Quarter 4 2024/25 (January to March 2025)
Patient Safety Event Data Quarterly Publication
1. National Patient Safety Data Context
1.1. Transition of recording systems
NHS England previously published official statistics using National Reporting Learning Service (NRLS) patient safety incident data: the National Patient Safety Incident Reports (NaPSIR), and Organisation Patient Safety Incident Reports (OPSIR). In addition, we published monthly summary data which complemented our official statistics data reports.
However, due to its aging infrastructure, NRLS was withdrawn on 30th June 2024, and replaced by the Learn from Patient Safety Events (LFPSE) service, which has been operating since July 2021. You can read more about the new service here. Transition of all secondary care providers from the old system to the new completed in 2024. This is the first experimental publication of statistics relating to LFPSE, and as a result there are some key differences between NRLS and LFPSE which should be considered when interpreting this data. The change contributes significantly to the alteration of data output in our new official publications.
NRLS submissions required manual extract and upload, whereas LFPSE submissions occur in real time, including any updates made to records after their initial submission as the provider works towards a full and accurate picture of the event over time.
NRLS used older definitions, and was primarily used by secondary care providers, due to its reliance on secondary-use data inputted to Local Risk Management System (LRMS) software, which varies from provider to provider.
LFPSE offers an interface for providers without LRMS software to use the same tools, making it more accessible to primary care and other settings, as well as supporting submissions from private healthcare providers.
This means that NRLS and LFPSE data are not comparable, and we expect to see differences in recording patterns and usage through the transition period and beyond. This is also true for the taxonomies (question set, and answer options), as the taxonomies used within LFPSE have been updated to capture more mechanistic details of how things go wrong, to allow us to develop targeted interventions to improve safety where they will be most effective.
Although connection to the LFPSE service is now a contractual obligation, LFPSE operates as NRLS did in terms of being a largely voluntary system. Decisions on which events to record are not mandatory, except where recording a death or instance of severe harm fulfills mandatory notification requirements. Providers are encouraged to record as much as they can, and particularly what is thought useful for national learning. The same caution should therefore be applied when interpreting data which represents the numbers of events recorded, and not the number of actual events that occurred. Data principles setting out how LFPSE data can and cannot be used are available here.
1.2. Patient Safety Incident Definition
The LFPSE service defines a patient safety incident as: ‘something unexpected or unintended has happened, or failed to happen, that could have or did lead to patient harm for one or more person(s) receiving healthcare’. Full details of the definitions and harm gradings are available here.
LFPSE also captures three other patient safety event types: outcomes of concern, risks to patient safety, and instances of good care. Throughout this report, with the exception of table 1, we will be using patient safety incidents only, which constitute the vast majority of patient safety events data reported to LFPSE. Future versions of this publication will encompass other event types.
2. Data quality information
2.1. Interpreting the data
National data collected by LFPSE comes mainly as a secondary use from what is recorded by staff into local risk management systems (LRMSs). Currently NHS acute providers submit most reports we receive. However, anyone can record a patient safety event on the service: they may be healthcare staff from any NHS or private provider, patients or members of the public. LFPSE data is submitted voluntarily to foster openness and encourage continual increases in reporting. This means LFPSE data does not, and cannot, provide the definitive number of patient safety events occurring in the NHS; it measures the number of safety events recorded. The number of recorded safety events has increased year on year, which likely reflects improved recording culture and cannot necessarily be interpreted as the NHS becoming less safe. This document was extracted on 13th May 2025 and serves as a quarterly snapshot of the data currently held in LFPSE.
2.2. Missing values
Missing values have been handled and removed from the tables and plots, so the total counts will vary across tables.
2.3. Cleansing
Records that have been submitted with patient identifiable information and are yet to be anonymised will not appear in these data. Records that have submitted and subsequently updated that contain patient identifiable information, and are yet to be re-anonymised, will be displayed as their previous version in these data until anonymised.
2.4. Event Types
As described in section 1.2, LFPSE brings the feature to record patient safety event types beyond incidents. Recorders can now also upload patient safety risks, outcomes, and instances of good care. This is to ensure the database contains more instances of care that the healthcare system can learn from instead of only detailing errors involving patients.
Table 1: Count of the Event Types in LFPSE
Based on patient safety event records from January 2025 to March 2025.
| CL001 – Event Type | Number of Events | Percentage |
|---|---|---|
| Incident | 800,714 | 96.78% |
| Good care | 12,035 | 1.45% |
| Risk | 9,824 | 1.19% |
| Outcome | 4,824 | 0.58% |
| Total | 827,397 | – |
3. Recording patterns by physical harm
3.1. Psychological Harm
LFPSE has a new variable for grading of the psychological harm associated with the reported patient safety incidents. This is an experimental field which seeks to explore if responses to safety incidents need to be different if psychological harm is considered separately from physical harm, rather than rolling them together into one measure (as was done in the NRLS). Currently, there is low confidence in the grading of psychological harm, as users familiarise themselves with its use, and as such, it is excluded from this analysis.
3.2. Physical Harm
Grading the degree of harm to a patient resulting from a patient safety incident can be a challenge for reporters, but by grading patient safety incidents according to the harm they cause patients, local organisations can ensure consistency and comparability of data. This consistent approach locally will enable LFPSE to compare, analyse and learn from data nationally. This grading can also be used to “triage” incidents for review both locally and nationally, ensuring the most serious events are looked at first.
3.3 Harm policy
For more information on harm grading please see the harm grading policy guidelines.
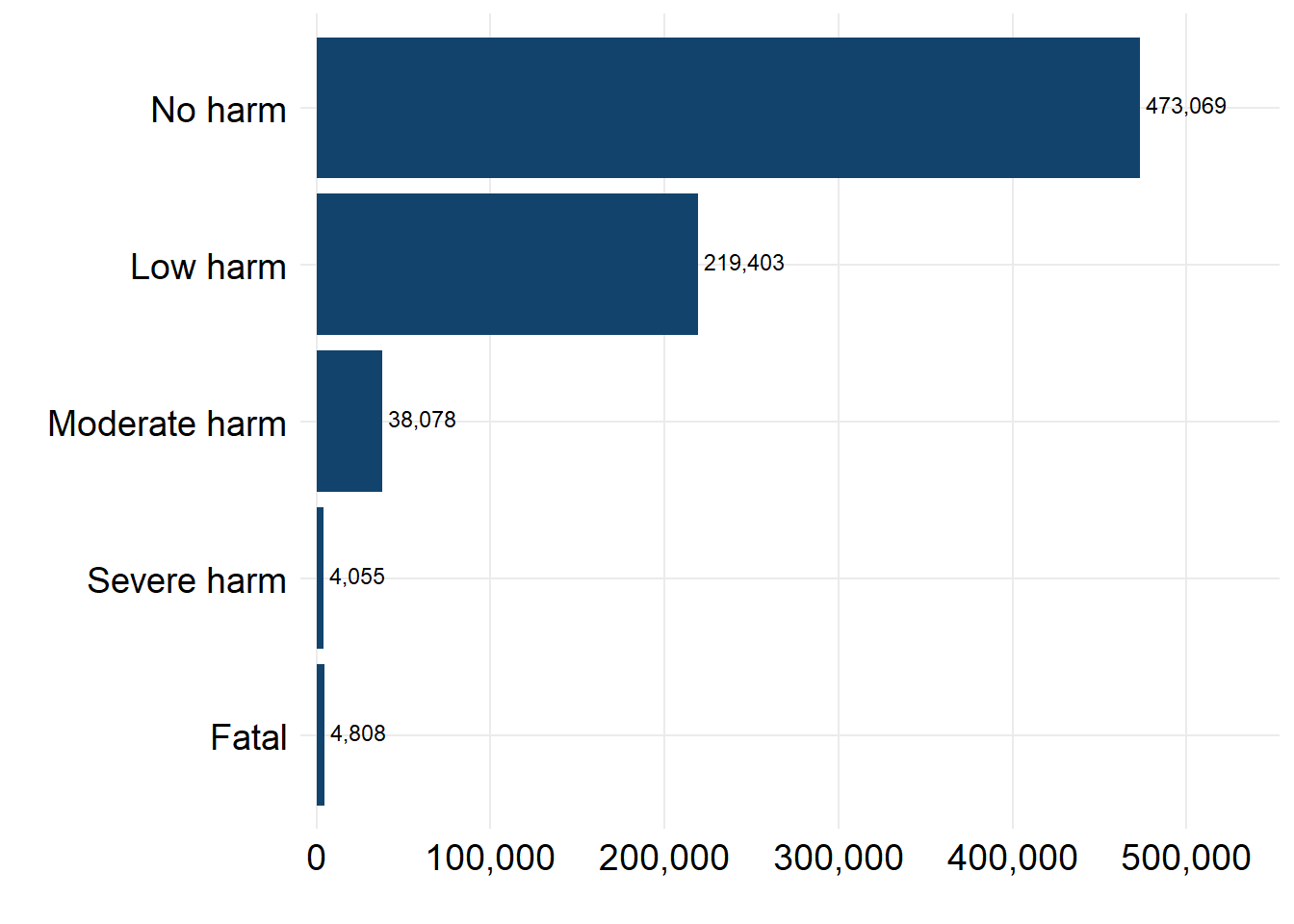
Sometimes a problem in care can affect more than one patient, or none at all. To capture this, as a new feature of LFPSE, recorders can submit information for multiple patients per incident, meaning there can be multiple degrees of harm per incident. For the following figure and table we have taken the highest harm level per incident. Where a degree of harm was recorded (n = 739,413), the majority of incidents (93.65%) recorded low or now physical harm to patients.
Figure 1: Count of patient safety incidents by maximum physical harm
Based on patient safety incidents records from January 2025 to March 2025.
| OT001 – Maximum level of physical harm | Count of Reported Incidents | Percentage |
|---|---|---|
| No harm | 473,069 | 63.98% |
| Low harm | 219,403 | 29.67% |
| Moderate harm | 38,078 | 5.15% |
| Severe harm | 4,055 | 0.55% |
| Fatal | 4,808 | 0.65% |
| Total | 739,413 | – |
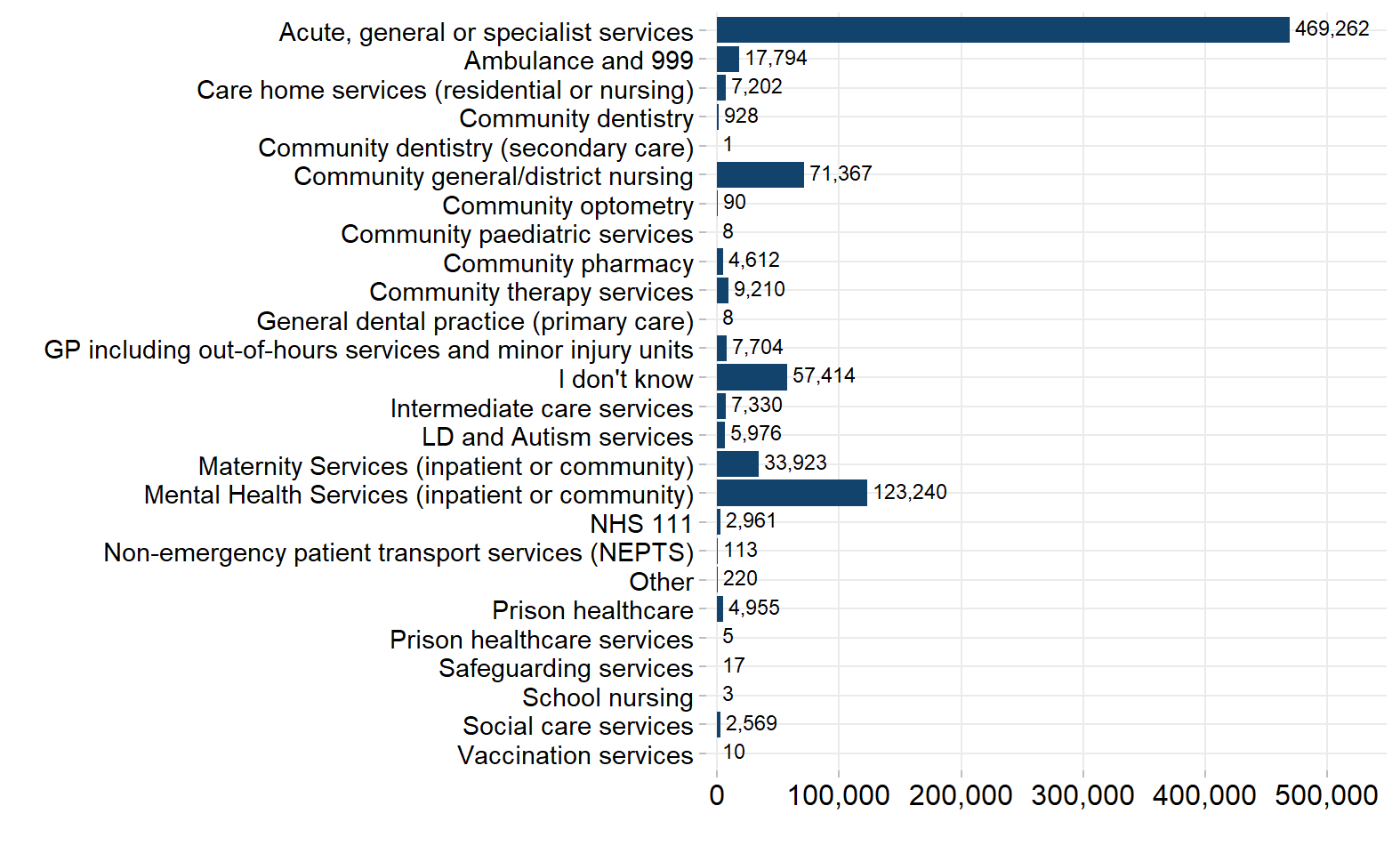
4. Recording by service area
LFPSE taxonomy is periodically updated based on the insight/value they provide as well as data capture and user experience. This means there will be some variability between the data captured under different versions. In the plot below, we have grouped some granular categories into broader service groups to account for differences in the recording of service areas between version 5 (used by the majority of the LRMS users) and version 6 (used in the online forms).
- ‘Maternity inpatient services’, ‘Maternity community services’ and ‘Maternity services (inpatient or community)’, have been coalesced to ‘Maternity Services (inpatient or community)’
- ‘Mental health community services’, ‘Mental health services (inpatient or community)’ and ‘Mental health inpatient services’, have been coalesced to ‘Mental Health Services (inpatient or community)’
- ‘GP including out-of-hours services and minor injury units’, ‘GP including out-of-hours services’ and ‘Minor injury unit (MIU) / Urgent treatment centre’, have been coalesced to ‘GP including out-of-hours services and minor injury units’
The service area variable can contain multiple responses if the incident occurred in more than one area. As a result, some incidents will be counted more than once, so the figures here cannot be totalled without double-counting records.
Figure 2: Count of incident records by service area
Based on patient safety incidents records from January 2025 to March 2025.
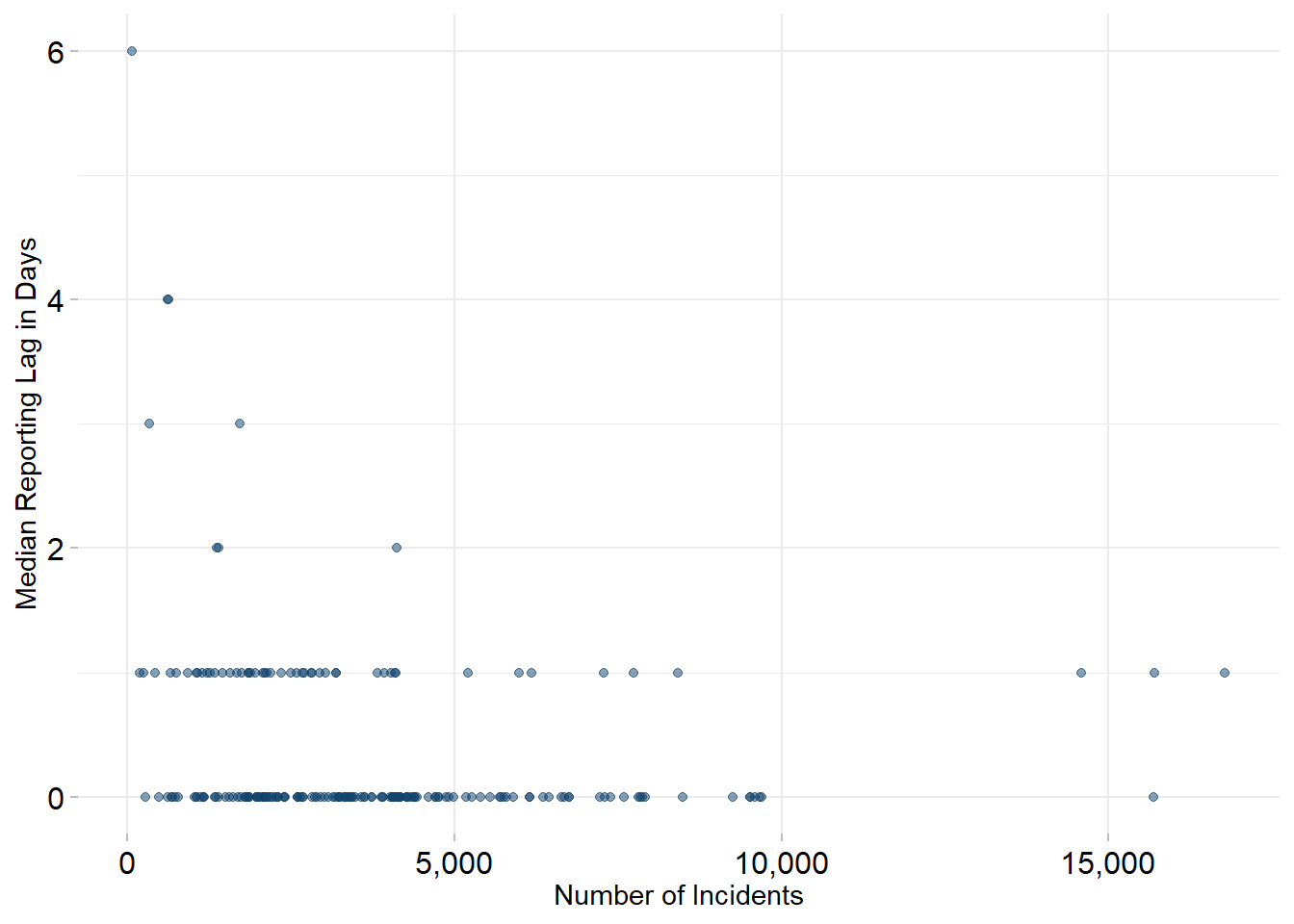
5. Reporting lag
Reporting lag for patient safety events is measured as the difference in the number of days between the date the patient safety incident occurred and the date that it was reported to LFPSE. The median lag is then taken to minimise the effect of any outliers (such as events which only become apparent many years after occurring). In the current period there are 4,165 patient safety incidents without an incident occurring date and therefore a lag could not be calculated for these records.
In the financial year ending March 2022 (the latest period for which data is published), the median lag for reporting into the NRLS was 20 days. In LFPSE for the current reporting period, the equivalent figure was 0 days. This reduction is due to the live nature of LFPSE, replacing the requirement for providers to manually extract and upload data as was the case for NRLS.
Figure 3: Number of incidents and median reporting lag across NHS trust
Based on patient safety incident records from January 2025 to March 2025.
6. Organisation level
This table contains the number of patient safety incidents recorded, and the median lag for recording these incidents, for NHS Trusts. During the current period there were 18,399 incidents where an organisation code was not present and therefore an organisation could not be identified. These incidents are thus not included in these counts.
Table 3: Median day lag and number of reports across NHS trusts
The organisation-level table can be downloaded as a CSV file.
7. Future publications
For the next iteration of this report due to be published on 12th June 2025, bed days data will be published for the reporting period, which will enable us to provide patienty safety event recording rates by NHS trust, using bed days as a proxy to standardise their overall activity. Your feedback is welcome on the format, frequency and utility of this document, so that we can provide reports that are of most benefit. Please contact patientsafety.analysis@nhs.net with any suggestions.