Martha’s Rule Programme July 2025
Please note that this data has been published as management information.
1 Background
Martha’s Rule is a patient safety initiative to support the early detection of deterioration by ensuring the concerns of patients, families, carers and staff are listened to and acted upon.
It has been developed in response to the death of Martha Mills and other cases related to the management of deterioration. Central to Martha’s Rule is the right for patients, families and carers to request a rapid review if they are worried that their or their loved one’s condition is getting worse and their concerns are not being responded to. The three core components of Martha’s Rule are:
- Patients will be asked, at least daily, about how they are feeling, and if they are getting better or worse, and this information will be acted on in a structured way.
- All staff will be able, at any time, to ask for a review from a different team if they are concerned that a patient is deteriorating, and they are not being responded to.
- This escalation route will also always be available to patients themselves, their families and carers and advertised across the hospital.
Martha’s Rule can work alongside existing physiological scoring systems to increase the sensitivity of identifying and responding to acute deterioration.
Further information about Martha’s Rule and its implementation can be found here.
This report provides analysis of submissions to the Martha’s Rule Data Collection from September 2024 to July 2025. This data relates to phase 1 pilot sites within NHS acute trusts across England.
2 Response rate
Table 1: Number of valid submissions each month and response rate. The number of valid submissions excludes the submissions that had to be removed due to data quality issues (see Data quality notes). The number of phase 1 pilot sites changed in July 2025 because one organisation moved from reporting once across two sites to reporting once for each site.
| Date | Number of valid submissions | Number of phase 1 pilot sites | Response rate (%) |
|---|---|---|---|
| Sep-24 | 144 | 147 | 98% |
| Oct-24 | 144 | 147 | 98% |
| Nov-24 | 141 | 147 | 96% |
| Dec-24 | 142 | 147 | 97% |
| Jan-25 | 142 | 147 | 97% |
| Feb-25 | 143 | 147 | 97% |
| Mar-25 | 144 | 147 | 98% |
| Apr-25 | 144 | 147 | 98% |
| May-25 | 142 | 147 | 97% |
| Jun-25 | 140 | 147 | 95% |
| Jul-25 | 142 | 148 | 96% |
3 Summary
The key figures for the Martha’s Rule Programme data across NHS England from September 2024 to July 2025 are:
- In total, 5,583 Martha’s Rule escalation calls have been received.
- The highest percentage of calls came via the family/carer escalation process (72%).
- 2,277 (41%) Martha’s Rule escalation calls related to acute deterioration.
- 265 calls (12% of acute deterioration calls) required transfers of care to ICU/HDU, enhanced levels of care, tertiary centre or referral/transfer to specialists or a specialist ward.
- 793 (35% of acute deterioration calls) required other changes in treatment.
4 Calls analysis
This section examines who made the Martha’s Rule escalation call, calls per region and whether the call related to acute deterioration.
4.1 Key call insights
Key call insights from September 2024 to July 2025 are:
- Since September 2024, 5,583 Martha’s Rule escalation calls have been received.
- Calls have increased in line with increasing implementation.
- The highest proportion of calls (72%) came via the family/carer escalation process.
- 2,277 (41%) Martha’s Rule escalation calls related to acute deterioration.
4.2 Call trends over time
Note that this collection is not mandatory, so sites may not respond every month. Please refer to the response rates for context.
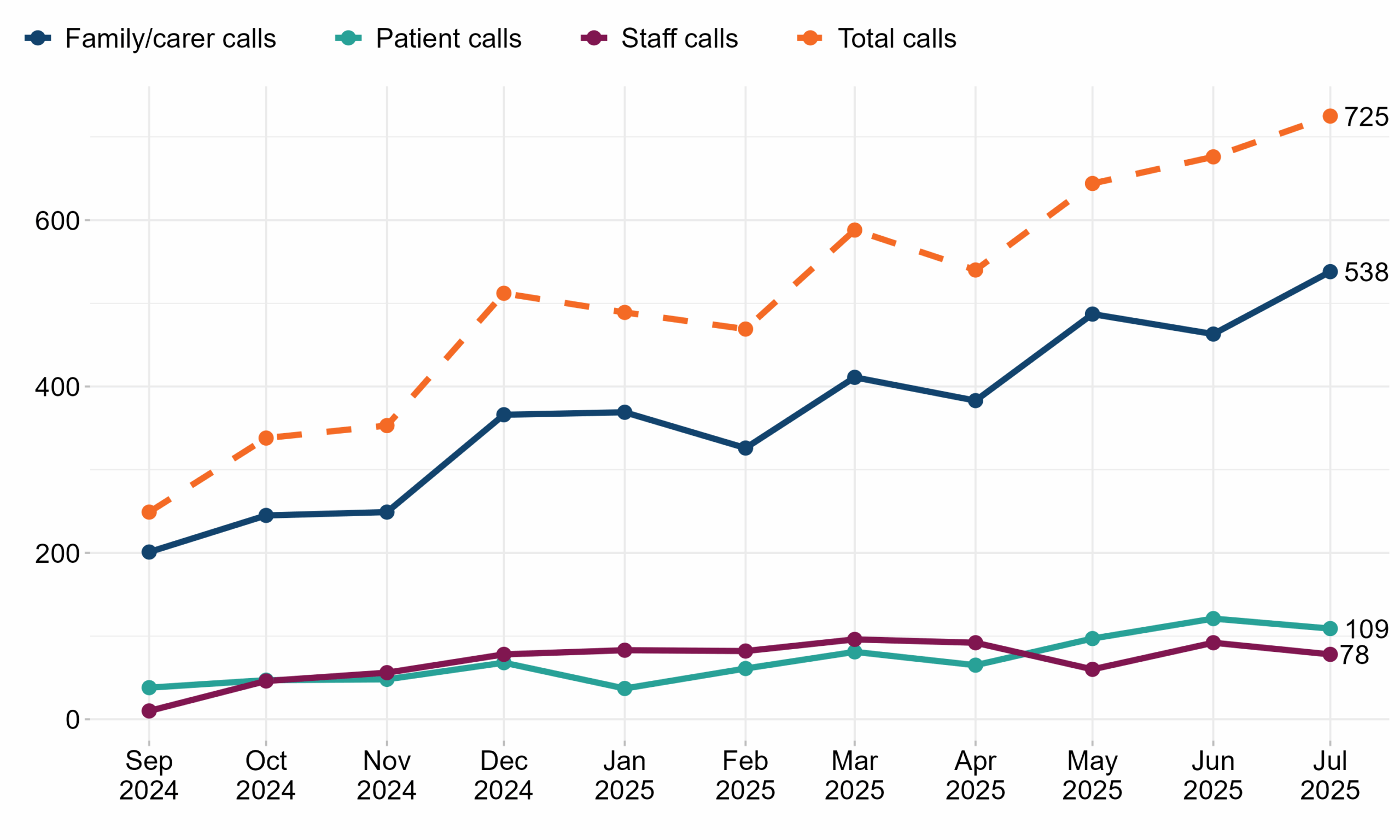
Figure 1: Number of Martha’s Rule calls per month by escalation process. Reporting period from September 2024 to July 2025.
| Date | Patient calls | Family/carer calls | Staff calls | Total calls |
|---|---|---|---|---|
| Sep-24 | 38 | 201 | 10 | 249 |
| Oct-24 | 47 | 245 | 46 | 338 |
| Nov-24 | 48 | 249 | 56 | 353 |
| Dec-24 | 68 | 366 | 78 | 512 |
| Jan-25 | 37 | 369 | 83 | 489 |
| Feb-25 | 61 | 326 | 82 | 469 |
| Mar-25 | 81 | 411 | 96 | 588 |
| Apr-25 | 65 | 383 | 92 | 540 |
| May-25 | 97 | 487 | 60 | 644 |
| Jun-25 | 121 | 463 | 92 | 676 |
| Jul-25 | 109 | 538 | 78 | 725 |
4.3 Martha’s Rule calls by NHS England region
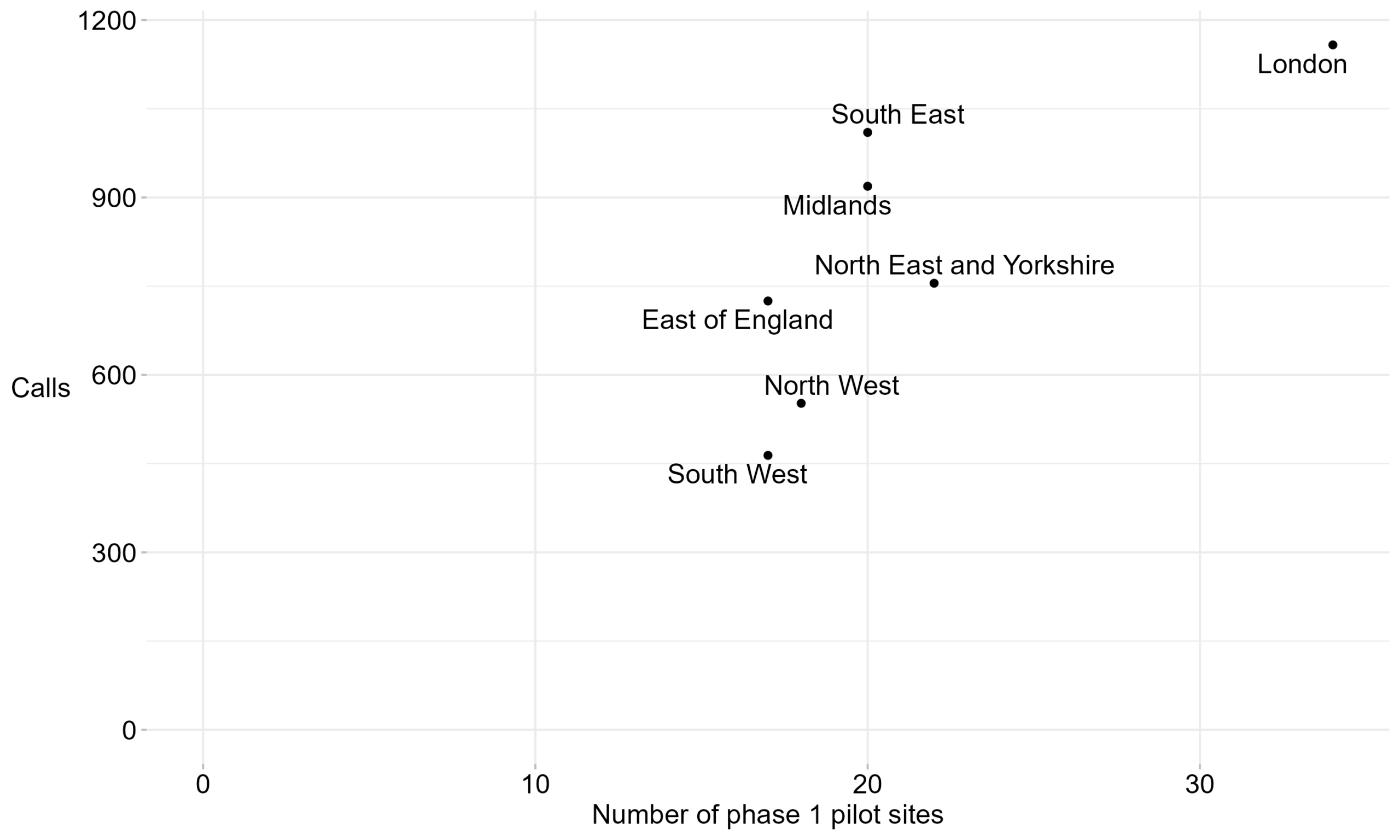
Figure 2: Number of calls and phase 1 pilot sites per NHS England region. Reporting period from September 2024 to July 2025.
Table 3: Number of calls and phase 1 pilot sites per NHS England region. Reporting period from September 2024 to July 2025.
| Region | Total calls | Number of phase 1 pilot sites |
|---|---|---|
| East of England | 725 | 17 |
| London | 1,158 | 34 |
| Midlands | 919 | 20 |
| North East and Yorkshire | 755 | 22 |
| North West | 552 | 18 |
| South East | 1,010 | 20 |
| South West | 464 | 17 |
4.4 Martha’s Rule call flow analysis
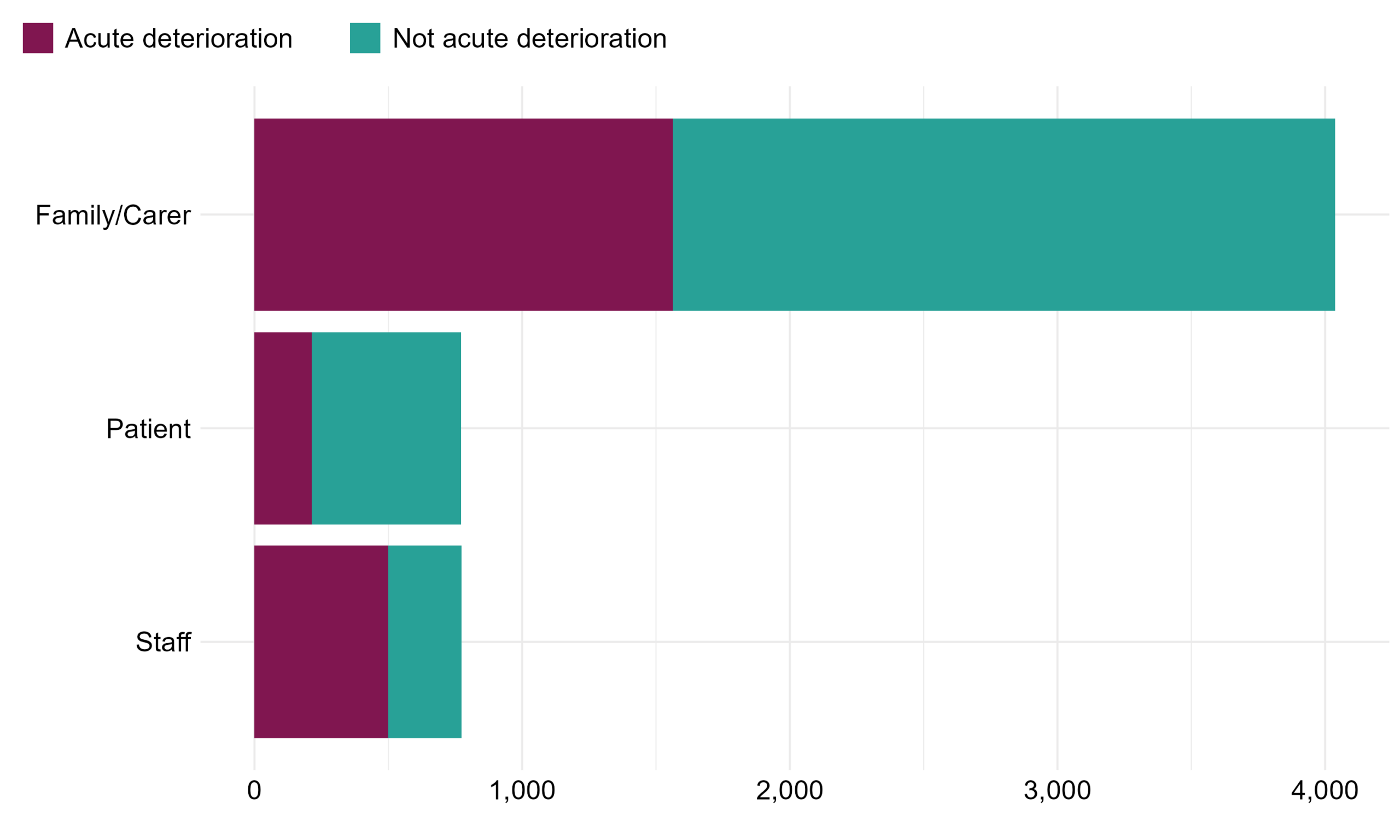
Figure 3: Number of calls by escalation process and whether the call was related to acute deterioration. Reporting period from September 2024 to July 2025.
Table 4: Flow of calls by escalation process and whether the call was related to acute deterioration. Reporting period from September 2024 to July 2025.
| Escalation route | Acute deterioration | Not acute deterioration | Total calls | Percentage of calls that related to acute deterioration |
|---|---|---|---|---|
| Family/Carer | 1,564 | 2,474 | 4038 | 39% |
| Patient | 214 | 558 | 772 | 28% |
| Staff | 499 | 274 | 773 | 65% |
| Total | 2,277 | 3,306 | 5583 | 41% |
5 Outcomes of Martha’s Rule calls
5.1 Data consolidation
In addition to the number of calls, the Martha’s Rule Data Collection also collects high-level information on the outcomes of these calls. In June 2025, the outcomes collected were refined using insight from the early pilot to strengthen learning. For the purpose of this report, outcomes have been consolidated into groups where clinically similar.
For acute deterioration calls, the number of possible outcomes expanded from six to eleven, and are grouped into three as follows:
- Documented advice (no intervention), where following acute deterioration review, no further changes were made to patient care.
- Transfers of care, which includes transfers to ICU/HDU, enhanced levels of care, tertiary centres or referral/transfer to specialists or a specialist ward.
- Other change in treatment, which includes changes to nursing, surgical or medical management such as investigations or diagnostics, new medications including antibiotics or the commencement of IV fluids or oxygen. These changes in treatment do not require transfer of a patient from a ward in-patient setting.
For the calls not related to acute deterioration, the number of possible outcomes expanded from five to eight, and are grouped into five as follows:
- Clinical concern (including medication issues, management of long-term conditions and delayed investigations)
- Communication issue (including discharge planning)
- Non-clinical concern
- Signpost to another service/team
- Other
These groups are used for Figure 4 and tables 5a and 5b, with the full outcomes data provided in tables 5c and 5d.
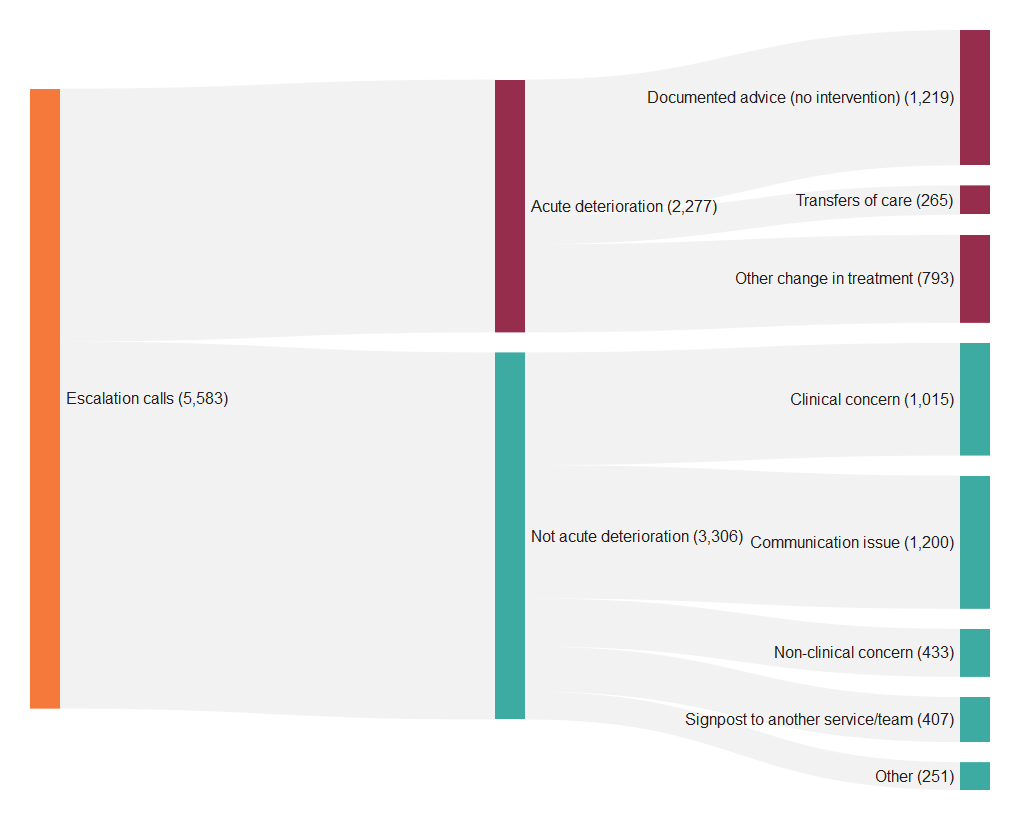
5.2 Outcome flow analysis
- Of the 5,583 Martha’s Rule escalation calls, 2,277 (41%) related to acute deterioration.
- 265 calls (12% of acute deterioration calls) required transfers of care to ICU/HDU, enhanced levels of care, tertiary centre or referral/transfer to specialists or a specialist ward.
- 793 (35% of acute deterioration calls) required other changes in treatment.
Figure 4: Flow of escalation calls from initial contact through to outcomes. Reporting period from September 2024 to July 2025. Note that from June 2025, up to three outcomes were collected for each acute deterioration call. Only the primary outcome has been visualised here.
| Outcome | Number of calls | Percentage of the acute deterioration calls |
|---|---|---|
| Documented advice (no intervention) | 1,219 | 54% |
| Transfers of care | 265 | 12% |
| Other change in treatment | 793 | 35% |
| Total | 2,277 | – |
Table 5b: Table of outcomes for calls not related to acute deterioration. Reporting period from September 2024 to July 2025.
| Outcome | Number of calls | Percentage of the not acute deterioration calls |
|---|---|---|
| Clinical concern | 1,015 | 31% |
| Communication issue | 1,200 | 36% |
| Non-clinical concern | 433 | 13% |
| Signpost to another service/team | 407 | 12% |
| Other | 251 | 8% |
| Total | 3,306 | – |
5.3 Ungrouped outcomes
Table 5c: Full table of outcomes for acute deterioration calls. Reporting period from September 2024 to July 2025.
| Outcome | Status | Grouping in report | Number of calls |
|---|---|---|---|
| Documented advice (no intervention) | Existing outcome | Documented advice (no intervention) | 1219 |
| Referral to specialist input or transfer to specialist ward | New outcome in June 2025 | Transfer of care | 32 |
| Transfer to enhanced level | Existing outcome | Transfer of care | 18 |
| Transfer to HDU/ICU | Existing outcome | Transfer of care | 99 |
| Transfer to tertiary centre (off or onsite) | Existing outcome | Transfer of care | 37 |
| Other | Removed in June 2025 | Transfer of care | 79 |
| Change in management/intervention required | Removed in June 2025 | Other change in treatment | 628 |
| End of life pathway (not for critical care) | New outcome in June 2025 | Other change in treatment | 9 |
| Investigations / diagnostics including scans / blood tests | New outcome in June 2025 | Other change in treatment | 51 |
| IV fluids, oxygen, secretion management, pain or changes to nursing care | New outcome in June 2025 | Other change in treatment | 36 |
| New medications including antibiotics | New outcome in June 2025 | Other change in treatment | 23 |
| Procedural interventions including going to theatre, drains | New outcome in June 2025 | Other change in treatment | 2 |
| Other change in management / intervention required | New outcome in June 2025 | Other change in treatment | 44 |
Table 5d: Full table of outcomes for the calls not related to acute deterioration. Reporting period from September 2024 to July 2025.
| Outcome | Status | Grouping in report | Number of calls |
|---|---|---|---|
| Clinical concern/management of a long term condition | Existing outcome | Clinical concern | 883 |
| Delayed investigations | New outcome in June 2025 | Clinical concern | 55 |
| Medication issue/delay | New outcome in June 2025 | Clinical concern | 77 |
| Communication issue | Existing outcome | Communication issue | 1115 |
| Discharge planning | New outcome in June 2025 | Communication issue | 85 |
| Non-clinical concern | Existing outcome | Non-clinical concern | 433 |
| Signpost to another service/team | Existing outcome | Signpost to another service/team | 407 |
| Other | Existing outcome | Other | 251 |
6 Children and young people
This section specifically focuses on acute deterioration calls related to children and young people (0-18 years old).
Table 6: Calls relating to deterioration in children and young people. Note: Age boundaries changed in the November 2024 data collection template so this only shows data from November 2024 to July 2025.
| Age Group | Family/carer calls | Patient calls | Staff calls | Total |
|---|---|---|---|---|
| 0-4 years | 66 | 0 | 10 | 76 |
| 5-12 years | 37 | 0 | 4 | 41 |
| 13-15 years | 13 | 0 | 3 | 16 |
| 16-18 years | 18 | 0 | 4 | 22 |
| Total | 134 | 0 | 21 | 155 |
7 Data quality notes
- This data collection is not mandatory. Therefore, different sites may submit information each month.
- The national data relates to calls made and thus one patient may have used Martha’s rule escalation multiple times.
- This data is true as of the time it was extracted, some of these figures may change subject to sites re-submitting.
- Where data quality issues were identified, these submissions were removed. This impacted 14 different sites over 8 different months (15 submissions in total).
8 Glossary
Table 7: Glossary of terms.
| Term | Definition |
|---|---|
| Martha’s Rule | Martha’s Rule is a patient safety initiative to support the early detection of deterioration by ensuring the concerns of patients, families, carers and staff are listened to and acted upon. |
| Escalation | The process of raising concerns about a patient’s deteriorating condition to ensure appropriate clinical review. |
| HDU/ICU | High Dependency Unit/Intensive Care Unit – a specialised setting within hospitals that manage patients who are critically ill and/or require additional support that cannot be provided in an in-patient ward setting. |
| Acute deterioration | Acute physical deterioration is the rapid worsening of health from a patient’s baseline. It can be identified from changes in physiology (such as respiratory rate, blood pressure or consciousness), or more subtle signs (such as not eating or a patient’s or family’s report of a change in sense of wellness, mental status or behaviour). |
| Acute deterioration call | A Martha’s Rule escalation call that has been reviewed and identified as relating to acute deterioration. |
9 Additional information
The Martha’s Rule Programme is led by the National Director of Patient Safety in NHS England. The implementation is being led and facilitated by the National Patient Safety team in partnership with the National Nursing Directorate.
Data source: the Martha’s Rule Data Collection.
10 Future publications
Your feedback is welcome on the format, frequency and utility of this document, so that we can provide reports that are of most benefit. Please contact patientsafety.analysis@nhs.net with any suggestions.