Quarter 3 2024/25 (October to December 2024)
Patient Safety Incident Data Quarterly Publication
1. National Patient Safety Data Context
1.1. Transition of recording systems
NHS England previously published official statistics using National Reporting Learning Service (NRLS) patient safety incident data: the National Patient Safety Incident Reports (NaPSIR), and Organisation Patient Safety Incident Reports (OPSIR). In addition, we published monthly summary data which complemented our official statistics data reports.
However, due to its aging infrastructure, NRLS was withdrawn on 30th June 2024, and replaced by the Learn from Patient Safety Events (LFPSE) service, which has been operating since July 2021. You can read more about the new service here. Transition of all secondary care providers from the old system to the new completed in 2024. This is the first publication of official statistics in development relating to LFPSE, and as a result there are some key differences between NRLS and LFPSE which should be considered when interpreting this data. The change contributes significantly to the alteration of data output in our new official publications.
NRLS submissions required manual extract and upload, whereas LFPSE submissions occur in real time, including any updates made to records after their initial submission as the provider works towards a full and accurate picture of the event over time.
NRLS used older definitions, and was primarily used by secondary care providers, due to its reliance on secondary-use data inputted to Local Risk Management System (LRMS) software, which varies from provider to provider.
LFPSE offers an interface for providers without LRMS software to use the same tools, making it more accessible to primary care and other settings, as well as supporting submissions from private healthcare providers.
LFPSE also captures four distinct event types: patient safety incidents, outcomes of concern, risks to patient safety, and instances of good care. For all tables except for table 1 we will be using just the incidents.
This means that NRLS and LFPSE data are not comparable, and we expect to see differences in recording patterns and usage through the transition period and beyond. This is also true for the taxonomies, as the taxonomies used within LFPSE have been updated to capture more mechanistic details of how things go wrong, to allow us to develop targeted interventions to improve safety where they will be most effective.
However, LFPSE operates as NRLS did, in terms of being a largely voluntary system. The same caution should be applied when interpreting data which represents the numbers of events recorded, and not the number of incidents that occurred. Full Data Principles setting out LFPSE data can and cannot be used are available here.
1.2. Patient Safety Incident Definition
We use the LFPSE definition of a patient safety incident: ‘something unexpected or unintended has happened, or failed to happen, that could have or did lead to patient harm for one or more person(s) receiving healthcare’. Full details of the definitions and harm gradings are available here.
2. Data quality information
2.1. Interpreting the data
National data collected by LFPSE comes mainly as a secondary use from what is recorded by staff into local risk management systems (LRMS). Currently NHS acute providers submit most reports we receive. However, anyone can record a patient safety event on the service: they may be healthcare staff from any NHS or private provider, patients or members of the public. LFPSE data is submitted voluntarily to foster openness and encourage continual increases in reporting. This means LFPSE data does not, and cannot, provide the definitive number of patient safety incidents occurring in the NHS; it measures the number of safety events recorded. The number of recorded safety events has increased year on year, which likely reflects improved recording culture and cannot necessarily be interpreted as the NHS becoming less safe. This document serves as a quarterly snapshot of the data currently held in LFPSE.
2.2. Missing values
Missing values have been handled and removed from the tables and plots, so the total counts will vary across tables.
2.3. Cleansing
Records that have been submitted with patient identifiable information and are yet to be anonymised will not appear in these data. Records that have submitted and subsequently updated that contain patient identifiable information, and are yet to be re-anonymised, will be displayed as their previous version in these data until anonymised.
2.4. Event Types
A feature of LFPSE is that reporters can upload more than just incidents, reporters can now also upload risks, outcomes, instances of good care, and incidents. This is to ensure the database contains more instances of care that the healthcare system can learn from instead of only detailing errors involving patients.
Table 1: Count of the Event Types in LFPSE
Based on patient safety event records from October 2024 to December 2024.
| CL001 – Event Type | Number of Events | Percentage |
|---|---|---|
| Incident | 788,185 | 96.45% |
| Good care | 12,679 | 1.55% |
| Risk | 10,439 | 1.28% |
| Outcome | 5,867 | 0.72% |
| Total | 817,170 | – |
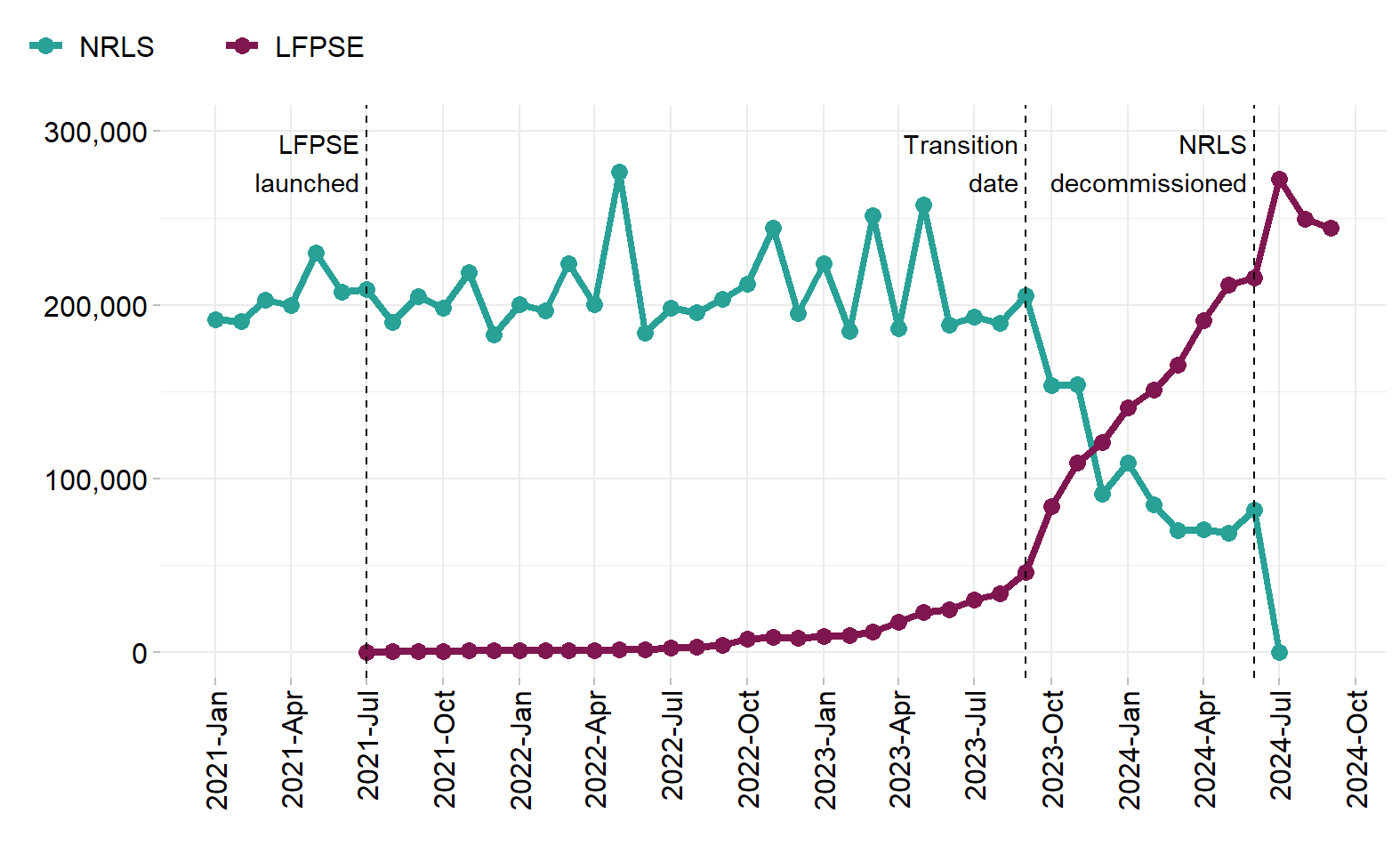
Figure 1 is plotting just the ‘incidents’ event type
Figure 1: Total patient safety incidents reported per month for the NRLS and LFPSE
This plot illustrates the recording transition of patient safety incidents from the NRLS to LFPSE. Based on patient safety incident records from January 2021 to September 2024.
| Month of Reporting | Count of NRLS Incidents | Count of LFPSE Incidents |
|---|---|---|
| 2021-Jan | 191,701 | NA |
| 2021-Feb | 190,761 | NA |
| 2021-Mar | 202,676 | NA |
| 2021-Apr | 199,960 | NA |
| 2021-May | 229,785 | NA |
| 2021-Jun | 207,684 | NA |
| 2021-Jul | 209,125 | 159 |
| 2021-Aug | 189,866 | 524 |
| 2021-Sep | 204,842 | 548 |
| 2021-Oct | 198,414 | 565 |
| 2021-Nov | 218,778 | 957 |
| 2021-Dec | 183,078 | 865 |
| 2022-Jan | 200,231 | 1,128 |
| 2022-Feb | 196,875 | 1,241 |
| 2022-Mar | 223,588 | 1,307 |
| 2022-Apr | 200,089 | 1,178 |
| 2022-May | 276,300 | 1,393 |
| 2022-Jun | 183,903 | 1,417 |
| 2022-Jul | 198,032 | 2,592 |
| 2022-Aug | 195,557 | 3,016 |
| 2022-Sep | 203,216 | 4,220 |
| 2022-Oct | 211,897 | 7,875 |
| 2022-Nov | 244,274 | 8,952 |
| 2022-Dec | 195,360 | 8,483 |
| 2023-Jan | 223,640 | 9,322 |
| 2023-Feb | 185,053 | 10,024 |
| 2023-Mar | 251,566 | 11,718 |
| 2023-Apr | 186,301 | 17,411 |
| 2023-May | 257,594 | 22,903 |
| 2023-Jun | 188,598 | 24,739 |
| 2023-Jul | 192,892 | 30,431 |
| 2023-Aug | 189,666 | 33,715 |
| 2023-Sep | 205,523 | 46,278 |
| 2023-Oct | 153,529 | 84,247 |
| 2023-Nov | 153,983 | 109,348 |
| 2023-Dec | 91,312 | 121,114 |
| 2024-Jan | 109,311 | 140,903 |
| 2024-Feb | 85,024 | 150,899 |
| 2024-Mar | 70,199 | 165,199 |
| 2024-Apr | 70,541 | 191,178 |
| 2024-May | 68,889 | 211,372 |
| 2024-Jun | 81,858 | 215,386 |
| 2024-Jul | 110 | 272,474 |
| 2024-Aug | NA | 249,460 |
| 2024-Sep | NA | 244,261 |
3. Recording patterns by physical harm
3.1. Psychological Harm
LFPSE has a new variable for grading of the psychological harm associated with the reported patient safety incidents. This is an experimental field which seeks to explore if responses to safety incidents need to be different if psychological harm is considered separately from physical harm, rather than rolling them together into one measure (as was done in the NRLS). Currently, there is low confidence in the grading of psychological harm, as users familiarise themselves with its use, and as such, it is excluded from this analysis.
3.2. Physical Harm
Grading the degree of harm to a patient resulting from a patient safety incident can be a challenge for reporters, but by grading patient safety incidents according to the harm they cause patients, local organisations can ensure consistency and comparability of data. This consistent approach locally will enable LFPSE to compare, analyse and learn from data nationally. This grading can also be used to “triage” incidents for review both locally and nationally, ensuring the most serious events are looked at first.
3.3 Harm policy
For more information on harm grading please see the harm grading policy guidelines.
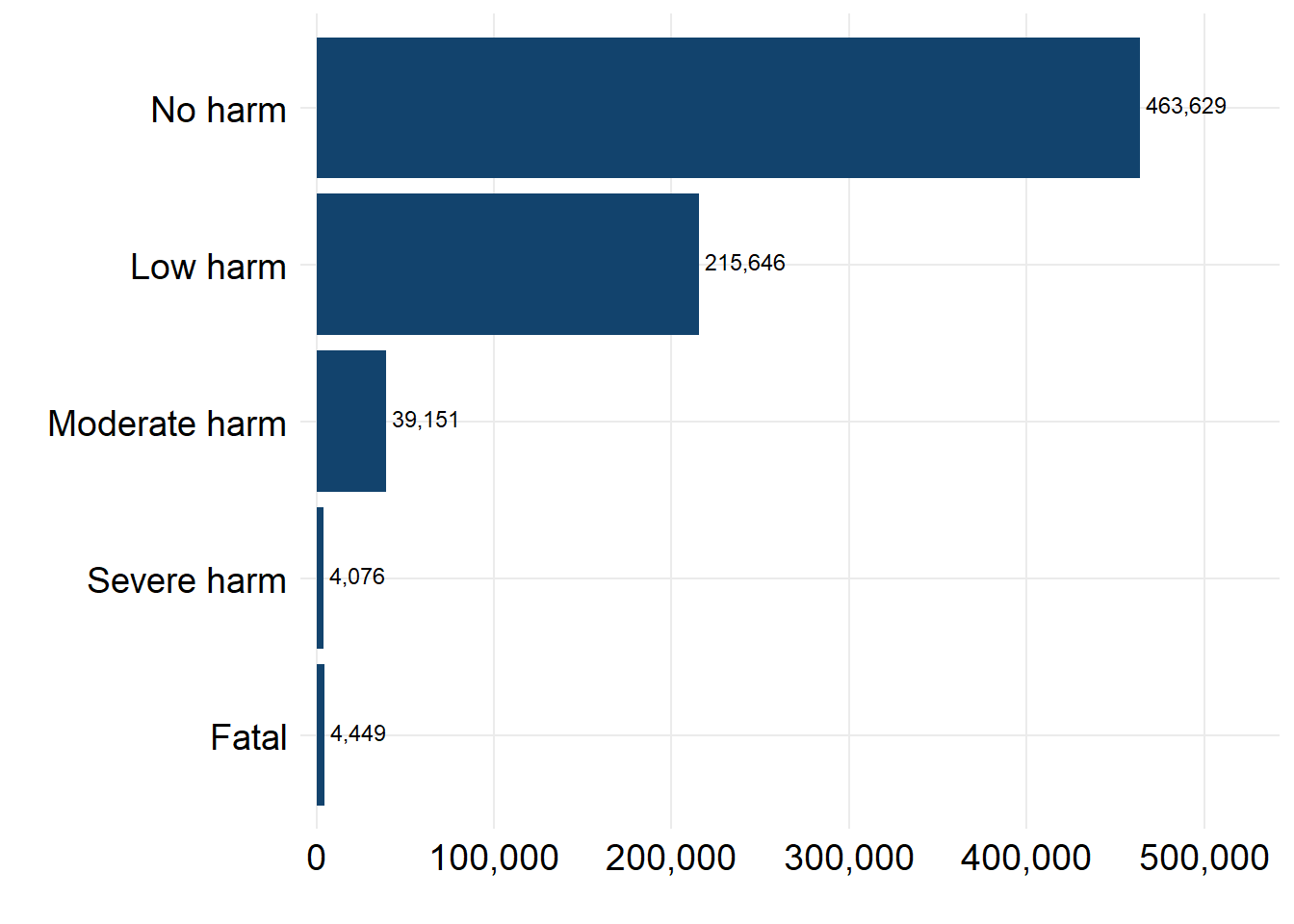
Sometimes a problem in care can affect more than one, or no patients. To capture this, a new feature of LFPSE is that recorders can submit information for multiple patients per incident, meaning there can be multiple degrees of harm per incident. For the following figure and table we have taken the highest harm level per incident.
Figure 2: Count of patient safety incidents by maximum physical harm
Based on patient safety incidents records from October 2024 to December 2024.
Table 3: Count of patient safety incidents by maximum physical harm
Based on patient safety incidents records from October 2024 to December 2024.
| OT001 – Maximum level of physical harm | Count of Reported Incidents | Percentage |
|---|---|---|
| No harm | 463,629 | 63.78% |
| Low harm | 215,646 | 29.66% |
| Moderate harm | 39,151 | 5.39% |
| Severe harm | 4,076 | 0.56% |
| Fatal | 4,449 | 0.61% |
| Total | 726,951 | – |
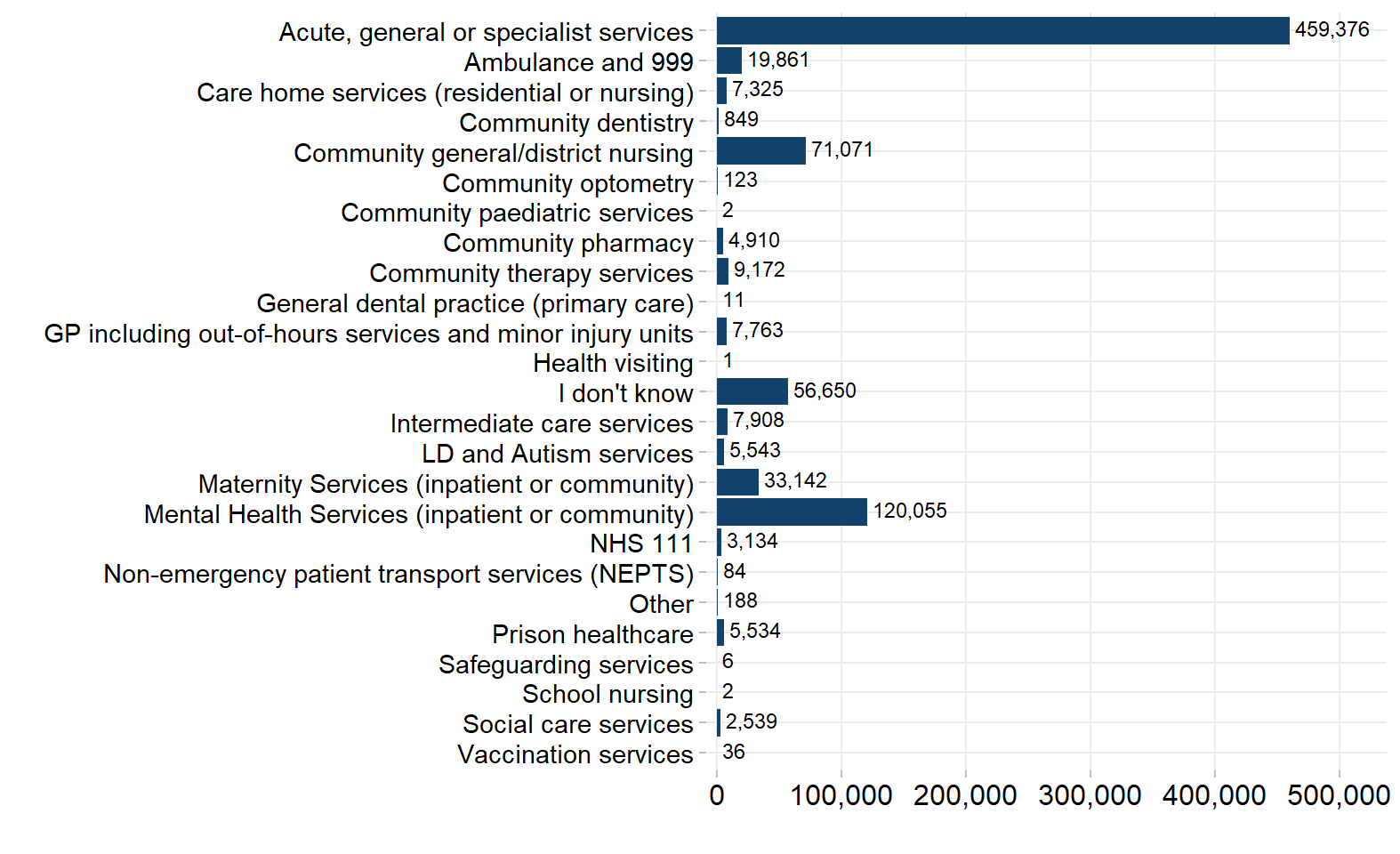
4. Recording by service area
LFPSE taxonomy (question set, and answer options) is periodically updated based on the insight/value they provide as well as ’data capture and user experience. This means there will be some variability between the data captured under different versions. In the plot below, we have grouped some granular categories into broader service groups to account for differences in the recording of service areas between version 5 (used by the majority of the LRMS users) and version 6 (used in the online forms).
- ‘Maternity inpatient services’, ‘Maternity community services’ and ‘Maternity services (inpatient or community)’, have been coalesced to ‘Maternity Services (inpatient or community)’
- ‘Mental health community services’, ‘Mental health services (inpatient or community)’ and ‘Mental health inpatient services’, have been coalesced to ‘Mental Health Services (inpatient or community)’
- ‘GP including out-of-hours services and minor injury units’, ‘GP including out-of-hours services’ and ‘Minor injury unit (MIU) / Urgent treatment centre’, have been coalesced to ‘GP including out-of-hours services and minor injury units’
The service area variable can contain multiple responses if the incident occurred in more than one area, as a result some incidents will be counted more than once making the total for this section look greater than other sections.
Figure 3: Count of incident records by service area
Based on patient safety incidents records from October 2024 to December 2024.
5. Future publications
For the next iteration of this report due to be published on 15th May 2025 we will aim to include organisation-level data along with the current tables and figures. Your feedback is welcomed on the format, frequency and utility of this document, so that we can provide reports that are of most benefit. Please contact patientsafety.analysis@nhs.net with any suggestions.