local Risk Management Systems (LRMS) and therefore transitioned to LFPSE much later, when NRLS was decommissioned in mid-2024. GP practice recording remains broadly comparable to NRLS levels, with further scope for improving future recording rates.
Figure 5: Patient safety incidents recorded by primary care organisations to NRLS and LFPSE
Based on patient safety incidents recorded between January 2021 to December 2024 and recorded by English healthcare organisations.
The aggregate data displayed below can be downloaded from this file:
7 Feedback
This report is intended as a stand-alone document to provide answers to commonly asked questions, and we are open to revising it should demand arise. We also intend to incorporate some of these measures into our regular LFPSE patient safety events data publications. Your feedback is welcome on the format and utility of this document, so that we can provide reports that are of most benefit. Please contact patientsafety.analysis@nhs.net with any suggestions.
The analysts with overall responsibility for this report are:
Joshua Mutio
Lead Analyst
Patient Safety, Medical Directorate Programmes
Data & Analytics
NHS England
Juan Sebastian Gonzalez-Martinez
Analyst
Patient Safety, Medical Directorate Programmes
Data & Analytics
NHS England
Matthew Webb
Analytical Officer
Patient Safety, Medical Directorate Programmes
Data & Analytics
NHS England